Abstract
A group of organic acidurias, including Canavan disease (N-acetylaspartic aciduria), glutaric aciduria type I, l-2-hydroxylgutaric aciduria and d-2-hydroxyglutaric aciduria types I and II, are characterised by a predominantly or even exclusively neurological presentation and have therefore been termed ‘cerebral’. Frequent neurological symptoms are motor and/or mental retardation or regression, extrapyramidal movement disorders and epilepsy. These symptoms are the result of acute and/or chronic pathological changes in various brain regions including grey matter (cortex, basal ganglia, cerebellum) and white matter (periventricular and subcortical). Unlike ‘classic’ organic acidurias (e.g. propionic and methylmalonic aciduria), acute metabolic decompensations with hyperammonemia, metabolic acidosis and elevated concentrations of lactate and ketone bodies are uncommon for cerebral organic acidurias. Biochemically, these diseases are characterised by accumulation of characteristic organic acids, mostly dicarboxylic acids, in body fluids. At high concentrations some of these may become neurotoxic. Since the blood–brain barrier has a low transport capacity for dicarboxylic acids, cerebral accumulation of dicarboxylic acids is facilitated. Impairment of brain energy metabolism is suggested to play a central role in the pathophysiology of this disease group. Metabolic treatment initiated in neonatally diagnosed patients with glutaric aciduria type I has significantly improved the neurological outcome, whereas current treatment strategies for the other cerebral organic acidurias are ineffective.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara SummaryA group of organic acidurias, including Canavan disease (N-acetylaspartic aciduria), glutaric aciduria type I, l-2-hydroxylgutaric aciduria and d-2-hydroxyglutaric aciduria types I and II, are characterised by a predominantly or even exclusively neurological presentation and have therefore been termed ‘cerebral’. Frequent neurological symptoms are motor and/or mental retardation or regression, extrapyramidal movement disorders and epilepsy. These symptoms are the result of acute and/or chronic pathological changes in various brain regions including grey matter (cortex, basal ganglia, cerebellum) and white matter (periventricular and subcortical). Unlike ‘classic’ organic acidurias (e.g. propionic and methylmalonic aciduria), acute metabolic decompensations with hyperammonemia, metabolic acidosis and elevated concentrations of lactate and ketone bodies are uncommon for cerebral organic acidurias. Biochemically, these diseases are characterised by accumulation of characteristic organic acids, mostly dicarboxylic acids, in body fluids. At high concentrations some of these may become neurotoxic. Since the blood–brain barrier has a low transport capacity for dicarboxylic acids, cerebral accumulation of dicarboxylic acids is facilitated. Impairment of brain energy metabolism is suggested to play a central role in the pathophysiology of this disease group. Metabolic treatment initiated in neonatally diagnosed patients with glutaric aciduria type I has significantly improved the neurological outcome, whereas current treatment strategies for the other cerebral organic acidurias are ineffective.
1 Introduction
Canavan disease (Van Bogaert-Bertrand disease, N-acetylaspartic aciduria) is caused by an autosomal recessively inherited deficiency of aspartoacylase (aminoacylase 2) which is exclusively expressed in oligodendrocytes. Most patients have the infantile form which generally manifests at 2–4 months of age with head lag, muscular hypotonia and macrocephaly, progressing to marked developmental delay, seizures, optic nerve atrophy, progressive spasticity and opisthotonic posturing (Matalon et al. 1995). Death usually occurs in a few years. However, the initial symptoms may already start at or shortly after birth (neonatal form) or after the age of 5 years (juvenile form). Cranial MRI studies show diffuse or exclusively subcortical involvement of the white matter due to spongiform myelinopathy and involvement of thalamus and globus pallidus. Diagnosis can be made by finding elevated N-acetylaspartate concentrations in urine using GC/MS analysis of organic acids. A decreased aspartoacylase activity in cultured skin fibroblasts and/or the identification of two disease-causing mutations in the ASPA gene localised on 17p13.3 confirms the diagnosis. N-acetylaspartate is formed in neurons and hydrolysed to l-aspartate and acetate by oligodendrocytes. No effective treatment exists for Canavan disease. Lithium citrate decreases brain N-acetylaspartate concentrations (Assadi et al. 2010) and glyceryl triacetate treatment supplies the brain with acetate (Segel et al. 2011). Although this treatment is considered as safe, there is still no proof for its therapeutic efficacy. Adenoviral transfer of the ASPA gene to the brain has been initiated but no follow-up data have been published (Leone et al. 2000).
