Abstract
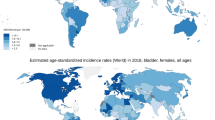
Worldwide, approximately 330,000 new cases of bladder cancer (BC) are diagnosed each year and 130,000 people die annually of this disease. Median age at diagnosis is 70 years and men are at 3.8 times higher risk than women. In western countries, the lifetime risk of developing BC is 2.4 % and it is the fourth most common solid tumor in men. Exposures known to increase the risk of BC include tobacco smoke, occupational carcinogens, and schistosomiasis. Dietary factors that decrease BC risk include high water intake and cruciferous legume consumption.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 General Facts
Worldwide, approximately 330,000 new cases of bladder cancer (BC) are diagnosed each year and 130,000 people die annually of this disease. Median age at diagnosis is 70 years and men are at 3.8 times higher risk than women. In western countries, the lifetime risk of developing BC is 2.4 % and it is the fourth most common solid tumor in men. Exposures known to increase the risk of BC include tobacco smoke, occupational carcinogens, and schistosomiasis. Dietary factors that decrease BC risk include high water intake and cruciferous legume consumption.
2 Symptoms, Classification, and Grading
Presenting symptoms of BC include hematuria (75 %), irritative lower urinary tract symptoms (20 %), and pain (5 %, which is usually due to ureteral obstruction by tumor). In western countries, the most common histologic subtype of BC is urothelial carcinoma (90 %), with squamous cell carcinoma (5 %), adenocarcinoma (2 %), and small cell carcinoma (1 %) being less common. In areas where schistosomiasis is endemic, squamous cell carcinomas comprise 50 % of BCs.
Conventional white light cystoscopy remains the gold standard for diagnosing bladder cancer (sensitivity 90 %, specificity 90 %), though fluorescent cystoscopy is an alternative that is slightly more sensitive but less specific. Urine tests are also used in the diagnosis of bladder cancer though their precise role is unclear. Urine cytology has a sensitivity of 35 % (80 % for CIS) and specificity of 95 % for BC and remains the most frequently used urine test. Once a tumor is visualized at cystoscopy, the first step in diagnosis/treatment is transurethral resection (TURBT).
BC is staged using the TNM/AJCC system (Table 31.1). The TURBT procedure determines the preliminary T stage, while the N and M stages are determined by cross-sectional imaging of the abdomen/pelvis, chest imaging, and bone imaging. Brain imaging is only indicated if metastases are present elsewhere. The upper urinary tracts should be imaged at diagnosis (CT or MRI urography, retrograde or intravenous pyelography) since 5 % of patients will have ureteral or renal pelvic tumors. At diagnosis, 70 % of bladder tumors are non-muscle invasive (NMIBC; Ta, T1, or Tis), 20 % are muscle invasive (MIBC; T2, T3, or T4), and 10 % are metastatic (N + or M1). Median and relative survival rates are stage dependent (Table 31.1).
BC grading is done using the WHO/ISUP system (Table 31.2). NMIBC is characterized by a very high local recurrence rate which ranges from 25 to 85 % depending on known risk factors. The risk of stage progression ranges from 5 to 35 % also depending on risk factors. The EORTC BC risk prediction tool quantifies these risk factors (www.eortc.com/tools/bladdercalculator).
3 Therapy
TURBT is the gold standard for the initial diagnosis/treatment of BC. Immediate postoperative instillation of intravesical chemotherapy (e.g., mitomycin C, epirubicin, doxorubicin) is indicated after TURBT for NMIBC since it lowers the recurrence rate by 35 %. Patients at intermediate or high risk of recurrence or progression should be treated with adjuvant intravesical chemotherapy or BCG (preferred for CIS and high-risk patients). These treatments should include an induction phase (weekly instillations for 6 weeks) and a maintenance phase lasting at least 1 year. A second look TURBT is performed 2–6 weeks later if the initial TURBT was incomplete, if a large tumor burden was present (size or multifocality), or if high-grade or T1 pathology was noted. Surveillance for recurrence consists of periodic cystoscopy and/or urine testing and imaging, the frequency of which is risk adapted. Patients with high-risk NMIBC that fail to respond to intravesical therapy should undergo radical cystectomy since survival decreases if these tumors progress to MIBC.
When MIBC is found at TURBT, more invasive therapies are needed to prevent metastasis and local progression. The gold standard therapy for MIBC is radical cystectomy (RC). In men, RC consists of resection of the bladder, prostate, and lymph nodes, while in women the uterus, fallopian tubes, and ovaries are also included. Urinary diversion options include ileal and colonic conduits, catheterizable cutaneous pouches, and neobladders. Bladder sparing chemoradiation therapy is an alternative to RC but is only administered to relatively asymptomatic patients with low tumor burden. Chemotherapy is a critical component of the management of MIBC and is best given neoadjuvantly to RC or concurrently with radiation. The two most active chemotherapy regimens are GC (gemcitabine, cisplatin) and MVAC (methotrexate, vinblastine, Adriamycin, cisplatin). These regimens increase survival by 5–10 % in MIBC patients and by 6 months in patients with metastases.

4 Complications
TURBT is a minimally invasive procedure and serious complications are rare, but include bladder perforation and bleeding. Contrarily, RC is a very invasive procedure and perioperative mortality ranges from 1 to 5 % and is age and comorbidity dependent. While early postoperative complications occur in 25–50 % of RCs, most are minor and treatable. Late morbidity after RC is mainly associated with the urinary diversion (Fig. 31.1).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Kramer, M.W., Cash, H., Inman, B.A. (2014). Bladder Cancer. In: Merseburger, A., Kuczyk, M., Moul, J. (eds) Urology at a Glance. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-54859-8_31
Download citation
DOI: https://doi.org/10.1007/978-3-642-54859-8_31
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-54858-1
Online ISBN: 978-3-642-54859-8
eBook Packages: MedicineMedicine (R0)