Abstract
The incidence of fracture non-union has been estimated to be as high as 10 %. The treatment of fracture non-union remains challenging even for the most experienced surgeons. The presence of a poor soft tissue envelope, deformity, avascular bone edges, reduced bone stock, low-grade infection and patient related co-morbidities are some of the important contributing factors that need to be addressed. Evaluation of the complexity of the non-union and formulating the appropriate pre-operative plan and treatment modality requires good understanding of the pathogenicity of this condition and having extensive surgical experience.
The state of both the mechanical and biological environment, is thought to play a crucial role in the decision making process regarding revision surgery. Application of the so-called ‘diamond concept’ provides the optimum mechano-biological conditions for bone repair and should be considered in cases where difficulties to achieve union are anticipated.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vascular Endothelial Growth Factor
- Fracture Healing
- Bone Repair
- Osteoprogenitor Cell
- Open Reduction Internal Fixation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Fracture healing and bone regeneration represent a complex and well-orchestrated physiological process that involves timed cellular recruitment, gene expression and secretion of multiple signalling molecules [1]. In response to injury and fracture, bone has a unique intrinsic capacity for repair and regeneration [2, 3]. In contrast to the majority of tissues in the human body that heal by the formation of a scar of inferior quality, bone generated by the process of fracture healing encompasses its former biochemical and biomechanical properties [4]. This phenomenon can be described as a regenerative process that recapitulates aspects of embryonic skeletal development, combined with normal responses to acute tissue injury [1, 5].
Types of Bone Healing
With regards to the histology of bone healing two basic types have been described, depending on the stability of fixation of the fracture’s bone fragments [2, 3, 6].
-
1.
The primary (direct) healing pattern occurs when there is absolute contact of the bone fragments (anatomical reduction) along with almost complete stability (commonly obtained with open reduction and internal fixation) and therefore minimisation of the inter-fragmentary strains [7, 8]. In this type of healing that rarely happens in nature, the disrupted continuity of the bone is re-established with regeneration of lamellar bone and the Harvesian system, and has no need of any remodelling [8, 9].
-
2.
The secondary (indirect) healing pattern occurs in the vast majority of clinical cases and depends on the formation of fibrocartilaginous callus that matures to mineralised cartilage and finally bone [2, 7]. Callus is formed as a physiological reaction to the inter-fragmentary movement and involves both intramembranous and endochondral ossification [2, 7–9]. It originates from committed osteoprogenitor cells of the periosteum and undifferentiated multipotent mesenchymal stem cells (MSCs) [7].
Fracture Healing and Bone Repair
Several types of tissues are involved in the process of fracture healing including cortical bone, periosteum, undifferentiated fascial tissue that surrounds the fracture, and bone marrow [9, 10]. Bone repair follows a well defined chain of events starting with haematoma formation, followed by inflammation, angiogenesis and granulation tissue formation, fibrous tissue formation, fibrocartilage, hyaline cartilage (soft callus), cartilage mineralisation, woven bone (hard callus), and finally remodelling [2, 6, 11]. The process of remodelling can last for several months.
In more detail, following an injury the bone architecture and the surrounding soft tissue continuity are both disrupted. The concomitant tearing of the blood vessels at the site of injury leads to bleeding, activation of the coagulation cascade and therefore the formation of a haematoma that encloses the fracture area [12]. The haematoma contains cells that originate from the peripheral and intramedullary blood, as well as bone marrow cells [8]. Different cellular populations have been described including inflammatory immune cells, neutrophils, monocytes and macrophages (activated by the coagulation process), fibroblasts and MSC’s [2, 12]. Through the different type of mediators secreted, the formed haematoma exhibits a complex micro-environment that can exert different effects on diverse cell populations [2].
All stages of fracture healing are well co-ordinated but any insufficiency to one or more of these pathways can alter the physiological sequence of fracture healing. This interruption can lead to complications such as an impaired fracture healing response expressed as delayed union or non-union. In order to reverse any deficiency to one or more of these pathways, planned targeted interventions should be well-timed and well-aimed [7].