Glutaric aciduria type I (glutaric acidemia type I) is caused by an autosomal recessively inherited deficiency of glutaryl-CoA dehydrogenase, an FAD-dependent mitochondrial matrix enzyme. This enzyme is involved in the catabolic pathways of lysine, hydroxylysine and tryptophan, catalysing the oxidative decarboxylation of glutaryl-CoA to crotonyl-CoA. Transient muscular hypotonia and macrocephaly is often found in newborns. At this age, cranial MRI of affected individuals reveals temporal hypoplasia, dilated external CSF spaces, subependymal pseudocysts, myelination delay and an immature gyral pattern which all may improve or even resolve in early treated children (Harting et al. 2009). In the time interval between 3 and 36 (−72) months, however, most untreated patients develop a complex movement disorder best described as generalised dystonia superimposed on axial hypotonia (Gitiaux et al. 2008). These symptoms are the consequence of bilateral striatal injury which may occur acutely during acute encephalopathic crises precipitated by catabolism or insidiously without preceding crises (Kölker et al. 2006). Aside from striatal injury, MRI may show additional frontal atrophy and subdural haemorrhage. A few adolescent and adult patients with a late-onset form have been reported presenting with headaches, vertigo, reduced fine motor skills and white matter abnormalities (Harting et al. 2009). Patients can be identified in the first week of life by newborn screening using glutarylcarnitine as diagnostic parameter. Glutarate and 3-hydroxyglutarate concentrations are increased in urine and other body fluids but may be (intermittently) normal in patients with a low-excreter phenotype. Therefore, a normal organic acid analysis result does not unequivocally exclude the diagnosis. Suspected diagnosis is confirmed by significantly decreased glutaryl-CoA dehydrogenase activity in leukocytes or fibroblasts and/or the identification of two disease-causing mutations in the GCDH gene localised on 19p13.2. Glutarate and 3-hydroxyglutarate concentrations are 100–1,000-fold higher in the brain than in plasma which is caused by the very low efflux transport of dicarboxylic acids across brain capillary endothelial cells (Sauer et al. 2006). At high concentrations, accumulating dicarboxylic acids may become neurotoxic inhibiting energy metabolism (2-oxoglutarate dehydrogenase, dicarboxylate shuttle between astrocytes and neurons) and activating N-methyl-d-aspartate receptors. The development of prognostic relevant striatal injury can be prevented in the majority of children if the diagnosis is made and metabolic treatment is started neonatally (Heringer et al. 2010). Metabolic treatment according to a recently revised guideline includes a low lysine diet, carnitine supplementation and emergency treatment to counteract catabolism (Kölker et al. 2011). Patients with a high- and low-excreter phenotype have the same risk of developing striatal injury and thus receive the same treatment (Kölker et al. 2006).
l-2-hydroxyglutaric aciduria (L2HGA) is an autosomal recessive inborn error of metabolism, caused by mutations in the L2HG dehydrogenase (L2HGDH) gene. The L2HGDH gene product, i.e. L2HGDH, is an FAD-dependent membrane-bound enzyme responsible for the conversion of l-2-hydroxyglutarate (L2HG) into 2-ketoglutaric acid (2KG). The current opinion is that nonspecific mitochondrial formation of L2HG out of 2KG by l-malic dehydrogenase is the sole source of L2HG and that L2HGDH is an enzyme for metabolite repair (Van Schaftingen et al. 2009). L2HGA has an insidious onset starting in childhood with developmental delay, macrocephaly, epilepsy and cerebellar ataxia as clinical signs. In a minority of patients, the diagnosis is established in adulthood, but retrospective evaluation of the clinical course reveals an earlier subtle onset (Steenweg et al. 2010). MRI reveals disease-specific alterations characterised by predominantly subcortical cerebral white matter abnormalities and abnormalities of the dentate nucleus, globus pallidus, putamen and caudate nucleus (Steenweg et al. 2009). Metabolic investigations will reveal increased 2HG in the urinary organic acid screening, and subsequent chiral differentiation shows the increased excretion of exclusively L2HG. Apart from the massive increase of L2HG in all body fluids, a modest increase of CSF lysine is observed, while plasma lysine levels may be normal. Since the massive increase of L2HG is the major biochemical finding, pathology is likely to be explained by the pathologic levels of L2HG; however, lowered (peripheral) 2KG levels might also attribute to the disease. Currently, there is no established treatment protocol for L2HGA apart from two anecdotic reports mentioning positive effects of treatment with riboflavin and/or FAD.
