Abstract
Hemoglobin (Hb)-based oxygen (O2) carriers (HBOCs) are continuously being optimized as red blood cell (RBC) substitutes in order to overcome the well-known side-effects that are associated with transfusion of cell-free Hb (Alayash 1999, 2004). These side-effects include vasoconstriction, systemic hypertension and oxidative tissue toxicity (Alayash 1999, 2004). It is hypothesized that these side-effects are due to HBOC extravasation into the tissue space and the NO scavenging ability of cell-free Hb (Suaudeau et al. 1979; Nakai et al. 1998; Dull et al. 2004; Liu et al. 1998; Liao et al. 1999). Polymerized HBOCs (PolyHbs) were thus engineered with molecular sizes larger than that of cell-free Hb, with the goal of reducing extravasation of the HBOC from the vascular space into the tissue space (Alayash 2004; Palmer 2006). This approach should reduce the proximity of the HBOC to the endothelium, which in turn should reduce/eliminate the aforementioned side-effects (Alayash 2004; Palmer 2006). In order to address this need for large sized HBOCs compared to cell-free Hb, the following commercial PolyHbs were initially developed: Oxyglobin® (OPK Biotech LLC, Cambridge, MA), Hemopure® (OPK Biotech LLC, Cambridge, MA), PolyHeme® (Northfield Laboratories Inc., Evanston, IL) and Hemolink™ (Hemosol Inc., Toronto, Canada) (OPK Biotech 2012; Rentko et al. 2006; Day 2003; Adamson and Moore 1998). However, these commercial products still elicited the aforementioned side-effects and are coincidentally close together in molecular weight (MW) (Rentko et al. 2006; Day 2003; Adamson and Moore 1998; Tsai et al. 2006; Butt et al. 2010, 2011; Kasper et al. 1996; LaMuraglia et al. 2000; Jahr et al. 2008; Freilich et al. 2009; Yu et al. 2010; Handrigan et al. 2005; Cheng et al. 2004; Greenburg and Kim 2004; Hill et al. 2002; Lieberthal et al. 1999). In the case of Oxyglobin®, its’ side-effects were directly attributed to PolyHb extravasation from the blood vessel lumen into the tissue space Butt et al. (2010; 2011). Therefore, the ultrahigh MW HBOC Oxyvita™ (OXYVITA Inc., New Windsor, NY) was developed, which did not extravasate and induce significant vasoconstriction or hypertension (OXYVITA Inc. 2012; Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009). However, Oxyvita® has a high O2 affinity so it is unclear how well it will deliver O2 in vivo, despite its lack of vascular side-effects (Matheson et al. 2002; Jia and Alayash 2009). It is interesting to note that these commercial PolyHbs differ in MW by several orders of magnitude, and until recently there has been no systematic study of PolyHb MW on its’ in vivo safety profile (Rentko et al. 2006; Day 2003; Adamson and Moore 1998; Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009). To address this deficit in the literature, recent studies have shed light on the relationship between PolyHb molecular size and its’ in vivo safety profile (Cabrales et al. 2009; Cabrales et al. 2010; Baek et al. 2012). These studies demonstrate that increasing the molecular size of tense (T)-state bovine PolyHb reduces vasoconstriction, systemic hypertension, and oxidative tissue toxicity (Cabrales et al. 2009, 2010; Baek et al. 2012). Therefore, it is expected that further work in this area will lead to the optimization of PolyHb size in order to improve its in vivo safety profile for eventual human use.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Negative Side-Effects of Early Generation HBOCs
1.1 Cell-Free Hb
Hb was one of the first HBOCs to be evaluated as a RBC substitute (Savitsky et al. 1978). Unfortunately, Hb is able to extravasate through endothelial cell–cell junctions and scavenge NO several orders of magnitude more than RBCs (Suaudeau et al. 1979; Nakai et al. 1998; Dull et al. 2004; Liu et al. 1998; Liao et al. 1999). This is attributed to the smaller molecular dimensions of cell-free Hb compared to the RBC, which allows it to extravasate through the endothelial cell–cell junctions in capillaries into the surrounding tissue space (Suaudeau et al. 1979; Nakai et al. 1998; Dull et al. 2004). Consequently, vasoconstriction (i.e. reduction in blood vessel diameter) ensues, due to scavenging of the gaseous signaling molecule nitric oxide (NO) by the extravasated cell-free Hb (Vogel et al. 1986; Kavdia et al. 2002). Vasoconstriction at the microcirculatory level then leads to systemic hypertension, or high blood pressure (Doherty et al. 1998). In a human clinical trial, human Hb (HbA) induced mild hypertension in patients (Savitsky et al. 1978). HbA has also been shown to elevate the mean arterial blood pressure in hemorrhaged pigs and rats (Hess et al. 1993; Thompson et al. 1994). Therefore in light of these vascular side-effects, Hb is not used as a RBC substitute. Table 37.1 lists the biochemical and biophysical properties of Hb and various HBOCs.
In addition to its’ vascular side-effects, cell-free Hb can also elicit tissue toxicity due to its ability to induce oxidative stress. In the blood stream, tetrameric Hb easily dissociates into two αβ dimers (Alayash 1999; Bunn et al. 1969). The ferrous heme iron of the αβ dimer autoxidizes to the ferric or methemoglobin (metHb) form at a higher rate than the ferrous heme of tetrameric Hb (Zhang et al. 1991; D’Agnillo 2006). MetHb formation via autoxidation produces the reactive oxygen species (ROS) superoxide anion and indirectly hydrogen peroxide (H2O2) (D’Agnillo 2006; Misra and Fridovich 1972). Hence, the ROS hydroxyl radical can be generated by the reaction of superoxide with H2O2, and this is catalyzed by iron released from degraded heme (D’Agnillo 2006; Graf et al. 1984). Hence, Hb oxidation drives the production of ROS (D’Agnillo 2006; Misra and Fridovich 1972; Graf et al. 1984). Unfortunately, in vivo exposure to hydroxyl radicals has been linked to renal failure and apoptosis of vascular cells (Walker and Shah 1988; Shah and Walker 1988; Li et al. 1997). To compound matters further, the small size of αβ dimers also facilitates their filtration through the kidneys, and thus increases the opportunity for tissue exposure to ROS (Bunn et al. 1969). In clinical human trials, cell-free HbA infusion caused noticeable hemoglobinuria, indicative of HbA clearance through the kidneys (Savitsky et al. 1978). The highly reactive species ferryl Hb can also be formed from further reactions of Hb with H2O2 (D’Agnillo 2006; Giulivi and Davies 1990; Kanner et al. 1988). Ferrous Hb can be oxidized to ferric Hb via H2O2 exposure, and ferryl Hb is formed as an intermediate during this reaction (D’Agnillo 2006; Giulivi and Davies 1990). MetHb itself can also be converted to ferryl Hb in the presence of H2O2 (D’Agnillo 2006; Kanner et al. 1988). Ferryl Hb can elicit inflammation of vascular endothelial cells (Silva et al. 2009). Overall, oxidative stress facilitated by Hb oxidation products is a problem many HBOCs face and aim to prevent.
