Abstract
The management of osteonecrosis (ON) remains one of the more perplexing problems facing the orthopedic surgeon. There is still much to be learned about the etiology, pathophysiology, and management of this condition. Because prognosis and treatment are determined in large part by the stage of the disease, it is important to use a reliable and efficient method of evaluation and staging. The uniform use of such a system of classification would also enable us to compare the effectiveness of various methods of treatment and determine the best method of management for different stages of osteonecrosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The management of osteonecrosis (ON) remains one of the more perplexing problems facing the orthopedic surgeon. There is still much to be learned about the etiology, pathophysiology, and management of this condition. Because prognosis and treatment are determined in large part by the stage of the disease, it is important to use a reliable and efficient method of evaluation and staging. The uniform use of such a system of classification would also enable us to compare the effectiveness of various methods of treatment and determine the best method of management for different stages of osteonecrosis.
During the 1970s we began to see a steady increase in the number of patients with osteonecrosis being treated at our institution. In attempting to evaluate these patients, we found that the classification systems in use at that time were helpful, but none was ideal [1, 2]. These included the classifications of Ficat and Arlet [3, 4]; the system of Marcus, Enneking, and Massam [5]; the use of angular measurements described by Kerboul [6]; and the radiographic staging of Sugioka [7]. We therefore felt that it would be valuable to formulate a new, comprehensive, and quantifiable system of classification and staging. Initially we set down the parameters to be included in an ideal system:
-
It should correspond closely to the pathologic and radiographic changes that occur in osteonecrosis.
-
It should clearly and distinctly characterize each separate stage.
-
In addition to the stage, it must allow us to measure and indicate both the size of the necrotic lesion and the extent of joint involvement.
-
It should be objective, simple to use, and reproducible.
-
It should allow us to trace progression or resolution from the earliest to the latest stages.
-
Symptoms and physical findings, although important in management, should not be part of the classification itself.
-
Older, invasive techniques should be eliminated and newer diagnostic modalities such as MRI must be included.
-
The system should allow for the future development of even more sensitive methods of diagnosis and evaluation.
-
Its effectiveness should be established in actual clinical use and its advantages over other systems should be documented.
In 1979, in conjunction with our colleagues in the Department of Radiology, we began to develop a quantitative method for classification and staging which would include the parameters outlined above. Initially, technetium scans and computerized tomography were used to identify pre-radiographic lesions. By 1982 we had begun to use nuclear magnetic resonance (NMR) – later designated as magnetic resonance imaging (MRI) [8–10]. We examined 55 hips with biopsy-proven ON which were studied by radiographs, technetium scans, CT, and MRI. We found MRI to be the single most effective method for early diagnosis of this condition with a high degree of sensitivity and specificity. It was found to be significantly more accurate in diagnosis of pre-radiographic lesions than either technetium scans or CT. On the basis of these studies, MRI became an integral part of our staging system, and CT and technetium scans were rarely used [11, 12].
The classification that was developed was presented in 1982 at the Third International Symposium on Circulation in Bone in Toulouse, France, and published in 1984 [13]. Initially the type of pathologic change identified on imaging studies is used to place the hip in one of seven stages. Once the stage has been determined, the size of the necrotic segment and the extent of involvement of the femoral head and acetabulum are indicated as mild (A), moderate (B), or severe (C). For routine clinical use a simple estimate of the extent of involvement is sufficient, whereas for research projects and publications, it can be measured [11, 14] (Table 25.1).
1.1 Determining Stage
-
Stage 0. Stage 0 indicates that a hip is suspected of having ON although radiographs and MR are normal or nondiagnostic, such as a painful hip in a patient with proven ON in the opposite hip. Stage 0 would include hips evaluated too soon after a precipitating event for changes to appear or hips with too small an area of involvement to be detected with current modalities. The diagnosis might be made some time after the original evaluation when the lesion appears on imaging studies. A definitive diagnosis in stage 0 will also most likely be possible in the future with further refinements in our diagnostic techniques. Thus, inclusion of stage 0 will extend the useful life of this classification.
-
Stage I. Plain radiographs are normal, but MRI and/or technetium scans indicate the presence of ON.