d-2-hydroxyglutaric aciduria (D2HGA) type I is one of the two subtypes of D2HGA and has an autosomal recessive pattern of inheritance. The disease is caused by mutations in the D2HG dehydrogenase (D2HGDH) gene, resulting in a deficiency of d-2-hydroxyglutarate (D2HG) dehydrogenase (Struys et al. 2005). This FAD-dependent mitochondrial enzyme converts D2HG, most likely formed by the action of hydroxyacid:oxoacid transhydrogenase (HOT), into 2KG. Although several hypothetical metabolic pathways for D2HG have been proposed, there is strong evidence that D2HG is directly and exclusively formed out of 2KG (Struys et al. 2004). The disease displays a strong clinical heterogeneity from severely affected individuals to asymptomatic individuals. However, frequently reported clinical findings are developmental delay, hypotonia and epilepsy. Usually, patients are first recognised by an increase of 2HG in the urinary organic acid screening. In contrast with L2HGA, these elevations can be modest. The increase of D2HG in all body fluids is the sole biochemical alteration in this disease, and the pathophysiology of the disease is likely to be explained by this. Currently, there is no treatment. However, it can be hypothesised that in individual cases, riboflavin supplementation might be beneficial.
d-2-hydroxyglutaric aciduria (D2HGA) type II is the second form of D2HGA and is caused by a gain-of-function mutation in the isocitrate dehydrogenase 2 (IDH2) gene (Kranendijk et al. 2010). Heterozygous mutations in IDH2 result in the formation of a neomorph enzyme which is able to efficiently convert 2KG into D2HG. This is in contrast with the normal action of IDH2, i.e. the conversion of isocitrate into 2KG. D2HGA type II has an autosomal dominant trait, and in the vast majority of patients, the mutation arose de novo. The degree of D2HG accumulation in D2HGA type II is higher than in type I, despite properly functioning D2HG dehydrogenase. Patients affected with D2HGA type II suffer from developmental delay, hypotonia and epilepsy, and their clinical presentation is generally more severe than that of patients with D2HGA type I. Cardiomyopathy is frequently observed in D2HGA type II and absent in type I. The unique underlying mechanism of D2HGA type II opens perspectives to specifically inhibit the neomorph enzyme.
A most recent review covering L2HGA and both types of D2HGA was published by Kranendijk et al. (2012).
2 Nomenclature
No. | Disorder | Alternative name | Abbreviation | Gene symbol | Chromosomal localisation | Affected protein | OMIM no. | Subtype |
|---|---|---|---|---|---|---|---|---|
8.1 | Canavan disease | Van Bogaert-Bertrand disease | CD | ASPA | 17p13.3 | Aspartoacylase (aminoacylase 2) | 271900 | All forms |
8.2 | Glutaric aciduria type I | Glutaric acidemia type I | GA-I | GCDH | 19p13.2 | Glutaryl-CoA dehydrogenase | 231670 | All forms |
8.3 | l-2-hydroxyglutaric aciduria | l-2-hydroxyglutarate dehydrogenase deficiency | L2HGA | L2HGDH | 14q21.3 | l-2-hydroxyglutarate dehydrogenase | 236792 | All forms |
8.4 | d-2-hydroxyglutaric aciduria type I | d-2-hydroxyglutarate dehydrogenase deficiency | D2HGA type I | D2HGDH | 2q37.3 | d-2-hydroxyglutarate dehydrogenase | 600721 | All forms |
8.5 | d-2-hydroxyglutaric aciduria type II | Isocitrate dehydrogenase defect | D2HGA type II | IDH2 | 15q26.1 | Isocitrate dehydrogenase 2 | 613657 | All forms |
3 Metabolic Pathways
Canavan Disease
