Abstract
In the new millennium, evidence-based practice (EBP) cannot be overlooked by dental clinicians. Mineral trioxide aggregate (MTA) is a biomaterial that has made a great impact in dental practice. Evidence-based practitioners who wish to utilise the current best evidence into their practices are sometimes confused with the MTA research exponential growth since 1993, i.e. existence of several randomised clinical trials with inhomogeneous results.
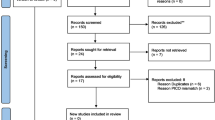
This chapter aims to guide the reader through the steps and concepts of EBP in dentistry. The chapter will provide readers with basic knowledge of EBP by discussing the levels of evidence and grades of recommendation, framing a foreground question, finding the evidence, and then critical appraisal. Using the principles and methods of EBP, the chapter tends to focus on MTA and its multiple uses in dentistry, thus providing a timely resource for evidence-based practice with MTA for four specific clinical applications: (1) root-end filling, (2) vital pulp therapy in primary teeth, (3) management of immature permanent teeth, and finally (4) vital pulp therapy in mature permanent teeth.
Every attempt has been made to find the most recent and highest ranking evidences for this chapter, hoping that such a remarkable collection of evidence with high quality might increase MTA evidence-based practice in modern dentistry.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
9.1 Introduction
This new millennium has seen a huge ‘information explosion’; each day produces vast amounts of data and knowledge in all branches of science. Knowledge doubling studies indicate that the trend of human data production has gradually increased over time. Within the recent decades, growth has become exponential, with significant amounts of data being added regularly to the pool.
It has been estimated that the doubling time of medical knowledge in 1950 was 50 years, in 2010 it was as little as 3.5 years, and in 2020, if this trend continues, it will be a staggering 73 days [37]. It means that students who began medical school in 2010 will experience roughly three doubling of knowledge before graduation, whilst students who graduate in the year 2020 will experience at least four doubling of medical knowledge throughout the course. Incredibly, medical knowledge till the beginning of the third millennium is likely to be less than 2 % of what will be known by 2020.
This exponential growth in medical/dental knowledge has created new and complex problems when clinicians wish to retrieve suitable information. Numerous new scientific articles and journals are added to various databases each day. PubMed at present is the most popular medical database covering 5,500 journals and more than 24 million citations, nearly 1 % of which are dental publications. In the presence of this huge amount of data, the question posed is: Are dental practitioners accessing and utilising the correct information? Clearly, keeping up to date is an overwhelming task.
Such a task can only be efficiently carried out by utilising the principles and methods of evidence-based practice. EBP involves scientific ranking of studies, selection of beneficial data and summarisation of results from the selected studies. Ultimately, these steps lead to a wealth of information into a simple and coherent statement: the clinical bottom line.
9.2 What Is ‘Evidence-Based Practice’?
Aim
To define evidence-based practice (EBP) and to introduce the steps of EBP.
The first and most important question is ‘what is evidence-based practice?’ The term ‘evidence-based’ was first described by Gordon Guyatt in Canada in the early 1990s; now it is a very established term in medical and dental glossaries.
Based on the book entitled Evidence-Based Medicine: How to Practice and Teach EBM, by Sackett et al. [95], EBP is a way of thinking and working. It can be defined as a systematic approach to clinical problem solving which allows integration of (1) the best current/available evidence with (2) our clinical knowledge/skills and (3) our patient’s value/preferences. When these three elements are integrated, clinicians and patients form a diagnostic and therapeutic alliance, which optimises clinical outcomes and quality of life [95]. In addition, EBP is not a static state of information but rather represents a continuously developing state of knowledge. In this systematic approach, employment of the best valid evidence invalidates or further elaborates previously accepted treatments and replaces or strengthens their evidence with proven successful and safe interventions.
To accomplish EBP, the following five steps are essential: (1) constructing an answerable, relevant and foreground clinical question; (2) finding/collecting the best available evidence to answer the question; (3) appraising critically the evidence for its results/validity/relevance; (4) pragmatic integration of the best current evidence with the practitioner’s knowledge/skills and the patient’s value/preferences; and (5) self-evaluating and audit of the effectiveness/efficiency of previous steps with a view to improvement.
The main objective of EBP using these five steps is the application of the best current evidence in forming clinical decisions/actions to improve the quality of the patient’s management and life. Dental clinicians need to be familiar with the concept of levels of evidence (LoE), have knowledge of correct appraisal of evidence and identify the grades of recommendation (GoR). These significant skills are discussed in detail in this chapter, alongside with the aforementioned steps 1–3 entitled ‘endodontic practice with mineral trioxide aggregate’. The application of the final two steps will be the clinicians’ responsibility.
9.3 Levels of Evidence and Grades of Recommendation
Aim
To learn the different schemes of levels of evidence and grades of recommendation available when making clinical decisions.
As a component of EBP, there are a range of ranking systems that are used to sort published studies into their respective levels of evidence (LoE). These systems are designed as guidance and can be very useful in acquiring a quick overview of the desirable LoE.
LoE is classified in many different ways; the Oxford Centre for Evidence-Based Medicine and the Scottish Intercollegiate Guidelines Network (SIGN) are two of the best-known ranking systems worldwide. Using these two systems, a new modified ranking system was developed in the Knowledge Management Unit (KMU) of the Iranian Center for Endodontic Research (Table 9.1). In this ranking system, the strength of published studies is determined in accordance to their study designs and quality ranking.
High-quality systematic reviews and prospective randomised clinical trials (RCTs) with a very low risk of bias (well-designed methodology) are designated the highest rank (LoE1), followed by high-quality semi-experimental studies or low-quality randomised controlled trials (LoE2), high-quality systematic reviews of case-control studies (LoE3), case series (LoE4) and finally case reports as well as an expert opinion (LoE5). Notably, high-quality studies require stronger research methodology, are more difficult to carry out and consequently are rarer. Also, in vitro and animal studies are not considered valid evidence as the effects of materials/techniques in laboratory (in vitro) situations are not essentially the same as in the human body; the intervention outcomes are often dissimilar in animals and humans and likely to be dissimilar within various mammals.
When biomaterials like MTA become available to the dental market, they are usually subjected to a number of studies conducted in vitro or ex vivo assessment of their biological/chemical/physical properties. However, these usually have no meaningful correlation with in situ clinical situations; the results of a limited number of review articles in the field of dental materials have revealed that there are poor correlations between laboratory test values and clinical performance [20, 21, 50]. Further reports have shown a lack of consistency between the results of two bacterial and dye microleakage methods for sealing ability of the same root-end filling materials [57]. Therefore, as the results of these methodologies do not have clinical significance, the results of in vitro and animal studies are not considered as valid evidence. As a final note, diagnosis, prognosis and treatment topics require different LoE for clinical application/decision.
Finding the appropriate evidence via searching scientific databases is a difficult task due to the large pool of individual studies available. This usually requires clinicians to access and critically appraise studies in order to classify the LoE and assess the clinical application of the best evidence. In contrast, summaries (systematic reviews) assess and present evidences from primary individual studies and tend to alleviate the need for accessing and appraising individual studies, thus greatly facilitating evidenced-based clinical decision-making.
In addition to individual original studies and systematic reviews, there are also two other categories of clinical information resources named synopses and systems. Synopses are summaries of research evidence that usually include guidance/advice regarding specific clinical application by qualified experts. This form of guidance externally assesses the evidence and provides strengths and weaknesses for each study; there are a limited number of synopses in dental literature. Systems are defined as textbook-like resources that summarise clinical evidence with other types of information directed at clinical practice decisions; this type of evidence is also limited but provides clear answers leading to appropriate clinical action/care, i.e. ‘health technology assessment (HTA)’ and ‘evidence-based practice guideline (EBPG)’. HTA is used for the evaluation and determination of safety and effectiveness of a new technology; for example, new biotechnology of ‘MTA pulpotomy of mature molars with irreversible pulpitis’ can be evaluated in terms of effectiveness as well as safety-related factors and social implications, i.e. affordability, availability, accessibility and acceptability. These studies usually evaluate the ethical, social and economic implications of a new technology on health status and health-related quality of life for the general populations. Like a bridge between the world of research and decision-making, HTA studies help health policymakers adopt appropriate decisions and subsequently propagate, popularise and establish the new technology.
Based on unbiased analysis of the best available evidence, numerous EBPGs have been developed by medical associations or governmental bodies as national/international recommendations to guide high-quality patient care. Typically, EBPGs can provide recommendations for prevention and treatment of diseases; they generally contain a simple summarised consensus statement on best practice in health care. A health-care provider is required to know the EBPG of his/her profession and has to decide whether or not to practise the recommendations for that individual patient.
Grades of recommendation (GoR) defined as the strength of evidence for a recommendation is determined by searching/reviewing all the related literature on that subject. The number and quality of available related literature should be used as the basis for ranking the recommendation. Most of the multiple grading schemes are based on LoE. The definitions of GoR used in this chapter are modification of those used in the classification system proposed by the Scottish Intercollegiate Guidelines Network (SIGN). Grades of recommendation are usually stated with letters. In this modified GoR, constructed in the Knowledge Management Unit (KMU) of the Iranian Center for Endodontic Research, grades A to E stand for good- to poor-quality evidence for recommending intervention (Table 9.2).
9.4 Framing a Foreground Question (Using PICO)
Aim
To present the process of formulating an accurate and effective foreground Population, Intervention, Comparison and Outcome (PICO) question.
A good question is half the science. (Hasan-ibn Ali Alayhis-salam)
In current clinical practice, answering to relevant questions requires special types of data/information. An imprecise question results in an imprecise answer; the more specifically we can formulate the question, the greater our chance of getting a decent answer in dental literature. Formulating a high-quality and answerable question is the preliminary step of EBP.
