Abstract
The primary pathophysiologic feature of advanced osteonecrosis is a zone of necrotic bone containing trabeculae with dead osteocytes associated with marrow necrosis and fibrosis [1]. This pathognomonic feature led to the use of the expression “avascular necrosis,” although the international society for the study of the circulation to bone and its disorders, ARCO International (Association Internationale pour la Recherche sur la Circulation Osseuse), recommends using the term “osteonecrosis.” There are several theories regarding the pathogenesis of osteonecrosis [ON], as discussed in several outstanding review articles [2–6]. These can be categorized as (1) extraosseous, (2) intraosseous, or (3) direct cellular. There are many other theories as well, such as intravascular or extravascular pathologies. John Paul Jones, Jr., suggested that multiple etiologies may lead to a final common pathway of intravascular coagulation. He hypothesized that intravascular coagulation is an “intermediary mechanism” in the development of ON [7]. The evidence that intravascular coagulation plays an integral role in the pathogenesis of ON is both direct and indirect and will be the focus of this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
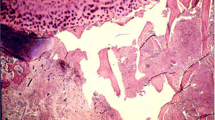
The primary pathophysiologic feature of advanced osteonecrosis is a zone of necrotic bone containing trabeculae with dead osteocytes associated with marrow necrosis and fibrosis [1]. This pathognomonic feature led to the use of the expression “avascular necrosis,” although the international society for the study of the circulation to bone and its disorders, ARCO International (Association Internationale pour la Recherche sur la Circulation Osseuse), recommends using the term “osteonecrosis.” There are several theories regarding the pathogenesis of osteonecrosis [ON], as discussed in several outstanding review articles [2–6]. These can be categorized as (1) extraosseous, (2) intraosseous, or (3) direct cellular. There are many other theories as well, such as intravascular or extravascular pathologies. John Paul Jones, Jr., suggested that multiple etiologies may lead to a final common pathway of intravascular coagulation. He hypothesized that intravascular coagulation is an “intermediary mechanism” in the development of ON [7]. The evidence that intravascular coagulation plays an integral role in the pathogenesis of ON is both direct and indirect and will be the focus of this chapter.
2 Clinical Laboratory Assessments
In 1970, Boettcher et al. reported the results of clinical and laboratory testing of 50 patients with nontraumatic osteonecrosis [8]. The patients underwent a battery of hematological and coagulation tests including ESR (erythrocyte sedimentation rate), platelet number, thrombin time, and prothrombin utilization. Direct evidence of a clotting abnormality was detected in 26 patients and indirect evidence in 48 patients. However, no specific test was “consistently abnormal.” For example, for platelet counts, 16 patients were normal, 15 patients had low counts (thrombocytopenic), and 6 patients had elevated counts (thrombocythemia). The authors propose that any of the vascular abnormalities could “cause circulatory disturbance and infarction when anastomoses are insufficient to maintain viability of the head” [8]. Using the clot lysis test, Pósán et al. observed a significantly lower “speed of the lysis” for patients with either primary or secondary ON [9]. Using an assay for beta-thromboglobulin, they also noted significantly higher platelet activation in the ON patients compared to controls.
Thrombophilia (increased clots in blood vessels) and hypofibrinolysis (decreased ability to break down clots) have both been implicated as “causative factors” for osteonecrosis [5]. Several investigators have identified thrombi within the arterial and venous circulation of diseased femoral heads (Table 10.1). In their evaluation of human biopsy samples, Ficat and Arlet frequently observed sinusoidal distension, thickening of the arteriolar walls, and arteriolar thrombosis [1]. In three cases of osteonecrosis, Jones observed fibrin thrombi in the subchondral Haversian capillaries, arterioles, and marrow sinusoids [14]. He also noted microfocal marrow hemorrhages with extravasated erythrocytes. Jones suggested that the intravascular thrombosis of the intraosseous arterioles was initiated by lipid embolism and endothelial damage [7, 22]. Saito et al. also observed thrombosed intraosseous arterioles associated with damage to the vascular wall [12]. Starklint and colleagues observed dilated veins and venules within the transitional zone between the necrotic lesion and the “normal” bone [17]. Using the Martius Scarlet Blue stain, tightly packed erythrocytes and fibrin thrombi were detected within these blood vessels, suggesting that the dilated vessels are a consequence of thrombi in other areas. There is, however, considerable debate as to the role of thrombi in the pathogenesis of ON and whether, if it exists at all, it is a primary or secondary event [23]. The lack of thrombi in some histological sections has been explained away by some as a result of the delay in the timing of histological sampling from the onset of disease and that thrombolysis had removed the implicating stimulus [14].