1.2 Recombinant HbA 1.1 (rHb 1.1)
Therefore in order to reduce renal filtration of αβ dimers, recombinant HbA (rHb 1.1) was developed by Somatogen Inc. (Boulder, CO) (Looker et al. 1992). Mutations to the native structure of HbA include an oxygen affinity lowering asparagine to lysine mutation at the β-108 position, and the insertion of a glycerin residue which covalently links the neighboring α chains together (Looker et al. 1992; Moo-Penn et al. 1978). Linking the α globin subunits together stabilized the structure of rHb 1.1 and inhibited dissociation of the tetramer into αβ dimers (Looker et al. 1992). Several clinical human trials demonstrated that prevention of rHb 1.1 dissociation into αβ dimers led to reduced oxidative stress and diminished renal toxicity (Viele et al. 1997; Hayes et al. 2001). Unfortunately, rHb 1.1 also elicited noticeable levels of hypertension in surgery patients (Hayes et al. 2001). In another clinical trial, rHb 1.1 caused lower esophageal sphincter tension in humans (Murray et al. 1995). It was hypothesized that the mechanism of this inhibition is linked to NO scavenging by rHb 1.1 (Murray et al. 1995). Therefore, although rHb 1.1 exhibited reduced oxidative stress and renal toxicity, it still exhibited undesirable vascular side-effects (Viele et al. 1997; Hayes et al. 2001; Murray et al. 1995). In light of these side-effects and after acquiring Somatogen Inc. (Boulder, CO), Baxter International Inc. (Deerfield, IL) subsequently engineered rHb 3011 with a reduced dioxygenation rate constant in order to eliminate vasoconstriction and systemic hypertension (Olson et al. 2004; Varnado et al. 2012; Baxter 2012). However, it has recently been shown that rHb 3011 autoxidizes at a greater rate in vitro compared to the earlier generation rHb 0.1, which could lead to increased oxidative stress on the vasculature (Varnado et al. 2012).
1.3 Diaspirin Cross-Linked HbA (DCLHb)
Site specifically cross-linking HbA represents another strategy to eliminate HbA dissociation into αβ dimers. Hence, diaspirin cross-linked HbA (DCLHb) was developed by the United States (US) Army and commercially as HemAssit™ by Baxter International Inc. (Deerfield, IL) (Baxter 2012; Winslow 2003). DCLHb is composed of HbA, in which the neighboring α globin chains are covalently cross-linked using bis-(3,5-dibromosalicyl) fumarate (Chatterjee et al. 1986). DCLHb consists of 96 % tetrameric HbA and 2–3 % of HbA tetrameric dimers (Yu et al. 1997). In Phase III clinical trials, DCLHb induced hypertension in stroke patients (Saxena et al. 1999). Elevated blood pressure levels were also reported when DCLHb was infused in patients after cardiac surgery (Lamy et al. 2000). When administered to traumatic hemorrhagic shock patients, DCLHb recipients died more often than saline recipients (Sloan et al. 1999). Despite stabilization of DCLHb’s tetrameric structure via α globin chain cross-links, DCLHb readily oxidized in vitro when H2O2 was present (Cashon and Alayash 1995). Therefore, DCLHb exhibited many of the side-effects associated with transfusion of cell-free Hb and is no longer being pursued by Baxter International Inc. (Winslow 2003; Saxena et al. 1999; Lamy et al. 2000; Sloan et al. 1999; Cashon and Alayash 1995).
2 Hb Polymerization as a Strategy to Mitigate Vascular Side-Effects
In order to prevent many of the side-effects commonly associated with early commercial HBOCs, the focus has turned to developing HBOCs which are too large to pass through the endothelial cell–cell junctions of blood vessels (Alayash 2004; Palmer 2006). The rationale behind this approach centers on reducing HBOC extravasation into the tissue space so that the HBOC is not in close proximity to the endothelium (Alayash 2004; Palmer 2006). This should lead to less scavenging of endothelial-derived NO by the HBOC, reduced vasoconstriction and hypertension, as well as reduced oxidative tissue toxicity (Alayash 2004; Palmer 2006). In light of this approach, several companies have developed polymerized Hb (PolyHb) solutions as potential RBC substitutes.
2.1 Oxyglobin®
OPK Biotech LLC (Cambridge, MA) developed two HBOCs, which have gone through extensive studies, namely Oxyglobin® and Hemopure® (OPK Biotech 2012). Both Oxyglobin® and Hemopure® consist of glutaraldehyde polymerized bovine Hb (PolybHb) (OPK Biotech 2012). Glutaraldehyde forms intramolecular cross-links within the Hb tetramer and intermolecular cross-links between neighboring Hb tetramers (Chang 1998). Oxyglobin® is composed of PolybHb with an average MW of 200 kDa (Rentko et al. 2006; Day 2003). It is approved for veterinary use in the US (Day 2003). However, Oxyglobin® has been shown to elicit both vasoconstriction and hypertension in vivo (Tsai et al. 2006). Because of its availability, multiple studies have explored the toxicity of Oxyglobin® Butt et al. (2010, 2011). The oxidative stress caused by Oxyglobin® damaged blood brain barrier endothelial cells and elicited cellular apoptosis in vivo (Butt et al. 2011). Iron was found to be deposited in endothelial cells and neurons associated with the blood brain barrier after administration of Oxyglobin® (Butt et al. 2011) In addition, Oxyglobin® administered to guinea pigs and rats has been shown to facilitate iron deposition in renal tissues (Butt et al. 2010). These results indicate extravasation of Oxyglobin® through endothelial cell–cell junctions and its deposition in the tissue space Butt et al. (2010, 2011).
2.2 Hemopure®
Hemopure® is a glutaraldehyde PolybHb solution with an average MW of 250 kDa, which was also developed by OPK Biotech LLC (Cambridge, MA) (OPK Biotech 2012; Rentko et al. 2006; Day 2003). Hemopure® is composed of 2 % unpolymerized bovine Hb (bHb) compared to Oxyglobin®, which is composed of 31 % unpolymerized bHb (Rice et al. 2008). A study of resuscitated hemorrhagic shock-induced swine reported that Hemopure® elevated blood pressure less than Oxyglobin®, and this was attributed to the reduced amount of unpolymerized bHb present in Hemopure® compared to Oxyglobin® (Rice et al. 2008). When administered before, during, and after elective aortic surgery, Hemopure® produced hypertension in patients (Kasper et al. 1996; LaMuraglia et al. 2000). Data from another Hemopure® clinical trial highlighted a possible vulnerability in elderly orthopedic surgery patients to negative vascular side-effects (Jahr et al. 2008; Freilich et al. 2009). These findings indicate that despite having less unpolymerized bHb than Oxyglobin®, Hemopure® still presents risks to the vasculature in clinical settings (Kasper et al. 1996; LaMuraglia et al. 2000; Jahr et al. 2008; Freilich et al. 2009; Rice et al. 2008).