-
Stage II. Radiographs now show definitive abnormalities consistent with ON. These consist of radiolucent and/or sclerotic regions, at times demarcated from normal bone by a sclerotic border. Rarely, the earliest radiographic findings will include generalized osteopenia of the femoral head.
-
Stage III. Stage III is diagnosed by the appearance of a radiolucent crescent line just beneath the subchondral end plate, but without flattening of the femoral head. This indicates collapse of the cancellous trabeculae beneath an intact articular surface. A crescent sign does not always appear as the head progresses from earlier to later stages and may be seen in only one radiographic projection. A relatively small percentage of hips will fit the criteria for stage III. However, we feel that they should be assigned a separate stage rather than being grouped together with hips which show gross flattening of the articular surface because clinical experience documents a better outcome for hips in stage III than for hips in stage IV, where flattening is already present [1, 15–18]. The hip is still spherical at this stage and it is theoretically possible to preserve its normal anatomy by bone grafting or other procedures.
-
Stage IV. There is now definite flattening of the femoral head which appears in either the AP, lateral, or both views. Occasionally small areas of collapse cannot be seen on plain radiographs but can be detected with CT. The acetabulum appears radiographically normal at this stage. However, early changes in the acetabular cartilage have been identified in the majority of stage IV hip patients whose pain and disability were sufficient for them to require arthroplasty. Stage IV has serious implications, because irreversible changes have taken place and a “normal” femoral head cannot be anticipated despite appropriate treatment.
-
Stage V. In addition to flattening of the femoral head, there is now clear radiographic evidence of joint line narrowing and later sclerosis and cystic changes in the acetabulum. Progressive degenerative changes follow.
-
Stage VI. Degenerative changes in both the femoral head and acetabulum have progressed to the point where the joint line is virtually obliterated and marked deformity appears. Other staging systems have grouped stages V and VI together; however, a small but definite number of hips develop changes so advanced that they can be distinguished from stage V. We thus feel that they deserve a separate designation and this allows us to follow progression more accurately.
1.2 Determining Extent of Involvement
After the type of radiographic and pathologic changes has determined the stage, the extent of involvement is next estimated or measured. For clinical purposes it is adequate to make a simple estimate and to describe this as mild (A), moderate (B), or severe (C). However, for research purposes it is preferable to make actual measurements as described below. No attempt is made to quantify the extent of involvement in stages 0 or VI.
In stages I and II the three-dimensional size or volume of the necrotic lesion is determined and expressed as a percentage of the entire head. In stage I this is estimated or calculated from serial MRI sections. In stage II, the MRI can be used in a similar fashion if it is available. However, in many cases where the lesion is clearly seen on radiographs, MRI will not be available and several methods can be used to determine the lesion size from plain radiographs. The most accurate involve the use of computerized image analysis. However, a reasonable estimate of lesion size has been made by some investigators using different types of angular measurements or by a simple visual estimate [1, 2, 6, 19–23].
In stage III it is first determined whether the crescent sign is more prominent in the AP or the lateral view. This view is then used to measure the length of the crescent and to express it as a percent of the length of the entire articular surface of the femoral head. This can be done with modern imaging techniques. If not available, one can use a map reading planimeter, a specially designed grid, or simple angular measurements.
In stage IV, as in stage III, measurements are made on either the AP or the lateral film, whichever shows the greatest amount of collapse. The normal contour of the femoral head before collapse is reconstituted, and then the length of the collapsed segment is measured and expressed as a percentage of the entire articular surface. The maximum depression of the collapsed segment is also measured and expressed in millimeters. This can be done as described for stage III.
In stage V the length of the collapsed segment and the amount of collapse of the femoral head are determined as described above. The degree of acetabular involvement is then estimated. The average of the femoral head and acetabular involvement determines the overall grade.
More detailed information about the University of Pennsylvania Classification can be found in our earlier publications [13, 14, 21]. These include a specific description of the methods originally used to measure lesion size and the extent of joint involvement. However, a number of technological advances using image analysis software have been made since that time, making it simpler and more accurate to obtain these measurements [22, 24].
