Abstract
Autoimmune pancreatitis has a wide range of possible imaging features, and there are overlaps in appearance with other pancreatic diseases. However, in the diagnosis of autoimmune pancreatitis, imaging findings are important components of diagnostic criteria and should be considered in conjunction with the clinical, serologic, and pathological findings. Imaging methods employed in the diagnosis and treatment response evaluation of autoimmune pancreatitis include computed tomography (CT), magnetic resonance imaging (MRI), transabdominal ultrasonography (US), endoscopic retrograde cholangiopancreatography (ERCP), and endoscopic ultrasonography (EUS) [1–4]. Here we focus on typical and atypical findings of autoimmune pancreatitis in CT, MRI, and MRCP and the differential points with other diseases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Apparent Diffusion Coefficient
- Primary Sclerosing Cholangitis
- Main Pancreatic Duct
- Sclerosing Cholangitis
- Autoimmune Pancreatitis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Autoimmune pancreatitis has a wide range of possible imaging features, and there are overlaps in appearance with other pancreatic diseases. However, in the diagnosis of autoimmune pancreatitis, imaging findings are important components of diagnostic criteria and should be considered in conjunction with the clinical, serologic, and pathological findings. Imaging methods employed in the diagnosis and treatment response evaluation of autoimmune pancreatitis include computed tomography (CT), magnetic resonance imaging (MRI), transabdominal ultrasonography (US), endoscopic retrograde cholangiopancreatography (ERCP), and endoscopic ultrasonography (EUS) [1–4]. Here we focus on typical and atypical findings of autoimmune pancreatitis in CT, MRI, and MRCP and the differential points with other diseases.
Pancreas
Typical Findings
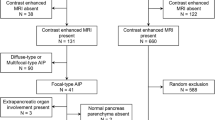
The most important imaging feature of autoimmune pancreatitis is pancreatic enlargement with loss of the lobular architecture often termed “sausage-shaped pancreas” (seen in 40–60 % of cases) [2–6], which is typical when diffuse, and atypical when focal or segmental enlargement according to the International Consensus Diagnostic Criteria [7]. These findings are well delineated on cross-sectional imaging studies, CT (Fig. 11.1) and MRI (Fig. 11.2), the most commonly used modalities due to their availability, reproducibility, and noninvasive nature.
A 59-year-old woman with typical imaging features of autoimmune pancreatitis in the pancreatic (a) and portal venous phase images (b) of CT showing mild diffuse enlargement of the pancreas with loss of the lobular architecture (“sausage-shaped pancreas”), hypoattenuation in the pancreatic phase and hyperattenuation on the portal venous phase (“delayed enhancement”). Note that the pancreas enhances less than the normal pancreas in the pancreatic phase (a) and then exhibits delayed enhancement in the portal venous phase (b). Also note the paucity of peripancreatic stranding
A 56-year-old man with typical imaging features of autoimmune pancreatitis. (a) Axial portal venous phase CT image shows mild diffuse enlargement of the pancreas with hypoattenuating capsule-like rim surrounding the pancreas. (b) Axial T2-weighted MR image shows diffuse enlargement of the pancreas appearing as moderate hyperintensity with hypointense capsule-like rim around the pancreas. (c) MRCP image shows diffuse irregular luminal narrowing of the main pancreatic duct
On CT or MRI, autoimmune pancreatitis enhances less than normal pancreas in the pancreatic phase (or arterial phase) and then demonstrates delayed enhancement in the portal venous and equilibrium phase in over 90 % of cases [2, 7–9]. This delayed enhancement pattern of autoimmune pancreatitis is one of the most important imaging features and useful in differentiating from other diseases, which will be discussed afterward in this chapter. On MRI, the pancreas appears moderately hyperintense on T2-weighted images and hypointense on T1-weighted images in autoimmune pancreatitis patients (Fig. 11.2).
Hypoattenuating or hypointense capsule-like rim surrounding the pancreas is a supplementary finding of autoimmune pancreatitis seen in 12–40 % of cases on CT and MRI [2, 6, 10] (Fig. 11.2). The rim reflects intense inflammatory infiltration and fibrosis of the peripancreatic tissue [8, 10]. On MRI, the rim appears hypointense on T1- and T2-weighted images and delayed enhancement. Peripancreatic fat stranding, which is a common feature in other causes of pancreatitis, is usually minimal in autoimmune pancreatitis [6] (Fig. 11.2). Regional lymphadenopathy and involution of the pancreatic tail can occur in patients with autoimmune pancreatitis [1, 5].