2.3 Polyheme®
Northfield Laboratories Inc. (Evanston, IL) developed a glutaraldehyde polymerized pyridoxal phosphate cross-linked HbA product known as PolyHeme® (Day 2003; Sehgal et al. 1984). PolyHeme® has an average MW of 150 kDa (Day 2003). The pyridoxilated HbA reduces the oxygen affinity of PolyHeme® Sehgal et al. (1981, 1984). In clinical trials, PolyHeme® was administered to trauma, surgery, and hemorrhagic shock patients, and did not increase blood pressure to unsafe levels (Gould et al. 1998, 2002; Moore et al. 2009). Unfortunately, PolyHeme® has been linked to negative side-effects in various animal studies (Yu et al. 2010; Handrigan et al. 2005). A recent study showed that PolyHeme® induced vasoconstriction in lambs (Yu et al. 2010). PolyHeme® administration also produced organ failure and death in hemorrhaged rats (Handrigan et al. 2005). Negative vascular responses are not surprising considering that Oxyglobin® and Hemopure®, both two larger sized glutaraldehyde PolybHbs, displayed similar negative side-effects in vivo (Rentko et al. 2006; Day 2003; Tsai et al. 2006; Kasper et al. 1996; LaMuraglia et al. 2000; Jahr et al. 2008; Freilich et al. 2009; Yu et al. 2010; Handrigan et al. 2005). PolyHeme® production was shut down after ethical questions were raised over the consent requirements of the final clinical trial (Moore et al. 2009; Chen et al. 2009; Kipnis et al. 2006).
2.4 Hemolink™
Hemosol Inc. (Toronto, Canada) developed the O-raffinose cross-linked HbA product Hemolink™ (Day 2003; Adamson and Moore 1998). Hemolink™ has a wide range of MWs which consists of less than or equal to 5 % 32 kDa, 33 % 64 kDa, 63 % 128–600 kDa, and less than or equal to 3 % greater than 600 kDa species (Adamson and Moore 1998). In Phase II and Phase III clinical trials, Hemolink™ administration lead to hypertension in coronary artery surgery patients (Cheng et al. 2004; Greenburg and Kim 2004; Hill et al. 2002). Hemolink™ exhibited diminished renal toxicity in vivo and NO reactions in vitro compared to HbA (Lieberthal et al. 1999). In this study, Hemolink™ also induced hypertension in rats (Lieberthal et al. 1999). Thus despite HemolinkTM having a low affinity for NO in vitro, there was still evidence of systemic hypertension (Lieberthal et al. 1999). Hemolink™ production was discontinued due to negative side-effects observed in clinical trials (Chen et al. 2009).
2.5 OxyVita™
Of all the aforementioned PolyHbs which have reported average MWs, all of them ranged between 150 and 250 kDa (Rentko et al. 2006; Day 2003). All four of the PolyHbs exhibited some form of vasoconstriction, hypertension, and/or oxidative stress (Tsai et al. 2006; Butt et al. 2010, 2011; Kasper et al. 1996; LaMuraglia et al. 2000; Jahr et al. 2008; Freilich et al. 2009; Yu et al. 2010; Handrigan et al. 2005; Cheng et al. 2004; Greenburg and Kim 2004; Hill et al. 2002; Lieberthal et al. 1999). The presence of vasoconstriction and systemic hypertension make it reasonable to assume that these commercial HBOCs are still able to extravasate through the endothelium and scavenge NO despite their larger size compared to HbA (Rentko et al. 2006; Day 2003; Adamson and Moore 1998; Tsai et al. 2006; Kasper et al. 1996; LaMuraglia et al. 2000; Jahr et al. 2008; Freilich et al. 2009; Yu et al. 2010; Handrigan et al. 2005; Cheng et al. 2004; Greenburg and Kim 2004; Hill et al. 2002; Lieberthal et al. 1999). Therefore, it is possible that since Oxyglobin® induces oxidative stress, similarly sized HBOCs may possess similar potential for oxidation Butt et al. (2010, 2011). To avoid vasoconstriction, hypertension, and oxidative stress, some groups have developed ultrahigh MW PolyHbs.
OXYVITA Inc. (New Windsor, NY) developed a high MW RBC substitute known as OxyVita™ (OXYVITA Inc. 2012; Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009). Also known as zero-link polymerized bHb, the ultrahigh MW of Oxyvita™ has been reported to be 25, 33 and 42 MDa in separate studies (Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009). OxyVita™ is synthesized by cross-linking the β globin chains of bHb with bis(3,5-dibromosalicy)-adipoate (Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009; Kwansa et al. 2000). 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide is then used to polymerize the bHb tetramers (Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009). OxyVita™ has been shown to produce low levels of vasoconstriction, which did not lead to hypertension in animal studies (Matheson et al. 2002; Bucci et al. 2007). These benefits have been attributed to the large size of the PolybHb, which prevents its extravasation into the tissue space and thus its inability to scavenge NO (Matheson et al. 2002; Bucci et al. 2007). Therefore, the zero-link cross-linking process appears to be able to prevent vascular side-effects common to many commercial HBOCs (Matheson et al. 2002; Bucci et al. 2007). Despite this major advantage, OxyVita™ possesses a high oxygen affinity (Matheson et al. 2002; Jia and Alayash 2009). The high oxygen affinity makes it unclear how well OxyVitaTM will deliver oxygen under physiological conditions compared to other commercial HBOCs (Matheson et al. 2002; Jia and Alayash 2009). OXYVITA Inc. is presently raising resources to pursue further trials of OxyVita™ (OXYVITA Inc. 2012).
2.6 Overview of Commercial PolyHbs
Many of the commercial PolyHbs discussed above failed Phase III clinical trials, before their potential for negative side-effects were fully understood (Jahr et al. 2008; Freilich et al. 2009; Moore et al. 2009; Greenburg and Kim 2004; Chen et al. 2009). It is reasonable to expect that if a systematic study of these PolyHbs had been performed they would not have progressed as far without serious design alterations. Investigations into the gaseous ligand binding/release kinetics, ability to induce vasoconstriction, systemic hypertension, and oxidative stress-inducing potential of these PolyHbs could have foreshadowed the side-effects observed during Phase III clinical trials (Jahr et al. 2008; Freilich et al. 2009; Greenburg and Kim 2004). In the future, PolyHb development should include systematic preliminary studies to prevent a reoccurrence of these common side-effects. Therefore, the wide difference in MW between the low MW PolyHbs Oxyglobin®, Hemopure®, PolyHeme®, Hemolink™ and the ultrahigh MW PolyHb OxyVita™ highlight the need for a systematic study to investigate the effects of PolyHb MW on its’ safety profile (i.e. ability to induce vasoconstriction, systemic hypertension and oxidative toxicity) (Rentko et al. 2006; Day 2003; Adamson and Moore 1998; Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009).
3 Systematic Study of PolyHb MW on Safety Profile
In a series of publications, Palmer’s group reported the results of a systematic study investigating the biophysical properties and in vivo responses of variable MW glutaraldehyde PolybHbs (Cabrales et al. 2009; Cabrales et al. 2010; Baek et al. 2012; Palmer et al. 2009a; Buehler et al. 2010; Zhou et al. 2011).