2 Evaluation and Comparison with Other Classifications
The two most important features of the University of Pennsylvania Classification are the incorporation of MRI and specific measurements of lesion size as integral parts of the system. Both of these are now recognized as essential for inclusion in any effective classification. MRI is the single best modality for the early diagnosis of ON, before changes appear on radiographs. Its sensitivity and specificity have been confirmed [1, 10–12, 22–25]. Its use has made invasive mechanism for diagnosis, scintigraphy, and CT no longer necessary.
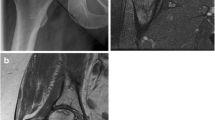
It is well established that the prognosis and hence the treatment of hips with ON is directly related to the size of the necrotic region even within the same stage [1, 15, 17–20, 22, 23, 26]. It is therefore essential to include an accurate measurement of lesion size as an integral part of the classification. This allows us to establish a prognosis, follow progression or resolution, compare different methods of treatment, and determine the best management for a patient with osteonecrosis. These represent significant improvements over older methods of classification which indicated only the stage and not the extent of involvement (Fig. 25.1).
The importance of lesion size is further supported by the number of more recent publications which describe alternate methods of measurement [19, 20, 23]. Several of these use angular measurements made on radiographs or MRI. Essentially all of these techniques have demonstrated some degree of correlation between lesion size and outcome. However, it is virtually impossible to determine which is more accurate because of the large number of variables involved, including the different methods of management they are used to evaluate. Although these techniques are useful and relatively simple to use, they cannot provide an accurate measurement of an irregular three-dimensional lesion. Neither are they designed to measure the extent of femoral head flattening or joint involvement. These techniques have been used to supplement an older, non-quantitative classification, such as that of Ficat and Arlet, and have not been incorporated into a comprehensive classification [2, 21].
Concern has been expressed that the University of Pennsylvania Classification may be too complex for general use. This concern has led to support for simpler methods to measure the size of the necrotic region such as the angular measurements described. It should be noted that the use of modern techniques of image analysis have simplified our ability to obtain accurate measurements compared to our original methods. In addition, both we and other investigators have found that visual estimates of lesion size made from radiographs or MRI by experienced examiners are both simple to obtain and reasonably accurate [2, 20, 21, 24].
Attempts to simplify this classification have also led some to combine our stages III and IV and eliminate stage VI. However, it has been shown that the prognosis and hence the management is different for hips with subchondral collapse alone (stage III), from hips with flattening of the articular surface (stage IV) [1, 15, 16, 18, 26]. Thus, not distinguishing between these stages has inherent disadvantages. This has also been supported by Arlet and Ficat who expanded their four-part classification to six parts to include a transition stage [3, 4, 27].
It has also been suggested that this classification be modified by adding an additional parameter of evaluation which combines the location with the size of the necrotic region [28, 29], as proposed by the Japanese Investigation Committee [30]. However, it is well established that the majority of necrotic lesions involve the anterolateral aspect of the femoral head and attempting to classify them as medial, central, or lateral does not accurately reflect the pathophysiology of ON. This modification would make the classification unnecessarily complex and provide little additional information [2, 26, 31, 32].
There are several other features of ON which are important to consider. For example, clinical evaluation of the patient with ON is, of course, essential to determine management. However, there is often little correlation between the radiographic stage and a patient’s symptoms or physical findings, and therefore they are not included in this staging system. Whether the necrotic region appears primarily radiolucent or sclerotic may correlate with outcome. This should be noted, but likewise this is not part of the classification per se. We sought to include the most important factors but tried to prevent the system from becoming so complex as to be unwieldy.
The University of Pennsylvania Classification has been in use essentially unchanged since 1982. It has been used clinically to evaluate numerous patients with ON of the hip or shoulder, has been described in several publications, and specifically cited over 253 times. It was endorsed in 1991 by the ARCO Committee on Terminology and Staging [33], although it was modified in 1992 [29] and 1993 [34]. In 1992 it was also endorsed by the Committee on the Hip of the American Academy of Orthopaedic Surgeons. The essential parts of the system have been validated [14, 22, 24, 26], and it has proven itself quite useful in the evaluation and management of patients with ON. It has allowed us to develop an effective algorithm for the treatment of patients with osteonecrosis.