Sackett et al. identified two types of questions: background and foreground [95]. Background questions are general knowledge questions and are usually answered by original articles (primary resource), review articles (secondary resource) and textbooks (tertiary resource); review articles are the best source as they condense and summarise evidence derived from original studies. These articles cover a broad topic, are rich sources of background information, are usually readily available and provide numerous references. Background questions typically have two parts: a question root, ‘i.e. what, why, when, where, who and how?’ and ‘the name of a disease/treatment’. For example, ‘What is irreversible pulpitis?’ or ‘How do I perform primary molar formocresol pulpotomy?’ Dental students and junior residents most frequently ask background questions.
Foreground questions concentrate on specific information required for clinical decision/actions and include questions of diagnosis, treatment or prognosis of a disease, e.g. Can irreversible pulpitis be accurately diagnosed clinically? and Is root canal therapy the only treatment available? These questions are best answered by searching the high-LoE published articles, not by textbooks; foreground questions are the most frequent type of questions generated by senior residents and clinicians. Generally, the question must be phrased in a way that directs the subsequent search to relevant and precise answers. Finding an accurate answer in scientific literature can be attained by subdividing the foreground question into four parts: (P) Patient(s)/Problem, (I) Intervention, (C) Comparison and (O) Outcomes; the acronym PICO helps to remember the key components of a clear and well-focused question. The question needs to identify the main problem of the patient, the main intervention/treatment considering the patient’s problem, the standard management, and the effectiveness/outcome(s) of interest. A PICO feature is also accessible on PubMed (http://pubmedhh.nlm.nih.gov).
PICO formulating method provides a conceptual framework for more effective searching. An example for a single, well-focused and clearly identified foreground question is: ‘In children with asymptomatic pulp exposure (P) how does MTA pulpotomy (I) compare with conventional formocresol pulpotomy (C) for the successful clinical and radiographic outcomes (O)?’
9.5 Finding the Evidence
Aim
To develop a research strategy in order to locate and find published high-level evidences in that field of dentistry.
After framing a PICO question, the next step is good literature search for evidence with the highest LoE. Searching for evidence is a difficult and time-consuming task, particularly with the rapid growth of knowledge in peer-reviewed published literature. To identify relevant studies, the search strategy may include hand searching of hard copies or electronic searching of databases and search engines; however, hand searching is a difficult job for clinicians and even researchers.
Question type (i.e. aetiology, diagnosis, treatment and prognosis) can play a significant role to determine the best source of evidence. For example, a PICO treatment question regarding ‘outcome comparison of current best practice with a new therapy’ needs to find LoE1 studies from the Cochrane Library, Medline (PubMed) and evidence-based websites (i.e. The Dental Elf); however, for a prognosis question, searching Medline (PubMed) alone for cohort studies suffices.
The Cochrane Library is the best source of summarised high-quality systematic reviews of randomised controlled trials, named Cochrane Reviews. Cochrane researchers usually perform hand searching as well as searches of Medline (PubMed) and Embase databases to identify studies that are relevant to the question they are trying to answer. Then, the quality of studies found is carefully assessed using valid quality scales such as Delphi or van Tulder Lists. They apply statistical analysis to compare the data of the clinical trials and to create a systematic review which usually gives the best current word on the effectiveness/efficacy of an intervention. The reviews are available at http://www.thecochranelibrary.com.
If there are no Cochrane reviews that can answer the PICO question, the next step is search PubMed. PubMed is a free search service of the US National Library of Medicine (NLM) that collects >22,500,000 citations from 5,500 indexed journal on life sciences and biomedical topics; 13,326 million articles are recorded with their abstracts, and 14,369 million articles have links to full text; there are 3,916 million free full-text articles. A staggering 700,000 new articles were added to the database in year 2012. This useful and easy-to-use bibliographic database contains titles, citations, keywords and abstracts for most of the peer-reviewed scientific biomedical literature dating back to the 1950s. PubMed is part of the Entrez information retrieval system accessing primarily the Medline database and was first released in January 1996.
Simple search strategies on PubMed can be a mix of controlled vocabulary such as Medical Subject Headings (MeSH) terms and free text or keywords related to a PICO question which enter into search window (http://www.ncbi.nlm.nih.gov/pubmed/). PubMed automatically translates the term/words and adds field names, relevant MeSH terms and synonyms, which greatly enhances the search formulation; i.e. ‘causes pulpitis’ is translated as (“etiology”[Subheading] OR “etiology”[All Fields] OR “causes”[All Fields] OR “causality”[MeSH Terms] OR “causality”[All Fields]) AND (“pulpitis”[MeSH Terms] OR “pulpitis”[All Fields]). This simple broad search is likely to find most of the relevant articles; however, it may also retrieve many irrelevant citations. The appropriate use of Boolean operators AND, OR and NOT is a reliable way to control searches and retrieves a good degree of relevant citations. In addition, applying limits such as human versus animal research, age groups, year of publication, language and more importantly publication types reduces the number of irrelevant hits and usually uncovers the highest level of evidence.
Clinical Queries filter is a unique feature of PubMed tools and provides a quick/simple way to search ‘Clinical Study Categories’, as well as ‘Systematic Reviews’ subjects. The Category and Scope methodological filters can retrieve clinically relevant studies with significant precision. It was shown that ‘systematic reviews can be retrieved from Medline with close to perfect sensitivity or specificity, or with high precision, by using empirical search strategies’ [67].
Assessing the evidence-based synopses such as The Dental ELF or critically appraised topic such as UTHSCSA Dental School CAT Library are another options for finding the required evidence. These databases show CATs or synopses of individual studies that have been critically appraised and include evidence-based journal reviews, critically appraised topics and clinical evidence.
There are a few useful evidence-based dentistry resources on the Internet including ‘Journal of Evidence-Based Dental Practice’ and ‘Evidence-Based Dentistry’ journals as well as websites such as ‘The Centre for Evidence-Based Dentistry’. The two journals report on high-quality clinical studies that can impact dental practice. In addition, ClinicalTrials.gov as a service of the US National Institutes of Health is a registry site and searchable database of clinical trials in progress which are being conducted around the world. Even then the clinician is required to use his/her own critical appraisal.
Locating and exploiting print and electronic resources has normally been the role of the librarian; therefore, assistance of an expert familiar with various electronic resources, search terms and search strategies is always valuable.
9.6 Interpreting the Best Evidence (Critical Appraisal)
Aim
To focus on the skills necessary to critically evaluate and weigh information concerning the effectiveness of a new intervention.
Many clinicians believe that a wide range of study types can be brought to bear on answering clinical questions; undoubtedly, that is an accepted initial concept [94]. However, for an ‘A’ grade evidence-based clinical recommendation (GoR-A) regarding a treatment topic, the best level of evidence includes results from high-quality meta-analyses/systematic reviews of randomised controlled trials or high-quality randomised controlled trials. This chapter focuses on such evidences, as the next level of the recommendation (GoR-B) might be from low-quality conducted meta-analyses/systematic reviews of good trials or high-quality conducted of fair studies (Table 9.2), which are both insufficiently powered.
Development of critical appraisal skills is essential for clinicians to have an evidence-based approach to practice; the individual practitioner should be able to review and rate the evidence. However, time can be saved by looking for sources of summarised LoE1; the first port of call and the easiest is searching the Cochrane Library for Cochrane Reviews. If a suitable paper is not found, we would recommend searching Medline via PubMed for systematic reviews and randomised controlled trials.
There is a general consensus that systematic reviews provide the highest evidence; however, they are not equally reliable and successful in minimising bias. A number of techniques are available to assess the methodological quality of systematic reviews; amongst which is AMSTAR (a measurement tool to assess systematic reviews), a reliable and valid measurement tool that has been widely accepted and utilised [101]. It consists of eleven items with good face and content validity (available at http://www.amstar.ca/Amstar_Checklist.php); when all the checklist items have been fully addressed, a well-done systematic review is established.
Published randomised controlled trials in peer-reviewed journals also have different quality and level of evidence. The LoE provided by a randomised controlled trial depends on the ability of the study design to minimise the possibility of bias. To assess the risk of bias, the methodological quality of randomised controlled trials is commonly evaluated using various quality scales. It was reported that there are more than 20 scales and associated modifications to assess the quality of randomised controlled trails [81]. Most of these scales have not been adequately developed for assessing the internal and external validity of trails.
Internal validity is the degree to which research results are likely to be correct and free of bias. It usually reflects the extent to which the trial meets the criteria of random allocation, concealment, baseline comparability, blinding of patients/therapist(s)/assessor(s), withdrawal/dropout rate/reasons and statistical analysis. Internal validity is a prerequisite for external validity. External validity refers to the ability to generalise the results of a trial to other settings/populations outside the experimental situation; this is also called generalisability.
There are usually five main items in the various quality assessment scales; these consist of patient selection, blinding, interventions, outcomes and statistics. Jadad scale is the most common tool for ‘pain’ research assessment; however, it contains very few items (n = 5). On the other hand, Nguyen scale, which is based on generally accepted methodological criteria for evaluation of ‘dental injury’ trials, contains too many items (n = 100). The 9-item Delphi List, as a generic criteria list, was developed by international consensus and introduced in 1998 [119]. It was reported that this list is the original source for most of the quality scales. The Cochrane Collaboration Review Groups (CCRG) also used the Delphi List for their analysis in more than 2000 reviews before 2003. More recently, CCRG adopted the van Tulder List with 11 items as the latest modification of the Delphi List for many of its systematic reviews [118]. This criteria list has been adequately developed and tested for face and content validity and reliability. A modified van Tulder comprehensive list was adapted by our KMU, which consists of the following items:
-
1.
Patient selection (i) randomisation, (ii) allocation concealment and (iii) groups’ similarity at baseline
-
2.
Blinding (iv) of outcome assessor(s), (v) care provider(s) and (vi) patient(s) and also calibration (vii) of outcome assessor(s)
-
3.
Interventions : (viii) avoidance of co-interventions, (ix) adequate follow-up period, (x) description of withdrawal and dropouts, (xi) comparison of the outcome assessment timing in all groups, (xii) relevant outcomes, (xiii) adequate sample size and (xiv) using of objective outcome measures
-
4.