Metabolic pathway of Canavan disease. N-acetylaspartate is produced in neurons from l-aspartate and acetyl-CoA and is transported to oligodendrocytes where it is hydrolysed to l-aspartate and acetyl-CoA by aspartate aminoacylase II. Inherited deficiency of this enzyme results in accumulation of N-acetylaspartate in patients with Canavan disease
Glutaric Aciduria Type I
Metabolic pathway of glutaric aciduria type I. Glutaryl-CoA is formed within the catabolic pathways of lysine, tryptophan and hydroxylysine. The quantitatively major precursor is lysine. Deficient activity of glutaryl-CoA dehydrogenase (4) results in variable accumulation of glutaric, 3-hydroxyglutaric and glutaconic acid as well as glutarylcarnitine, which are important for the diagnosis and can be determined in body fluids. Elevated glutaryl-CoA – similarly to homologous succinyl-CoA – results in feedback inhibition of the TCA cycle enzyme 2-oxoglutarate dehydrogenase complex (3). 1 2-aminoadipic semialdehyde dehydrogenase (enzyme is deficient in pyridoxine-dependent epilepsy), 2 2-aminoadipate aminotransferase, 3 2-oxoglutarate dehydrogenase-like complex (enzyme complex contains three subunits: DHTKD1 is deficient in 2-aminoadipic/2-oxoadipic aciduria; the E2 subunit is deficient in 2-oxoglutarate dehydrogenase complex deficiency; E3 subunit (lipoamide dehydrogenase), which is shared with pyruvate dehydrogenase and branched-chain oxoacid dehydrogenase complexes, is deficient in E3 deficiency, biochemically resembling maple syrup urine disease, 2-oxoglutarate dehydrogenase complex deficiency and pyruvate dehydrogenase complex deficiency, 4 glutaryl-CoA dehydrogenase
l -2-Hydroxyglutaric Aciduria
Metabolic pathway of l-2-hydroxyglutaric aciduria. l-2-hydroxyglutaric acid is formed by a nonspecific conversion of mitochondrial 2KG into l-2-hydroxyglutaric acid by the action of NADH-dependent l-malic acid dehydrogenase. L2HG dehydrogenase corrects for this metabolic imperfection by reconverting L2HG into 2KG
d -2-Hydroxyglutaric Aciduria Type I
d -2-Hydroxyglutaric Aciduria Type II
Metabolic pathway of d-2-hydroxyglutaric aciduria type II. As a consequence of a heterozygous mutation in IDH2, the neomorph IDH2 enzyme produces vast amounts of D2HG, which exceed the capacity of D2HG dehydrogenase, an enzyme with a low Km, and as a net result, D2HG accumulates. The neomorph IDH2 enzyme consumes both 2KG and NADPH, which might lead to their shortages
4 Signs and Symptoms
5 Reference Values
6 Pathological Values
Disease 8.1 (CD): N -Acetylaspartic Acid (NAA)
Disease 8.2 (GA-I): Glutaric Acid (GA), 3-Hydroxyglutaric Acid (3-OH-GA), Glutarylcarnitine (C5DC)
Disease 8.3 (L2HGA)
Age | L2HG (U) | L2HG (P) | L2HG (CSF) |
|---|---|---|---|
mmol/mol creatinine | μmol/L | μmol/L | |
226–4,299 | 7–84 | 23–474 |
Disease 8.4 (D2HGA type I)
Age | D2HG (U) | D2HG (P) | D2HG (CSF) |
|---|---|---|---|
mmol/mol creatinine | μmol/L | μmol/L | |
103–2,414 | 26–123 | 6–18 |
Disease 8.5 (D2HGA type II)
Age | D2HG (U) | D2HG (P) | D2HG (CSF) |
|---|---|---|---|
mmol/mol creatinine | μmol/L | μmol/L | |
448–11,305 | 99–757 | 30–172 |
7 Diagnostic Flow Chart(s)
Disease 8.1 (CD)
If neurological symptoms occur and/or neuroradiological abnormalities are found (→8.5, Signs and symptoms) which are characteristic for Canavan disease, the diagnostic process should be initiated by analysis of N-acetylaspartate (NAA) in urine. If increased NAA concentrations are found, the diagnosis can be confirmed by significantly decreased aspartoacylase activity in cultured skin fibroblasts and/or the identification of two disease-causing mutations in the ASPA gene.