Biological Pre-requisites for Successful Union
Certain biological pre-requisites have been identified during the complex process of fracture healing. Different types of cells are recognised to interact with local and systemic regulatory molecules, cytokines, hormones and extracellular osteoconductive matrix [7, 11].
Osteogenic Cells
The first element for an unimpeded fracture repair is a vibrant cell population [7]. These cells include specific mesenchymal stem cells (MSC’s) that under the appropriate molecular signalling are recruited, proliferate and differentiate to osteogenic cells [8]. These MSC’s originate from the surrounding soft tissues, cortex, periosteum, bone marrow and systemic circulation (mobilised from remote haemopoietic sites) [8], with their transformation to cells with an osteoblastic phenotype occurring in areas of high cellular density [13, 14].
Since the identification and quantification of the role of MSC’s in osteogenesis, several in vitro and in vivo studies concentrated on the use of genetically engineered MSCs [15–19] and differentiated osteoblasts to enhance fracture healing [20, 21].
Growth Factors
Several signalling molecules exerting a direct influence on the faith of MSC’s have been isolated within the fracture haematoma. These are categorised into three groups: the pro-inflammatory cytokines; the transforming growth factor-beta (TGF-β) superfamily and other growth factors; and the angiogenic factors [3].
The major signalling molecules include: transforming growth factor-β (TGF-β) that upregulates the undifferentiated MSC’s [10, 12]; bone morphogenic proteins (BMP’s) that promote the differentiation of MSC’s into chondrocytes and osteoblasts, and osteoprogenitor cells into osteoblasts [9, 10, 12]; fibroblast growth factor (FGF) that enhances mitogenesis of MSCs [10, 12]; insulin-like growth factor (IGF) that promotes proliferation and differentiation of osteoprogenitor cells [10, 12]; platelet-derived growth factor (PDGF) that facilitates mitogenesis of MSCs and is responsible for macrophage chemotaxis [10, 12]. Vascular endothelial growth factor (VEGF) is responsible for the blood vessel invasion of hyaline cartilage, growth-plate morphogenesis, and cartilage remodelling, by regulating recruitment, survival and activity of endothelial cells, osteoblasts and osteoclasts [12]. An increased secretion of factors promoting the recruitment of inflammation cells and angiogenesis is also evident (tumour necrosis factor-α (TNF-α), interleukin-1 (IL-1), IL-6, IL-11 and IL-18) [8, 10].
Many of these molecules have been extensively studied to evaluate their clinical effectiveness in enhancing fracture healing. BMP’s represent the sole clinically approved agents for applications related to fracture repair [1]. BMP-7 is FDA(Federal Drug Administration) approved for treatment of long bone non-unions, whereas BMP-2 has recently gained FDA approval for the treatment of open tibial fractures and spinal fusion surgery [1]. The clinical data on their safety and efficacy appears to be positive [22–25], whereas their application for off-label indications is also promising [22–31].
PDGF has also demonstrated promising results in the enhancement of fracture healing when used in animal studies [32, 33]. Other growth factors that are currently under investigation include growth and differentiation factor-5 (GDF-5) [34], insulin-like growth factor-1 (IGF-1) [35, 36], growth hormone (GH) [37] and platelet-rich plasma (PRP) [38–40].
Osteoconductive Scaffolds
During the natural process of indirect fracture healing, a fibrin-rich granulation tissue derives from the fracture haematoma [8]. This extra-cellular matrix provides a natural scaffold (osteoconductive properties) where all the cellular events and interactions take place, including cell adhesion, migration, proliferation and differentiation [1, 7, 41].
In the clinical setting, the ideal material to be used should mimic the native characteristics of the tissue, provide a source of cells capable of promoting proliferation and differentiation, as well as acting as a scaffold for angiogenesis, cell migration and attachment [13].