Statistics (xv) intention-to-treat analysis (Table 9.3)
Table 9.3 Modified van Tulder List
These criteria can be scored as yes (+1), or no/don’t know (0). The quality score of randomised controlled trials is computed by counting the number of positive scores. A published study reporting a randomised controlled trial could therefore receive a modified van Tulder score of between 0 and 15 (strongest evidence).
9.7 MTA in Clinical Practice
9.7.1 Background
A recent study that conducted a keyword search ‘mineral trioxide aggregate’ in PubMed found 1,024 published articles from 1993 till August 2012 [17]. Only ~5 % were classified as LoE1; Iran, Brazil and the UK ranked highest for providing LoE1 MTA articles. MTA was first introduced for repair of lateral root perforations as well as root-end fillings in 1993 [58, 115]. After FDA approval of the material in 1998, Prof. Torabinejad, the inventor of this novel biomaterial, described the clinical procedures for four applications of grey-coloured ProRoot MTA based on 19 published in vitro and animal studies; these include direct pulp capping (permanent teeth with reversible pulpitis), apexification, repair of root perforations and root-end fillings [112].
To overcome the potential discolouration of tooth structure with grey MTA in aesthetically sensitive areas, a new type of MTA with a tooth-coloured formula was introduced. However, there are few reports which discuss the new white ProRoot MTA discolouration effect.
The introduction of MTA as an excellent sealant of the pathways of the pulp (inner and outer dental surfaces) has made a great worldwide impact in endodontic and general dental practice. The new millennium has seen the introduction of numerous brands of MTA and MTA-like materials worldwide as well as additional uses and applications of this biomaterial which are described in detail in this book. Many published studies showed favourable outcomes for additional clinical applications for different types of MTA including vital pulp therapies in primary teeth as well as permanent teeth with established irreversible pulpitis, revascularisation treatments, management of internal and external root resorption and root canal obturations. The various clinical applications of MTA are discussed in detail in Chap. 6.
A Cochrane Library search up to April 2013 amongst ~7,800 records revealed less than 200 reviews published in the field of dentistry/endodontics and just two reviews that only mentioned the name of MTA: ‘Pulp management for caries in adults: maintaining pulp vitality’ and ‘Pulp treatment for extensive decay in primary teeth’ [66, 70].
In the first review, however, the results revealed that there is no definitive conclusion as ‘the most effective method of pulp treatment of asymptomatic carious teeth’; the authors stated that there has been a recent move towards using alternative materials and methods such as the direct/indirect placement of bonding agents and mineral trioxide aggregate for the management of the pulp in extensively decayed teeth. They concluded that ‘further well-designed randomized controlled trials are needed to investigate the potential of contemporary materials which may be suitable when used in the management of carious teeth’. In the second review, the authors also stated that more evidence of effectiveness is required for mineral trioxide aggregate pulp treatment technique.
It is disappointing that after 20 years of introducing MTA in the dental world there are no high-quality Cochrane reviews discussing its clinical applications. However, we hope that in the near future such reviews will be formulated. Accordingly, data locating, finding and collection in this chapter will be based on electronic searches of the PubMed (Medline; 1966 to April 2013), The Dental ELF, UTHSCSA Dental School CAT Library, Journal of Evidence-Based Dental Practice as well as Evidence-Based Dentistry and ClinicalTrials.gov.
9.7.2 Mineral Trioxide Aggregate for Root-End Fillings
PICO Question
When endodontic surgery is indicated, how does MTA compare to other root-end filling materials in terms of clinical and radiographic outcomes?
9.7.2.1 Definition
Surgical endodontics is an important treatment option for teeth with persistent apical periodontitis (AP). It usually includes pathological tissue removal, root-end resection, root-end cavity preparation and finally insertion of a root-end filling material; the filling material seals the root canal contents and thus prevents exit of microorganisms and their by-product into the periradicular tissues.
MTA was first introduced as a root-end filling material, and it has shown good sealing property compared to traditional filling materials in vitro and favourable biocompatibility ex vivo as well as in animal studies [113]; it stimulates hard tissue healing in surrounding tissues particularly cementogenesis in animal models [12, 114]. There are many case reports and clinical studies that show positive outcomes; however, there are a few randomised controlled trials as discussed below.
Apical/periradicular periodontitis (AP) is a type of periodontal disease usually with an endodontic origin. The disease presents itself as a low-grade inflammation of the periodontium in the area around the main entrances of the root canal system at the root apex or various levels along the root surface of a tooth and is usually asymptomatic (chronic form). The inflammation is generally accompanied by bone destruction which allows radiographic detection of AP. Appearance of symptoms such as pain, swelling and impaired function is an indicator for acute form of AP. It is generally agreed that either newly developed or persistent AP in radiographic examination is a sign of failed endodontic treatment.
9.7.2.2 Incidence/Prevalence
A systematic review of epidemiological studies in 2012 on more than 300,000 teeth from 33 studies mostly performed in developed countries demonstrated that the prevalence of endodontically treated teeth is very high, broadly equivalent to two treatments per patient with 36 % failure rate (persistent AP) [83].
9.7.2.3 Aetiology
Persistent AP after endodontic treatment is an indication of inflammation of periodontal ligament which is usually due to microbial invasion. There is a dynamic process at the interface of root canal system (the source of microbial invasion in necrotic teeth) and host defence in periodontal tissues. This leads to breakdown of both soft and hard periapical tissues. However, in a vital tooth, the inflammation of the periodontal ligament is usually caused by immunological mediators.
9.7.2.4 Prognosis
When AP persists after endodontic treatment, a more complex therapeutic situation arises than in untreated teeth with AP [72]. Hence, the prognosis of AP after surgical endodontic treatment is related to a number of factors, including age [odds ratio (OR), 2.5; confidence interval (CI), 1.01–6.00], preoperative root-filling length (OR, 3.4; CI, 1.34–8.76) and size of the surgical crypt (OR, 1.9; CI, 1.19–3.16) [19], as well as interproximal bone levels at the treated tooth (OR, 5.10; CI, 1.67–16.21), the type of root-end filling material used (OR, 7.65; CI, 2.60–25.27) [120] and the position of treated teeth (OR, 3.52; CI, 1.78–6.96) [103]. According to the results of these three prognostic studies, treatment outcome was superior in subjects older than 45 years, in anterior teeth, tooth with inadequate (versus adequate) root canal fillings, surgical crypt smaller or equal to 1 cm, bone level from the cementoenamel junction more than 3 mm and root-end fillings with ProRoot MTA.
9.7.2.5 Aim of Treatment
The main aims of endodontic surgery are the eradication of microbial factors and prevention of reinfection by establishing a hermetic apical seal with an ideal root-end filling material. Historically, root-end filling materials such as silver amalgam, Cavit, gold foil, polycarboxylate cement and zinc phosphate cement were suggested, as well as glass ionomer, composite resin, reinforced zinc oxide eugenol cements [intermediate restorative material (IRM), super ethoxy-benzoic acid (EBA)], calcium-enriched mixture (CEM) cement and mineral trioxide aggregate biomaterials.
9.7.2.6 Outcomes
The desired outcomes of an intervention are the absence of clinical signs/symptoms of inflammation/infection as well as radiographic resolution of a persistent AP in the long term. Clinical success rates are usually higher than success rates from radiographic evaluation because AP may be asymptomatic clinically; accordingly, the outcome should be mainly extrapolated from the radiographic evaluation.
The radiographic appearance of the periapical area will reflect the gradual stages of AP healing. A common scoring system for radiographic assessment of apical periodontitis, the periapical index (PAI), was introduced by Ørstavik in 1986 [82]. However, several recent studies have shown that cone-beam computed tomography (CBCT) is more sensitive in detecting AP compared to conventional radiography [35]. In other words, conventional radiography is more likely to miss AP; however, CBCT is not recommended as routine diagnostic tool due to its high cost and patient exposure.
9.7.2.7 Methods of Search and Appraisal
Studies dating back to 1966 were located by searching PubMed (Medline). The main search terms were systematic review(s) or randomised controlled trial(s) or clinical trial(s), mineral trioxide aggregate and surgery. We also searched The Dental ELF, UTHSCSA Dental School CAT Library, Journal of Evidence-Based Dental Practice as well as Evidence-Based Dentistry and ClinicalTrials.gov for the keywords ‘mineral trioxide aggregate’. Only English-language trials were assessed. Using modified van Tulder List and AMSTAR checklist, randomised controlled trials and systematic reviews of randomised controlled trials were scored, respectively.
9.7.2.8 Efficacy
Our search found four randomised controlled trials [31, 32, 60, 104] (Table 9.4) and one systematic review [111]. The only systematic review found in this field, collected and analysed quasi-controlled trials as well as randomised controlled trials; therefore, the review was classified as LoE2. Four randomised controlled trials provided evidence that MTA significantly increases the radiographic success rate in comparison to no root-end cavity preparation and filling control (gutta-percha smoothed); however, such outcomes are similar with IRM and Super EBA. There are no randomised controlled trials to compare MTA with many other root-end fillings such as amalgam and CEM cement as yet.
9.7.2.9 Drawbacks
Long setting time of MTA is a known drawback of the material for root-end filling [84].
9.7.2.10 Comments
A recent study reported that the 5-year prognosis of post-endodontic surgery to be 8 % poorer than the 1-year prognosis [120], showing that recall time can influence analysis of treatment outcomes. In addition, the similarity between the treatment outcomes in the intervention and control groups in three randomised controlled trials [31, 60, 104] reveals that ‘expected power of study’ was dissimilar to ‘observed power’ at the end of the trials. Furthermore, there are limitations in small clinical trials versus large multicentre trials that are often better representatives of a population [87]. Therefore, a greater body of evidence is required to reach definitive conclusions regarding MTA as a gold standard root-end filling material in routine clinical practice. There is still a need for prospective, multicentre, long-term and large-scale randomised controlled trials for making evidence-based decisions.
Clinical Bottom Line
To answer the PICO question, randomised controlled trials that have LoE1 and GoR-A demonstrate that in surgical endodontics:
-
1.
