Abstract
Hemoglobin (Hb), a tetrameric protein, is responsible for the transport of oxygen in red blood cells (Perutz 1980). Attempts to use hemolysate (Amberson 1937) and stroma-free Hb as Hb based oxygen carrier (Rabiner et al. 1967) resulted in nephrotoxicity and cardiovascular adverse effects (Savitsky et al. 1978). Thus, nanobiotechnological modification is needed before it can be used (Chang 1964)
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Hemoglobin (Hb), a tetrameric protein, is responsible for the transport of oxygen in Red Blood Cells (RBC) (Perutz 1980). Attempts to use hemolysate (Amberson 1937) and stroma-free Hb as Hb based oxygen carrier (Rabiner et al. 1967) resulted in nephrotoxicity and cardiovascular adverse effects (Savitsky et al. 1978). Thus, nanobiotechnological modification is needed before it can be used (Chang 1964)
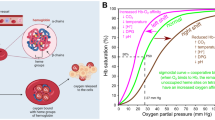
1.1 Artificial Red Blood Cell
The first artificial RBC that contains Hb and RBC enzymes (Fig. 1.1) have oxygen dissociation curve similar to RBCs, since 2-3-DPG is retained inside (Chang 1957, 1964). Hb stays inside as tetramers and RBC enzymes like carbonic anhydrase and catalase retain their activities (Chang 1964, 1972). These artificial RBCs do not have blood group antigens on the membrane and therefore do no aggregation in the presence of blood group antibodies (Chang 1972). However, the single major problem was the rapid removal of these artificial cells from the circulation. Nanobiotechnology based soluble complex was therefore investigated to increase the circulation time.
Micro dimension artificial RBC with ultrathin nylon-protein membrane from Chang 1965
1.2 First Generation Hemoglobin Based Oxygen Carriers
The first nanobiotechnology approach reported is the crosslinking of Hb into ultrathin polyhemoglobin (PolyHb) membrane with nanodimension thickness (Chang 1964, 1965, 1972) (Fig. 1.2). This is used to form the membrane of artificial RBCs (Chang 1964, 1965, 1972). If the emulsion is made very small, then the whole submicron artificial cells can be crosslinked into PolyHb of nanodimension. Glutaraldehyde can crosslink Hb into soluble PolyHb each consisting of an assembly of 4–5 Hb molecules (Chang 1971) (Fig. 1.2). Crosslinking of Hb into PolyHb includes both intermolecular and intramolecular crosslinking. Bunn and Jandl (1968) chose to do only intramolecular crosslinking of a single Hb molecule. Sebacyl chloride crosslinks hemoglobin and diamine to form polyamide conjugated hemoglobin (Chang 1964, 1972) (Fig. 1.2). An useful extension of this is the crosslinking of single protein molecule to soluble polymers like dextran (Wong 1988) and polyethylene glycol (PEG) (Park et al. 1981) (Fig. 1.2).
Upper left basic method of using bifunctional agents to assemble and crosslink Hb into PolyHb. Upper right soluble complex of PolyHb. Lower left basic method of conjugating Hb to polymer. Lower right conjugation of Hb to polyamide, soluble dextran or PEG (with copyright permission from Chang 2007 Monograph on Artificial Cells)
1.3 Little Interest Until It was Too Late When HIV Contaminated Donor Blood Arrived
It was thought by many that blood substitute was a simple matter to develop without the need for basic research. Thus, there was little or no interest in blood substitutes at that time. As a result, researchers had to channel their major research effort into other areas (Chang 1964, 1972, 2005, 2007, 2009–2013). It was only when the HIV contaminated donor blood crisis came in the 1980s that intense interest started to focus on blood substitutes. Concerned researchers and industries then placed maximal effort into solving this urgent need. Unfortunately, without the needed basic research and basic knowledge, development of blood substitutes had to be done by trial and error. Furthermore, the urgent need was such that the simplest and shortest route was chosen, in the form of simple oxygen carriers like Hb based oxygen carrier.
2 First Generation Hemoglobin Based Oxygen Carriers
2.1 Four Common Types
The four types of most commonly studied first generation Hb based oxygen carriers are shown in Figs. 1.3 and 1.4. These are PolyHb, conjugated Hb, intramolecularly crosslinked tetrameric Hb and recombinant Hb.
First generation Hb based oxygen carriers (with copyright permission from Chang 2007 Monograph on Artificial Cells)
Left Stabilized tetrameric Hb is small enough to cross intercellular junction and remove interstitial nitric oxide resulting in vasoconstriction. However this will not happen if stabilized tetrameric Hb has been modified to prevent NO removal. Right PolyHb and conjugated Hb are large enough so they cannot cross the intercellular junction to cause vasoconstriction. Exceptions are in endothelial dysfunction or those preparations that contain substantial amount of tetrameric Hb—unless modified to prevent removal of nitric oxide (with copyright permission from Chang 2007 Monograph on Artificial Cells)
2.2 PolyHb for Use as Oxygen Carrier for Transfusion
The 1971 basic principle of glutaraldehyde crosslinked PolyHb (Chang 1971) (Fig. 1.2) has been independently developed most extensively by centers around the world (Dudziak and Bonhard 1980; DeVenuto 1982; Keipert et al. 1982; Keipert and Chang 1987; Segal et al. 1983; Moss et al. 1988; Gould et al. 1995; Pearce and Gawryl 1998). Unlike RBCs, there is no blood group, and thus PolyHb can be given on the spot, without waiting for typing and cross-matching in the hospital. They are also free from infective agents such as HIV, hepatitis C, bacteria, parasites and so on. Whereas donor blood has to be stored at 4 °C and is only good for 42 days, PolyHb can be stored at room temperature for more than one year. Thus, PolyHb can have important uses in a number of clinical conditions.
The following is a summary of the recent ongoing research, development and clinical use.
2.3 Glutaraldehyde Crosslinked Human PolyHb
Gould and Moss started the Northfield Laboratory to develop glutaraldehyde crosslinked human PolyHb (Sehgal et al. 1983; Moss et al. 1988; Gould et al. 1995). Their clinical trial shows that this can replace blood lost in trauma surgery by keeping the blood Hb at an acceptable level (Gould et al. 2002). This clinical trial on 171 patients showed that this product can successfully replace extensive blood loss in trauma surgery by maintaining the Hb level at the 8–10 g/dl needed for safe surgery with no reported side effects. More recently, they have carried out clinical trials on its used in pre-hospital emergencies since no typing and cross-matching is needed and it can be used right on the spot. This clinical trial involves giving this in the ambulance to about 700 hemorrhagic shock patients shows that PolyHb can maintain the patient for 12 h after reaching the hospital. In the control group, most of the patients need blood transfusion on reaching the hospital (Moore et al. 2009).