Another imaging hallmark of autoimmune pancreatitis is an irregular luminal narrowing of the main pancreatic duct, of which MRCP is the modality of choice [11, 12] (Fig. 11.2). Typically, there is long (>1/3 of the main pancreatic duct) or multiple strictures in the main pancreatic duct without marked upstream dilatation. And segmental or focal narrowing of the main pancreatic duct without marked upstream dilatation in atypical cases [7]. However, ERCP is necessary if there is any symptomatic biliary obstruction [11, 12].
Of the two known forms of autoimmune pancreatitis, type 1 (lymphoplasmacytic sclerosing pancreatitis) is associated with IgG4-related disease and tends to develop in middle-aged and elderly men (mean age, 59–68 years) with a male-to-female ratio of 4–7.5:1 [13, 14]. The prevalence rate is 2–11 % among patients with chronic pancreatitis [15]. On the other hand, autoimmune pancreatitis type 2 is seen in a younger population in comparison with patients with autoimmune pancreatitis type 1, which lacks elevated IgG4 levels. However, there was no imaging feature of the pancreas reported to differentiate the two types of autoimmune pancreatitis. And the two types may be definitively distinguished only by histopathologic assessment [14].
Atypical Findings and Differential Diagnosis
Autoimmune pancreatitis sometimes exhibits atypical imaging features, which makes the diagnosis difficult. Therefore, the diagnosis of autoimmune pancreatitis requires a combination of clinical, laboratory, imaging, and histologic findings.
The most important atypical imaging finding in autoimmune pancreatitis is focal pancreatic mass-like lesion in 30–40 % of cases, resulting from localized involvement of autoimmune pancreatitis seen commonly in the pancreatic head [1] (Fig. 11.3). The focal form of autoimmune pancreatitis may simulate pancreatic ductal adenocarcinoma, and there are ancillary imaging features helpful in distinguishing the two diseases; prominent lymphadenopathy, vascular occlusion, abrupt narrowing of the pancreatic duct, and marked atrophy of the pancreas distal to the mass increase the possibility of pancreatic carcinoma rather than autoimmune pancreatitis. The pancreatic duct penetrating through the mass-like lesion, known as “duct-penetrating sign,” is considered to be helpful for differentiating focal form of autoimmune pancreatitis from pancreatic cancer even though the finding has low specificity as up to 50 % [16] (Figs. 11.3 and 11.4). Although both autoimmune pancreatitis and pancreatic carcinoma show restricted diffusion (Fig. 11.3), diffusion-weighted MRI has been reported to be helpful in differentiation between autoimmune pancreatitis and pancreatic carcinoma [17, 18]. In a series of Kamisawa et al., the apparent diffusion coefficient (ADC) values were lower in patients with autoimmune pancreatitis than in those with pancreatic carcinoma. A possible ADC cutoff value (1.075 × 10–3 mm2/s) can be used in distinguishing between the two entities [18]. Histological confirmation, however, remains for a diagnosis for many cases of focal autoimmune pancreatitis for differentiation from pancreatic carcinoma. Moreover, although rare in prevalence, pancreatic carcinoma may occur concurrently or during follow-up for autoimmune pancreatitis, even after histological confirmation of the diagnosis [19, 20].
A 56-year-old man with focal autoimmune pancreatitis. A round mass in the pancreas head appearing as moderate hyperintense lesion on (a) axial and (b) coronal T2-weighted MR images. (c) On MRCP image, the distal common bile duct shows segmental narrowing at level of the mass-like lesion in the pancreas head, but patency was preserved (“duct-penetrating sign”). (d) Diffusion-weighted image obtained at b value of 400 s/mm2 and (e) apparent diffusion coefficient map show restricted diffusion of the mass-like lesion in the pancreas head. After steroid treatment, the mass-like lesion in the pancreas head and distal CBD narrowing disappeared on (f) axial CT and (g) ERCP images
A 64-year-old man with pancreatic ductal adenocarcinoma. (a) On axial contrast-enhanced CT image, mild dilatation of the main pancreatic duct and cutoff at body portion was observed without any visible mass lesion. Further evaluation was performed under the suspicion of isoattenuating pancreatic cancer. (b) On axial precontrast T1-weighted MR image, it shows hypointense mass at the portion of duct cutoff. (c) MRCP image also shows abrupt termination of the main pancreatic duct (arrow) at the level of mass. Duct-penetrating sign is negative here, which suggests pancreatic carcinoma
Diffuse autoimmune pancreatitis must be differentiated from other causes of pancreatitis or diffuse pancreatic infiltration. Features that favor autoimmune pancreatitis over acute pancreatitis include the presence of a peripancreatic halo or capsule-like rim, minimal or no peripancreatic fat stranding, and the absence of peripancreatic necrosis [5, 21]. The presence of causative factors, such as gallstones, in addition to imaging features of acute pancreatitis, such as peripancreatic fat stranding and fluid collections, and necrosis of the pancreas or peripancreatic tissue reduce the likelihood of autoimmune pancreatitis (Fig. 11.5) Pseudocyst is a rare finding of autoimmune pancreatitis [5, 22], but often combined in patients with alcohol-induced pancreatitis [23].