Many of the comorbidities associated with osteonecrosis are also associated with vascular pathologies (Table 10.2). For example, systemic lupus erythematosus (SLE) is associated with vasculitis, premature atherosclerosis, and hypercoagulability. The incidence of thrombosis in patients with SLE is 2 per 100 person-years of follow-up [39]. There are also several reports of intraosseous thrombi in ON cases associated with dysbarism [40], antiphospholipid antibody syndrome [41, 42], and Crohn’s disease [43, 44]. It should be noted here that many of these conditions result in corticosteroid therapy. The association of corticosteroids to ON will be discussed thoroughly later in the chapter.
3 Coagulation Cascade and Regulation
Every basic physiology and hematology textbook describes the physiologic mechanisms involved in the formation and the resolution of blood clots [45, 46]. While it is not the intention of this chapter to provide a detailed description of the pathways involved (e.g., extrinsic vs. intrinsic pathways), it is important to understand the complexity of the coagulation factors involved in both coagulation and fibrinolysis.
Blood clots form via one of the two pathways based upon whether the inciting event is tissue factor (TF) pathway (extrinsic) or amplification by the formation of a primary complex of factors in contact with collagen in the endothelium of damaged vessel walls (intrinsic) [45]. While some of the factors involved in the cascades are the same (e.g., factor X), others are different [factor VII (extrinsic) vs. factor XII (intrinsic)] (Fig. 10.1). In both pathways, the final step is the conversion of prothrombin to thrombin by prothrombin activator in the presence of calcium ions. Thrombin converts fibrinogen to fibrin monomers, which, in turn, polymerize into long fibrin threads. The clot acts to entrap platelets, blood cells, and plasma [48]. A thrombus is established when a blood clot attaches and remains stationary along the wall of a blood vessel, impairing blood flow and, in some cases, totally obscuring lumen [48]. The downregulation of coagulation is effected by proteolytic inactivation of specific coagulation factors [49]. These factors include antithrombin III, protein C, protein S, and others.
The intrinsic and extrinsic coagulation pathways (Published with permission Aaron and Ciombor [47])
As with the coagulation cascades, the fibrinolytic system is built upon a system of activators and inhibitors [50]. The induction of fibrinolysis is dependent on the formation of the active enzyme, proplasmin, a serine protease that degrades fibrin clots. Plasminogen is released as a zymogen and converted to plasmin by one of two activators: tissue plasminogen activator (tPA) and urokinase plasminogen activator (u-PA) – based upon whether fibrin is in the circulation or cell bound, respectively. Inhibitors of the fibrinolytic system include α2-macroglobluin (A2M) and α1 antitrypsin as well as the plasminogen activator inhibitors (PAI-1 and PAI-2) [51].
4 Osteonecrosis and Coagulation Factors
The literature is replete with reports of an association between osteonecrosis and abnormalities of the factors participating in both the coagulation and fibrinolytic pathways. Many studies have focused on the circulating levels of these factors, while others have evaluated whether there is an association with inherited thrombophilia or hypofibrinolysis. While a genetic abnormality may lead to unusually high or low circulating levels of a specific coagulation factor, this may not always be the case. It is, therefore, important to conduct both genetic and serologic studies to explore this association. Several external factors such as corticosteroid therapy and alcoholism have also been associated with abnormal circulating levels of these factors and increased risk of thromboembolism [52–54]. Unfortunately, many of these associations have been based on case reports or small series [14, 55–67]. The following discussion will address the results of the larger studies.