Various materials simulating some of the properties of this extra-cellular matrix have been clinically used. Autologous bone graft harvested from the iliac crest remains the “gold standard” for bone augmentation in non-unions [6, 42]. The Reamer-Irrigator-Aspirator (RIA) technique has also been used for obtaining from long bones and particularly the intramedullary (IM) canal of the femur autologous bone graft avoiding some of the complications related to the iliac crest harvesting [43]. Other porous biomaterials used as bone void fillers include allograft or xenograft trabecular bone, demineralised bone matrix (DBM), collagen, hydroxyapatite, polylactic or polyglycolic acid, bio-active glasses and calcium-based ceramics [7, 44]. Modern scaffolds recently introduced involve osteoconductive synthetic metallic materials (Porous Tantalum, Trabecular Titanium etc.), offering a three-dimensional reticular frame where osteoblasts and osteoclasts proliferate producing bone [44–46].
Mechanical Environment
The process of inflammation and angiogenesis depend largely upon the mechanical conditions [2] and should therefore be taken under consideration in optimising fracture healing. Mechanical stability is essential for the formation of callus and its progressive maturation from woven to lamellar bone [7], whereas in case of rigid fixation no callus is evident (primary bone healing).
Mechanical stability at the fracture site is relevant to the selected type of fixation and can be achieved using ORIF (open reduction internal fixation), locking plating systems, intramedullary nailing and external fixation systems [41]. Plaster-of-Paris also represents a form of stabilisation using non-invasive external immobilisation support. In general terms it can be said that any surgical intervention (external or internal fixation systems) that improves fracture stability enhances the physiological process of bone repair.
Vascularity
Blood supply and revascularisation are essential for a successful fracture healing, including the final stage of remodelling [8]. The process of revascularisation involves not only neo-angiogenesis, but also the apoptosis of chondrocyte cells, the cartilaginous degradation and the removal of cells and extracellular matrices for blood vessel in-growth [8]. During uncomplicated bone repair, the medullary, periosteal and osseous blood supply can be enhanced according to the physiological needs [12].
Two molecular pathways mainly regulate the vascularisation process: the angiopoietin-dependent pathway and the vascular endothelial growth factor (VEGF)-dependent pathway, with the second being considered as the key regulator of vascular regeneration [8, 47]. VEGF is an osteogenic, pro-resorptive, oxygen-sensitive, signalling molecule that can regulate the function of osteoblasts, osteoclasts and osteocytes [48]. Evidence of the importance of this molecule has been reported with the inhibition of VEGF activity, by neutralizing VEGF receptor [49]. On the contrary, exogenous administration of VEGF enhanced blood vessel formation, ossification, and new bone (callus) maturation [49]. Evidence is now emerging that VEGF can be used to promote angiogenesis and osteogenesis, therefore improving bone repair [50–52].
Host
The optimal treatment of these challenging clinical problems should be tailored and individualised to the mechanical and molecular biology of the host. Identified risk factors for impaired bone healing amongst others include: poor blood supply, poor apposition of fractured bone ends, interposition of soft tissues or necrotic bone between bone fragments, inadequate immobilisation, infection, drug use (e.g. corticosteroid therapy or nicotine), advanced age, and systemic disorders such as diabetes or poor nutrition [12].
Apart from the previously described biological variation of the host, genetic predisposition is believed to be yet another important element of fracture healing [53–55]. Gene therapy is an emerging but rapidly developing approach to the treatment of non-unions, with encouraging results [56, 57].
“Diamond Concept”
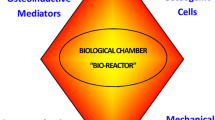
The so-called “Diamond Concept” has been proposed for the successful regeneration of bone and the treatment of fracture non-unions and bone defects [6, 7, 58, 59]. It represents a conceptual framework, which takes into consideration all the essential biological pre-requisites for a successful fracture healing response. It supports the implantation of MSCs, an osteoconductive scaffold and application of a growth factor to reconstitute the molecular milieu known to be necessary for the initiation and successful completion of bone repair. However, prior to any intervention and implantation of any or all of these constituents, the non-union bed of the host should be optimised, in terms of vascularity, containment and possessing adequate mechanical support where molecular and physiological processes will evolve promoting an early and successful osteogenesis [59] (Fig. 1).