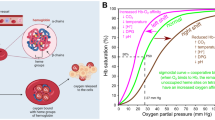
Palmer’s group first demonstrated that the quaternary state of bHb could be used to control the oxygen affinity of the resultant PolybHb solution Palmer et al. (2009a). This work took advantage of the fact that Hb can be held in either the tense (T) or relaxed (R) quaternary state by simply fully deoxygenating or fully oxygenating the bHb solution, respectively (Palmer et al. 2009a). Hence, T-state and R-state PolybHbs were synthesized by polymerizing T-state and R-state bHb with glutaraldehyde, respectively (Palmer et al. 2009a). In this work, T- and R-state PolybHbs were synthesized at the following glutaraldehyde to bHb molar ratios (i.e. cross-link densities): 10:1, 20:1, 30:1 and 40:1 (Palmer et al. 2009a). It was observed that T-state PolybHb displayed a higher P50 compared to R-state PolybHb (Palmer et al. 2009a). In addition, the cooperativity coefficient of both T- and R-state PolybHb decreased with increasing cross-link density (Palmer et al. 2009a). This result is consistent with increasing cross-linking density, thereby reducing the mobility of the globin chains in the Hb tetramer (Palmer et al. 2009a).
A subsequent study evaluated the effect of T-state PolybHb MW on the extent of vasoconstriction and systemic hypertension (Cabrales et al. 2009). In this study, T-state PolybHbs with glutaraldehyde to bHb molar ratios of 20:1, 30:1, 40:1, and 50:1 were synthesized in the lab (Cabrales et al. 2009). Ultrafiltration was then used to fractionate each PolybHb solution into a fraction greater than 500 kDa in MW and a fraction less than 500 kDa in MW (Cabrales et al. 2009). All of the PolybHb solutions with MW less than 500 kDa were shown to induce vasoconstriction and hypertension in top-loaded hamsters outfitted with the window chamber, and this was likely due to extravasation of low MW PolyHb through the endothelium and subsequent PolybHb scavenging of endothelium-derived NO (Cabrales et al. 2009). Negative vascular effects were less prevalent for the PolybHbs with MW greater than 500 kDa. (Cabrales et al. 2009). Most notably, no vasoconstriction and only minor hypertension were present with the 40:1 and 50:1 PolybHbs (Cabrales et al. 2009). The diminished vascular side-effects exhibited by the PolybHbs greater than 500 kDa were similar to those observed for the ultrahigh MW PolybHb OxyVita™ (Matheson et al. 2002; Bucci et al. 2007; Jia and Alayash 2009; Cabrales et al. 2009). An important distinction between OxyVita™ and the high MW T-state PolybHbs is the high P50 of the T-state PolybHbs and the low P50 of OxyVita™ (Matheson et al. 2002; Jia and Alayash 2009; Cabrales et al. 2009). Previous work has shown that high P50 HBOCs deliver oxygen to tissues more readily versus low P50 HBOCs (Sakai et al. 2005).
Therefore, the ability of T-state and R-state PolybHbs to deliver O2 was evaluated in vivo to better understand the effect of PolybHb oxygen affinity in influencing tissue oxygenation (Cabrales et al. 2010). Hence, 40:1 R-state and 50:1 T-state PolybHbs were used in this study, and all HBOCs possessed MWs greater than 500 kDa (Cabrales et al. 2010). It was observed that T-state PolybHb delivered more O2 to tissues in the hamster chamber window model versus R-state PolybHb (Cabrales et al. 2010). As expected, this was largely attributed to the high oxygen affinity of R-state PolybHb (Cabrales et al. 2010). Thus the ability of T-state PolybHbs to adequately transport oxygen in vivo was confirmed in this study (Cabrales et al. 2010).
A thorough investigation into the gaseous ligand binding/release kinetics and autoxidation kinetics of high MW T- and R-state PolybHbs was then conducted to better understand their in vivo oxidation potential and pharmacokinetics (Buehler et al. 2010). Stop flow kinetic measurements were used to determine the O2 dissociation, CO association, and NO dioxygenation rate constants of 40:1 R-state and 50:1 T-state PolybHbs, all PolybHbs had MWs > 500 kDa (Buehler et al. 2010). The O2 dissociation rate constant increased for 50:1 T-State PolybHb and decreased for 40:1 R-state PolybHb compared to bHb, indicating that O2 is released faster from the 50:1 T-state PolybHb compared to 40:1 R-state PolybHb (Buehler et al. 2010). The reported value of the CO association rate constant of 50:1 T-state PolybHb was marginally lower than that of bHb, whereas this rate constant increased for 40:1 R-state PolybHb (Buehler et al. 2010). The NO dioxygenation rate constants of both the 50:1 T-state and 40:1 R-state PolybHbs were shown to be similar to that of bHb (Buehler et al. 2010). This indicates that both PolybHbs and cell-free bHb interact similarly with NO (Buehler et al. 2010). Counter intuitively, an earlier study observed that T-state PolybHbs do not produce vasoconstriction and hypertension, which have been linked to NO scavenging (Cabrales et al. 2009). Thus since PolybHbs are capable of interacting with NO, it is hypothesized that their large size (compared to the size of the endothelial cell–cell junctions lining the blood vessel wall) prevents them from extravasating through the endothelium and scavenging NO (Cabrales et al. 2009; Buehler et al. 2010). In vivo, 50:1 T-state PolybHb underwent autoxidation at a significantly lower rate and remained in circulation longer than 40:1 R-state PolybHb (Buehler et al. 2010). This result is important, since the reduced rate of heme oxidation prolongs T-state PolybHb oxygen delivery in vivo (Buehler et al. 2010). Therefore, high MW T-state PolybHbs seem to be an ideal HBOC due to their lack of vasoconstriction and hypertension, increased circulatory half-life, and reduced in vivo oxidation compared to R-state PolybHbs (Buehler et al. 2010).
An evaluation of T- and R-state glutaraldehyde polymerized HbA (PolyhHb) demonstrated that PolybHbs and PolyhHbs share many of the same biophysical characteristics (Buehler et al. 2010; Zhang et al. 2011). In this study, 50:1 and 40:1 T-state PolyhHbs and 30:1 and 20:1 R-state PolyhHbs were synthesized with MWs > 500 kDa (Zhang et al. 2011). Both the P50 and oxygen dissociation rate constants of T-state PolyhHbs were higher than those of hHb and R-state PolyhHbs (Zhang et al. 2011). Thus the low oxygen affinity of T-state PolybHbs and high oxygen affinity of R-state PolybHbs are maintained in T- and R-state PolyhHbs, respectively (Buehler et al. 2010; Zhang et al. 2011). Polymerization decreased the CO association binding rate constant of T-state PolyhHbs, while this rate constant increased for R-state PolyhHbs (Zhang et al. 2011). This is similar to the trends observed in T- and R-state PolybHbs (Buehler et al. 2010; Zhang et al. 2011). T- and R-state PolyhHbs also maintained their ability to interact with NO similar to HbA, regardless of Hb quaternary state (Buehler et al. 2010; Zhang et al. 2011). In addition to these kinetic experiments, the ability of PolyhHbs to deliver O2 was simulated using a mathematical model of a hepatic hollow fiber bioreactor (Zhang et al. 2011). Modeling results indicated that T-state PolyhHbs were more effective at delivering oxygen to hepatocytes housed in the bioreactor compared to R-state PolyhHbs (Zhang et al. 2011). This study showed that PolyhHbs share many of the same biophysical characteristics as PolybHbs, and indicated that T-state PolyhHbs possess the best potential to serve as oxygen transporting RBC substitutes (Buehler et al. 2010; Zhang et al. 2011).