4.1 Thrombophilia
Thrombophilia is the increased tendency towards intravascular thrombosis [28]. Elevations in anticardiolipin antibodies, anti-β-GPI antibodies, homocysteine and activated protein C resistance have been observed with thrombophilia [34, 46, 68]. Inherited thrombophilia is associated with mutations in the genes for factor V (factor V Leiden, a mutation in the F5 gene at position 1691), prothrombin (prothrombin G20210A, at position 20210 in the 3′ untranslated region of the gene), factor XIII, methylenetetrahydrofolate reductase (MTHFR), and abnormal fibrinogen [46, 68]. When factor V is mutated, it is unable to bind to protein C so that factor V is more resistant to inactivation by protein C [28, 47]. Deficiencies in antithrombin III, protein C, or protein S are also associated with thrombophilia [28, 46]. As proteins C and S are involved in the activation of factor V, decreased levels of these proteins result in an increased tendency to form thrombi [47]. As shown in Tables 10.2 and 10.3, numerous reports have indicated an association between osteonecrosis and abnormal levels of specific factors or gene mutations involved with thrombophilia.
-
Glueck and colleagues have studied the association between osteonecrosis and coagulopathies for over 20 years. They have reported higher resistance to activated protein C [28], low protein C [28], low protein S [30, 31], high anticardiolipin antibodies [34], high homocysteine levels [30, 31, 34], and high factor VIII [30]. Korompilias et al. have also reported increased resistance to activated protein C, high levels of anticardiolipin antibody, and low levels of protein S in some osteonecrosis patients [35, 36]. Deficiencies in antithrombin III, protein C, and protein S are associated with deep venous thrombosis of the extremities [73].
Heritable thrombophilia has also been investigated, especially in regard to mutations in genes for MTHFR, V Leiden, and prothrombin. The mutant form of MTHFR, the C677T polymorphisms, decreases the activity of the enzyme and interferes with the intracellular metabolism of homocysteine, resulting in an elevated plasma homocysteine level [74, 75]. Elevated levels of homocysteine are associated with thrombophilia [76]. As shown by Glueck et al. [31], osteonecrosis patients were more likely to have the heterozygous for the MTHFR mutation (64 %) than were controls (38 %) (p = 0.014). This was associated with elevated homocysteine levels in this patient cohort (p = 0.05). Resistance to activated protein C (RAPC) is associated with the Arg506Gln mutation in factor V (factor V Leiden) [24]. In a study of 68 patients with osteonecrosis, Björkman and colleagues reported 13.2 % of the patients with the factor V Leiden mutation, while the idiopathic group exhibited a 22.9 % rate [24]. In a study of 244 ON patients, Glueck et al. found that 9.4 % of the patients were heterozygous for factor V Leiden; the rates were similar for both idiopathic (9.3 %) and secondary (9.6 %) osteonecroses [71].
Thrombin plays a critical role in the conversion of fibrinogen to fibrin in the coagulation pathway (Fig. 10.1). Prothrombin is enzymatically cleaved by activated factor X to form thrombin, and this action is further enhanced in the presence of factor V. The mutation in prothrombin (20210A) causes increased circulating levels and therefore predisposes to thrombotic events [24, 75]. While Glueck et al. found no difference in the presence of prothrombin gene heterozygosity between osteonecrosis cases (3.4 %) and controls (2.9 %) [71], Björkman et al. reported a 5.9 % incidence of heterozygosity for the prothrombin 20210A mutation [24].