2.4 Glutaraldehyde Crosslinked Bovine PolyHb
Bing L, Wong and Carl Rausch were the cofounders of Biopure to start work in this. Recent overviews of the development and extensive clinical trials are available (Pearce and Gawryl 1998; Jahr et al. 2008; Greenburg et al. 2008; Greenburg 2013). For example, they have carried out multicenter, multinational, randomized, single-blind, RBC-controlled Phase III clinical trials in patients undergoing elective orthopedic surgery. A total of 688 patients were randomized 1:1 to receive either the PolyHb or RBC at the time of the first perioperative RBC transfusion decision and 59.4 % of the patients receiving PolyHb required no RBC transfusion all the way to follow up and 96.3 % avoided transfusion with RBC on the first postoperative day and up to 70.3 % avoided RBC transfusion up to day 7 after. Russia and South Africa have approved this for routine clinical uses in patients.
2.5 Other Sources of Hemoglobin for PolyHb
In addition to Hb from outdated human donor blood, bovine Hb, as mentioned above is another source (Feola et al. 1983; Wong et al. 2011). Other sources of Hb have also been used for PolyHb. These included, for example, preclinical studies on porcine Hb (Zhu et al. 2007; Zhu and Chen 2013) and Hb from human placental blood (Li et al. 2006). These two groups have carried out extensive laboratory and preclinical studies. Other possible sources of Hb include recombinant Hb (Hoffman et al. 1990), marina Hb (Rousselot et al. 2006) and others.
2.6 Conjugated Hemoglobin
In the presence of diamine, sebacyl chloride crosslinks Hb with polyamide to form conjugated Hb (Chang 1964, 1965) (Fig. 1.2). An extension of this is the crosslinking of single Hb molecule to soluble polymers like dextran (Wong 1988; Tam et al. 1976) or PEG (Abuchowski and Es 1977; Iwashita 1992; Yabuki 1990; Shorr, Viau and Abuchowski 1996; Li 2005; Winslow 2006; Liu and Xiu 2008; Seetharama et al. 2013) (Fig. 1.3). PEG-Hb shares many of the advantages of PolyHb as described above. More details are available in other later chapter. Clinical trials are ongoing for two types of PEG-Hb (Winslow 2006; Li 2005; Liu and Xiu 2008). A Double-Blind, Randomized, Multicenter Study of MP4OX has been reported (Van der Linden et al 2011).
2.7 Stabilized Tetrameric Hb and Other Factors
In addition to glutaraldehyde crosslinked PolyHb and conjugated Hb there are other ways of modifying Hb (Fig. 1.3). These include intramolecularly crosslinked tetrameric Hb (Walder 1979; Przybelski et al. 1996; Burhop and Estep 2001), recombinant human Hb (Looker 1992; Shoemaker 1994). Some have resulted in adverse effects like vasoconstriction in clinical trials. This has led to the proposal that the intercellular junctions of the endothelial lining of vascular wall allow tetrameric Hb to enter into the interstitial space. There, Hb acts as a sink in binding and removing nitric oxide needed for maintaining the normal tone of smooth muscles. This results in the constriction of blood vessels and other smooth muscles especially those of the esophagus and the GI tract (Fig. 1.4). However, this can be avoided if nitric oxide removal is prevented by a specially designed recombinant Hb (Doherty et al. 1998) or a modified form of stabilized intramolecularly crosslinked Bovine Hb (Wong and Kwok 2011) or by the administration of nitric oxide (Yu et al. 2010; Zapol 2012).
Even PolyHb, for example raffinose polymerized Hb (Hsia et al. 1992), that contains more than 30 % tetrameric Hb can have some vasoconstriction effects. Those PolyHb or conjugated Hb that contain high levels of uncrosslinked Hb or low molecular weight PolyHb could also have adverse effects (Kim and Greenburg 1997; Chang 1997, 2007; Bucci 2011, 2013) (Fig 1.4). There are also other factors including pathological characteristics of patients, like endothelial dysfunction (Yu et al. 2010). Furthermore, the design of preclinical and clinical study is complicated (Greenburg and Kim 1992; Zuck 1994; Fratantoni 1994; Klein 2000; Chang, 1997, 2007; Winslow 2006; Greenburg 1992, 2008, 2013). As mentioned earlier, vasoconstriction can be avoided if nitric oxide removal is prevented by a specially designed recombinant Hb (Doherty et al. 1998) or a modified form of stabilized intramolecularly crosslinked Bovine Hb (Wong and Kwok 2011) or by the administration of nitric oxide (Yu et al. 2010; Zapol 2012).
In medicine, nothing can be considered to be a “cure all”. First generation Hb oxygen carriers are suitable for many clinical conditions especially in patients with no endothelial dysfunction or as discussed below in patients with no sustained ischemia or elevated tissue pCO2. Thus, one cannot attempt to combine the clinical trial results of different types of Hb based blood substitutes and different clinical conditions into a single meta-analysis as has been done (Natanson et al. 2008). First generation Hb based oxygen carrier is like penicillin that is a good basic method for use in many conditions. However, as for penicillin, with experience gained from clinical results, new generations need to be developed to complement and supplement the first generation. However, there is no reason to use a more complicated and more expensive new generation system if the clinical conditions can be treated safely and effective using the first generation ones.
3 New Generations
3.1 Nanobiotechnology to Assemble Hemoglobin with Antioxidant Enzmyes
In heart attack or stroke due to arterial obstruction, RBCs, being 7 micron in diameter, cannot go through the obstruction (Fig. 1.5). PolyHb being in solution, can more readily go through the obstruction to supply the needed oxygen (Fig. 1.5). However, this has to be done early since if there is much delay, PolyHb alone might result in the production of oxygen radicals that can cause tissue injury (ischemia reperfusion injuries). As mentioned above PolyHb is also ideal for use in hemorrhagic shock since it can be given on the spot. Here again there is a window of safety since ischemia reperfusion injury can result if there is much delay. Even antioxidant enzymes normally present in RBCs are not enough to prevent this problem in severe sustained hemorrhagic shock (Biro et al. 1995).
Arterial obstruction from the narrowing of artery can result in Stroke and heart attack. RBCs being 7–8 micron in diameter have difficulty flowing through obstructed vessels to supply the needed oxygen. PolyHb being a solution can perfuse through to supply the needed oxygen. However, if oxygen lack is prolonged, reperfusion with an oxygen carrier can release damaging oxygen radicals. One possible solution is to use PolyHb-SOD-CAT that has the dual function of an oxygen carrier and the ability to remove oxygen radicals (with copyright permission from Chang 2007 Monograph on Artificial Cells)
We therefore design a soluble nanobiotechnological complex of PolyHb containing two RBC antioxidant enzymes, superoxide dismutase (SOD) and catalase (CAT) in the form of PolyHb-SOD-CAT (D’Agnillo and Chang 1998) (Figs. 1.5 and 1.6) In this form the SOD and CAT can be enhanced to be much higher than those in RBCs. Thus in a rat stroke model, after 60 min of ischemia, reperfusion with PolyHb resulted in significant increase in the breakdown of the blood–brain barrier and an increase in brain water (brain edema) (Powanda and Chang 2002). On the other hand, PolyHb-SOD-CAT did not result in these adverse changes (Powanda and Chang 2002) (Fig. 1.6). Ischemia–reperfusion injury in severe sustained hemorrhagic shock can result in damage to the intestine with leakage of E-coli or endotoxin to the systemic circulation resulting in irreversible shock. Thus, we tested and found that PolyHb-SOD-CAT can decrease oxygen radicals formation in a rat model of intestinal ischemia reperfusion (Razack et al. 1997). Others have used this for pancreatic beta cells in rats (Nadithe and Bae 2011a); for myocardial infarction attenuation in rats (Wang et al. 2012) and rat kidney transplantation from Korea (Chang et al. 2004). Hsia extended the PolyHb-SOD_CAT approach to prepare a Hb with synthetic antioxidant based on the covalently binding of nitroxides (Buehler et al. 2004; Ma and Hsia 2013). In another approach, using his background on the subject (Alayash 2004), a Hb-haptoglobin complex can also be used to protect against oxidative stress (Jia 2013). Another one is Arenicola marina Hb (Rousselot et al. 2006) with antioxidant activity. Simoni et al. (1997) added a pharmacological solution with antioxidant function to their modified Hb. More details will be available by these authors in later chapters.