A recent review of articles on the treatment of ON, published in the past 25 years, showed that, although non-quantitative classifications are still frequently used and the four-part classification of Ficat and Arlet [4] is still the most often cited, there has been a steady trend towards the use of more comprehensive, quantitative systems of staging. The University of Pennsylvania Classification was cited next in frequency to that of Ficat and Arlet [32, 35].
3 Summary and Conclusions
The University of Pennsylvania Classification of osteonecrosis was first presented in 1982 at the Third International Symposium on Circulation in Bone and published in 1984. It was designed to identify each of the pathophysiologic changes which take place in joints afflicted by osteonecrosis, from the earliest to the most advanced. Seven specific stages were described based upon the type of change present. The extent of involvement was then identified and indicated by “A” (mild), “B” (moderate), or “C” (severe). To the best of our knowledge, this was the first classification to include both MRI and the extent of involvement as integral parts of a comprehensive method of evaluation and staging. It has withstood the test of time, has been validated, and has been described and cited in many publications. It allows us to establish a prognosis, follow progression or resolution, compare different methods of treatment, and determine the best method of management for a patient with osteonecrosis. It has proven more effective than earlier, non-quantitative methods of staging and has improved our ability to evaluate and treat patients with osteonecrosis. It is being used with increasing frequency by investigators treating and studying patients with osteonecrosis.
References
Steinberg ME. Diagnostic imaging and the role of stage and lesion size in determining outcome in osteonecrosis of the femoral head. Tech Orthop. 2001;16(1):6–15.
Steinberg ME, Steinberg DR. Classification systems for osteonecrosis: an overview. Orthop Clin North Am. 2004;35:273–83.
Arlet J, Ficat RP. Forage-biopsie de la tete femorale dans l’osteonecrose primitive. Observations histopathologiques portant sur huit foranes. Rev Rhum. 1964;31:257–64.
Ficat RP, Arlet J. Necrosis of the femoral head. In: Hungerford DS, editor. Ischemia and necrosis of bone. Baltimore: Williams and Wilkins; 1980. p. 53–74.
Marcus ND, Enneking WF, Massam RA. The silent hip in idiopathic aseptic necrosis: treatment by bone grafting. J Bone Joint Surg Am. 1973;55:1351–66.
Kerboul M, Thomine J, Postel M, Merle D’Aubigne R. The conservative surgical treatment of idiopathic aseptic necrosis of the femoral head. J Bone Joint Surg Br. 1974;56:291–6.
Sugioka Y, Katsuki I, Hotokebuchi T. Transtrochanteric rotational osteotomy of the femoral head for the treatment of osteonecrosis: follow-up statistics. Clin Orthop. 1982;169:115–25.
Axel L, Thickman D, Kressel HY, Weingrad T, Steinberg ME, Chen H, Edelstein W. NMR imaging of avascular necrosis. Magn Reson Med. 1984;1:93–4.
Steinberg ME, Chen HH, Thickman D, Alavi KA, Axel L, Fallon M, Kressel HY, Steinberg DR, Velchick MG. Early diagnosis of avascular necrosis by nuclear magnetic resonance. Orthop Trans. 1985;9(3):419.
Mitchell MD, Kundel HL, Steinberg ME, Kressel HY, Alavi A, Axel L. Avascular necrosis of the hip: comparison of MR. CT and scintigraphy. AJR Am J Roentgenol. 1986;147:67–71.
Steinberg ME, Brighton CT, Steinberg DR, Tooze SE, Hayken GD. Treatment of avascular necrosis of the femoral head by a combination of bone grafting, decompression, and electrical stimulation. Clin Orthop Relat Res. 1984;186:137–53.
Steinberg ME. Early diagnosis of avascular necrosis of the femoral head. Instructional course lectures. Published by the American Academy of Orthopaedic Surgeons. Vol 37. p. 51–7. Chapter 6; 1988.
Steinberg ME, Hayken GD, Steinberg DR. A new method for evaluation and staging of avascular necrosis of the femoral head. In: Arlet J, Ficat RP, Hungerford DS, editors. Bone circulation. Baltimore: Williams and Wilkins; 1984. p. 398–403.
Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77:34–41.