4.2 Hypofibrinolysis
Markers of hypofibrinolysi s have also been identified in some patients with osteonecrosis (Tables 10.3 and 10.4). Plasminogen activator inhibitor-1 (PAI-1) acts to inhibit tissue plasminogen activator (tPA) which is an activator of plasminogen (Fig. 10.2). When plasminogen becomes activated, it is converted to plasmin which then acts to dissolve the fibrinogen fibers within a blood clot (fibrinolysis). An increase in PAI-1 activity suppresses the generation of plasmin resulting in hypofibrinolysis [47]. Several studies have documented elevated levels of plasminogen activator inhibitor 1 (PAI-1) and/or low levels of tissue plasminogen activator [27–29, 31, 33, 34, 86].
The fibrinolytic pathway (Aaron and Ciombor [47])
Glueck et al. found differences in the basal and stimulated levels of tPA-Fx, tPA-Ag, PAI-Fx, and PAI-Ag between patients with idiopathic ON and secondary ON [27]. (These abbreviations need to be defined and explained here.) Three secondary ON patients had basal tPA-Fx outside of the normal range (elevated), while only one idiopathic patient was outside of the range (low). Most of the 2° ON patients had stimulated levels within the normal range (only 4 patients elevated), while 9/12 idiopathic patients had levels below the range of normal. Furthermore, the majority of the 2° ON patients had basal and stimulated PAI-Fx and PAI-Ag within normal range, while two thirds of the idiopathic patients had elevated PAI-Fx and PAI-Ag levels as compared to the normal controls. They also noted that patients with 2° ON had markedly lower basal and stimulated PAI-Fx and PAI-Ag than patients with idiopathic osteonecrosis.
Lipoprotein(a) Lp(a) has also been associated with hypofibrinolysis and hypercoagulability [75, 76]. One of the subunits of Lp(a), apolipoprotein(a), contains domains with extensive homology to plasminogen [36]. Apo(a) inhibits the conjunction of plasminogen and tPA at the surface of fibrin, thereby interrupting fibrinolysis [76]. Elevated levels of Lp(a) have been observed in osteonecrosis patients in numerous studies [9, 27, 28, 30, 31, 33, 36, 38, 87]. Glueck et al. [27] observed that the mean Lp(a) level was within the normal range for the idiopathic patients, while it was elevated for the secondary osteonecrosis patients. While they did not note any elevated levels of Apo A1 for either group as compared to controls, a significant elevation Apo B for the idiopathic group was observed. Apo B is a major component in the formation of low density lipoprotein (LDL) and is responsible for carrying into the tissues. Hirata et al. [88] found that there was a strong association between the low molecular weight phenotype of apolipoprotein (a) and ON in renal transplant patients (adjusted odds ratio 5.75). Furthermore, Korompilias et al. reported an association between anticardiolipin antibody and Lp(a) [36].
Heritable hypofibrinolysis has also been studied extensively. The mutated 4G/4G genotype for PAI-1 was more prevalent in patients with AVN (61.5 %) than in control patients without ON (clinical, 20.7 %; radiological, 17.3 %) [69]. In another study, Kim et al. reported that three single nucleotide polymorphisms (SNP) [rs1799889 (4G allele), rs2227631 (A allele), and rs11178 (C allele)] were associated with increased risk of ON [70]. Asano et al. reported that plasma PAI-1 levels were the highest in ON patients with the 4G/4G genotype [89]. However, univariate analysis demonstrated no significant difference in the incidence of ON between patients with different genotypes of PAI-1. Whether their results reflect the etiology (renal transplant) or ethnicity (Japanese) of the patient population requires further evaluation.
4.3 No Association
A number of studies have reported no association between thrombophilic and fibrinolytic factors and osteonecrosis. However, it is important to appreciate that this conclusion is based on a selective analysis of factors known to be thrombophilic and hypofibrinolytic. Furthermore, as stated previously, lack of evidence for gene mutations associated with heritable hypofibrinolysis or thrombophilia does not necessarily mean that there are no abnormalities in the local and systemic levels of the gene products, i.e., the proteins and enzymes involved in the coagulation and fibrinolytic cascades.