Disease 8.2 (GA-I)
Diagnostic flow chart for glutaric aciduria type I. A. Newborn screening for glutaric aciduria type I (GA-I) is performed using tandem mass spectrometry (MS/MS). In low-excreter cohorts with known mutations, GCDH gene mutation analysis should be considered as alternative method (dotted line). Note that in these patients, treatment should be started after the identification of two disease-causing mutations . B. Selective screening should be started if diagnosis of GA-I is suspected or a positive family history is known. Note that a few patients with a low-excreting phenotype may show (intermittently) normal urinary excretion of 3-hydroxyglutaric acid (3-OH-GA) and glutaric acid (GA). If an individual shows normal 3-OH-GA (and GA) concentrations in urine but presents with highly suspicious signs and symptoms for GA-I, it should be decided individually whether diagnostic work-up is continued (**)
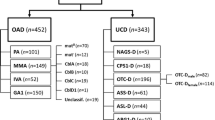
Diseases 8.3–8.5 (L2HGA, D2HGA type I and D2HGA type II)
Flowchart for the diseases 8.3, 8.4 and 8.5. The observed increase in 2HG in the urinary organic acid screening has to be pursued by an enantiomeric separation and individual quantification of both D2HG and L2HG. In case of an isolated increase of L2HG, subsequent molecular investigation of the L2HGDH gene usually reveals mutations confirming the biochemical diagnosis. In case of an isolated increase of D2HG, the diagnostic algorithm is more complicated. D2HG (whereas L2HG is within the reference range) can be secondary increased in SSADH deficiency and GA-I. If these options are excluded, molecular investigation on the two known heterozygous gain-of-function mutations will either exclude or confirm mutated IDH2 as the cause of the D2HG increase. If IDH2 molecular studies are negative, the D2HGDH gene should be investigated for the presence of mutations
8 Specimen Collection
Disease no. | Symbol | Test | Preconditions | Material | Handling | Pitfalls |
|---|---|---|---|---|---|---|
8.1 | CD | Organic acids (NAA) | None | Urine | Keep frozen (−20 °C) | Compound has poor recovery in organic solvent extraction |
8.2 | GA-I | Quantitative amino acids | 3.5–4 h postprandially, no dietary changes prior to the test | Plasma | Keep frozen (−20 °C) | |
Trytophan | 3.5–4 h postprandially, no dietary changes prior to the test | Plasma | Keep frozen (−20 °C) | Losses due to inappropriate deproteinisation | ||
Organic acids (3-OH-GA, GA) | None | Urine | Keep frozen (−20 °C) | Reliable identification of 3-OH-GA may require the use of a quantitative GC/MS method; differential diagnoses of elevated GA and 3-OH-GA include GA-II and GA-III, SCHAD deficiency and ketosis | ||
Carnitine status | None, also informs on adherence to carnitine supplementation | Plasma serum | Keep frozen (−20 °C) | |||
Acylcarnitine profile (C5DC) | None | Dried blood spots | Plasma, keep frozen (−20 °C) | C5DC may be also elevated in GA-II, renal insufficiency, MCAD deficiency (pseudoglutarylcarnitinemia) | ||
Plasma | ||||||
Enzyme activity (GCDH) | None | Fibroblasts | RT | |||
Leukocytes from heparinised blood | Keep frozen (−20 °C) | |||||
8.3 | L2HGA | Organic acids | None | Urine | Keep frozen (−20 °C) | For specific quantification of L2HG enantiomeric separation, hyphenated to mass spectrometry is required |
L2HGA | L2HG dehydrogenase activity | Isolation of cells according to specific protocol | Fibroblasts, lymphoblasts, lymphocytes | RT, pellets should be frozen | ||
8.4 | D2HGA type I | Organic acids | None | Urine | Keep frozen (−20 °C) | For specific quantification of D2HG enantiomeric separation, hyphenated to mass spectrometry is required |
D2HGA type I | D2HG dehydrogenase activity | Isolation of cells according to specific protocol | Fibroblasts, lymphoblasts | RT, pellets should be frozen | ||
8.5 | D2HGA type II | Organic acids | None | Urine | Keep frozen (−20 °C) | For specific quantification of D2HG enantiomeric separation, hyphenated to mass spectrometry is required D2HG also accumulates GA-I and SSADH |
D2HGA type II | IDH2 gain-of-function assay | Isolation of cells according to specific protocol | Lymphoblasts | RT, pellets should be frozen |
9 Treatment Summary
Effective metabolic treatment has only been described for glutaric aciduria type I (low lysine diet, carnitine supplementation, emergency treatment). Riboflavin should be considered as a treatment option for patients with l-2-hydroxyglutaric aciduria aiming to activate residual enzyme activity. Treatment of patients’ Canavan disease with lithium citrate, lowering brain N-acetylaspartate concentrations, and glycerol triacetate, supplying the brain with acetate, is considered as safe; however, it is yet unknown whether it helps to improve the outcome. Metabolic treatment for d-2-hydroxyglutaric aciduria type I and II has not yet been described.