A 42-year-old man with acute alcoholic pancreatitis. (a) The arterial phase and (b–c) portal venous phase images of axial contrast-enhanced CT show extensive peripancreatic fat stranding (arrows) and peripancreatic fluid collection in addition to diffuse enlargement of the pancreas. These imaging features point toward acute pancreatitis rather than autoimmune pancreatitis
Another differential diagnosis of autoimmune pancreatitis is lymphoma. Multiple and widespread lymphadenopathy and diffuse pancreatic infiltration would suggest lymphoma. Also, the delayed enhancement pattern of autoimmune pancreatitis is useful in differentiating from lymphoma and ductal adenocarcinoma, which exhibit lower degree of contrast enhancement compared to that of autoimmune pancreatitis in both of the pancreatic and portal venous phases [8, 9, 24].
Imaging Features After Treatment
Recent evidence suggests that most patients have been found to have significant symptomatic improvement after treatment with corticosteroids, and this is usually accompanied by radiological resolution [3, 25, 26] (Fig. 11.3). However, the resolution of radiological features is dependent upon the degree of fibrosis, and inflammatory change is more likely to resolve quickly. Therefore, a long-standing fibrotic disease may not change appearance with treatment, and extrapancreatic manifestations may resolve at a different rate from the pancreatic findings [27].
Bile Duct and Gallbladder
Biliary involvement is the most common extrapancreatic manifestation of autoimmune pancreatitis seen in up to 67–96 % cases, especially in type 1 autoimmune pancreatitis, which is a multisystem fibro-inflammatory disorder and called as IgG4-related disease [3, 16, 28–30]. This condition has been termed IgG4-related sclerosing cholangitis. It can occur without pancreatic findings, and the distal common bile duct is the most common site of biliary involvement.
On contrast-enhanced CT and MRI, the affected segments of the bile duct show mural thickening with enhancement, luminal narrowing, and stenosis (Fig. 11.6). In addition to CT and MRI, MRCP is helpful for a precise assessment of the location and extent of biliary involvement, especially when there are multifocal involvement in both the intra- and extrahepatic bile ducts.
A 71-year-old man presented with diffuse biliary dilatation. (a) On axial CT image, the pancreas shows mild enlargement with hypoattenuating capsule-like rim around the pancreas. (b) On axial contrast-enhanced T1-weighted image and (c) coronal T2-weighted MR image, long segmental luminal narrowing and wall thickening of the hilar duct (arrow) was noted at the hepatic hilum. (d) On MRCP, multifocal stenosis and dilatation of IHD and irregular stricture and dilatation of the main pancreatic duct
There are some overlaps in the imaging features of IgG4-related sclerosing cholangitis and cholangiocarcinoma [21] and primary sclerosing cholangitis in 10–35 % of cases [31]. On MRCP, primary sclerosing cholangitis shows multifocal, short segmental, band-like strictures. A beaded appearance with alternating strictures and normal or slightly dilated segments, a pruned-tree appearance with decreased in number of visible peripherally located intrahepatic ducts, and diverticulum-like lesions involving the intra- or extrahepatic bile ducts are characteristic findings [28] (Fig. 11.7). In IgG4-related sclerosing cholangitis, stricture typically affects a long segment and is continuous with prestenotic dilatation. And isolated stricture of the distal common bile duct is common unlike multifocal involvement in primary sclerosing cholangitis [28]. In a series of Kim et al., multifocal stricture and/or wall thickening of intrahepatic bile duct stricture and pruned-tree appearance were more frequent on MRCP in primary sclerosing cholangitis than in IgG4-related sclerosing cholangitis patients [32]. In their series, on CT and MRI, the bile duct wall was thicker (5.1 mm vs. 3.1 mm and 4.3 mm vs. 3.0 mm, respectively) in IgG4-related sclerosing cholangitis than in primary sclerosing cholangitis patients.