In a prospective case-controlled study, Mehsen et al. reported no significant difference in the frequency of thrombosis risk factors between aseptic osteonecrosis patients (56.4 %) and their matched controls (48.7 %) [90]. Assessment of thrombosis was based on circulating levels of protein S, homocysteine level, anticardiolipin Ab, β2 glycoprotein I Ab, and antiprothrombin. Seventy-one percent of the patients presented with at least one risk factor vs. 38 % of the controls. However, no significant difference was shown between the ON patients and the matched controls. They did find a significant association between smoking and risk for developing ON. Séguin et al. [91] also found no association between osteonecrosis of the femoral head and any specific marker for thrombophilia (antithrombin III, protein C, protein S, anticardiolipin Ab). Although deficiencies were observed in a few patients, their frequency was within the expected range published for healthy controls. Furthermore, there is no allelic or genotypic association or trend found for each PAI-1 genotype analyzed. Studies have also reported no association between osteonecrosis and antiphospholipid antibodies [92, 93].
In genetic studies, Celik et al. [94] reported no significant difference in the presence of factor V Leiden, prothrombin G20210A, and MTHFR C677T mutations between osteonecrosis (renal transplant patients) and volunteer controls. One limitation of this study was the relatively small numbers of patients (n = 11, ON; n = 39 controls). In a study of 31 Japanese osteonecrosis patients (renal transplant patients), Asano et al. did not find a correlation between osteonecrosis and the distribution of different genotypes for PAI-1 (4G/5G) or MTHFR C677T [89]. Kim et al. [95] evaluated 443 Korean patients with osteonecrosis and compared their results to that obtained for 273 controls. Genotyping using 15 single nucleotide polymorphisms (SNPs) for MTHFR, they found no significant difference in frequencies of the MTHFR polymorphisms and haplotypes. Cenni et al. detected homozygosity or heterozygosity for factor V Leiden in two corticosteroid-associated patients and no idiopathic ON patients [26]. While they state that the frequency of thrombophilia was not different than controls, more steroid-associated ON patients had 4G/5G (50 %) and fewer had 4G/4G (22 %) as compared to the idiopathic (39 %/33 %) or control (36 %/43 %) groups. In a study of post-severe acute respiratory distress syndrome patients with osteonecrosis, Sun et al. did not detect any mutations of factor V Leiden or prothrombin G20210A [96]. With respect for the gene for PAI-1, Asano et al. suggest that the differences between published results may reflect differences in the genetic backgrounds and frequency of thrombotic diseases in different ethnic groups [89].
4.4 Intravascular Coagulation and Pathogenesis
In order to understand the potential role that thrombophilia and hypofibrinolysis may play in the pathogenesis of osteonecrosis, one should appreciate the concept of intravascular coagulation as proposed by John Paul Jones, Jr. In 1974, he hypothesized that intravascular osteonecrosis is the final common pathway in the early pathogenesis of osteonecrosis [97]. He expanded on this to emphasize that he did not believe that intravascular coagulation was the cause of osteonecrosis but that it was an intermediary event initiated by an underlying etiologic factor, i.e., a factor associated with anunderlying disease [7, 14, 98, 99]. The list of comorbidities that could potentially activate intravascular coagulation is extensive and includes both genetic (e.g., familial thrombophilia, Gaucher’s disease, hemoglobinopathies) and nongenetic (hyperlipemia, fat emboli, hypercortisonism, alcoholism, dysbaric phenomenon, hypersensitivity reactions, allograft organ rejection, endotoxic (Shwartzman) reactions, proteolytic enzyme). Other prothrombotic and hypofibrinolytic conditions, tissue factors such as TNF, antiphospholipid Ab, pancreatitis, malignancies, collagen vascular diseases, pregnancy, and immune complex disorders must also be considered [4, 98]. Intraosseous fat embolism as an initiator of intravascular coagulation was proposed by Jones [7, 14] and supported by others [47, 100]. Once triggered, intravascular coagulation may then result in irreversible cell injury with ATP depletion and cell membrane damage, leading to ischemic osteocytic and adipocytic necrosis [6]. Jones also suggests that many of the factors associated with the underlying disease or disorder lead to intravascular coagulation as well as “rapid endothelial sloughing, exposure of subendothelial collagen, and release of tissue thromboplastin” [14]. Endothelial damage has been suggested by others as an underlying mechanism in the pathogenesis of osteonecrosis [73, 101–103]. Corticosteroids have also been shown to directly injure endothelial cells [104]. Jones proposed, “There is upregulation of procoagulant activity, because the perturbed endothelial cell surface represents a binding site for Factor VIIa mediating the activation of the extrinsic pathway of coagulation. There is downregulation of anticoagulant activity, because the perturbed endothelial cell loses its thrombomodulin membrane receptor and the protein C pathway is not activated.” This would create a vicious cycle where the prothrombotic response becomes amplified.