MTA as root-end filling has better radiographic success rates than heat smoothing of the orthograde gutta-percha (no root-end filling).
-
2.
MTA as root-end filling has similar radiographic success rates with IRM in single-rooted teeth.
-
3.
MTA as root-end filling has similar radiographic success rates with Super EBA after endodontic microsurgery.
9.7.3 Mineral Trioxide Aggregate for Vital Pulp Therapy of Primary Teeth
PICO Question
In case of pulp exposures in primary teeth, how does MTA pulp cover compare with other pulp covering agents in terms of treatment outcome?
9.7.3.1 Definition
Vital pulp therapy (VPT) techniques consist of six definite treatments. From the least to most invasive are non-invasive stepwise excavation [62], indirect pulp capping (IPC), direct pulp capping (DPC), miniature pulpotomy (MP) [9], partial or Cvek pulpotomy (PP) [33] and full/coronal pulpotomy (FP). Clinicians can employ these techniques in either primary or permanent teeth.
The surgical removal of the entire coronal pulp, i.e. full pulpotomy, is a common treatment modality to maintain functionality of primary molar teeth with carious/traumatic pulp exposures which would otherwise be extracted.
Treatment approaches for the pulpotomy of primary teeth consist of devitalisation, preservation or regeneration using various materials including formocresol, ferric sulphate, calcium hydroxide, calcium-enriched mixture (CEM) cement, Portland cement (PC) and MTA. Currently, formocresol pulpotomy is the most common treatment approach worldwide; however, in recent years, clinicians and researchers have voiced their concerns about the safety of formocresol use in paediatric dentistry (i.e. mutagenicity, carcinogenicity and immune sensitisation). It seems that modern pedodontics/endodontics has recently shifted the objective of pulpotomy from devitalisation to revitalisation/vitalisation: infected/inflamed coronal pulp is amputated, and the radicular pulp is covered with biomaterials to induce a favourable biological response. In other words, regeneration of dentinal bridges over uninflamed remaining pulp recreating an effective biological seal [64].
Direct pulp capping (DPC) is a less invasive treatment than pulpotomy; though, due to reported unwanted treatment outcomes of CH pulp capping (i.e. internal resorption, pulp calcification, etc.), this treatment modality is rarely employed in primary teeth. However, recent evidence demonstrates that this treatment option can be effective if good coronal seal is provided.
9.7.3.2 Incidence/Prevalence
The prevalence of dental caries in the primary dentition for children aged 2–5 years increased from 24 % in 1988–1994 to 28 % in 1999–2004, according to the most recent data released by the US Department of Health and Human Services (www.cdc.gov/nchs/data/series/sr_11/sr11_248.pdf). A recent Cochrane review stated that the overall mean incidence of pulp exposure after complete caries removal is 34.7 % for the management of dentinal caries in previously unrestored primary and permanent teeth [92].
9.7.3.3 Aetiology
Vital pulp therapies (VPT) of primary teeth are most often necessitated by progression of caries into/close to the pulp and are usually indicated due to removal of all caries/soft demineralised dentine by the dentist as well as traumatic injuries to the teeth.
9.7.3.4 Prognosis
It was reported that pulpotomy success rate for teeth restored with a stainless steel crown was higher than for those restored with amalgam [105].
9.7.3.5 Aim of Treatment (Intervention)
The objective of VPT in primary dentition is pulp dressing to relieve sensitivity/pain and also to prevent the supporting periodontal tissues from breaking down up to exfoliation time.
9.7.3.6 Outcomes
The main outcome measure for determining clinical success is the absence of spontaneous pain, abscess, sinus tract or pathologic mobility; radiographic success is determined according to the absence of furcation/periapical lesion, internal or pathologic external resorption and root canal obliteration as well as the presence of a normal periodontal ligament.
Note: Many researchers have reported cases of canal obliteration as success.
9.7.3.7 Methods of Search and Appraisal
Studies dating back to 1966 were located by searching PubMed (Medline). The main search terms were [systematic review(s) or randomized controlled trial(s) or clinical trial(s)] and [mineral trioxide aggregate] and [pulpotomy or vital pulp therapy or primary molar/teeth]. We also searched The Dental ELF, UTHSCSA Dental School CAT Library, Journal of Evidence-Based Dental Practice as well as Evidence-Based Dentistry and ClinicalTrials.gov for the key term ‘mineral trioxide aggregate’. Only English-language trials were assessed. Using modified van Tulder List and AMSTAR checklist, RCTs and systematic reviews of RCTs were scored respectively.
9.7.3.8 Efficacy
9.7.3.8.1 MTA Versus Formocresol Pulpotomy
The only Cochrane review assessing pulp therapy for extensive decay in primary teeth concluded that based on the randomised controlled trials available, there is ‘no reliable evidence’ supporting the superiority of one type of treatment/material over the other for pulpally involved primary molars and that ‘high quality randomized controlled trials, with appropriate unit of randomization and analysis are needed’ [70]. As this review was published in 2003 and several systematic reviews as well as randomised controlled trials have been published thereafter, more recent research should be analysed.
The result of our search reveals that three systematic reviews [74, 85, 102] as well as 19 randomised controlled trials [2, 3, 5, 8, 40, 43, 47, 49, 51, 52, 54, 69, 71, 75, 106, 107, 109, 110, 125] (Table 9.5) compared the success rates of MTA alone with formocresol pulpotomies. One of systematic reviews collected and analysed clinical trials as well as randomised controlled trials [74]; therefore, the review was classified as LoE2. Based on the date of publication and selection criteria, six randomised controlled trials were included in each of two remaining reviews. Four of these RCTs are the same, and totally eight randomised controlled trials were included in the two reviews (Table 9.6) [2, 3, 40, 47, 51, 54, 71, 75]. The results of the two systematic reviews are identical, and the meta-analysis [85] indicated that ‘clinical and radiographic finding show that MTA is superior to formocresol in primary molars pulpotomy resulting in a lower failure rate, with the relative risk being 0.32 (CI, 0.11–0.90) and 0.31 (CI, 0.13–0.74), respectively’; in addition, MTA has less undesirable sequelae.
Eleven randomised controlled trials [5, 8, 43, 49, 52, 69, 106, 107, 109, 110, 125] were published after the publication of these two systematic reviews (Table 9.5); therefore, to make comprehensive conclusions, we performed meta-analyses using the Mantel-Haenszel model and calculation of pooled relative risk (RR). We only included studies with 24-month follow-up. The results clearly showed that MTA is significantly superior to formocresol in primary molar pulpotomy in terms of treatment outcomes (Fig. 9.1).
9.7.3.8.2 MTA Versus Other Pulpotomy Agents
Eleven studies compared MTA with various pulpotomy agents other than formocresol (Table 9.7); five of these studies compared MTA with calcium hydroxide [61, 69, 80, 86, 106], four studies compared MTA to ferric sulphate [38, 43, 79, 106], two studies compared MTA with Portland cement [80, 96], one study compared MTA with calcium-enriched mixture (CEM) cement [63], and one study compared white with grey MTA [28].
The results of various randomised controlled trials comparing MTA with calcium hydroxide or ferric sulphate are mixed; some report significant and others insignificant differences between the pulpotomy agents. Due to the controversy, two separate meta-analyses with the Mantel-Haenszel model with calculation of pooled relative risk (RR) were performed. Our results clearly showed that MTA is superior to calcium hydroxide as well as ferric sulphate in primary molar pulpotomy at a 24-month follow-up (Figs. 9.2 and 9.3).
9.7.3.8.3 MTA Versus Other DPC Materials
Two randomised controlled trials compared MTA with calcium hydroxide and calcium-enriched mixture (CEM) cement for DPC of primary molars [45, 46, 117] (Table 9.8); there were no significant differences found for all the treatment outcomes assessed.
9.7.3.9 Drawbacks
It was reported that crown discolouration is common after ProRoot MTA pulpotomy in primary teeth [61, 71]. High price and long setting time are two other main drawbacks of MTA [84].
9.7.3.10 Comments
It appears that there are adequate randomised controlled trials and systematic reviews comparing MTA pulpotomy of primary teeth to formocresol, ferric sulphate and calcium hydroxide. The results are clear; however, we need to take into account the effects of MTA pulpotomy on the oral health-related quality of life as well as health technology assessments.
Note: MTA originated from Portland cement; however, according to FDA and CE regulations, materials that are manufactured outside of the dental industries, i.e. Portland cement, should not be used in the dental clinics [90].
Clinical Bottom Line
To answer the PICO question, systematic reviews as well as recent LoE1 randomised controlled trials with GoR-A showed that in vital pulp therapy of primary teeth:
-
1.
MTA as pulpotomy agent has superior success rates when compared to formocresol, calcium hydroxide and ferric sulphate in primary molar pulpotomies.
-
2.
MTA as pulpotomy agent has similar success rates when compared to calcium-enriched mixture cement in primary molar pulpotomies.
-
3.
Grey and white MTAs have similar treatment effects in primary molar pulpotomies.
-
4.
MTA as pulp capping agent has similar success rates when compared to calcium hydroxide in primary molar direct pulp capping.
-
5.
MTA as pulp capping agent has similar success rates when compared to calcium-enriched mixture cement in primary molar direct pulp capping.
9.7.4 Mineral Trioxide Aggregate for Management of Immature Permanent Teeth
PICO Question
In endodontic management of immature permanent teeth, how does MTA compare with other materials in terms of treatment outcomes?
9.7.4.1 Definition
When endodontic treatment is indicated for an immature open apex tooth, apexogenesis is the best treatment option. Continued root development, dentin formation and apex closure usually lead to longer and stronger roots and consequently higher survival rate for the treated vital tooth. If the immature tooth is nonvital, clinicians may choose calcium hydroxide apexification, apical plug apexification using biomaterials or revitalisation (revascularisation) technique. In the first traditional procedure, necrotic tissue is removed, and calcium hydroxide is applied in several visits to induce apical closure by stimulating the formation of a calcified barrier; the extended treatment time increases brittleness of root dentin and risk of fracture.