Although effective treatment is only known for some cerebral organic acidurias, symptomatic and supportive treatment is important. This includes adequate supply with nutrient, minerals and micronutrients, physiotherapy, occupational therapy and pharmacotherapy of epilepsy and extrapyramidal movement disorder among others. The therapeutic concept should be implemented after the assessment of individual needs and, subsequently, monitored and evaluated by an interdisciplinary team of specialists.
Emergency Treatment Table for All Disorders of Your Chapter (If Applicable) and Medication Requirements (A. Including Box After the Table, with Pitfalls and Important Information)
Diseases 8.1 and 8.3–8.5
No emergency treatment is available.
Disease 8.2 (GA-I)
Emergency treatment is thought to be the most effective component of current treatment strategies to prevent acute striatal injury during infectious disease and for other causes of catabolism in glutaric aciduria type I (Heringer et al. 2010). It must be initiated before the onset of severe neurological signs, which already indicate the manifestation of neuronal damage. Therefore, during episodes that are likely to induce catabolism (e.g. infectious disease) emergency treatment should start without delay. Treatment should consist of frequent high carbohydrates feeds and increased carnitine supplementation, followed by high-dose intravenous glucose and carnitine (Kölker et al. 2011). All patients with glutaric aciduria type I should be supplied with an emergency card. This concept should be strictly followed for the first 6 years of life. After this age emergency treatment is individually adjusted.
Standard Treatment Table for All Disorders of Your Chapter (if applicable) and Medication Requirements (A. Including Box After the Table, with Pitfalls and Important Information)
Diseases 8.1, 8.3, 8.4 and 8.5
No specific treatment is available.
Disease 8.2 (GA-I)
Disorder no. | Symbol | Age | Medication/diet | Dosage | Doses/day (n) |
|---|---|---|---|---|---|
8.2 | GA-I | <6 years | Carnitine | (50–) 100 mg/kg per day | 3 |
>6 years | Carnitine | (30–) 50 mg/kg per day | 3 | ||
Riboflavina | 100 mg | 2 | |||
Treatment of extrapyramidal movement disordersb | |||||
Antiepileptic treatmentc | |||||
Diet (see below) |
Dangers/Pitfalls
-
1.
Dietary treatment needs to be adapted to the individual needs, in particular in dystonic patients. Overtreatment by protein restriction may result in malnutrition with essential nutrients.
-
2.
Dysphagia is a frequent problem in dystonic patients. Tube feeding (via nasogastric tube or percutaneous gastrostomy) should be considered if oral food intake is inadequate.