Different fluids were infused after 90 min of combined hemorrhagic shock and brain ischemia. Brain edema was followed. PolyHb-SOD-CAT treated animals did not have any brain edema. On the other hand, PolyHb or free solution of Hb, SOD and CAT caused significant increases in brain edema (From Powanda and Chang 2002 with copyright permission from J. Artificial Cells, Blood Substtutes and Biotechnology)
3.2 Nanobiotechnology to Assemble Hemoglobin with Superoxide Dismutase, Catalase and Carbonic Anhydrase Resulting in a Carrier for Both Oxygen and Carbon Dioxide with Enhanced Antioxidant Activity
PolyHb-SOD-CAT is an oxygen carrier with enhanced antioxidant properties. Since RBCs also carry out the important function of transport of carbon dioxide from tissue to the lung for excretion, do we need this component? Sims et al. (2001) used a novel microelectrode to measure tissue pCO2 in animal model of severe hemorrhagic shock. He shows that mortality is related to the elevation of tissue pCO2. The enzyme carbonic anhydrase (CA) in RBC is the major means for the transport of tissue CO2 to the lung. We therefore use the nanobiotechnological method to assemble CA with Hb and antioxidant enzymes to form PolyHb-SOD-CAT-CA (Bian et al. 2011). Our recent study in a rat hemorrhagic shock model shows that this is more efficient than RBC in lowering the elevated pCO2 level in the tissue in a hemorrhagic shock rat model (Bian et al. 2013a) (Fig. 1.7).
Hemorrhage shock rats maintained at a mean arterial blood pressure of 30 mm Hg. The tissue pCO2 increases steady with time. Reinfusion of different fluids shows that lactated Ringer salt solution or PolyHb did not lower the tissue pCO2 as much as blood or PolyHb-SOD-CAT-CA. The later is even more effective than blood. (From Bian et al. 2013a with copyright permission from J Artificial Cells, Nanomedicine and Biotechnology)
3.3 Stability of PolyHb-Enzymes Nanobiotechnology Complexes
One obvious question is how stable are these type of PolyHb-enzymes complexes. Unlike PolyHb, the enzyme component may not be sufficiently stable with storage especially in room temperature and hot climate. Our very recent study shows that freeze-dried powder preparation of PolyHb-SOD-CAT-CA is stable with very long-term storage at −80 and 4 °C. It is also very stable at room temperature and even at 37 °C when compared to the solution Bian, Yang and Chang (2013). The freeze-dried powder is much easier for storage since it takes up little space also being very light and compact, it is easy for transportation. This is especially important for emergency, disasters or war.
3.4 Nanobiotechnology to Assemble Hemoglobin and Fibrinogen into an Oxygen Carrier with Platelet-Like Activity
PolyHb can replace the Hb level in very severe hemorrhage, but platelets also need to be replaced (Gould et al. 2002). We studied this in a rat model and found that replacing more than 80 % of the total blood volume with PolyHb leads to defects in blood clotting (Wong and Chang 2007) (Fig. 1.7). We use nanobiotechnology to assmble Hb with fibrinogen to form PolyHb-fibrinogent (Wong and Chang 2007). Using this, we can replace up to 98 % of the total blood volume with PolyHb-fibrinogen without causing clotting problems (Wong and Chang 2007) (Fig. 1.8).
Exchange transfusion in rats. There is clotting problem when more than 80 % of blood has been exchanged with PolyHb. There is no problem with clotting when 98 % of the blood is replaced with PolyHb-fibrinogen with platelet-like activity (From Wong and Chang, 2007 with copyright permission from J. Artificial Cells, Blood Substitutes and Biotechnology)
3.5 Hemoglobin Based Oxygen Carriers in the Treatment of Cancer
Abnormal microcirculation in tumour leads to decrease in perfusion by oxygen carrying RBCs. PolyHb can more easily perfuse the abnormal microcirculation of tumours to supply oxygen needed for chemotherapy or radiation therapy (Robinson et al. 1995; Teicher 1995) (Fig. 1.9). Thus, PEG conjugated Hb has been used this way (Han et al. 2012; Shorr et al. 1996). PolyHb also decreases the growth of tumour and increases the lifespan in a rat model of gliosarcoma brain tumour (Pearce and Gawryl 1998).
Unlike RBC, PolyHb and PEG-Hb can better perfused the microcirculation of tumours. This increases the low oxygen tension in tumour and thus increases their sensitivity to radiation and chemotherapy. PolyHb-tyrosinase combine this effect with the removal of tyrosine needed for the growth of melanoma (with copyright permission from Chang 2007 Artificial Cells)
We have crosslinked tyrosinase with Hb to form a soluble PolyHb-tyrosinase complex (Yu and Chang 2004) (Figs. 1.9, 1.10). This has the dual function of supplying the needed oxygen and at the same time lowering the systemic levels of tyrosine needed for the growth of melanoma. Intravenous injections delayed the growth of the melanoma without causing adverse effects in the treated animals (Yu and Chang 2004) (Fig. 1.10). Our more recent study include the use of PLA and PEG-PLA membrane nano artificial cells containing polyHb-tyrosinase (Furstier and Chang 2012; Wang and Chang 2012).
Effects of daily intravenous injection of PolyHb-tyrosinase on tumor growth of B16F10 melanoma in mice. (i) sham control: no intravenous injection; (ii) saline control: (iii) PolyHb-tyrosinase group (with copyright permission from Chang 2007 Monograph on Artificial Cells)
4 Nanodimension Complete Artificial Red Blood Cells
4.1 Early Artificial Red Blood Cells
The first artificial RBCs (Fig. 1.1) have all the in vitro function of RBCs as shown by oxygen dissociation curve (Chang 1957), carbonic anhydrase activity (Chang 1964) and catalase activities (Chang and Poznansky 1968). These artificial RBCs do not have blood group antigens on the membrane and therefore do no aggregation in the presence of blood group antibodies (Chang 1972). However, the single major problem is the rapid removal of these artificial cells from the circulation. Much of the studies since that time are to improve survival in the circulation by decreasing uptake by the reticuloendothelial system. Since removal of sialic acid from biological RBCs resulted in their rapid removal from the circulation (Chang 1965, 1972), we started to modify the surface properties on artificial RBCs. This included synthetic polymers, negatively charge polymers, crosslinked protein, lipid–protein, lipid–polymer and others (Chang 1965, 1972). As discussed below, artificial RBCs have since been extensively explored by many researchers around the world. These include Beissinger, Bian, Chang, Farmer, Gao, Hunt, Kobayashi, Lee, Mobed, Nishiyia, Rabinovic, Rudolph, Sakai, Schmidt, Sinohara, Szebeni, Takeoka, Tsuchida, Takahashi, Usuba and many others.