Another study evaluated the ability of PolybHbs to deliver oxygen using the same mathematical model of a hepatic hollow fiber bioreactor used to evaluate PolyhHbs (Zhou et al. 2011; Zhang et al. 2011). In this study, T- and R-state PolybHbs were synthesized at the following glutaraldehyde to bHb molar ratios: 10:1, 20:1, and 30:1, and previous results for 40:1 R-state and 50:1 T-state PolybHbs were incorporated in the hepatic hollow fiber model (Buehler et al. 2010; Zhou et al. 2011). The results of these simulations showed that all T-state PolybHbs were able to more efficiently deliver O2 to hepatocytes housed in the bioreactor compared to R-state PolybHbs, further solidifying the superior oxygenation potential of T-state PolybHbs as RBC substitutes (Zhou et al. 2011).
In order to evaluate the effect of PolybHb size on oxidative tissue toxicity, T-state PolybHbs were synthesized at the following glutaraldehyde to bHb molar ratios: 10:1, 20:1, 30:1 and 40:1 (Baek et al. 2012). Guinea pigs were then subjected to a 50 % blood for PolybHb solution exchange transfusion and the pharmacokinetics of PolybHb was evaluated along with iron deposition in the spleen, liver and kidneys (Baek et al. 2012). The results of this study showed that the 30:1 PolybHb elicited less in vivo oxidation in the blood compared to the 10:1, 20:1, and 40:1 PolybHbs, that was not a function of PolybHb size (Baek et al. 2012). However, iron deposition in the kidneys decreased as a function of increasing PolybHb size (Baek et al. 2012). Similarly, the extent of systemic hypertension decreased with increasing PolybHb size, while the circulatory half-life of PolybHb increased as a function of increasing PolybHb size until it reached a maximum for the 30:1 PolybHb (Baek et al. 2012). In light of these results, the 30:1 T-state PolybHb exhibited the best pharmacokinetics with the least iron deposition in the kidneys along with the absence of systemic hypertension upon transfusion (Baek et al. 2012). Additional studies will need to be performed to further assess the clinical safety of this material.
4 Conclusions
In summary, Palmer’s group has systematically investigated the biophysical properties, and in vivo responses upon transfusion of variable sized T- and R-state PolyHbs (Cabrales et al. 2009, 2010; Baek et al. 2012; Palmer et al. 2009a; Buehler et al. 2010; Zhou et al. 2011; Zhang et al. 2011). The results of these studies have identified high MW T-state PolyHbs as a low oxygen affinity HBOC, which does not elicit vasoconstriction, hypertension, or oxidative tissue toxicity (Cabrales et al. 2009, 2010; Baek et al. 2012). In addition, high MW T-state PolyHbs are able to deliver O2 in both in vitro and in vivo scenarios (Cabrales et al. 2010; Buehler et al. 2010; Zhou et al. 2011; Zhang et al. 2011). Therefore, these results set the stage for exploring the clinical potential of high MW T-state PolyHbs as RBC substitutes in transfusion medicine.
References
Adamson JG, Moore C (1998) Hemolink™, an o-raffinose crosslinked hemoglobin-based oxygen carrier. In: Chang TMS (ed) Blood substitutes: principles, methods, products, and clinical trials vol 2. Krager Landes Systems, Basel, Switzerland, pp 62–81
Alayash AI (1999) Hemoglobin-based blood substitutes: oxygen carriers, pressor agents, or oxidants? Nat Biotechnol 17(6):545–549. doi:10.1038/9849
Alayash AI (2004) Oxygen therapeutics: can we tame haemoglobin? Nat Rev Drug Discovery 3(2):152–159. doi:10.1038/nrd1307
Alayash AI, Summers AG, Wood F, Jia Y (2001) Effects of glutaraldehyde polymerization on oxygen transport and redox properties of bovine hemoglobin. Arch Biochem Biophys 391(2):225–234. doi:10.1006/abbi.2001.2426
Baek JH, Zhou Y, Harris DR, Schaer DJ, Palmer AF, Buehler PW (2012) Down selection of polymerized bovine hemoglobins for use as oxygen releasing therapeutics in a guinea pig model. Toxicol Sci: Official J Soc Toxicol 127(2):567–581. doi:10.1093/toxsci/kfs109
Baxter (2012) Baxter international Inc. http://www.baxter.com/index.html. Accessed 13 October 2012
Bucci E, Kwansa H, Koehler RC, Matheson B (2007) Development of zero-link polymers of hemoglobin, which do not extravasate and do not induce pressure increases upon infusion. Artif Cells Blood Substit Immobil Biotechnol 35(1):11–18. doi:10.1080/10731190600974277
Buehler PW, Boykins RA, Jia Y, Norris S, Freedberg DI, Alayash AI (2005) Structural and functional characterization of glutaraldehyde-polymerized bovine hemoglobin and its isolated fractions. Anal Chem 77(11):3466–3478. doi:10.1021/ac050064y
Buehler PW, Zhou Y, Cabrales P, Jia Y, Sun G, Harris DR, Tsai AG, Intaglietta M, Palmer AF (2010) Synthesis, biophysical properties and pharmacokinetics of ultrahigh molecular weight tense and relaxed state polymerized bovine hemoglobins. Biomaterials 31(13):3723–3735. doi:10.1016/j.biomaterials.2010.01.072
Bunn HF, Esham WT, Bull RW (1969) The renal handling of hemoglobin. I. Glomerular filtration. J Exp Med 129(5):909–923
Butt OI, Buehler PW, D’Agnillo F (2010) Differential induction of renal heme oxygenase and ferritin in ascorbate and nonascorbate producing species transfused with modified cell-free hemoglobin. Antioxid Redox Signal 12(2):199–208. doi:10.1089/ars.2009.2798
Butt OI, Buehler PW, D’Agnillo F (2011) Blood-brain barrier disruption and oxidative stress in guinea pig after systemic exposure to modified cell-free hemoglobin. Am J Pathol 178(3):1316–1328. doi:10.1016/j.ajpath.2010.12.006
Cabrales P, Sun G, Zhou Y, Harris DR, Tsai AG, Intaglietta M, Palmer AF (2009) Effects of the molecular mass of tense-state polymerized bovine hemoglobin on blood pressure and vasoconstriction. J Appl Physiol 107(5):1548–1558. doi:10.1152/japplphysiol.00622.2009