Following a successful implementation of the “Diamond Concept”, the non-union bed should have been transformed to a ‘biological chamber’, the so called ‘local bioreactor’, capable of supporting efficiently all the vital interactions between cells, growth factors and the underlying osteoconductive matrix facilitating a successful outcome [59]. In a sense the ‘biological chamber’ constitutes the centre of the highest biological activity, where all the cascade of events of bone repair and regeneration progress in a time-dependent fashion so that bone continuity can be restored [59]. The induced membrane formed following the application of the ‘Masquelet technique’ appears to be the ideal material to surround this ‘biological chamber’, as it can be produced naturally and possesses unique osteogenic promoting properties [60, 61].
“Diamond Concept” in the Clinical Setting
The “Diamond Concept” has been applied in the clinical setting in recalcitrant non-unions with multiple failed previous interventions, and the results obtained are very promising [6, 29–31]. However, one may argue whether it is always necessary to apply the conceptual framework of the diamond configuration (signals, cells, scaffold and/or revision of the fixation) for a successful outcome. The issue of whether there is still adequate mechanical stability present, and as such there is no need for revision of the fixation, can be addressed by careful evaluation of the radiographic findings of the affected extremity. Is there evidence of loosening or osteolysis of the interface between the bone and the existing implant? Is there failure of the metalwork? Does the patient report the presence of substantial painful stimuli whilst mobilising? How long the implant has been in situ prior to our planned intervention? Will the existing implant following our intervention continue to provide adequate mechanical support for the subsequent 6–9 months or else until the anticipated amount of time for union to occur has been reached? These are some of the important parameters that need to be answered in order to decide whether revision of the fixation is mandatory. The decision whether to apply only one of the biological constituents (monotherapy) of the ‘diamond concept’ or all of them simultaneously ((cells, signals and a scaffold) – (polytherapy)) remains more challenging. Will it be sufficient to implant only osteoprogenitor cells? Only a growth factor or perhaps only a scaffold? How can I reach a sensible decision to ensure that my biological based therapy would be enough to promote successfully bone regeneration? Obviously the natural history of the non-union or else the bone defect area is crucial to be accurately documented. How many previous interventions have taken place without success? Are we dealing with a recalcitrant non-union? What is the state of the surrounding soft tissue envelope? Is there muscle wasting, local atrophy? Does the colour of the extremity/skin look compromised? Is there a history of underlying host pathology (i.e. diabetes, peripheral vascular disease)? Is the patient a smoker? These are some of the important factors to be evaluated to allow us to take the right decision.
In order to address the above issues a non-union scoring system was developed so that the clinician can be assisted to reach the right decision [62]. It takes into account the bone/anatomical criteria and soft tissues condition, as well as the patient’s characteristics, co-morbidities and drug use (Table 1), [62]. According to this non-union scoring system, scores from 0 to 25 would be considered straightforward non-unions and should respond well to standard treatments. Scores from 26 to 50 would require more specialised care. For patients with scores from 51 to 75, specialised care and specialised treatments should be sought. Finally, patients with scores above 75 may be candidates for consideration for primary amputation [62]. Application of a biologically- based therapy should be considered in patients with a score of more than 26 points and when the score is above 51 points the diamond concept must be applied (Fig. 2).