Jones proposed the concept of an “ischemic threshold ” [7]. In relation to the theory of fat emboli, Jones proposed that an ischemic threshold could develop when the intravascular fat load exceeds or overwhelms the anti-lipemic and anticoagulant clearance mechanisms. Below the threshold level, there is fatty degeneration of subchondral and subperiosteal osteocytes and osteoblasts; above the threshold, there is free fatty acid production, no clearance of procoagulant factors, leading to bony ischemia. Increased circulating free fatty acids were observed by Kabata et al. in an animal model of corticosteroid-induced osteonecrosis [100].
5 Corticosteroid Therapy
One of the major risk factors for osteonecrosis is high-dose corticosteroid therapy. There are several mechanisms by which corticosteroid therapy may have an impact on the incidence of hypercoagulability in patients with ON. Corticosteroids may directly injure endothelial cells and thereby initiate the coagulation cascade [73, 101, 105, 106]. Corticosteroids may act to increase PAI-1 activity [5, 69] as well as decrease tPA activity [5, 106]. Of particular note, in a systemic review of the literature, Van Zaane et al. reported there was an increase in the activity of factors VII, VIII, and XI following corticosteroid treatment; this was found to be exacerbated during active inflammation [107].
Although one study reported no significant difference in the frequency of genetic mutations for factor V, prothrombin, or MTHFR [94], this does not preclude the possibility that the corticosteroid treatment had an effect on the circulating levels of the gene products for these are other procoagulants.
6 Conclusions
Hypercoagulability and hypofibrinolysis have both been implicated in the pathogenesis of osteonecrosis. Both may be inherited or acquired. Acquired coagulation abnormalities are related to external factors such as corticosteroid therapy, smoking, or excessive alcohol consumption. In contradistinction, genetic studies have identified inherited abnormalities in the genes coding for a number of different coagulation factors in both the coagulation and fibrinolytic pathways. Understanding the clinical ramifications of these findings is complicated. There is no one abnormality which is common to all patients with osteonecrosis. In fact, some of the most frequent abnormalities have included abnormal RAPC levels (50 %) [28, 32, 33, 36], elevated PAI-1 [26, 27, 33, 34, 86], and Lp (a) [9, 33, 36, 38] of ON patients. A major confounding factor is that many of the studies proposing a link between osteonecrosis and specific coagulation factors have either limited numbers of ON patients or have not included adequate controls. Individual orthopedic surgeons often do not see sufficient numbers of osteonecrosis patients to be able to conduct a statistically robust study. Furthermore, a complete battery of serologic and genetic markers is expensive, and external funding is frequently lacking. While some investigators have made an effort to age and sex/gender match their controls, more appropriate disease-matched controls would provide additional information. A study evaluating lupus patients with and without steroid therapy and with or without osteonecrosis is a perfect example but extremely difficult to undertake and complete with adequate follow-up. A third major factor adding to the complexity of risk assessment in ON is that the abnormal coagulation factors may be associated with diverse etiologic factors already identified for osteonecrosis – this may be particularly true for those diseases associated with autoimmune disorders such as lupus erythematosus (Table 10.4). It is these associations between coagulation abnormalities and the comorbidities that may help to define which patients are more truly at risk to develop osteonecrosis. Finally, as we continue to increase our knowledge of the regulation and interrelationships between different modulators of the coagulation and fibrinolytic cascades, new associations will emerge. There may be factors upstream or downstream of those already identified that play a critical role and may eventually unify the pathogenetic mechanisms involved.