Cabrales P, Zhou Y, Harris DR, Palmer AF (2010) Tissue oxygenation after exchange transfusion with ultrahigh-molecular-weight tense- and relaxed-state polymerized bovine hemoglobins. Am J Physiol Heart Circulatory Physiol 298(3):H1062–H1071. doi:10.1152/ajpheart.01022.2009
Cashon RE, Alayash AI (1995) Reaction of human hemoglobin HbA0 and two cross-linked derivatives with hydrogen peroxide: differential behavior of the ferryl intermediate. Arch Biochem Biophys 316(1):461–469. doi:10.1006/abbi.1995.1061
Chang TM (1998) Modified hemoglobin-based blood substitutes: crosslinked, recombinant and encapsulated hemoglobin. Vox Sang 74(Suppl 2):233–241
Chatterjee R, Welty EV, Walder RY, Pruitt SL, Rogers PH, Arnone A, Walder JA (1986) Isolation and characterization of a new hemoglobin derivative cross-linked between the alpha chains (lysine 99 alpha 1—lysine 99 alpha 2). J Bio chem 261(21):9929–9937
Chen JY, Scerbo M, Kramer G (2009) A review of blood substitutes: examining the history, clinical trial results, and ethics of hemoglobin-based oxygen carriers. Clinics (Sao Paulo) 64(8):803–813. doi:10.1590/S1807-59322009000800016
Cheng DC, Mazer CD, Martineau R, Ralph-Edwards A, Karski J, Robblee J, Finegan B, Hall RI, Latimer R, Vuylsteke A (2004) A phase II dose-response study of hemoglobin raffimer (Hemolink) in elective coronary artery bypass surgery. J Thorac Cardiovasc Surg 127(1):79–86. doi:10.1016/j.jtcvs.2003.08.024
D’Agnillo F (2006) Pro-oxidant activity of hemoglobin and endothelial cytotoxicity. In: Winslow RM (ed) Blood substitutes vol 19. Elsevier Academic Press, Amsterdam, pp 206–216
Day TK (2003) Current development and use of hemoglobin-based oxygen-carrying (HBOC) solutions. J Vet Emerg Crit Care 13(2):77–93
Doherty DH, Doyle MP, Curry SR, Vali RJ, Fattor TJ, Olson JS, Lemon DD (1998) Rate of reaction with nitric oxide determines the hypertensive effect of cell-free hemoglobin. Nat Biotechnol 16(7):672–676. doi:10.1038/nbt0798-672
Doyle MP, Apostol I, Kerwin BA (1999) Glutaraldehyde modification of recombinant human hemoglobin alters its hemodynamic properties. J Biol chem 274(4):2583–2591
Dull RO, DeWitt BJ, Dinavahi R, Schwartz L, Hubert C, Pace N, Fronticelli C (2004) Quantitative assessment of hemoglobin-induced endothelial barrier dysfunction. J Appl Physiol 97(5):1930–1937. doi:10.1152/japplphysiol.00102.2004
Freilich D, Pearce LB, Pitman A, Greenburg G, Berzins M, Bebris L, Ahlers S, McCarron R (2009) HBOC-201 vasoactivity in a phase III clinical trial in orthopedic surgery subjects–extrapolation of potential risk for acute trauma trials. J Trauma 66(2):365–376. doi:10.1097/TA.0b013e3181820d5c
Gelderman MP, Yazer MH, Jia Y, Wood F, Alayash AI, Vostal JG (2010) Serial oxygen equilibrium and kinetic measurements during RBC storage. Transfus Med 20(5):341–345. doi:10.1111/j.1365-3148.2010.01016.x
Giulivi C, Davies KJ (1990) A novel antioxidant role for hemoglobin. The comproportionation of ferrylhemoglobin with oxyhemoglobin. J Biol chem 265(32):19453–19460
Gould SA, Moore EE, Hoyt DB, Burch JM, Haenel JB, Garcia J, DeWoskin R, Moss GS (1998) The first randomized trial of human polymerized hemoglobin as a blood substitute in acute trauma and emergent surgery. J Am Coll Surg 187(2):113−120. discussion 120−112
Gould SA, Moore EE, Hoyt DB, Ness PM, Norris EJ, Carson JL, Hides GA, Freeman IH, DeWoskin R, Moss GS (2002) The life-sustaining capacity of human polymerized hemoglobin when red cells might be unavailable. J Am Coll Surg 195(4):445−452. discussion 452−445
Graf E, Mahoney JR, Bryant RG, Eaton JW (1984) Iron-catalyzed hydroxyl radical formation. Stringent requirement for free iron coordination site. J Biol chem 259(6):3620–3624
Greenburg AG, Kim HW (2004) Use of an oxygen therapeutic as an adjunct to intraoperative autologous donation to reduce transfusion requirements in patients undergoing coronary artery bypass graft surgery. J Am Coll Surg 198(3):373–383. doi:10.1016/j.jamcollsurg.2003.11.020 discussion 384–375
Handrigan MT, Bentley TB, Oliver JD, Tabaku LS, Burge JR, Atkins JL (2005) Choice of fluid influences outcome in prolonged hypotensive resuscitation after hemorrhage in awake rats. Shock 23(4):337–343
Hayes JK, Stanley TH, Lind GH, East K, Smith B, Kessler K (2001) A double-blind study to evaluate the safety of recombinant human hemoglobin in surgical patients during general anesthesia. J Cardiothorac Vasc Anesth 15(5):593–602. doi:10.1053/jcan.2001.26538
Hess JR, MacDonald VW, Brinkley WW (1993) Systemic and pulmonary hypertension after resuscitation with cell-free hemoglobin. J Appl Physiol 74(4):1769–1778
Hill SE, Gottschalk LI, Grichnik K (2002) Safety and preliminary efficacy of hemoglobin raffimer for patients undergoing coronary artery bypass surgery. J Cardiothorac Vasc Anesth 16(6):695–702. doi:10.1053/jcan.2002.128416
Jahr JS, Mackenzie C, Pearce LB, Pitman A, Greenburg AG (2008) HBOC-201 as an alternative to blood transfusion: efficacy and safety evaluation in a multicenter phase III trial in elective orthopedic surgery. J Trauma 64(6):1484–1497. doi:10.1097/TA.0b013e318173a93f
Jahr JS, Weeks DL, Desai P, Lim JC, Butch AW, Gunther R, Driessen B (2008) Does OxyVita, a new-generation hemoglobin-based oxygen carrier, or oxyglobin acutely interfere with coagulation compared with normal saline or 6 % hetastarch? an ex vivo thromboelastography study. J Cardiothorac Vasc Anesth 22(1):34–39. doi:10.1053/j.jvca.2007.02.016
Jia Y, Alayash AI (2009) Effects of cross-linking and zero-link polymerization on oxygen transport and redox chemistry of bovine hemoglobin. Biochim Biophys Acta 1794(8):1234–1242. doi:10.1016/j.bbapap.2009.04.008
Jia Y, Ramasamy S, Wood F, Alayash AI, Rifkind JM (2004) Cross-linking with O-raffinose lowers oxygen affinity and stabilizes haemoglobin in a non-cooperative T-state conformation. Biochem J 384(Pt 2):367–375. doi:10.1042/BJ20040612
Kanner J, Harel S, Salan AM (1988) The generation of ferryl or hydroxyl radicals during interaction of hemeproteins with hydrogen peroxide. Basic Life Sci 49:145–148