(a) Radiographs AP, Lateral of a subtrochanteric non-union of a male patient 40 years of age. The patient had sustained a previous fracture that was stabilised with a cephalomedullary nail which was associated with implant failure and infection. The radiographs seen are 12 months after the removal of the failed implant. The initial non-union had been managed with temporarily stabilisation with an external fixator and several operative procedures for the control and eradication of the infection. In total the patient had undergone five previous procedures. He was a smoker. There was muscular wasting in the right lower extremity and a leg length discrepancy of 3 cm. Radiographs revealed signs of bone disuse and porosis. He was on a long-term prescription of non-steroidal anti-inflammatory medication. His non-union score was (bone component = 16, soft tissue component = 2, patient component = 8). Total points 26 × 2 = 52. (b) Intra-operative photograph illustrating that the right femoral non-union has been stabilised with a blade-plate following debridement of the non-union site. A collagen membrane (white material shown between the plate and the bone was inserted for the containment of the graft material. (c) Introperative photograph illustrating the diamond concept application: implantation of a growth factor (BMP-7), concentrated bone marrow aspirate (osteoprogenitor cells) and bone graft (scaffold). (d) Containment of the implanted graft using the collagen membrane. (e) Post-operative AP and Lateral radiographs. (f) Four months follow-up radiographs revealing osseous union of the previous right femoral subtrochanteric non-union
Conclusion
Several cells and molecules are actively involved in fracture healing, each having a distinct temporal expression pattern and role. A better understanding and deeper knowledge of the pathways involved would give us the opportunity to target each of these cascades independently. “Tissue engineering” is expected to revolutionise the treatment of patients with impaired bone healing, providing novel treatment strategies in the years to come [41]. However, there are several challenging technical issues that still need to be overcome. The “diamond concept” attributes equal importance to both the biological and mechanical environment and provides the clinician with a stepwise approach in dealing complex clinical cases of non-unions [41]. Moreover, the concept of the ‘biological chamber’ sitting at the heart of the diamond concept allows the clinician to consider in a more structured way the underlying molecular environment. With combination of therapies, the results of these difficult clinical conditions may be optimised providing a better, cost-effective treatment modality.
References
Komatsu DE, Warden SJ. The control of fracture healing and its therapeutic targeting: improving upon nature. J Cell Biochem. 2010;109:302–11.
Kolar P, Schmidt-Bleek K, Schell H, Gaber T, Toben D, Schmidmaier G, Perka C, Buttgereit F, Duda GN. The early fracture hematoma and its potential role in fracture healing. Tissue Eng Part B Rev. 2010;16:427–34.
Dimitriou R, Tsiridis E, Giannoudis PV. Current concepts of molecular aspects of bone healing. Injury. 2005;36:1392–404.
Henle P, Zimmermann G, Weiss S. Matrix metalloproteinases and failed fracture healing. Bone. 2005;37:791–8.
Ferguson C, Alpern E, Miclau T, Helms JA. Does adult fracture repair recapitulate embryonic skeletal formation? Mech Dev. 1999;87:57–66.
Giannoudis PV, Ahmad MA, Mineo GV, Tosounidis TI, Calori GM, Kanakaris NK. Subtrochanteric fracture non-unions with implant failure managed with the “Diamond” concept. Injury. 2013;44 Suppl 1:S76–81.
Giannoudis PV, Einhorn TA, Marsh D. Fracture healing: the diamond concept. Injury. 2007;38 Suppl 4:S3–6.
Marsell R, Einhorn TA. The biology of fracture healing. Injury. 2011;42:551–5.
Einhorn TA. The science of fracture healing. J Orthop Trauma. 2005;19:S4–6.
Phillips AM. Overview of the fracture healing cascade. Injury. 2005;36 Suppl 3:S5–7.
Tsiridis E, Upadhyay N, Giannoudis P. Molecular aspects of fracture healing: which are the important molecules? Injury. 2007;38 Suppl 1:S11–25.
Carano RA, Filvaroff EH. Angiogenesis and bone repair. Drug Discov Today. 2003;8:980–9.
Pountos I, Corscadden D, Emery P, Giannoudis PV. Mesenchymal stem cell tissue engineering: techniques for isolation, expansion and application. Injury. 2007;38 Suppl 4:S23–33.
Papathanasopoulos A, Giannoudis PV. Biological considerations of mesenchymal stem cells and endothelial progenitor cells. Injury. 2008;39 Suppl 2:S21–32.