4.2 Bilayer Lipid Membrane Nano Artificial RBC
Bangham (1965) reported the preparation of liposomes each consisting of microspheres of onion like concentric lipid bilayers—multi-lamellar. This was initially used as membrane models in basic research. The large amount of lipid in the multi-lamellar liposome limits the amount of water-soluble drugs that can be enclosed. Thus, the basic principle and method of preparing artificial cells using ether as the dispersing phase (Chang 1957, 1964) was extended by into what they call an “ether evaporation method” to form single bilayer (unilamellar) lipid membrane liposomes for drug delivery (Deamer and Bangham 1976). Using an extension of this a major progress is the preparation of submicron lipid membrane artificial RBC (Djordjevich and Miller, 1980; Farmer et al. 1988; Philips et al. 1999; Rudolph 1994; Kobayashi et al. 2005; Tsuchida et al. 2006; Sakai 2013). By the addition of PEG to the lipid membrane, the circulation time has been increased to a half time of about 36 h in rats (Philips et al. 1999). These advances make it now possible to scale up for detailed preclinical studies towards clinical trial (Tsuchida 1998; Kobayashi et al. 2005; Sakai 2013). The uptake is mainly by the reticuloendothelial system. It is possible to replace 90 % of the RBCs in rats with these artificial RBCs (Tsuchida 1998; Kobayashi et al. 2005; Sakai 2013). The animals with this percentage of exchange transfusion still remain viable. Studies also reported effectiveness in hemorrhagic shock. There are no changes in the histology of brain, heart, kidneys and lungs of rats. More details will be available in a later chapter by these authors.
4.3 Nanodimension Biodegradable Polymeric Artificial Cells
Using a modification of this author’s earlier method of micron dimension biodegradable polymeric membrane artificial cells (Chang 1976) we have prepared biodegradable polymeric membrane nano dimension PLA artificial RBCs (Chang 1997, 2007; Chang et al. 2003; Yu and Chang 2004). This decreases the amount of lipid needed for the nano artificial cells. Polymer membrane is stronger than bilayer lipid and a thinner polymer membrane can be used. Figure 1.11 shows the amount of membrane material in Hb lipid vesicles compared to PLA nano RBCs.
Amount of membrane material in Hb lipid vesicles compared to PLA nano RBCs (with copyright permission from Chang 2007 Monograph on Artificial Cells
Polylactide membrane in PLA nano RBCs is biodegradable into lactic acid and finally water and carbon dioxide and thus is not retained in the reticuloendothelial system (Fig. 1.12). Lactic acid in 500 ml of PLA nano artificial RBC is 83 meq/500 ml compared to resting body production of lactic acid of 1,200 meq/day and a maximal body removal capacity for lactic acid of 7,860 meq/day (Fig. 1.12).
Polylactide membrane in PLA nano RBCs is biodegraded into lactic acid and finally water and carbon Lactic acid in 500 ml of PLA nano artificial RBC compared to resting body production and maximal body removal capacity (Chang 2007)
These nano artificial RBC of 80–150 nm contain all the RBC enzymes and can convert methemoglobin to Hb (Chang et al. 2003) (Fig. 1.13). The membrane is not permeable to larger molecules, but freely permeable to small molecules like glucose and reducing agents from plasma. In vitro study shows that when incubated at 37 °C MetHb increases quickly (Fig. 1.13). Addition of a reducing agent, ascorbic acid prevents the increase in MetHb. Addition of glucose and NADH allows the Embden Meyerhof enzyme system in the nano artificial RBC to decrease MetHb further (Fig. 1.13).
Left Biodegradable polymeric membrane nano artificial RBC contains Hb and all the enzymes of RBC. The membrane is not permeable to larger molecules, but freely permeable to glucose and reducing agents from plasma. Right When incubated at 37 °C MetHb increases quickly. Addition of a reducing agent, ascorbic acid prevents the increase in MetHb. Addition of glucose and NADH allows the Embden Meyerhof enzyme system in the nano artificial RBC to decrease MetHb further (with copyright permission from Chang 2007 Monograph on Artificial Cells)
Our studies show that using a polyethylene-glycol-polylactide copolymer membrane we are able to strengthen the membrane and increase the circulation time of these nano artificial RBCs to double that of PolyHb (Fig. 1.14) (Chang et al. 2003). The result of other groups support these findings (Zhang et al. 2008; Sheng et al. 2009). We also reported that infusion of 1/3 blood volume into rats did not have any adverse effects on the kidney (Liu and Chang 2008a) or the liver (Liu and Chang 2008b) on a long term basis.
Comparison of the maximal systemic non-RBC Hb reached after infusion of different preparations and the time to reached a given non-RBC Hb level. The time for PolyHb-17 to reach a non-RBC Hb level of 1.67 gm/dl is 14 h in rats equivalent to 24 h in human. The time for different types of nano artificial RBCs to reach this non-RBC Hb concentration is used to calculate the equivalent time for human (Chang et al. 2003) (with copyright permission from J Artificial Cells, Blood Substitutes and Biotechnology)
Further studies show that one infusion with a volume of 1/3 the total blood volume, did not result in adverse effects on the biochemistry and histology of the kidney (Liu and Chang 2008a) or liver and spleen (Liu and Chang 2008b). Our most recent study uses PEG-PLA membrane nano artificial cells containing PolyHb-catalase-superoxide dismutase-carbonic anhydrase in a hemorrhagic shock rat model with 2/3 of the blood removed. After one hour of hemorrhagic shock at 30 mmHg, infusion of this preparation effectively resuscitated the animal and lowered the elevated tissue PCO2 (Wei et al. 2013).
4.4 Possible Variations in the Membrane of Nano Artificial RBC
Hb lipid vesicles are bilayer membrane nano artificial RBCs containing Hb (Adding PEG to the bilayer lipid membrane greatly increased the circulation time. These PEG-lipid vesicles are more like the lipid–polymer membrane artificial cells (Chang 1972) and are no longer pure lipid vesicles. Discher’s group (Photos et al. 2003) tried to increase the strength of the PEG–lipid membrane artificial cells by using self-assembling of block copolymers. PEG was the hydrophilic block and polyethylene or polybutadiene (PB) was the hydrophobic block. This significantly increased strength when compared to PEG–lipid membrane artificial cells. This so-call polymersomes are PEG-PB nano artificial RBC similar to PEG-PLA nano artificial RBC. Thus, polymeric membrane artificial cells have branched off into multilamellar liposome that then has evolved into lipid membrane artificial cells, then polymer-lipid membrane artificial cells, and finally back to the polymeric membrane artificial cells that are now called by different names including polymersomes, nanocapsules, nanoparticles, vesicles and others.