MTA apical plug can be also used to create an artificial apical barrier in usually one or maximum two steps; this alternative treatment reduces the treatment time as well as the required visits to the dental office. The newly introduced treatment modality, i.e. revascularisation, applies a triple antibiotic which medicates the root canal(s), providing an intra-canal clot scaffold into which blastic cells can grow. The coronal access is then sealed with a bioactive material. This procedure typically leads to formation of a vascularised tissue and subnormal development of the entire root in anterior as well as posterior teeth [18, 77].
9.7.4.2 Incidence/Prevalence
There is no comprehensive study to report the incidence/prevalence of pulp exposure of vital/nonvital immature open apex teeth after caries removal and trauma; despite the common nature of this condition in children and adolescents. It must be noted that untreated nonvital immature teeth are sometimes found in adults.
9.7.4.3 Aetiology
Pulp therapy of vital permanent immature teeth (apexogenesis) is usually indicated after iatrogenic or carious pulp exposure as well as accidental traumatic injuries to the teeth. In the case of no/inadequate treatment for such teeth, the dental pulp becomes nonvital, and apexification, apical plug or revascularisation techniques may be indicated.
9.7.4.4 Prognosis
Loss of vitality before complete root development leaves a short, thin and weak root which is more prone to fracture and has poorer crown/root ratio. It was reported that 32 % of teeth with apexification ended up with root fracture mainly subsequent to another minor trauma episode [6].
9.7.4.5 Aim of Treatment (Intervention)
As a general rule, the clinicians must always try to avoid apexification if apexogenesis is possible. In vital immature teeth with open apices, every attempt must be made to maintain pulp vitality until root development is complete. Simulation of apexogenesis via revascularisation is also the desired treatment. If apexogenesis cannot be achieved, then artificial apical closure and apexification must be utilised.
9.7.4.6 Outcomes
Root development and apical closure are two main treatment outcomes. Also, the absence of clinical/radiographic signs and/or symptoms of inflammation or infection is interpreted as success.
9.7.4.7 Methods of Search and Appraisal
Studies dating back to 1966 were located by searching PubMed (Medline). The main search terms were [systematic review(s) or randomized controlled trial(s) or clinical trial(s)] and [mineral trioxide aggregate] and [pulp cap or pulpotomy or vital pulp therapy or apexogenesis or apexification or apical plug or artificial apical closure or revascularization or revitalization]. We also searched The Dental ELF, UTHSCSA Dental School CAT Library, Journal of Evidence-Based Dental Practice as well as Evidence-Based Dentistry and ClinicalTrials.gov for the keywords ‘mineral trioxide aggregate’. Only English-language trials were assessed. Using modified van Tulder List and AMSTAR checklist, randomised controlled trials and systematic reviews of randomised controlled trials were scored, respectively.
9.7.4.8 Efficacy
9.7.4.8.1 MTA Apexogenesis
The result of our search revealed that three randomised controlled trials compared the success rates of MTA apexogenesis with calcium hydroxide [41], zinc oxide eugenol [48] and calcium-enriched mixture cement [78] (Table 9.9). In comparison with calcium hydroxide, zinc oxide eugenol or CEM cement, MTA showed nonsignificant clinical and radiographic success to induce apical closure in vital immature permanent teeth.
9.7.4.8.2 MTA Apical Plug Versus Calcium Hydroxide Apexification
Two randomised clinical trials compared MTA with calcium hydroxide for apexification of necrotic immature permanent teeth between 1993 and 2011 [42, 88]; one was a systematic review, and the other was a meta-analysis [29]. They analysed the randomised controlled trials using Jadad scale; results of the meta-analysis showed comparable radiographic success and apical barrier formation with both calcium hydroxide and mineral trioxide aggregate in immature teeth.
Two randomised controlled trials were also published after the publication of the systematic review with similar results and without significant differences (Table 9.10); one study compared two commercial types of MTA (ProRoot vs. Angelus) [68], and the second compared MTA with calcium hydroxide [34]. In addition, there is a registered clinical trial which is completed [25]; however, the results have not been reported yet.
9.7.4.8.3 MTA for Regenerative Endodontic Procedures
There is a lack of randomised controlled trials for MTA.
9.7.4.9 Drawbacks
The use of MTA promotes a mild grey discolouration in the crown after apexification [55]; it was reported that coronal discolouration was observed in 22.7 % of teeth following white MTA placement in immature open apex teeth [68]. Severe discolouration after grey MTA pulpotomy in immature permanent teeth was also reported [108]. It was also reported that the roots of two maxillary central incisors were not developed after regenerative endodontic treatment using MTA [76]. High price and long setting time are two other main drawbacks of MTA [84].
9.7.4.10 Comments
A paradigm shift in endodontology in the last decade has altered the traditional treatment concepts towards more biologically based regenerative research and practice. Regeneration of necrotic immature permanent teeth could be an invaluable technique to save countless numbers of anterior teeth each year; however, there are no standardised treatment protocols based on high-level evidence. There is a pressing need for prospective high-quality RCTs to develop and recommend appropriate treatment regimen for continued hard tissue formation of immature teeth.
In addition, full pulpotomy which is the most invasive form of VPT in apexogenesis treatment of vital immature permanent teeth is supported with limited number of randomised controlled trial evidence; however, there is a gap of data for other less aggressive VPT techniques.
Clinical Bottom Line
To answer the PICO question for permanent immature teeth, GoR-A recommendations were formulated (based on one systematic review and recent randomised controlled trials with LoE1 evidence) as outlined below:
-
1.
MTA vital pulp dressing placed for apexogenesis treatment has similar success rates when compared to calcium hydroxide, zinc oxide eugenol and calcium-enriched mixture cement.
-
2.
MTA when used as apical plug for apexification has similar success rates when compared to calcium hydroxide but reduces treatment time.
-
3.
ProRoot and Angelus MTA apical plugs have similar effects in apexification treatment.
9.7.5 Mineral Trioxide Aggregate for Vital Pulp Therapy of Mature Permanent Teeth
PICO Question
In vital pulp therapy of mature permanent teeth, how does MTA compare with other pulp protecting materials in terms of treatment outcomes?
9.7.5.1 Definition
Theoretically, dressing and protecting an exposed vital pulp in mature permanent teeth from bacterial invasion with an ideal pulp capping material would maintain pulp vitality. The general evidence-based consensus is that iatrogenic and symptom-free pulp exposures can be successfully treated by VPT [4]. For this reason, an ideal pulp capping material should be biocompatible, antimicrobial, non-toxic and specifically able to seal the path of communication between exposed dental pulp and oral microbial flora. Calcium hydroxide used to be the universal capping material in the past; however, new materials, i.e. MTA and CEM, have replaced it with a very positive trend in recent years.
The traditional school of thought recommended high-price root canal therapy for carious pulp exposures in mature permanent teeth specifically with signs of irreversible pulpitis and apical periodontitis; however recently, several clinical studies have reported that vital teeth can be treated successfully with low-price VPT [4, 16, 26, 39]. One- and two-year results of an ongoing multicentre randomised clinical trial have revealed that in comparison with root canal therapy, VPT/CEM is a cost-effective and reliable bio-method for management of permanent molars with irreversible pulpitis with/without apical periodontitis [14, 15]. Moreover, it also has an outstanding pain-reducing effect in irreversible pulpitis [10] and can be recommended for general clinical practice. This treatment modality will doubtlessly improve quality of dental care for mature vital permanent teeth.
9.7.5.2 Incidence/Prevalence
Dental caries has remained the most prevalent chronic disease of humans; the main chief complaint of patients with deep dental caries/irreversible pulpitis, seeking for dental care, is pain [7].
A recent Cochrane review stated that mean incidence of pulp exposure is 34.7 % after complete caries removal for the management of dentinal caries in previously unrestored primary and permanent teeth [92].
On the other hand, apical periodontitis is an important radiographic sign for untreated decayed teeth as well as failed root canal treated teeth. Current evidence demonstrates that an inflamed vital pulp can lead to AP and a recent study showed that CBCT can detect AP better than conventional radiography specifically in teeth with irreversible pulpitis [1]. A systematic review of epidemiological studies on more than 300,000 teeth from 33 studies mostly performed in developed countries verified that the prevalence of AP is very high, broadly equivalent to 1 radiolucency per patient [83].
9.7.5.3 Aetiology
The cause and effect relationship between the presence of microorganisms and pulpal inflammation and necrosis is well documented [56, 99]. In germ-free animal models, the pulp-periapical complex remained vital and without any inflammation/necrosis after pulp exposure. Therefore, microorganisms and their toxins play the most important role in the aetiology of pulp and periapical pathosis (e.g. pulpitis and AP) [99].
Note: There is no scientific basis on which to assess the value of markers of inflammation intended to differentiate between reversible and irreversible pulpitis [65], making clinical diagnosis of pulpal status perplexing. As a general consensus in endodontology, there is poor correlation between clinical signs/symptoms of pulpal diseases with histological features, i.e. inflammation [98]; therefore, these complicated clinico-histological terminologies need reconsideration. Added to this ambiguity is the finding that several clinical studies have proved that clinically diagnosed irreversible pulpitis can be associated with radiographically apical periodontitis [26, 116]. Immuno-histological evidence revealed that not only an infected necrotic pulp but also an inflamed vital pulp has the potential to extend the inflammation to periapical tissues at an early stage and create apical periodontitis [122]. Whilst two-dimensional periapical radiographs have limited ability to detect such lesions [24], three-dimensional cone-beam computed tomography can distinguish AP in 13.7 % of examined human teeth with established irreversible pulpitis [1].
9.7.5.4 Prognosis
Current best evidence provides inconclusive information regarding factors influencing treatment outcome of vital pulp therapy in permanent teeth [4]. A preliminary retrospective study stated that there is a statistically significant association between the clinical status of pulpotomy and quality of restoration [36]; however, a recent prognostic study reported that the type of pulp capping material (i.e. MTA) was the single most important factor influencing the tooth survival rate [30].