Qi Y, Zhao T, Yan W, Xu K, Shi Z, Wang J. Mesenchymal stem cell sheet transplantation combined with locally released simvastatin enhances bone formation in a rat tibia osteotomy model. Cytotherapy. 2013;15:44–56.
Cheung WH, Chin WC, Wei FY, Li G, Leung KS. Applications of exogenous mesenchymal stem cells and low intensity pulsed ultrasound enhance fracture healing in rat model. Ultrasound Med Biol. 2013;39:117–25.
Obermeyer TS, Yonick D, Lauing K, Stock SR, Nauer R, Strotman P, Shankar R, Gamelli R, Stover M, Callaci JJ. Mesenchymal stem cells facilitate fracture repair in an alcohol-induced impaired healing model. J Orthop Trauma. 2012;26:712–18.
Keramaris NC, Kaptanis S, Moss HL, Loppini M, Pneumaticos S, Maffulli N. Endothelial progenitor cells (EPCs) and mesenchymal stem cells (MSCs) in bone healing. Curr Stem Cell Res Ther. 2012;7:293–301.
Toupadakis CA, Granick JL, Sagy M, Wong A, Ghassemi E, Chung DJ, Borjesson DL, Yellowley CE. Mobilization of endogenous stem cell populations enhances fracture healing in a murine femoral fracture model. Cytotherapy. 2013;15:1136–47.
Chen F, Mao T, Tao K, Chen S, Ding G, Gu X. Bone graft in the shape of human mandibular condyle reconstruction via seeding marrow-derived osteoblasts into porous coral in a nude mice model. J Oral Maxillofac Surg. 2002;60:1155–9.
Mao X, Chu CL, Mao Z, Wang JJ. The development and identification of constructing tissue engineered bone by seeding osteoblasts from differentiated rat marrow stromal stem cells onto three-dimensional porous nano-hydroxylapatite bone matrix in vitro. Tissue Cell. 2005;37:349–57.
Aro HT, Govender S, Patel AD, Hernigou P, Perera de Gregorio A, Popescu GI, Golden JD, Christensen J, Valentin A. Recombinant human bone morphogenetic protein-2: a randomized trial in open tibial fractures treated with reamed nail fixation. J Bone Joint Surg Am. 2011;93:801–8.
Wei S, Cai X, Huang J, Xu F, Liu X, Wang Q. Recombinant human BMP-2 for the treatment of open tibial fractures. Orthopedics. 2012;35:e847–54.
Nauth A, Ristiniemi J, McKee MD, Schemitsch EH. Bone morphogenetic proteins in open fractures: past, present, and future. Injury. 2009;40 Suppl 3:S27–31.
Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, Song F. Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review. Health Technol Assess. 2007;11:1–150, iii–iv.
Ronga M, Fagetti A, Canton G, Paiusco E, Surace MF, Cherubino P. Clinical applications of growth factors in bone injuries: experience with BMPs. Injury. 2013;44 Suppl 1:S34–9.
Garrison KR, Shemilt I, Donell S, Ryder JJ, Mugford M, Harvey I, Song F, Alt V. Bone morphogenetic protein (BMP) for fracture healing in adults. Cochrane Database Syst Rev. 2010:CD006950.
Calori GM, D’Avino M, Tagliabue L, Albisetti W, d’Imporzano M, Peretti G. An ongoing research for evaluation of treatment with BMPs or AGFs in long bone non-union: protocol description and preliminary results. Injury. 2006;37 Suppl 3:S43–50.
Kanakaris NK, Lasanianos N, Calori GM, Verdonk R, Blokhuis TJ, Cherubino P, De Biase P, Giannoudis PV. Application of bone morphogenetic proteins to femoral non-unions: a 4-year multicentre experience. Injury. 2009;40 Suppl 3:S54–61.