Kasper SM, Walter M, Grune F, Bischoff A, Erasmi H, Buzello W (1996) Effects of a hemoglobin-based oxygen carrier (HBOC-201) on hemodynamics and oxygen transport in patients undergoing preoperative hemodilution for elective abdominal aortic surgery. Anesth Analg 83(5):921–927
Kavdia M, Tsoukias NM, Popel AS (2002) Model of nitric oxide diffusion in an arteriole: impact of hemoglobin-based blood substitutes. Am J Physiol Heart Circulatory Physiol 282(6):H2245–H2253. doi:10.1152/ajpheart.00972.2001
Kipnis K, King NM, Nelson RM (2006) Trials and errors: barriers to oversight of research conducted under the emergency research consent waiver. Irb 28(2):16–19
Kwansa HE, Young AD, Arosio D, Razynska A, Bucci E (2000) Adipyl crosslinked bovine hemoglobins as new models of allosteric systems. Proteins 39(2):166–169
LaMuraglia GM, O’Hara PJ, Baker WH, Naslund TC, Norris EJ, Li J, Vandermeersch E (2000) The reduction of the allogenic transfusion requirement in aortic surgery with a hemoglobin-based solution. J Vasc Surg 31(2):299–308
Lamy ML, Daily EK, Brichant JF, Larbuisson RP, Demeyere RH, Vandermeersch EA, Lehot JJ, Parsloe MR, Berridge JC, Sinclair CJ, Baron JF, Przybelski RJ (2000) Randomized trial of diaspirin cross-linked hemoglobin solution as an alternative to blood transfusion after cardiac surgery. the DCLHb Cardiac Surgery Trial Collaborative Group. Anesthesiology 92(3):646–656
Li PF, Dietz R, von Harsdorf R (1997) Reactive oxygen species induce apoptosis of vascular smooth muscle cell. FEBS Lett 404(2–3):249–252
Liao JC, Hein TW, Vaughn MW, Huang KT, Kuo L (1999) Intravascular flow decreases erythrocyte consumption of nitric oxide. Proc Natl Acad Sci U S A 96(15):8757–8761
Lieberthal W, Fuhro R, Freedman JE, Toolan G, Loscalzo J, Valeri CR (1999) O-raffinose cross-linking markedly reduces systemic and renal vasoconstrictor effects of unmodified human hemoglobin. J Pharmacol Exp Ther 288(3):1278–1287
Liu X, Miller MJ, Joshi MS, Sadowska-Krowicka H, Clark DA, Lancaster JR Jr (1998) Diffusion-limited reaction of free nitric oxide with erythrocytes. J biol chem 273(30):18709–18713
Looker D, Abbott-Brown D, Cozart P, Durfee S, Hoffman S, Mathews AJ, Miller-Roehrich J, Shoemaker S, Trimble S, Fermi G et al (1992) A human recombinant haemoglobin designed for use as a blood substitute. Nature 356(6366):258–260. doi:10.1038/356258a0
Matheson B, Kwansa HE, Bucci E, Rebel A, Koehler RC (2002) Vascular response to infusions of a nonextravasating hemoglobin polymer. J Appl Physiol 93(4):1479–1486. doi:10.1152/japplphysiol.00191.2002
Misra HP, Fridovich I (1972) The generation of superoxide radical during the autoxidation of hemoglobin. J Biol Chem 247(21):6960–6962
Moo-Penn WF, Wolff JA, Simon G, Vacek M, Jue DL, Johnson MH (1978) Hemoglobin Presbyterian: beta108 (G10) asparagine leads to lysine, a hemoglobin variant with low oxygen affinity. FEBS Lett 92(1):53–56
Moore EE, Moore FA, Fabian TC, Bernard AC, Fulda GJ, Hoyt DB, Duane TM, Weireter LJ Jr, Gomez GA, Cipolle MD, Rodman GH Jr, Malangoni MA, Hides GA, Omert LA, Gould SA (2009) Human polymerized hemoglobin for the treatment of hemorrhagic shock when blood is unavailable: the USA multicenter trial. J Am Coll Surg 208(1):1–13. doi:10.1016/j.jamcollsurg.2008.09.023
Murray JA, Ledlow A, Launspach J, Evans D, Loveday M, Conklin JL (1995) The effects of recombinant human hemoglobin on esophageal motor functions in humans. Gastroenterology 109(4):1241–1248
Nagababu E, Ramasamy S, Rifkind JM, Jia Y, Alayash AI (2002) Site-specific cross-linking of human and bovine hemoglobins differentially alters oxygen binding and redox side reactions producing rhombic heme and heme degradation. Biochemistry 41(23):7407–7415
Nakai K, Sakuma I, Ohta T, Ando J, Kitabatake A, Nakazato Y, Takahashi TA (1998) Permeability characteristics of hemoglobin derivatives across cultured endothelial cell monolayers. J lab clin med 132(4):313–319
Napolitano LM (2009) Hemoglobin-based oxygen carriers: first, second or third generation? Human or bovine? Where are we now? Crit Care Clin 25(2):279–301. doi:10.1016/j.ccc.2009.01.003 (Table of Contents)
Olson JS, Foley EW, Rogge C, Tsai AL, Doyle MP, Lemon DD (2004) No scavenging and the hypertensive effect of hemoglobin-based blood substitutes. Free Radical Biol Med 36(6):685–697. doi:10.1016/j.freeradbiomed.2003.11.030
OPK Biotech (2012) OPK Biotech LLC. http://www.opkbiotech.com/company/about.php. Accessed 12 October 2012
OXYVITA Inc. (2012) Revolutionizing blood science OXYVITA Inc. http://www.oxyvita.us/. Accessed 5 August 2012
Palmer AF (2006) Molecular volume and HBOC-induced vasoconstriction. Blood 108(10):3231–3232
Palmer AF, Sun G, Harris DR (2009a) The quaternary structure of tetrameric hemoglobin regulates the oxygen affinity of polymerized hemoglobin. Biotechnol Prog 25(6):1803–1809. doi:10.1002/btpr.265
Palmer AF, Sun G, Harris DR (2009b) Tangential flow filtration of hemoglobin. Biotechnol Prog 25(1):189–199. doi:10.1002/btpr.119
Rameez S, Palmer AF (2011) Simple method for preparing poly(ethylene glycol)-surface-conjugated liposome-encapsulated hemoglobins: physicochemical properties, long-term storage stability, and their reactions with O-2, CO, and NO. Langmuir 27(14):8829–8840. doi:10.1021/La201246m
Rentko VT, Pearce LB, Moon-Massat PF, Gawryl MS (2006) Hemopure® (HBOC-201, hemoglobin glutamer-250 (Bovine)): preclinical studies. In: Winslow RM (ed) Blood substitutes. Elsevier Academic Press, Amsterdam, pp 424–436
Rice J, Philbin N, Light R, Arnaud F, Steinbach T, McGwin G, Collier S, Malkevich N, Moon-Massatt P, Rentko V, Pearce LB, Ahlers S, McCarron R, Handrigan M, Freilich D (2008) The effects of decreasing low-molecular weight hemoglobin components of hemoglobin-based oxygen carriers in swine with hemorrhagic shock. J Trauma 64(5):1240–1257. doi:10.1097/TA.0b013e318058245e