When present, soft tissue around the bile ducts in IgG4-related sclerosing cholangitis tends to be larger in extent compared to that in primary sclerosing cholangitis. Periductal soft tissue mass is rarely seen, but can mimic cholangiocarcinoma [31]. In the differentiation of IgG4-related sclerosing cholangitis and cholangiocarcinoma, IgG4-related sclerosing cholangitis was reported to have more frequently intrapancreatic common bile duct involvement, concentric wall thickening, smooth outer margin of the thickened wall, and lower degrees of wall thickening, upstream dilatation, and contrast enhancement of the bile duct compared to common bile duct cancer in a series of Kim et al. [33]. Also in their study, IgG4-related sclerosing cholangitis appeared to have more frequently smooth margin, gradual and symmetric narrowing, multifocal involvement, and hourglass appearance of the bile duct than common bile duct cancer on ERCP and MRCP.
Gallbladder involvement can also occur in up to 25 % of patients with IgG4-related autoimmune pancreatitis with concurrent sclerosing cholangitis and manifest as diffuse thickening of the gallbladder wall [31]. In contrast to the nonspecific imaging appearance of acalculous diffuse cholecystitis of other causes, IgG4-related cholecystitis shows predominant extramural involvement and subserosal inflammatory nodules.
References
Finkelberg DL, Sahani D, Deshpande V, Brugge WR. Autoimmune pancreatitis. N Engl J Med. 2006;355(25):2670–6.
Suzuki K, Itoh S, Nagasaka T, Ogawa H, Ota T, Naganawa S. CT findings in autoimmune pancreatitis: assessment using multiphase contrast-enhanced multisection CT. Clin Radiol. 2010;65(9):735–43.
Sahani DV, Kalva SP, Farrell J, et al. Autoimmune pancreatitis: imaging features. Radiology. 2004;233(2):345–52.
Okazaki K, Kawa S, Kamisawa T, et al. Japanese consensus guidelines for management of autoimmune pancreatitis: I. Concept and diagnosis of autoimmune pancreatitis. J Gastroenterol. 2010;45(3):249–65.
Shanbhogue AK, Fasih N, Surabhi VR, Doherty GP, Shanbhogue DK, Sethi SK. A clinical and radiologic review of uncommon types and causes of pancreatitis. Radiographics. 2009;29(4):1003–26.
Kawamoto S, Siegelman SS, Hruban RH, Fishman EK. Lymphoplasmacytic sclerosing pancreatitis (autoimmune pancreatitis): evaluation with multidetector CT. Radiographics. 2008;28(1):157–70.
Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas. 2011;40(3):352–8.
Takahashi N, Fletcher JG, Hough DM, et al. Autoimmune pancreatitis: differentiation from pancreatic carcinoma and normal pancreas on the basis of enhancement characteristics at dual-phase CT. AJR Am J Roentgenol. 2009;193(2):479–84.
Ishigami K, Tajima T, Nishie A, et al. MRI findings of pancreatic lymphoma and autoimmune pancreatitis: a comparative study. Eur J Radiol. 2010;74(3):e22–8.
Kwak SW, Kim S, Lee JW, et al. Evaluation of unusual causes of pancreatitis: role of cross-sectional imaging. Eur J Radiol. 2009;71(2):296–312.
Kamisawa T, Tu Y, Egawa N, et al. Can MRCP replace ERCP for the diagnosis of autoimmune pancreatitis? Abdom Imaging. 2009;34(3):381–4.
Park SH, Kim MH, Kim SY, et al. Magnetic resonance cholangiopancreatography for the diagnostic evaluation of autoimmune pancreatitis. Pancreas. 2010;39(8):1191–8.
Kamisawa T, Yoshiike M, Egawa N, et al. Chronic pancreatitis in the elderly in Japan. Pancreatology. 2004;4(3–4):223–7; discussion 227–8.
Zhang L, Chari S, Smyrk TC, et al. Autoimmune pancreatitis (AIP) type 1 and type 2: an international consensus study on histopathologic diagnostic criteria. Pancreas. 2011;40(8):1172–9.