Giannoudis PV, Kanakaris NK, Dimitriou R, Gill I, Kolimarala V, Montgomery RJ. The synergistic effect of autograft and BMP-7 in the treatment of atrophic nonunions. Clin Orthop Relat Res. 2009;467:3239–48.
Kanakaris NK, Calori GM, Verdonk R, Burssens P, De Biase P, Capanna R, Vangosa LB, Cherubino P, Baldo F, Ristiniemi J, Kontakis G, Giannoudis PV. Application of BMP-7 to tibial non-unions: a 3-year multicenter experience. Injury. 2008;39 Suppl 2:S83–90.
Bordei P. Locally applied platelet-derived growth factor accelerates fracture healing. J Bone Joint Surg Br. 2011;93:1653–9.
Graham S, Leonidou A, Lester M, Heliotis M, Mantalaris A, Tsiridis E. Investigating the role of PDGF as a potential drug therapy in bone formation and fracture healing. Expert Opin Investig Drugs. 2009;18:1633–54.
Moore YR, Dickinson DP, Wikesjo UM. Growth/differentiation factor-5: a candidate therapeutic agent for periodontal regeneration? A review of pre-clinical data. J Clin Periodontol. 2010;37:288–98.
Myers TJ, Yan Y, Granero-Molto F, Weis JA, Longobardi L, Li T, Li Y, Contaldo C, Ozkan H, Spagnoli A. Systemically delivered insulin-like growth factor-I enhances mesenchymal stem cell-dependent fracture healing. Growth Factors. 2012;30:230–41.
Granero-Molto F, Myers TJ, Weis JA, Longobardi L, Li T, Yan Y, Case N, Rubin J, Spagnoli A. Mesenchymal stem cells expressing insulin-like growth factor-I (MSCIGF) promote fracture healing and restore new bone formation in Irs1 knockout mice: analyses of MSCIGF autocrine and paracrine regenerative effects. Stem Cells. 2011;29:1537–48.
Tran GT, Pagkalos J, Tsiridis E, Narvani AA, Heliotis M, Mantalaris A, Tsiridis E. Growth hormone: does it have a therapeutic role in fracture healing? Expert Opin Investig Drugs. 2009;18:887–911.
Chen L, Yang X, Huang G, Song D, Ye XS, Xu H, Li W. Platelet-rich plasma promotes healing of osteoporotic fractures. Orthopedics. 2013;36:e687–94.
Guzel Y, Karalezli N, Bilge O, Kacira BK, Esen H, Karadag H, Toker S, Göncü RG, Doral MN. The biomechanical and histological effects of platelet-rich plasma on fracture healing. Knee Surg Sports Traumatol Arthrosc. 2013 [Epub ahead of print].
Malhotra A, Pelletier MH, Yu Y, Walsh WR. Can platelet-rich plasma (PRP) improve bone healing? A comparison between the theory and experimental outcomes. Arch Orthop Trauma Surg. 2013;133:153–65.
Giannoudis PV, Jones E, Einhorn TA. Fracture healing and bone repair. Injury. 2011;42:549–50.
Sen MK, Miclau T. Autologous iliac crest bone graft: should it still be the gold standard for treating nonunions? Injury. 2007;38 Suppl 1:S75–80.
Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury. 2011;42 Suppl 2:S3–15.
Carulli C, Matassi F, Civinini R, Innocenti M. Tissue engineering applications in the management of bone loss. Clin Cases Miner Bone Metab. 2013;10:22–5.
Asti A, Gastaldi G, Dorati R, Saino E, Conti B, Visai L, Benazzo F. Stem cells grown in osteogenic medium on PLGA, PLGA/HA, and titanium scaffolds for surgical applications. Bioinorg Chem Appl. 2010;2010:831031.
Gastaldi G, Asti A, Scaffino MF, Visai L, Saino E, Cometa AM, Benazzo F. Human adipose-derived stem cells (hASCs) proliferate and differentiate in osteoblast-like cells on trabecular titanium scaffolds. J Biomed Mater Res A. 2010;94:790–9.