Experimental Treatment for All Disorders of Your Chapter (If Applicable) and Medication Requirements (A. Including Box After the Table, with Pitfalls and Important Information)
Disease no. | Symbol | Alternative therapies/experimental trials |
|---|---|---|
8.1 | CD | Lithium citrate |
Glycerol triacetate | ||
Gene therapy | ||
8.2 | GA-I | Arginine or homoarginine supplementation has yet only been studied in GCDH-deficient mice, an animal model for GA-I, and in a small number of patients (arginine) |
8.3 | L2HGA | Riboflavin supplementation |
8.4 | D2HGA type I | On the basis that D2HG dehydrogenase is an FAD-dependent enzyme, riboflavin supplementation is a therapeutic option |
8.5 | D2HGA type II | Development of specific inhibitor of the IDH2 mutant enzyme |
References
Assadi M, Janson C, Wan DJ et al (2010) Lithium citrate reduces excessive intracerebral N-acetylaspartate in Canavan disease. Eur J Paediatr Neurol 14:354–359
Gitiaux C, Roze E, Kinugawa K et al (2008) Spectrum of movement disorders associated with glutaric aciduria type 1: a study of 16 patients. Mov Disord 23:2392–2397
Harting I, Neumaier-Probst E, Seitz A et al (2009) Dynamic changes of striatal and extrastriatal abnormalities in glutaric aciduria type I. Brain 132:1764–1782
Heringer J, Boy SPN, Ensenauer R et al (2010) Use of guidelines improves the neurological outcome in glutaric aciduria type I. Ann Neurol 68:743–752
Kölker S, Garbade S, Greenberg CR et al (2006) Natural history, outcome, and treatment efficacy in children and adults with glutaryl-CoA dehydrogenase deficiency. Pediatr Res 59:840–847
Kölker S, Christensen E, Leonard JV et al (2011) Diagnosis and management of glutaric aciduria type I – revised recommendations. J Inherit Metab Dis 34:677–694
Kranendijk M, Struys EA, Van Schaftingen E et al (2010) IDH2 mutations in patients with D-2-hydroxyglutaric aciduria. Science 330:336
Kranendijk M, Struys EA, Salomons GS, Van der Knaap MS, Jakobs C (2012) Progress in understanding 2-hydroxyglutaric acidurias. J Inherit Metab Dis 35(4):571–587
Leone P, Janson CG, Bilanuk L et al (2000) Aspartoacylase gene transfer to the mammalian central nervous system with therapeutic implications for Canavan disease. Ann Neurol 48:27–38
Matalon R, Michals K, Kaul R (1995) Canavan disease: from spongy degeneration to molecular analysis. J Pediatr 127:511–517
Sauer SW, Okun JG, Fricker G et al (2006) Intracerebral accumulation of glutaric and 3-hydroxyglutaric acids secondary to limited flux across the blood–brain barrier constitutes a biochemical risk factor for neurodegeneration in glutaryl-CoA dehydrogenase deficiency. J Neurochem 97:899–910
Segel R, Anikster Y, Zevin S et al (2011) A safety trial of high glucose triacetate for Canavan disease. Mol Genet Metab 103:203–206
Steenweg ME, Salomons GS, Yapici Z et al (2009) L-2-Hydroxyglutaric aciduria: pattern of MR imaging abnormalities in 56 patients. Radiology 2009(251):856–865
Steenweg ME, Jakobs C, Errami A et al (2010) An overview of L-2-hydroxyglutarate dehydrogenase gene (L2HGDH) variants: a genotype-phenotype study. Hum Mutat 31:380–390
Struys EA, Verhoeven NM, Brunengraber H et al (2004) Investigations by mass isotopomer analysis of the formation of D-2-hydroxyglutarate by cultured lymphoblasts from two patients with D-2-hydroxyglutaric aciduria. FEBS Lett 557(1–3):115–120
Struys EA, Salomons GS, Achouri Y et al (2005) Mutations in the D-2-hydroxyglutarate dehydrogenase gene cause D-2-hydroxyglutaric aciduria. Am J Hum Genet 76:358–360
Van Schaftingen E, Rzem R, Veiga-da-Cunha M (2009) L-2-hydroxyglutaric aciduria, a disorder of metabolite repair. J Inherit Metab Dis 32:135–142
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Kölker, S., Struys, E.A., van der Knaap, M.S., Jakobs, C. (2014). Cerebral Organic Acidurias. In: Blau, N., Duran, M., Gibson, K., Dionisi Vici, C. (eds) Physician's Guide to the Diagnosis, Treatment, and Follow-Up of Inherited Metabolic Diseases. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-40337-8_8
Download citation
DOI: https://doi.org/10.1007/978-3-642-40337-8_8
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-40336-1
Online ISBN: 978-3-642-40337-8
eBook Packages: MedicineMedicine (R0)