Surprisingly, there is also a deficit of high-level evidence for the effect of treatment factors on primary root canal treatment outcome for management of various pulpal diagnoses [93]. Besides, a high-quality cohort study revealed that the survival rate of endodontically treated teeth in comparison to their vital counterparts is alarmingly low, with molars having the worst survival rates (hazard ratio = 7.4; CI 95 %: 3.2–15.1) [27].
9.7.5.5 Aim of Treatment
Vital pulp therapy for permanent mature teeth is typically indicated after iatrogenic or carious pulp exposure as well as accidental traumatic injuries to the teeth. When no/inadequate treatment is carried out for such teeth, the dental pulp becomes nonvital, and traditionally, pulpectomy and primary root canal therapy may be indicated. Consequently, the main treatment objective of VPT is to maintain pulp vitality of a carious permanent mature tooth by protecting the remaining pulp using a pulp capping agent so that the tooth becomes symptom-free and functional.
In case of ordinary root canal therapy, the three-dimensional seal of the root canal system after appropriate root canal cleaning and shaping is the main aim.
9.7.5.6 Outcomes
The clinical outcome is based on the absence of subjective symptoms (i.e. pain) and objective observation of inflammation and/or infection, i.e. abscess, swelling, sinus tract and tenderness upon palpation/percussion. The most important radiographic outcome is when AP is prevented or when healing of existing AP.
9.7.5.7 Methods of Search and Appraisal
Studies dating back to 1966 were located by searching PubMed (Medline). The main search terms were [systematic review(s) or randomized controlled trial(s) or clinical trial(s)] and [mineral trioxide aggregate] and [pulp* or pulp cap or pulpotomy or vital pulp therapy]. We also searched The Dental ELF, UTHSCSA Dental School CAT Library, Journal of Evidence-Based Dental Practice as well as Evidence-Based Dentistry and ClinicalTrials.gov for the keywords ‘mineral trioxide aggregate’. Only English-language trials were assessed. Using modified van Tulder List and AMSTAR checklist, randomised controlled trials and systematic reviews of randomised controlled trials were scored, respectively.
9.7.5.8 Efficacy
Whilst there were ten randomised controlled trial [11, 44, 53, 59, 73, 91, 97, 100, 123, 124], we found only one systematic review [4]. The review analysed nonrandomised clinical trials and therefore was not classified as LoE1. Seven histological/immunohistochemical studies (Table 9.11 [44, 53, 73, 97, 100, 123, 124]) were found that compared MTA pulp capping with calcium hydroxide (n = 4), calcium-enriched mixture (n = 2) and different powder/liquid ratio of itself (n = 1) on caries-free vital teeth; only one study looked at incipient caries [53]. There are three randomised controlled trials carried out for management of teeth with deep caries or established irreversible pulpitis (Table 9.12). One study compared MTA with calcium hydroxide for partial pulpotomy of permanent molars with deep caries [91], another study compared MTA with calcium hydroxide as indirect pulp capping [59], and finally a multicentre randomised controlled trial compared the post-operative pain relief as well as clinical and radiographic outcomes of pulpotomy in human permanent molars with irreversible pulpitis using calcium-enriched mixture cement or MTA [11]. There were no statistical significances between MTA and CEM or MTA and calcium hydroxide reported in these randomised controlled trials.
Note: Histological studies evaluating pulp response to vital pulp therapy have been mainly carried out on caries-free or incipient caries vital teeth which were candidates for extraction shortly after. This shows that the studies were undertaken in different population, i.e. normal intact teeth versus carious teeth with pulp exposure or pulpitis. According to evidence-based practice concepts, the results of these kinds of studies should be excluded because they address a different population than the one required. In addition, histological evaluation is classified as a surrogate outcome. The surrogate outcome usually allows prediction of treatment effect on the more clinically relevant outcome but does not directly measure the main clinical benefit. The surrogate outcome is considered valid for an intervention if it is statistically associated with the true clinical outcome [89]. However, the presence/absence, type and intensity of histological pulp inflammation as surrogate variables do not inevitably represent the true short- and long-term treatment outcome, i.e. pain and tooth survival. Furthermore, only a minimal association between clinical and histological findings could be established for MTA or calcium hydroxide direct pulp capping [53].
9.7.5.9 Drawbacks
Tooth discolouration caused by white MTA used for the management of a complicated crown fracture via partial pulpotomy has been reported [22]. High price and long setting time are two other main drawbacks of MTA [84].
9.7.5.10 Comments
In current dental practice, VPT has become an accepted treatment for reversible pulpitis, with predictable outcomes [23]. When irreversible pulpitis is clinically diagnosed, the common school of thought recommends removal of entire vital pulp, despite containing competent stem cells with proliferative potential [121]. In the light of recent evidences and in order to gain a better understanding of pulp healing capability, the inflammatory process and pathogenesis of the dental pulp need to be reconsidered, particularly in cases of irreversible pulpitis [14]; such a modern approach can lead to preservation of the dental pulp in mature permanent teeth and, thus by healing of the diseased pulp, can have a positive impact on improving the tooth survival rate as well as patients’ quality of life.
Current dental educational system defends the correlation between spontaneous pain or lingering pain in response to cold stimuli and the existence of irreversible pulpitis that necessitates the complex/expensive process of root canal therapy. However, several talented dental students have asked a long overdue and fundamental question: Currently pulp preservation and regeneration in endodontic procedures is being increasingly emphasised in the educational curriculum, clinicians even aim to revitalise the immature necrotic pulp; then why do endodontists intentionally extirpate inflamed vital pulps with clinical diagnosis of irreversible pulpitis? Root canal therapy of vital teeth is currently based on a poor correlation between clinical signs/symptoms and histological feature of the pulp [97]. Amazingly, there are LoE1 randomised controlled trials that show the vital pulp of mature molars with irreversible pulpitis that were successfully treated with simple low-cost pulpotomy treatment using appropriate biomaterials. These trials demonstrated that full pulpotomy with MTA or CEM biomaterials, as the most invasive form of VPT, established favourable short- to long-term outcomes [10, 11, 14, 15]. It seems that endodontology needs to reconsider the nomenclature of dental pulp diseases and consequently create a paradigm shift in endodontic treatment approaches.
Currently, the proportion of the population who is unable to afford dental services due to its high cost is increasing, even in developed affluent countries [13]. To solve this problem, governments should accept responsibility to increase the overall spending for dental disease prevention protocols as well as evidence-based low-cost dental services. Researchers, on the other hand, should provide evidence employing recent progresses in endodontology and constantly suggest more biologic, cost-effective and successful simple treatment alternatives.
In the future, conducting the studies that consider the effects of VPTs on the oral health-related quality of life as well as health technology assessment and evidence-based practice guidelines is recommended. Last but not least, is the need for outcome assessment of less or non-invasive forms of VPT.
Clinical Bottom Line
To answer the PICO question, randomised controlled trials with LoE1 have led to GoR-A (grade A recommendations) in vital pulp therapy of mature permanent teeth that state:
-
1.
MTA partial pulpotomy has similar success rates when compared to calcium hydroxide for management of symptom-free carious pulp exposure in first molars.
-
2.
MTA indirect pulp capping has similar success rates when compared to calcium hydroxide in teeth with active deep carious lesion/reversible pulpitis after 6 months.
-
3.
MTA full pulpotomy has similar pain relief effect as well as clinical/radiographic success rates when compared to calcium-enriched mixture (CEM) cement in molar teeth with irreversible pulpitis.
References
Abella F, Patel S, Duran-Sindreu F, Mercade M, Bueno R, Roig M. Evaluating the periapical status of teeth with irreversible pulpitis by using cone-beam computed tomography scanning and periapical radiographs. J Endod. 2012;38(12):1588–91.
Aeinehchi M, Dadvand S, Fayazi S, Bayat-Movahed S. Randomized controlled trial of mineral trioxide aggregate and formocresol for pulpotomy in primary molar teeth. Int Endod J. 2007;40(4):261–7.
Agamy HA, Bakry NS, Mounir MM, Avery DR. Comparison of mineral trioxide aggregate and formocresol as pulp-capping agents in pulpotomized primary teeth. Pediatr Dent. 2004;26(4):302–9.
Aguilar P, Linsuwanont P. Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. J Endod. 2011;37(5):581–7.
Airen P, Shigli A, Airen B. Comparative evaluation of Formocresol and mineral trioxide aggregate in pulpotomized primary molars – 2 year follow up. J Clin Pediatr Dent. 2012;37(2):143–7.
Al-Jundi SH. Type of treatment, prognosis, and estimation of time spent to manage dental trauma in late presentation cases at a dental teaching hospital: a longitudinal and retrospective study. Dent Traumatol. 2004;20(1):1–5.
Anderson R, Thomas DW. ‘Toothache stories’: a qualitative investigation of why and how people seek emergency dental care. Community Dent Health. 2003;20(2):106–11.
Ansari G, Ranjpour M. Mineral trioxide aggregate and formocresol pulpotomy of primary teeth: a 2-year follow-up. Int Endod J. 2010;43(5):413–18.
Asgary S, Ahmadyar M. Can miniature pulpotomy procedure improve treatment outcomes of direct pulp capping? Med Hypotheses. 2012;78(2):283–5.
Asgary S, Eghbal MJ. The effect of pulpotomy using a calcium-enriched mixture cement versus one-visit root canal therapy on postoperative pain relief in irreversible pulpitis: a randomized clinical trial. Odontology. 2010;98(2):126–33.
Asgary S, Eghbal MJ. Treatment outcomes of pulpotomy in permanent molars with irreversible pulpitis using biomaterials: a multi-center randomized controlled trial. Acta Odontol Scand. 2013;71(1):130–6.
Asgary S, Eghbal MJ, Ehsani S. Periradicular regeneration after endodontic surgery with calcium-enriched mixture cement in dogs. J Endod. 2010;36(5):837–41.
Asgary S, Eghbal MJ, Fazlyab M, Baghban AA, Ghoddusi J. Five-year results of vital pulp therapy in permanent molars with irreversible pulpitis: a non-inferiority multicenter randomized clinical trial. Clin Oral Investig. 2014 Apr 27. [Epub ahead of print].