5 Stem Cells for Blood Substitutes
Some feel that we should depend on stem cells to prepare RBCs. This may be useful for platelets and leucocytes since only small amounts are needed. Even then, platelets, unlike nanobiotechnological derived ones, has extremely short storage life. In the case of RBCs, despite much research, it is still not possible to scale this up sufficient for the large volume of RBC needed (Mazurier et al. 2011). When scale up becomes a reality, this will be an important source of RBC for many clinical conditions. However, these RBC will still have many of the same problems of RBC. These include:
-
RBCs need refrigeration but still have a short storage time at 4 °C of less than 42 days. PolyHb can be stored in room temperature for more than 1 year. Freeze-dry powder of PolyHb and PolyHb-enzyme has even longer stability.
-
RBCs cannot be freeze-dried into powder form. HBOCs in the freeze dry form are light and compact with ease of transport and storage for emergency, major disaster or war.
-
Unlike RBCs, HBOCs can better perfuse obstructed microcirculation as in stroke, heart attack, ischemic limbs, sickle cell anemia and other conditions. It can also better perfuse disturbed microcirculations as in tumour, hemorrhagic shock and other conditions.
-
Unlike RBCs, HBOCs can be enhanced with higher enzyme levels than RBCs to be more effective against severe ischemia–reperfusion injury, fatal elevation of tissue pCO2 and other conditions.
-
Nanobiotechnology can combine Hb with other enzymes and other bioreactants for specially designed oxygen therapeutics.
6 Future Perspectives and Learning from Past Experience
The first research on artificial cells was on artificial RBC (Chang 1957, 1964). Yet, instead of blood substitutes, this research has led to extensive extensions and development and medical uses and nonmedical uses in other areas. Examples include nanomedicine, nanobiotechnology, nanotechnology, gene therapy, enzyme therapy, cancer therapy, cell/stem cell therapy, regenerative medicine, liver support support systems, drug carriers, and even in agriculture, aquatic culture, fermentation industry, food industry, nanorobotics, nanocomputers, energy production and other areas (Chang 2007 and www.artcell.mcgill.ca). This is unfortunate, since we are neglecting one of the most important area, blood substitutes and oxygen therapeutics. What are the reasons for this neglect?
There was no blood substitute to replace HIV contaminated blood in the 1980 crisis. Large number of patients receiving donor blood were infected with HIV and died. During this time there was a short period of increase support for basic research and development around the world. Unfortunately we human have short memory and many have forgotten the major disaster that we have encountered and major support for blood substitutes has disappeared after a few years. It is unbelievable that many still think that blood substitute is a simple matter that can be left alone until there is an urgent need. Others think that stem cell derived blood can solve all the problems, but as discussed above, this is not the case. Whatever the excuse, there is little or no interest in supporting blood substitutes research and development at present. Are we waiting again for another crisis to come before repeating our error of doing catch up research and development? The industries have done their best. They have to find their own resources to carry the impossible task of doing everything in basic research, applied research, preclinical studies and clinical trials. With the lack of sufficient resources and with the lack of basic knowledge in this area they have been forced to do trial and error type of R&D with resulting delays and some failures and loss of revenue. Many companies have since given up this impossible endeavor. Without sufficient resources and support for academic basic research and industrial development around the world, development of blood substitutes will continue to be done by trial and error. Furthermore, only the simplest and shortest route will be chosen despite the many possible new generations that are available.
Enormous amount of resources have been placed into basic research and developments on cancer, rare genetic diseases, molecular biology, organ failure and other areas with far less clinically useful results. With far less support, dedicated researchers and developers have persisted beyond any expectation to come out with clinically useful first generation blood substitutes one of which, PolyHb, has been approved for routine clinical uses in South Africa and Russia. There are a number of others and possible new generation HBOCs. As discussed earlier, first generation Hb oxygen carrier appears to be safe and effective for many clinical conditions. There is no reason to use more complex or more expensive systems in these cases. However, it is not a “cure all” for all clinical conditions. Much research needs to be carried out to study the types of patients who are suitable for this. For instance, we now know that they are not for patients with endothelial dysfunction. They are not for patients with “sustained” ischemia especially if associated with extensive elevation in tissue pCO2. There is nothing in medicine that can be considered as “cure all” and new generations HBOCs need to be develop for those conditions that need these. Thus, much remains to be done before first generation and new generations of blood substitutes can be widely used in more clinical conditions (Liu and Xiu 2008; Mozzarelli 2010; Chang 2013).
Is it reasonable to expect that for blood substitutes, we should be able to come out with a perfect blood substitute with little or no resources for academic and industrial research and development? Should we wait for another crisis before doing catch-up R & D that we now know will not work?