Divatia M, Kim SA, Ro JY. IgG4-related sclerosing disease, an emerging entity: a review of a multi-system disease. Yonsei Med J. 2012;53(1):15–34.
Kim JH, Kim MH, Byun JH, et al. Diagnostic strategy for differentiating autoimmune pancreatitis from pancreatic cancer: is an endoscopic retrograde pancreatography essential? Pancreas. 2012;41:639–647
Taniguchi T, Kobayashi H, Nishikawa K, et al. Diffusion-weighted magnetic resonance imaging in autoimmune pancreatitis. Jpn J Radiol. 2009;27(3):138–42.
Kamisawa T, Takuma K, Anjiki H, et al. Differentiation of autoimmune pancreatitis from pancreatic cancer by diffusion-weighted MRI. Am J Gastroenterol. 2010;105(8):1870–5.
Loos M, Esposito I, Hedderich DM, et al. Autoimmune pancreatitis complicated by carcinoma of the pancreatobiliary system: a case report and review of the literature. Pancreas. 2011;40(1):151–4.
Takuma K, Kamisawa T, Tabata T, Inaba Y, Egawa N, Igarashi Y. Short-term and long-term outcomes of autoimmune pancreatitis. Eur J Gastroenterol Hepatol. 2011;23(2):146–52.
Vlachou PA, Khalili K, Jang HJ, Fischer S, Hirschfield GM, Kim TK. IgG4-related sclerosing disease: autoimmune pancreatitis and extrapancreatic manifestations. Radiographics. 2011;31(5):1379–402.
Welsch T, Kleeff J, Esposito I, Buchler MW, Friess H. Autoimmune pancreatitis associated with a large pancreatic pseudocyst. World J Gastroenterol. 2006;12(36):5904–6.
Gouyon B, Levy P, Ruszniewski P, et al. Predictive factors in the outcome of pseudocysts complicating alcoholic chronic pancreatitis. Gut. 1997;41(6):821–5.
Miller FH, Rini NJ, Keppke AL. MRI of adenocarcinoma of the pancreas. AJR Am J Roentgenol. 2006;187(4):W365–74.
Church NI, Pereira SP, Deheragoda MG, et al. Autoimmune pancreatitis: clinical and radiological features and objective response to steroid therapy in a UK series. Am J Gastroenterol. 2007;102(11):2417–25.
Ghazale A, Chari ST, Zhang L, et al. Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterology. 2008;134(3):706–15.
Sohn JH, Byun JH, Yoon SE, et al. Abdominal extrapancreatic lesions associated with autoimmune pancreatitis: radiological findings and changes after therapy. Eur J Radiol. 2008;67(3):497–507.
Nakazawa T, Ohara H, Sano H, et al. Cholangiography can discriminate sclerosing cholangitis with autoimmune pancreatitis from primary sclerosing cholangitis. Gastrointest Endosc. 2004;60(6):937–44.
Nishino T, Toki F, Oyama H, et al. Biliary tract involvement in autoimmune pancreatitis. Pancreas. 2005;30(1):76–82.
Kamisawa T, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Extrapancreatic lesions in autoimmune pancreatitis. J Clin Gastroenterol. 2005;39(10):904–7.
Bodily KD, Takahashi N, Fletcher JG, et al. Autoimmune pancreatitis: pancreatic and extrapancreatic imaging findings. AJR Am J Roentgenol. 2009;192(2):431–7.
Kim JH, Byun JH, Kim SY, et al. Sclerosing cholangitis with autoimmune pancreatitis versus primary sclerosing cholangitis: comparison on endoscopic retrograde cholangiography, MR cholangiography, CT, and MRI. Acta Radiol. 2013;54(6):601–7.
Kim JH, Byun JH, Lee SJ, et al. Differential diagnosis of sclerosing cholangitis with autoimmune pancreatitis and periductal infiltrating cancer in the common bile duct at dynamic CT, endoscopic retrograde cholangiography and MR cholangiography. Eur Radiol. 2012;22(11):2502–13.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Park, M.J., Chung, Y.E., Park, MS. (2015). Imaging Findings: CT and MRI with MRCP. In: Kamisawa, T., Chung, J. (eds) Autoimmune Pancreatitis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-55086-7_11
Download citation
DOI: https://doi.org/10.1007/978-3-642-55086-7_11
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-55085-0
Online ISBN: 978-3-642-55086-7
eBook Packages: MedicineMedicine (R0)