Asgary S, Eghbal MJ, Ghoddusi J. Two-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter randomized clinical trial. Clin Oral Investig. 2014;18(2):635–41.
Asgary S, Eghbal MJ, Ghoddusi J, Yazdani S. One-year results of vital pulp therapy in permanent molars with irreversible pulpitis: an ongoing multicenter, randomized, non-inferiority clinical trial. Clin Oral Investig. 2013;17(2):431–9.
Asgary S, Ehsani S. Permanent molar pulpotomy with a new endodontic cement: a case series. J Conserv Dent. 2009;12(1):31–6.
Asgary S, Motazedian HR, Parirokh M, Eghbal MJ, Kheirieh S. Twenty years of research on mineral trioxide aggregate: a scientometric report. Iran Endod J. 2013;8(1):1–5.
Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004;30(4):196–200.
Barone C, Dao TT, Basrani BB, Wang N, Friedman S. Treatment outcome in endodontics: the Toronto study – phases 3, 4, and 5: apical surgery. J Endod. 2010;36(1):28–35.
Bayne SC. Dental restorations for oral rehabilitation – testing of laboratory properties versus clinical performance for clinical decision making. J Oral Rehabil. 2007;34(12):921–32.
Bayne SC. Correlation of clinical performance with ‘in vitro tests’ of restorative dental materials that use polymer-based matrices. Dent Mater. 2012;28(1):52–71.
Belobrov I, Parashos P. Treatment of tooth discoloration after the use of white mineral trioxide aggregate. J Endod. 2011;37(7):1017–20.
Bender IB. Reversible and irreversible painful pulpitides: diagnosis and treatment. Aust Endod J. 2000;26(1):10–4.
Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: I. 1961. J Endod. 2003;29(11):702–6.
Beslot-Neveu A, Bonte E, Baune B, Serreau R, Aissat F, Quinquis L, et al. Mineral trioxide aggregate versus calcium hydroxide in apexification of non vital immature teeth: study protocol for a randomized controlled trial. Trials. 2011;12:174.
Caliskan MK. Pulpotomy of carious vital teeth with periapical involvement. Int Endod J. 1995;28(3):172–6.
Caplan DJ, Cai J, Yin G, White BA. Root canal filled versus non-root canal filled teeth: a retrospective comparison of survival times. J Public Health Dent. 2005;65(2):90–6.
Cardoso-Silva C, Barberia E, Maroto M, Garcia-Godoy F. Clinical study of Mineral Trioxide Aggregate in primary molars. Comparison between Grey and White MTA – a long term follow-up (84 months). J Dent. 2011;39(2):187–93.
Chala S, Abouqal R, Rida S. Apexification of immature teeth with calcium hydroxide or mineral trioxide aggregate: systematic review and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):e36–42.
Cho SY, Seo DG, Lee SJ, Lee J, Jung IY. Prognostic factors for clinical outcomes according to time after direct pulp capping. J Endod. 2013;39(3):327–31.
Chong BS, Pitt Ford TR, Hudson MB. A prospective clinical study of Mineral Trioxide Aggregate and IRM when used as root-end filling materials in endodontic surgery. Int Endod J. 2003;36(8):520–6.
Christiansen R, Kirkevang LL, Horsted-Bindslev P, Wenzel A. Randomized clinical trial of root-end resection followed by root-end filling with mineral trioxide aggregate or smoothing of the orthograde gutta-percha root filling – 1-year follow-up. Int Endod J. 2009;42(2):105–14.
Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod. 1978;4(8):232–7.
Damle SG, Bhattal H, Loomba A. Apexification of anterior teeth: a comparative evaluation of mineral trioxide aggregate and calcium hydroxide paste. J Clin Pediatr Dent. 2012;36(3):263–8.
de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod. 2009;35(7):1009–12.
Demarco FF, Rosa MS, Tarquinio SB, Piva E. Influence of the restoration quality on the success of pulpotomy treatment: a preliminary retrospective study. J Appl Oral Sci. 2005;13(1):72–7.
Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc. 2011;122:48–58.
Doyle TL, Casas MJ, Kenny DJ, Judd PL. Mineral trioxide aggregate produces superior outcomes in vital primary molar pulpotomy. Pediatr Dent. 2010;32(1):41–7.
Eghbal MJ, Asgary S, Baglue RA, Parirokh M, Ghoddusi J. MTA pulpotomy of human permanent molars with irreversible pulpitis. Aust Endod J. 2009;35(1):4–8.
Eidelman E, Holan G, Fuks AB. Mineral trioxide aggregate vs. formocresol in pulpotomized primary molars: a preliminary report. Pediatr Dent. 2001;23(1):15–8.
El-Meligy OA, Avery DR. Comparison of mineral trioxide aggregate and calcium hydroxide as pulpotomy agents in young permanent teeth (apexogenesis). Pediatr Dent. 2006;28(5):399–404.
El-Meligy OA, Avery DR. Comparison of apexification with mineral trioxide aggregate and calcium hydroxide. Pediatr Dent. 2006;28(3):248–53.
Erdem AP, Guven Y, Balli B, Ilhan B, Sepet E, Ulukapi I, et al. Success rates of mineral trioxide aggregate, ferric sulfate, and formocresol pulpotomies: a 24-month study. Pediatr Dent. 2011;33(2):165–70.
Eskandarizadeh A, Shahpasandzadeh MH, Shahpasandzadeh M, Torabi M, Parirokh M. A comparative study on dental pulp response to calcium hydroxide, white and grey mineral trioxide aggregate as pulp capping agents. J Conserv Dent. 2011;14(4):351–5.
Fallahinejad Ghajari M, Asgharian Jeddi T, Iri S, Asgary S. Direct pulp-capping with calcium enriched mixture in primary molar teeth: a randomized clinical trial. Iran Endod J. 2010;5(1):27–30.
Fallahinejad Ghajari M, Asgharian Jeddi T, Iri S, Asgary S. Treatment outcomes of primary molars direct pulp capping after 20 months: a randomized controlled trial. Iran Endod J. 2013;8(4):149–52.
Farsi N, Alamoudi N, Balto K, Mushayt A. Success of mineral trioxide aggregate in pulpotomized primary molars. J Clin Pediatr Dent. 2005;29(4):307–11.
Ghoddusi J, Shahrami F, Alizadeh M, Kianoush K, Forghani M. Clinical and radiographic evaluation of vital pulp therapy in open apex teeth with MTA and ZOE. N Y State Dent J. 2012;78(3):34–8.
Godhi B, Sood PB, Sharma A. Effects of mineral trioxide aggregate and formocresol on vital pulp after pulpotomy of primary molars: an in vivo study. Contemp Clin Dent. 2011;2(4):296–301.
Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9 Suppl 1:77–106.
Holan G, Eidelman E, Fuks AB. Long-term evaluation of pulpotomy in primary molars using mineral trioxide aggregate or formocresol. Pediatr Dent. 2005;27(2):129–36.
Hugar SM, Deshpande SD. Comparative investigation of clinical/radiographical signs of mineral trioxide aggregate and formocresol on pulpotomized primary molars. Contemp Clin Dent. 2010;1(3):146–51.
Iwamoto CE, Adachi E, Pameijer CH, Barnes D, Romberg EE, Jefferies S. Clinical and histological evaluation of white ProRoot MTA in direct pulp capping. Am J Dent. 2006;19(2):85–90.
Jabbarifar SEKA, Ghasemi D. Success rate of formocresol pulpotomy versus mineral trioxide aggregate in human primary molar tooth. J Res Med Sci. 2004;6:55–8.
Jacobovitz M, de Pontes Lima RK. The use of calcium hydroxide and mineral trioxide aggregate on apexification of a replanted tooth: a case report. Dent Traumatol. 2009;25(3):e32–6.
Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germfree and conventional laboratory rats. J South Calif Dent Assoc. 1966;34(9):449–51.
Kazem M, Eghbal MJ, Asgary S. Comparison of bacterial and dye microleakage of different root-end filling materials. Iran Endod J. 2010;5(1):17.
Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod. 1993;19(11):541–4.
Leye Benoist F, Gaye Ndiaye F, Kane AW, Benoist HM, Farge P. Evaluation of mineral trioxide aggregate (MTA) versus calcium hydroxide cement (Dycal(®)) in the formation of a dentine bridge: a randomised controlled trial. Int Dent J. 2012;62(1):33–9.
Lindeboom JA, Frenken JW, Kroon FH, van den Akker HP. A comparative prospective randomized clinical study of MTA and IRM as root-end filling materials in single-rooted teeth in endodontic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(4):495–500.
Liu H, Zhou Q, Qin M. Mineral trioxide aggregate versus calcium hydroxide for pulpotomy in primary molars. Chin J Dent Res. 2011;14(2):121–5.
Magnusson BO, Sundell SO. Stepwise excavation of deep carious lesions in primary molars. J Int Assoc Dent Child. 1977;8(2):36–40.
Malekafzali B, Shekarchi F, Asgary S. Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials. A 2-year randomised clinical trial. Eur J Paediatr Dent. 2011;12(3):189–93.
Mehrdad L, Malekafzali B, Shekarchi F, Safi Y, Asgary S. Histological and CBCT evaluation of a pulpotomised primary molar using calcium enriched mixture cement. Eur Arch Paediatr Dent. 2013;14(3):191–4.
Methods of diagnosis and treatment in endodontics: a systematic review. Swedish Council on Health Technology Assessment. 2012. p. 55.
Miyashita H, Worthington HV, Qualtrough A, Plasschaert A. Pulp management for caries in adults: maintaining pulp vitality. Cochrane Database Syst Rev. 2007;(2):CD004484.
Montori VM, Wilczynski NL, Morgan D, Haynes RB. Optimal search strategies for retrieving systematic reviews from Medline: analytical survey. BMJ. 2005;330(7482):68.
Moore A, Howley MF, O’Connell AC. Treatment of open apex teeth using two types of white mineral trioxide aggregate after initial dressing with calcium hydroxide in children. Dent Traumatol. 2011;27(3):166–73.