References
Abuchowski A, Es TV, Palczuk NC Davis FF (1977) Alteration of immunological properties of bovine serum albumin by covalent attachment of polyethylene glycol. J Biol Chem 252: 2578–3581
Bangham AD et al (1965) Diffusion of univalent ions across the lamellae of swollen phospholipids. J Mol Biol 13:238–252
Alayash AI (2004) Oxygen therapeutics: can we tame Hb? Nat Rev Drug Discov 3:152–159
Amberson WR (1937) Blood substitute. Biol Rev 12:48
Bian Y, Rong Z, Chang TMS (2011) Polyhemoglobin-superoxide dismutase-catalase-carbonic anhydrase: a novel biotechnology-based blood substitute that transports both oxygen and carbon dioxide and also acts as an antioxidant artificial cells. Blood Substitut Biotechnol 39:127–136
Bian YZ, Wei G, Chang TMS (2013a) Lowering of elevated tissue PCO2 in a hemorrhagic shock rat model after reinfusion of a novel nanobiotechnological polyhemoglobin-superoxide dismutase-catalase-carbonic anhydrase that is an oxygen and carbon dioxide carrier with enhanced antioxidant properties. Artif Cells Nanomed Biotechnol 41:60–68
Bian YZ, Yang L, Chang TMS (2013). Freeze dried polyhemoglobin-superoxide dismutase-catalase-carbonic anhydrase powder maintains long term stability at 37C, 20C, 4C and −70C (to be submitted)
Biro GP, Ou C, Ryan-MacFarlane C, Anderson PJ (1995) Oxyradical generation after resuscitation of hemorrhagic shock with blood or stroma free hemoglobin. Artif Cells Blood Substit Immob Biotechnol J 23:631–645
Bucci E (2011) Basic science offers a challenge for developing hemoglobin based oxygen carriers into therapeutic agent. Artif Cells Blood Substit Immob Biotechnol J 39:206–213
Bucci E (2013) Evidences regarding some pharmacologic characteristics of haemoglobin based oxygen carriers. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Buehler PW, Haney CR, Gulati A, Ma L, Hsia CJ (2004) Polynitroxyl hemoglobin: a pharmacokinetic study of covalently bound nitroxides to hemoglobin platforms. Free Radical Biol Med 37(1):124–135
Bunn HF, Jandl JH (1968) The renal handling of hemoglobin. Trans Assoc Am Phys 81:147
Burhop KE, Estep TE (2001) Hb induced myocardial lesions. Artf Cells Blood Subst Immob Biotech 29:101–106
Chang TMS (1957) Hemoglobin corpuscles-report of a research project for honours physiology. Medical Library, McGill University. Also reprinted in full in Chang’s 2007 Monograph on Artificial Cells
Chang TMS (1964) Semipermeable microcapsules. Science 146:524–525
Chang TMS (1965) Semipermeable aqueous microcapsules. Ph.D. Thesis, McGill University
Chang TMS (1971) Stabilisation of enzymes by microencapsulation with a concentrated protein solution or by microencapsulation followed by cross-linking with glutaraldehyde. Biochem Biophys Res Commun 44:1531–1536
Chang TMS (1972) Artificial Cells. Charles C Thomas Publisher, Springfield Illinois, USA www.artcell.mcgill.ca
Chang TMS (1976) Biodegradable semipermeable microcapsules containing enzymes hormones, vaccines, and other biologicals. J Bioeng 1:25–32
Chang, T.M.S. (1997) Red blood cell substitutes: principles, methods, products and clinical trials, vol 1. Karger/Landes Systems, Switzerland www.artcell.mcgill.ca or www.artificialcell.info)
Chang TMS (2005) Therapeutic applications of polymeric artificial cells. Nat Rev Drug Discov 4:221–235
Chang TMS (2007) Artificial cells: biotechnology, nanotechnology, blood substitutes, regenerative medicine, bioencapsulation, cell/stem cell therapy. World Scientific Publisher/Imperial College Press, UK p 435 www.artcell.mcgill.ca
Chang TMS (2009) Nanobiotechnology for hemoglobin based blood substitutes. Crit Care Clin 25:373–382
Chang TMS (2010) Blood replacement with engineered hemoglobin and hemoglobin nanocapsules. Wiley Interdiscipl Rev Nanomed Nanobiotechnol 2:418–430
Chang TMS (2011) Nanobiotechnology-based blood substitutes and the cardiovascular systems in transfusion medicine. In: Nanomedicine and cardiovascular system. TFM Publishing, UK pp 77–98
Chang TMS (2012) Artificial red blood cells, oxygen carriers, oxygen therapeutics to artificial cells and nanomedicine and beyond. Artif Cells Blood Substit Biotechnol J 40(3):197–199
Chang TMS (2013) Artif Cells Blood Substit Nanomed www.artcell.mcgill.ca
Chang EJ, Lee TH, Mun KC et al (2004) Effects of polyhemoglobin-antioxidant enzyme complex on ischemia-reperfusion in kidney. Trans Proc 36: 1952–1954
Chang TMS, Powanda D, Yu WP (2003) Analysis of polyethyleneglycol polylactide nano-dimension artificial red blood cells in maintaining systemic hemoglobin levels and prevention of methemoglobin formation. Artif Cells Blood Substit Biotechnol 31:231–248
Chang TMS, Poznansky MJ (1968) Semipermeable microcapsules containing catalase for enzyme replacement in acatalsaemic mice. Nature 218:242–245
D’Agnillo F, Chang TMS (1998) Polyhemoglobin-superoxide dismutasecatalase as a blood substitute with antioxidant properties. Nat Biotechnol 16:667–671
Deamer DW, Bangham AD (1976) Large-volume liposomes by an ether vaporization method. Biochem Biophys Acta 443:629–634
DeVenuto F, Zegna AI (1982) Blood exchange with pyridoxalated–polymerized hemoglobin. Surg Gynecol Obstet 155:342
Djordjevich L, Miller IF (1980) Synthetic erythrocytes from lipid encapsulated hemoglobin. Exp Hematol 8:584
Doherty DH, Doyle MP, Curry SR et al (1998) Rate of reaction with nitric oxide determine the hypertensive effect of cell free hemoglobin. Nat Biotechnol 16: 672–676
Dudziak R, Bonhard K (1980) The development of hemoglobin preparations for various indications. Anesthesist 29:181
Farmer MC, Rudolph AS, Vandegriff KD, Havre MD, Bayne SA, Johnson SA (1988) Lipsome–encapsulated hemoglobin: oxygen binding properties and respiratory function. Biomat Artif Cells Artif Organs 16:289–299
Feola MH, Gonzalez H, Canizaro PC, Bingham D (1983) Development of bovine stroma–free hemoglobin solution as a blood substitute. Sur Gynecol Obstet 157:399
Fratantoni JC (1994) Points to consider on efficacy evaluation of hemoglobin and perfluorocarbon based oxygen carriers. Transfusion 34:712–713
Fustier C, Chang TMS (2012) PEG-PLA nanocapsules containing a nanobiotechnological complex of polyhemoglobin-tyrosinase for the depletion of tyrosine in melanoma: preparation and in vitro characterisation 2:1
Gould SA, Sehgal LR, Sehgal HL, Moss GS (1995) The development of hemoglobin solutions as red cell substitutes: hemoglobin solutions. Trans Sci 16:5–17
Gould SA et al (2002) The life-sustaining capacity of human polymerized hemoglobin when red cells might be unavailable. J Am Coll Surg 195:445–452
Greenburg AG (2013) The clinical development of hemopure® : a selective commentary. In: Chang RMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Greenburg AG, Kim HW (1992) Evaluating new red cell substitutes: a critical analysis of toxicity models. Biomat Artif Cells Immob Biotechnol 20:575–581