Mont MD, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88:1117–32.
Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;405:14–23.
Steinberg ME, Bands RE, Parry S, Hoffman E, Chan T, Hartman KM. Does lesion size affect the outcome in avascular necrosis? Clin Orthop. 1999;367:262–71.
Steinberg ME, Larcom PG, Strafford B, Hosick WB, Corces A, Bands RE, Hartman KE. Core decompression with bone grafting for osteonecrosis of the femoral head. Clin Orthop Relat Res. 2001;386:71–8.
Koo K-H, Kim R. Quantifying the extent of osteonecrosis of the femoral head: a new method using MRI. J Bone Joint Surg Br. 1995;77:875–80.
Cherian SF, Laorr A, Saleh KJ, et al. Quantifying the extent of femoral head involvement is osteonecrosis. J Bone Joint Surg Am. 2003;85:309–15.
Steinberg DR, Steinberg ME, Garino JP, Dalinka M, Udupa JK. Determining lesion size in osteonecrosis of the femoral head. J Bone Joint Surg. 2006;88-A(Supplement 3):27–34.
Hernigou P, Lambotte SC. Volumetric analysis of osteonecrosis of the femur: anatomical correlation using MRI. J Bone Joint Surg Br. 2001;83-B:672–5.
Ha YC, Jung WH, Kim JR, et al. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006;88(Supp 3):35–40.
Theodorou DJ, Malizos KN, Beris AE, Theodorou SF, Soucacos PN. Multimodal imaging quantitation of the lesion size in osteonecrosis of the femoral head. Clin Orthop. 2001;386:54–63.
Thickman D, Axel L, Kressel HY, Steinberg M, Chen H, Velchick M, Fallon M, Dalinka M. Magnetic resonance imaging of avascular necrosis of the femoral head. Skeletal Radiol. 1986;15:133–40.
Mont MA, Jones LC, Pacheo I, Hungerford DS. Radiographic predictors of outcome of core decompression for osteonecrosis stage III. Clin Orthop. 1998;354:159–68.
Ficat RP. Idiopathic bone necrosis of the femoral head: early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9.
ARCO Committee on Terminology and Staging. Gardeniers JWM, Chairman. The ARCO perspective for reaching one uniform staging system of osteonecrosis. In: Schoutens A, Arlet J, Gardeniers JWM, Huges SPF, editors. Bone circulation and vascularization in normal and pathological conditions. New York/London: Plenum Press and NATO Scientific Affairs Division; 1993. p. 375–80.
Gardeniers J. A New international classification of osteonecrosis of the ARCO committee on terminology and classification. ARCO Newsl. 1992;4:41–6.
Sugano J, Atsumi T, Ohzone K, et al. The 2001 revised criteria for diagnosis, classification and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci. 2002;7(5):601–5.
Sugano N, Takaoka K, Ohzono K, Matsui M, Masuhara K, One K. Prognostication of non-traumatic avascular necrosis of the femoral head: significance of location and size of the necrotic lesion. Clin Orthop. 1994;303:155–64.
Mont MA, Marulanda GA, Jones LC, Saleh KJ, Gordon N, Hungerford DS, Steinberg ME. Systematic analysis of classification systems for osteonecrosis of the femoral head. J Bone Joint Surg. 2006;88-A(Supplement 3):16–26.
Gardeniers J. ARCO committee on terminology and staging. A new proposition of terminology and an international classification of osteonecrosis. ARCO Newsl. 1991;3:153–9.
Gardeniers J. ARCO Committee on terminology and staging report on the committee meeting at Santiago de Compostela. ARCO Newsl. 1993;5:79–82.
Lee GC, Steinberg ME. Are we evaluating osteonecrosis adequately? Int Orthop (SICOT). 2012;36:2433–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Steinberg, D.R., Steinberg, M.E. (2014). The University of Pennsylvania Classification of Osteonecrosis. In: Koo, KH., Mont, M., Jones, L. (eds) Osteonecrosis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-35767-1_25
Download citation
DOI: https://doi.org/10.1007/978-3-642-35767-1_25
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-35766-4
Online ISBN: 978-3-642-35767-1
eBook Packages: MedicineMedicine (R0)