Rohlfs RJ, Bruner E, Chiu A, Gonzales A, Gonzales ML, Magde D, Magde MD Jr, Vandegriff KD, Winslow RM (1998) Arterial blood pressure responses to cell-free hemoglobin solutions and the reaction with nitric oxide. J Biol Chemistry 273(20):12128–12134
Sakai H, Cabrales P, Tsai AG, Tsuchida E, Intaglietta M (2005) Oxygen release from low and normal P50 Hb vesicles in transiently occluded arterioles of the hamster window model. Am J Physiol Heart Circulatory physiol 288(6):H2897–H2903. doi:10.1152/ajpheart.01184.2004
Sakai H, Sato A, Sobolewski P, Takeoka S, Frangos JA, Kobayashi K, Intaglietta M, Tsuchida E (2008) NO and CO binding profiles of hemoglobin vesicles as artificial oxygen carriers. Biochim Biophys Acta 1784(10):1441–1447. doi:10.1016/j.bbapap.2008.03.007
Savitsky JP, Doczi J, Black J, Arnold JD (1978) A clinical safety trial of stroma-free hemoglobin. Clin Pharmacol Ther 23(1):73–80
Saxena R, Wijnhoud AD, Carton H, Hacke W, Kaste M, Przybelski RJ, Stern KN, Koudstaal PJ (1999) Controlled safety study of a hemoglobin-based oxygen carrier, DCLHb, in acute ischemic stroke. Stroke; J Cereb Circ 30(5):993–996
Sehgal LR, Rosen AL, Noud G, Sehgal HL, Gould SA, DeWoskin R, Rice CL, Moss GS (1981) Large-volume preparation of pyridoxylated hemoglobin with high P50. J Surg Res 30(1):14–20
Sehgal LR, Gould SA, Rosen AL, Sehgal HL, Moss GS (1984) Polymerized pyridoxylated hemoglobin: a red cell substitute with normal oxygen capacity. Surgery 95(4):433–438
Shah SV, Walker PD (1988) Evidence suggesting a role for hydroxyl radical in glycerol-induced acute renal failure. Am J Physiol 255(3 Pt 2):F438–F443
Silva G, Jeney V, Chora A, Larsen R, Balla J, Soares MP (2009) Oxidized hemoglobin is an endogenous proinflammatory agonist that targets vascular endothelial cells. J Biol Chemistry 284(43):29582–29595. doi:10.1074/jbc.M109.045344
Sloan EP, Koenigsberg M, Gens D, Cipolle M, Runge J, Mallory MN, Rodman G Jr (1999) Diaspirin cross-linked hemoglobin (DCLHb) in the treatment of severe traumatic hemorrhagic shock: a randomized controlled efficacy trial. JAMA, J Am Med Assoc 282(19):1857–1864
Stetter MN, Baerlocher GM, Meiselman HJ, Reinhart WH (1997) Influence of a recombinant hemoglobin solution on blood rheology. Transfusion 37(11–12):1149–1155
Suaudeau J, Fallon JT, Kunica E, Austen WG, Erdmann AJ 3rd (1979) Protection by plasma proteins of the isolated lamb heart perfused with stroma-free hemoglobin at 38 degrees. Ann Surg 189(3):322–333
Thompson A, McGarry AE, Valeri CR, Lieberthal W (1994) Stroma-free hemoglobin increases blood pressure and GFR in the hypotensive rat: role of nitric oxide. J Appl Physiol 77(5):2348–2354
Tsai AG, Cabrales P, Manjula BN, Acharya SA, Winslow RM, Intaglietta M (2006) Dissociation of local nitric oxide concentration and vasoconstriction in the presence of cell-free hemoglobin oxygen carriers. Blood 108(10):3603–3610. doi:10.1182/blood-2006-02-005272
Varnado CL, Mollan T, Birukou I, Smith BJ, Henderson DP, Olson JS (2012) Development of recombinant hemoglobin-based oxygen carriers. Antioxid Redox Signal. doi:10.1089/ars.2012.4917
Viele MK, Weiskopf RB, Fisher D (1997) Recombinant human hemoglobin does not affect renal function in humans: analysis of safety and pharmacokinetics. Anesthesiology 86(4):848–858
Vogel WM, Dennis RC, Cassidy G, Apstein CS, Valeri CR (1986) Coronary constrictor effect of stroma-free hemoglobin solutions. Am J Physiol 251(2 Pt 2):H413–H420
Walker PD, Shah SV (1988) Evidence suggesting a role for hydroxyl radical in gentamicin-induced acute renal failure in rats. J Clin Investig 81(2):334–341. doi:10.1172/JCI113325
Winslow RM (2003) Current status of blood substitute research: towards a new paradigm. J Intern Med 253(5):508–517
Winslow RM, Gonzales A, Gonzales ML, Magde M, McCarthy M, Rohlfs RJ, Vandegriff KD (1998) Vascular resistance and the efficacy of red cell substitutes in a rat hemorrhage model. J Appl Physiol 85(3):993–1003
Yu B, Shahid M, Egorina EM, Sovershaev MA, Raher MJ, Lei C, Wu MX, Bloch KD, Zapol WM (2010) Endothelial dysfunction enhances vasoconstriction due to scavenging of nitric oxide by a hemoglobin-based oxygen carrier. Anesthesiology 112(3):586–594. doi:10.1097/ALN.0b013e3181cd7838
Yu Z, Friso G, Miranda JJ, Patel MJ, Lo-Tseng T, Moore EG, Burlingame AL (1997) Structural characterization of human hemoglobin crosslinked by bis(3,5-dibromosalicyl) fumarate using mass spectrometric techniques. Protein Sci: Publ Protein Soc 6(12):2568–2577. doi:10.1002/pro.5560061209
Zhang L, Levy A, Rifkind JM (1991) Autoxidation of hemoglobin enhanced by dissociation into dimers. J Biol Chemistry 266(36):24698–24701
Zhang N, Jia Y, Chen G, Cabrales P, Palmer AF (2011) Biophysical properties and oxygenation potential of high-molecular-weight glutaraldehyde-polymerized human hemoglobins maintained in the tense and relaxed quaternary states. Tissue Eng Part A 17(7–8):927–940. doi:10.1089/ten.TEA.2010.0353
Zhou Y, Jia Y, Buehler PW, Chen G, Cabrales P, Palmer AF (2011) Synthesis, biophysical properties, and oxygenation potential of variable molecular weight glutaraldehyde-polymerized bovine hemoglobins with low and high oxygen affinity. Biotechnol Prog. doi:10.1002/btpr.624
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Belcik, B.M., Palmer, A.F. (2013). Vasoconstriction, Hypertension and Oxidative Toxicity are Regulated by Polymerized Hemoglobin Size. In: Kim, H., Greenburg, A. (eds) Hemoglobin-Based Oxygen Carriers as Red Cell Substitutes and Oxygen Therapeutics. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-40717-8_37
Download citation
DOI: https://doi.org/10.1007/978-3-642-40717-8_37
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-40716-1
Online ISBN: 978-3-642-40717-8
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)