Greenburg AG, Pitman A, Pearce LB, Kim HW (2008) Clinical contextualization and the assessment of adverse events in hboc trials. Artif Cells Blood Substit Biotechnol 36: 477–486
Han JQ, Yu MH, Dai M, Li HW, Xiu RJ, Liu Q (2012) Decreased expression of MDR1 in PEG-conjugated hemoglobin solution combined cisplatin treatment in a tumor xenograft model. Artif Cells Blood Substit Biotechnol 40:239–244
Hoffman SJ, Looker DL, Roehrich JM et al (1990) Expression of fully functional tetrameric human hemoglobin in Escherichia coli. Proc Natl Acad Sci USA 87:8521–8525
Hsia JC, Song DL, Er SS, Wong LTL (1992) Pharmacokinetic studies on a raffinose– polymerized human hemoglobin in the rat. Biomat Artif Cells Immob Biotechnol 20:587–596
Iwashita Y (1992) Relationship between chemical properties and biological properties of pyridoxalated hemoglobin–polyoxyethylene. Biomat Artif Cells Immob Biotechnol 20:299–308
Jahr JS, Mackenzie C, Pearce LB, Pitman A, Greenburg AG (2008) HBOC-201 as an alternative to blood transfusion: efficacy and safety evaluation in a multicenter phase III trial in elective orthopaedic surgery. J Trauma 64:1484–1497
Jia YP, Alayash AI (2013) Molecular basis of haptoglobin and hemoglobin complex formation and protection against oxidative stress and damage. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Keipert P, Chang TMS (1987) In–vivo effects of total and partial isovolemic exchange transfusion in fully conscious rats using pyridoxalated polyhemoglobin solution as a colloidal oxygen–delivery blood substitute. Vox Sanguinis 53:7–14
Keipert PE, Minkowitz J, Chang TMS (1982). Cross–linked stroma–free polyhemoglobin as a potential blood substitute. Int J Artif Organs 5(6):383
Kim HW, Greenburg AG (1997) Ferrous hemoglobin scavenging of endothelium derived nitric oxide is a principal mechanism for hemoglobin mediated vasoactivities in isolated rat thoracic aorta transfusion. Artif Cells Blood Substit Immob Biotechnol Int J 25:121–134
Klein HG (2000) The prospects for red-cell substitutes. N Engl J Med. 342(22):1666–68
Kobayashi K, Tsuchida E Horinouchi H (ed) (2005) Artificial oxygen carriers. Springer, Tokyo
Li XZ (2005) Determination of the molecular weight distribution of PEGylated bovine hemoglobin (PEG-bHb). Artif Cells Blood Substit Biotechnol Int J 33:13–28
Li T, Yu R, Zhang HH, Liang WG, Yang XM, Yang CM (2006) A method for purification and viral inactivation of human placenta hemoglobin. Artif Cells Blood Substit Biotechnol Int J
Liu ZC, Chang TMS (2008a) Effects of PEG-PLA-nano artificial cells containing hemoglobin on kidney function and renal histology in rats Artificial Cells. Blood Substit Biotechnol 36:421–430
Liu ZC, Chang TMS (2008b) Long term effects on the histology and function of livers and spleens in rats after 33 % top loading of PEG-PLA-nano artificial red blood cells. Artif Cells Blood Substit Biotechnol 36:513–524
Liu Q, Xiu RJ (2008) Proceedings of the 11th ISBS symposium at Peking union medical college, Chinese academy of medical sciences. Artif Cells Blood Substit Biotechnol Int J 36(3):169–293
Looker D, Brown D A, Cozart P et al (1992) A human recombinant hemoglobin designed for use as a blood substitute. Nature 356: 258–260
Ma L, Hsia CJC (2013) Polynitroxylated hemoglobin as a multifunctional therapeutic for critical care and transfusion medicine. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Mazurier C, Douay L, Lapillonne H (2011) Red blood cells from induced pluripotent stem cells: hurdles and developments. Curr Opin Hematol 18:249–253
Moore E, Moore FA, Fabian TC, Bernard AC, Fulda GJ, Hoyt DB et al (2009) Human polymerized hemoglobin for the treatment of hemorrhagic shock when blood is unavailable: the USA multicenter trial. J Am Coll Surg 208:1–13
Moss GS, Gould SA, Sehgal LR, Sehgal HL, Rosen AL (1988) Hemoglobin solution—from tetramer to polymer. Biomat Artif Cells Artif Organs 16:57–69
Mozzarelli A (2010) Proceedings of the 12th ISBS symposium. Artif Cells Blood Subst Biotechnol Int J 38(6):295–342
Nadithe V, Bae YH (2011a) Hemoglobin conjugates with antioxidant enzymes (hemoglobin-superoxide dismutase-catalase) via poly(ethylene glycol) crosslinker for protection of pancreatic beta RINM5F cells in hypoxia. Tissue Eng 17:2453–2462
Nadithe V, Bae YH (2011b) Hemoglobin conjugates with antioxidant enzymes (hemoglobin-superoxide dismutase-catalase) via poly(ethylene glycol) crosslinker for protection of pancreatic beta RINm5F cells in hypoxia. Tissue Eng 17:2453–2462
Natanson C, Kern SJ, Lurie P, Banks SM, Wolfe SM (2008) Cell-free hemoglobin-based blood substitutes and risk of myocardial infarction and death: a meta-analysis. JAMA 299:2304–2312
Park YK, Abuchowski A, Davis S, Davis F (1981) Pharmacology of Escherichia coli-L-asparaginase polyethylene glycol adduct. Anticancer Res 1:373–376
Pearce LB, Gawryl MS (1998) Overview of preclinical and clinical efficacy of Biopure’s HBOCs. In: Chang TMS (ed) Blood substitutes: principles, methods, products and clinical trials, vol 2. Karger, Basel, pp 82–98
Perutz MF (1980) Stereochemical mechanism of oxygen transport by hemoglobin. Proc R Soc Lond B 208:135
Philips WT, Klpper RW, Awasthi VD, Rudolph AS, Cliff R, Kwasiborski VV, Goins BA (1999) Polyethylene glyco-modified liposome-encapsulated Hb: a long circulating red cell substitute. J Pharm Exp Therapeutics 288:665–670
Powanda D, Chang TMS (2002) Cross-linked polyhemoglobin-superoxide dismutase-catalase supplies oxygen without causing blood brain barrier disruption or brain edema in a rat model of transient global brain ischemia-reperfusion. Artif Cells Blood Substit Immobil Biotechnol 30:25–42
Przybelski R, Blue J, Nanvaty M, Goldberg C, Estep T, Schmitz T (1996) Clinical studies with diaspirin cross-linked hemoglobin solution (DCLHb™): a review and update. Artif Cells Blood Substit Immob Biotechnol Int J 24:407
Rabiner SF, Helbert JR, Lopas H, Friedman LH (1967) Evaluation of stroma free hemoglobin solution as a plasma expander. J Exp Med 126:1127
Razack S, D’Agnillo F, Chang TMS (1997) Crosslinked hemoglobin-superoxide dismutase-catalase scavenges free radicals in a rat model of intestinal ischemia-reperfusion injury. Artif Cells Blood Substit Immob Biotechnology Int J 25:181–192
Robinson MF, Dupuis NP, Kusumoto T, Liu F, Menon K, Teicher BA (1995) Increased tumor oxygenation and radiation sensitivity in two rat tumors by a hemoglobin-based oxygen carrying preparation. Artif Cells Blood Substit Immob Biotechnol Int J 23:431–438
Rousselot M, Delpy E, DLRochelle C, Lagente V, Pirow R, Rees JF, Hagege A, LeGuen D, Hourdez S, Zal F (2006) Arenicola marina extracellular hemoglobin: a new promising blood substitute. Biotechnol J 1(3):333–45