Street J, Winter D, Wang JH, Wakai A, McGuinness A, Redmond HP. Is human fracture hematoma inherently angiogenic? Clin Orthop Relat Res. 2000;378:224–37.
Clarkin CE, Gerstenfeld LC. VEGF and bone cell signalling: an essential vessel for communication? Cell Biochem Funct. 2013;31:1–11.
Street J, Bao M, deGuzman L, Bunting S, Peale Jr FV, Ferrara N, Steinmetz H, Hoeffel J, Cleland JL, Daugherty A, van Bruggen N, Redmond HP, Carano RA, Filvaroff EH. Vascular endothelial growth factor stimulates bone repair by promoting angiogenesis and bone turnover. Proc Natl Acad Sci USA. 2002;99:9656–61.
Ogilvie CM, Lu C, Marcucio R, Lee M, Thompson Z, Hu D, Helms JA, Miclau T. Vascular endothelial growth factor improves bone repair in a murine nonunion model. Iowa Orthop J. 2012;32:90–4.
Ozturk BY, Inci I, Egri S, Ozturk AM, Yetkin H, Goktas G, Elmas C, Piskin E, Erdogan D. The treatment of segmental bone defects in rabbit tibiae with vascular endothelial growth factor (VEGF)-loaded gelatin/hydroxyapatite “cryogel” scaffold. Eur J Orthop Surg Traumatol. 2013;23:767–74.
Willems WF, Larsen M, Friedrich PF, Shogren KL, Bishop AT. Induction of angiogenesis and osteogenesis in surgically revascularized frozen bone allografts by sustained delivery of FGF-2 and VEGF. J Orthop Res. 2012;30:1556–62.
Dimitriou R, Giannoudis PV. The genetic profile of bone repair. Clin Cases Miner Bone Metab. 2013;10:19–21.
Dimitriou R, Kanakaris N, Soucacos PN, Giannoudis PV. Genetic predisposition to non-union: evidence today. Injury. 2013;44 Suppl 1:S50–3.
Dimitriou R, Carr IM, West RM, Markham AF, Giannoudis PV. Genetic predisposition to fracture non-union: a case control study of a preliminary single nucleotide polymorphisms analysis of the BMP pathway. BMC Musculoskelet Disord. 2011;12:44.
Feichtinger GA, Hofmann AT, Slezak P, Schuetzenberger S, Kaipel M, Schwartz E, Neef A, Nomikou N, Nau T, van Griensven M, McHale AP, Redl H. Sonoporation increases therapeutic efficacy of inducible and constitutive BMP2/7 in vivo gene delivery. Hum Gene Ther Methods. 2014; 25(1):57–71.
Han D, Li J. Repair of bone defect by using vascular bundle implantation combined with Runx II gene-transfected adipose-derived stem cells and a biodegradable matrix. Cell Tissue Res. 2013;352:561–71.
Giannoudis PV, Einhorn TA, Schmidmaier G, Marsh D. The diamond concept – open questions. Injury. 2008;39 Suppl 2:S5–8.
Calori GM, Giannoudis PV. Enhancement of fracture healing with the diamond concept: the role of the biological chamber. Injury. 2011;42:1191–3.
Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J. Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthop Res. 2004;22:73–9.
Masquelet AC, Fitoussi F, Begue T, Muller GP. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet. 2000;45:346–53.
Calori GM, Phillips M, Jeetle S, Tagliabue L, Giannoudis PV. Classification of non-union: need for a new scoring system? Injury. 2008;39 Suppl 2:S59–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 EFORT
About this chapter
Cite this chapter
Giannoudis, P.V., Panteli, M., Calori, G.M. (2014). Bone Healing: The Diamond Concept. In: Bentley, G. (eds) European Instructional Lectures. European Instructional Lectures, vol 14. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-54030-1_1
Download citation
DOI: https://doi.org/10.1007/978-3-642-54030-1_1
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-54029-5
Online ISBN: 978-3-642-54030-1
eBook Packages: MedicineMedicine (R0)