Moretti AB, Sakai VT, Oliveira TM, Fornetti AP, Santos CF, Machado MA, et al. The effectiveness of mineral trioxide aggregate, calcium hydroxide and formocresol for pulpotomies in primary teeth. Int Endod J. 2008;41(7):547–55.
Nadin G, Goel BR, Yeung CA, Glenny AM. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst Rev. 2003;(1):CD003220.
Naik S, Hegde AH. Mineral trioxide aggregate as a pulpotomy agent in primary molars: an in vivo study. J Indian Soc Pedod Prev Dent. 2005;23(1):13–6.
Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J. 2006;39(4):249–81.
Nair PN, Duncan HF, Pitt Ford TR, Luder HU. Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: a randomized controlled trial. Int Endod J. 2008;41(2):128–50.
Ng FK, Messer LB. Mineral trioxide aggregate as a pulpotomy medicament: an evidence-based assessment. Eur Arch Paediatr Dent. 2008;9(2):58–73.
Noorollahian H. Comparison of mineral trioxide aggregate and formocresol as pulp medicaments for pulpotomies in primary molars. Br Dent J. 2008;204(11):E20.
Nosrat A, Homayounfar N, Oloomi K. Drawbacks and unfavorable outcomes of regenerative endodontic treatments of necrotic immature teeth: a literature review and report of a case. J Endod. 2012;38(10):1428–34.
Nosrat A, Seifi A, Asgary S. Regenerative endodontic treatment (revascularization) for necrotic immature permanent molars: a review and report of two cases with a new biomaterial. J Endod. 2011;37(4):562–7.
Nosrat A, Seifi A, Asgary S. Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: a randomized clinical trial. Int J Paediatr Dent. 2013;23(1):56–63.
Odabas ME, Alacam A, Sillelioglu H, Deveci C. Clinical and radiographic success rates of mineral trioxide aggregate and ferric sulphate pulpotomies performed by dental students. Eur J Paediatr Dent. 2012;13(2):118–22.
Oliveira TM, Moretti AB, Sakai VT, Lourenco Neto N, Santos CF, Machado MA, et al. Clinical, radiographic and histologic analysis of the effects of pulp capping materials used in pulpotomies of human primary teeth. Eur Arch Paediatr Dent. 2013;14(2):65–71.
Olivo SA, Macedo LG, Gadotti IC, Fuentes J, Stanton T, Magee DJ. Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther. 2008;88(2):156–75.
Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2(1):20–34.
Pak JG, Fayazi S, White SN. Prevalence of periapical radiolucency and root canal treatment: a systematic review of cross-sectional studies. J Endod. 2012;38(9):1170–6.
Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review – Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36(3):400–13.
Peng L, Ye L, Tan H, Zhou X. Evaluation of the formocresol versus mineral trioxide aggregate primary molar pulpotomy: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(6):e40–4.
Percinoto C, de Castro AM, Pinto LM. Clinical and radiographic evaluation of pulpotomies employing calcium hydroxide and trioxide mineral aggregate. Gen Dent. 2006;54(4):258–61.
Pihlstrom BL, Barnett ML. Design, operation, and interpretation of clinical trials. J Dent Res. 2010;89(8):759–72.
Pradhan DP, Chawla HS, Gauba K, Goyal A. Comparative evaluation of endodontic management of teeth with unformed apices with mineral trioxide aggregate and calcium hydroxide. J Dent Child (Chic). 2006;73(2):79–85.
Prentice RL. Surrogate endpoints in clinical trials: definition and operational criteria. Stat Med. 1989;8(4):431–40.
Primus CM. Comments on “arsenic release provided by MTA and Portland cement” by Duarte MA, et al. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(4):416–17; author reply 417–8.
Qudeimat MA, Barrieshi-Nusair KM, Owais AI. Calcium hydroxide vs mineral trioxide aggregates for partial pulpotomy of permanent molars with deep caries. Eur Arch Paediatr Dent. 2007;8(2):99–104.
Ricketts D, Lamont T, Innes NP, Kidd E, Clarkson JE. Operative caries management in adults and children. Cochrane Database Syst Rev. 2013;(3):CD003808.
Rosenberg PA, Schindler WG, Krell KV, Hicks ML, Davis SB. Identify the endodontic treatment modalities. J Endod. 2009;35(12):1675–94.
Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71–2.
Sackett D, Straus S, Richardson W, Rosenberg W, Haynes R. Evidence-based medicine: how to practice and teach EBM. Edinburgh: Churchill Livingstone; 2000.
Sakai VT, Moretti AB, Oliveira TM, Fornetti AP, Santos CF, Machado MA, et al. Pulpotomy of human primary molars with MTA and Portland cement: a randomised controlled trial. Br Dent J. 2009;207(3):E5; discussion 128–9.
Sawicki L, Pameijer CH, Emerich K, Adamowicz-Klepalska B. Histological evaluation of mineral trioxide aggregate and calcium hydroxide in direct pulp capping of human immature permanent teeth. Am J Dent. 2008;21(4):262–6.
Seltzer S, Bender IB, Ziontz M. The dynamics of pulp inflammation: correlations between diagnostic data and actual histologic findings in the pulp. Oral Surg Oral Med Oral Pathol. 1963;16:969–77.
Shabahang S. State of the art and science of endodontics. J Am Dent Assoc. 2005;136(1):41–52; quiz 89–90.
Shahravan A, Jalali SP, Torabi M, Haghdoost AA, Gorjestani H. A histological study of pulp reaction to various water/powder ratios of white mineral trioxide aggregate as pulp-capping material in human teeth: a double-blinded, randomized controlled trial. Int Endod J. 2011;44(11):1029–33.
Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62(10):1013–20.
Simancas-Pallares MA, Diaz-Caballero AJ, Luna-Ricardo LM. Mineral trioxide aggregate in primary teeth pulpotomy. A systematic literature review. Med Oral Patol Oral Cir Bucal. 2010;15(6):e942–6.
Song M, Jung IY, Lee SJ, Lee CY, Kim E. Prognostic factors for clinical outcomes in endodontic microsurgery: a retrospective study. J Endod. 2011;37(7):927–33.
Song M, Kim E. A prospective randomized controlled study of mineral trioxide aggregate and super ethoxy-benzoic acid as root-end filling materials in endodontic microsurgery. J Endod. 2012;38(7):875–9.
Sonmez D, Duruturk L. Success rate of calcium hydroxide pulpotomy in primary molars restored with amalgam and stainless steel crowns. Br Dent J. 2010;208(9):E18; discussion 408–9.
Sonmez D, Sari S, Cetinbas T. A comparison of four pulpotomy techniques in primary molars: a long-term follow-up. J Endod. 2008;34(8):950–5.
Srinivasan D, Jayanthi M. Comparative evaluation of formocresol and mineral trioxide aggregate as pulpotomy agents in deciduous teeth. Indian J Dent Res. 2011;22(3):385–90.
Subay RK, Ilhan B, Ulukapi H. Mineral trioxide aggregate as a pulpotomy agent in immature teeth: long-term case report. Eur J Dent. 2013;7(1):133–8.
Subramaniam P, Konde S, Mathew S, Sugnani S. Mineral trioxide aggregate as pulp capping agent for primary teeth pulpotomy: 2 year follow up study. J Clin Pediatr Dent. 2009;33(4):311–14.
Sushynski JM, Zealand CM, Botero TM, Boynton JR, Majewski RF, Shelburne CE, et al. Comparison of gray mineral trioxide aggregate and diluted formocresol in pulpotomized primary molars: a 6- to 24-month observation. Pediatr Dent. 2012;34(5):120–8.
Tang Y, Li X, Yin S. Outcomes of MTA as root-end filling in endodontic surgery: a systematic review. Quintessence Int. 2010;41(7):557–66.
Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25(3):197–205.
Torabinejad M, Parirokh M. Mineral trioxide aggregate: a comprehensive literature review – part II: leakage and biocompatibility investigations. J Endod. 2010;36(2):190–202.
Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. J Endod. 1997;23(4):225–8.
Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993;19(12):591–5.
Torabzadeh H, Asgary S. Indirect pulp therapy in a symptomatic mature molar using calcium enriched mixture cement. J Conserv Dent. 2013;16(1):83–6.
Tuna D, Olmez A. Clinical long-term evaluation of MTA as a direct pulp capping material in primary teeth. Int Endod J. 2008;41(4):273–8.
van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290–9.
Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235–41.
von Arx T, Jensen SS, Hanni S, Friedman S. Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod. 2012;38(5):570–9.
Wang Z, Pan J, Wright JT, Bencharit S, Zhang S, Everett ET, et al. Putative stem cells in human dental pulp with irreversible pulpitis: an exploratory study. J Endod. 2010;36(5):820–5.
Yamasaki M, Kumazawa M, Kohsaka T, Nakamura H, Kameyama Y. Pulpal and periapical tissue reactions after experimental pulpal exposure in rats. J Endod. 1994;20(1):13–7.
Zarrabi MH, Javidi M, Jafarian AH, Joushan B. Histologic assessment of human pulp response to capping with mineral trioxide aggregate and a novel endodontic cement. J Endod. 2010;36(11):1778–81.
Zarrabi MH, Javidi M, Jafarian AH, Joushan B. Immunohistochemical expression of fibronectin and tenascin in human tooth pulp capped with mineral trioxide aggregate and a novel endodontic cement. J Endod. 2011;37(12):1613–18.
Zealand CM, Briskie DM, Botero TM, Boynton JR, Hu JC. Comparing gray mineral trioxide aggregate and diluted formocresol in pulpotomized human primary molars. Pediatr Dent. 2010;32(5):393–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Asgary, S. (2014). Mineral Trioxide Aggregate and Evidence-Based Practice. In: Camilleri, J. (eds) Mineral Trioxide Aggregate in Dentistry. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-55157-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-642-55157-4_9
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-55156-7
Online ISBN: 978-3-642-55157-4
eBook Packages: MedicineMedicine (R0)