Rudolph AS (1994) Encapsulated hemolgobin: current issues and future goals. Artif Cells Blood Substit Immob Biotechnol Int J 22:347–360
Sakai H (2013) Biocompatibility of a highly concentrated fluid of hemoglobin-vesicles as a transfusion alternative. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Savitsky JP, Doozi J, Black J, Arnold JD (1978) A clinical safety trial of stroma free hemoglobin. Clin Pharm Ther 23:73
Seetharama A, Acharya, Amy G, Tsai, Intaglietta M (2013) EAF PEG hemoglobins: novel class of non-hypertensive resuscitation fluids: simplicity and advantages of extension arm chemistry for PEGylation. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Sehgal LR, Rosen AL, Gould SA, Sehgal HL, Moss GS (1983) Preparation and in vitro characteristics of polymerized pyridoxalated hemoglobin. Transfusion 23:158
Sheng Y, Yuan Y, Liu C, Tao X, Shan X, Xu F (2009) In vitro macrophage uptake and in vivo biodistribution of PLA–PEG nanoparticles loaded with hemoglobin as blood substitutes: effect of PEG content. J Mat Sci Mat Med 20(9):1881–1891
Shoemaker S, Gerber SM, Evans G, Paik L, Scoggin C (Somatogen Co.USA) (1994) Initial clinical experience with a rationally designed genetically engineered recombinant human hemoglobin. Artif Cells Blood Substit Immob Biotechnol Int J 22: 457–465
Shorr RG, Viau AT, Abuchowski A (1996) Phase 1B safety evaluation of PEG hemoglobin as an adjuvant to radiation therapy in human cancer patients. Artif Cells Blood Substit Immob Biotechnol Int J 24:407
Simoni J, Simoni G, Lox CD, Prien SD, Shires GT(1997). Modified hemoglobin solution with desired pharmacological properties does not activate nuclear transcription factor NF-Kappa B in human vascular endothelial cells. Artif Cells Blood Substit Immob Biotechnol Int J 25:193–210
Sims C, Seigne P, Menconi M, Monarca J, Barlow C, Pettit J, Puyana JC (2001) Skeletal muscle acidosis correlates with the severity of blood volume loss during shock and resuscitation. J Trauma 51:1137–1146
Tam SC, Blumenstein J, Wong JT (1976) Dextran hemoglobin. Proc Natl Acad USA 73:2128
Teicher BA (1995) An overview on oxygen-carriers in cancer therapy. Artif Cells Blood Substit Immob Biotechnol Int J 23:395–405
Tsuchida E (ed) (1998) Blood substitutes: present and future perspectives. Elsevier, Amsterdam
Tsuchida E, Sakai H, Horinouchi H, Kobayashi K (2006) Artif Cells Blood Substit Immob Biotechnol Int J 34:581–588
Walder JA, Zaugg RH, Walder RY, Steele JM, Klotz IM (1979) Diaspirins that cross–link alpha chains of hemoglobin: bis(3,5–dibromosalicyl) succinate and bis(3,5–dibormosalicyl) fumarate. Biochemistry 18:4265–4270
Van der Linden P, Tadeusz SG, David J, Rene´ JH, Jan CS, _ David P, Ivo K, Andrzej ZG, Bengt F, Peter EK, Yun JH, Howard L (2011) A Double-Blind, Randomized, Multicenter Study of MP4OX for Treatment of Perioperative Hypotension in Patients Undergoing Primary Hip Arthroplasty Under Spinal Anesthesia. Anesth Analg 112:759–773
Wang Y, Chang TMS (2012) Nanobiotechnological nanocapsules containing polyhemoglobin-tyrosinase: effects on murine B16F10 melanoma cell proliferation and attachment—special issue on melanoma. J Skin Cancer http://www.hindawi.com/journals/jsc/2012/673291/
Wang Y et al (2012) Polymerized human placenta hemoglobin (PolyPHb) attenuates myocardial infarction injury in rats. Artif Cells Blood Substit Immobil Biotechnol 40(1–2):7–13
Wei G, Bian YZ, Chang TMS (2013) PLA-PEG nanoencapsulated nano artificial red blood cells that act as O2 and CO2 carrier with enhanced antioxidant activity: polyhemoglobin-superoxide dismutase-catalase-carbonic anhydrase. J Artif Cells Nanomed Biotechnol (in press)
Winslow RM (ed) (2006) Blood substitutes. Academic Press, Amsterdam
Wong JT (1988) Rightshifted dextran-hemoglobin as blood substitute. Biomater Artif Cells Artif Organs 16:237–245
Wong BL Kwok SY (2011) Method for the preparation of a heat stable oxygen carrier-containing pharmaceutical composition. US Patent 7(932):356
Wong N, Chang TMS (2007) Polyhemoglobin-fibrinogen: a novel blood substitutes with platelet-like activity for extreme hemodilution. Artif Cells Blood Substit Biotechnol 35:481–489
Wong BLS, Kwok SY, Lau SH (2011) Treatment methods using a heat stable oxygen carrier-containing pharmaceutical composition. November 2011: US 8048856
Yabuki A, Yamaji K, Ohki H, Iwashita Y (1990) Characterization of a pyridoxylated hemoglobin-polyoxyethylene conjugate as a physiologic oxygen carrier. Transfusion 30:516–20
Yu BL, Chang TMS (2004) In vitro and in vivo effects of polyhemoglobintyrosinase on murine B16F10 melanoma. Melanoma Res J 14:197–202
Yu B, Shahid M, Egorina EM, Sovershaev MA, Raher MJ, Lei C, Wu MX, Bloch KD, Zapol WM (2010) Endothelial dysfunction enhances vasoconstriction due to scavenging of nitric oxide by a hemoglobin-based oxygen carrier. Anesthesiology 112:586–594
Zapol W (2012) Proceedings of the 13th ISBS symposium at mass general hospital of Harvard medical school. Artif Cells Blood Substit Biotechnol Int J 40(3)
Zhang X, Liu C, Yuan Y, Zhang S, Shan X, Sheng Y, Xu F (2008). Key parameters affecting the initial leaky effect of hemoglobin-loaded nanoparticles are blood substitutes. J Mater Sci Mater Med. 19(6):2463–70
Zhu YJW, Chen C (2013) Glutaraldehyde polymerized porcine haemoglobin. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher/Imperial College Press, UK
Zhu XL, Chu W, Wang T, Wang F, Fan D, Dan N, Chen C (2007) Variations in dominant antigen determinants of glutaraldehyde polymerized human, bovine and porcine hemoglobin. Artif Cells Blood Substit Biotechnol 35:518–532
Zuck TF (1994) In: Winslow R (ed) Difficulties in demonstrating efficacy of blood substitutes. Artif Cells Blood Substit Immob Biotechnol Int J 22: 945–954
Acknowledgments
TMSC acknowledges the support of this research continuously since 1966 by the Medical Research Council of Canada (MRC) that is now called the Canadian Institutes of Health Research (CIHR). There are also a number of shorter term supports, in particular, the Quebec Hemovigillance and Transfusion Medicine Program under FRSQ.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Chang, T.M.S. (2013). From Hemoglobin Based Oxygen Carrier to Oxygen Therapeutics, Blood Substitutes, Nanomedicine and Artificial Cells. In: Kim, H., Greenburg, A. (eds) Hemoglobin-Based Oxygen Carriers as Red Cell Substitutes and Oxygen Therapeutics. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-40717-8_1
Download citation
DOI: https://doi.org/10.1007/978-3-642-40717-8_1
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-40716-1
Online ISBN: 978-3-642-40717-8
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)