A number of studies have shown a high percentage of patients with at least one coagulation factor abnormality [20, 28, 34, 36, 38]. Several of these studies show similar rates between patients with idiopathic and secondary ON [34, 38]. In a previous study, our group has shown that while 82.2 % of the patients with ON had at least one coagulopathy, 46.7 % had two or more abnormal tests (as compared to 2.5 % of controls) [34]. This could have implications regarding specific patients.
Previous investigators have suggested the multihit theory of osteonecrosis [4, 47, 106, 108]. There may be a genetic predisposition for osteonecrosis that may or may not be related to a hypercoagulable state. The individual may then experience external factors (such as alcoholism, corticosteroids therapy, hyperbaric exposure, or smoking) or develop a comorbidity (such as hemoglobinopathies, Gaucher’s disease, autoimmune diseases, and pregnancy) that act to “push them over” the threshold of disease [36]. Cosgriff [109] and Jones [7] have also suggested that steroid treatment may place some patients in a “prothrombotic state.” Without question, further study is needed to resolve these issues.
References
Ficat RP, Arlet J. Ischemia and Necroses of Bone. In: Hungerford DS, editor. Baltimore: Williams & Wilkins; 1980. p. 196.
Schroer WC. Current concepts on the pathogenesis of osteonecrosis of the femoral head. Orthop Rev. 1994;23(6):487–97.
Jones LC, Hungerford DS. The pathogenesis of osteonecrosis. Instr Course Lect. 2007;56:179–96.
Assouline-Dayan Y, et al. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32(2):94–124.
Powell C, Chang C, Gershwin ME. Current concepts on the pathogenesis and natural history of steroid-induced osteonecrosis. Clin Rev Allergy Immunol. 2011;41(1):102–13.
Jones JJP. Etiology and pathogenesis of osteonecrosis. Semin Arthroplasty. 1991;2(3):160–8.
Jones Jr JP. Intravascular coagulation and osteonecrosis. Clin Orthop Relat Res. 1992;277:41–53.
Boettcher WG, et al. Non-traumatic necrosis of the femoral head. I. Relation of altered hemostasis to etiology. J Bone Joint Surg Am. 1970;52(2):312–21.
Posan E, et al. Thrombotic and fibrinolytic alterations in the aseptic necrosis of femoral head. Blood Coagul Fibrinolysis. 2003;14(3):243–8.
Bonfiglio M. Development of bone necrosis lesions. In: Lambertsen C, editor. 5th symposium underwater physiology. Bethesda: Fed Am Soc Exp Biol; 1976. p. 117–32.
Spencer JD, Brookes M. Avascular necrosis and the blood supply of the femoral head. Clin Orthop Relat Res. 1988;235:127–40.
Saito S, et al. Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop Relat Res. 1989;244:198–207.
Asherson RA, et al. Avascular necrosis of bone and antiphospholipid antibodies in systemic lupus erythematosus. J Rheumatol. 1993;20(2):284–8.
Jones Jr JP. Fat embolism, intravascular coagulation, and osteonecrosis. Clin Orthop Relat Res. 1993;292:294–308.
Cheras PA, Freemont AJ, Sikorski JM. Intraosseous thrombosis in ischemic necrosis of bone and osteoarthritis. Osteoarthritis Cartilage. 1993;1(4):219–32.
Egan RM, Munn RK. Catastrophic antiphospholipid antibody syndrome presenting with multiple thromboses and sites of avascular necrosis. J Rheumatol. 1994;21(12):2376–9.
Starklint H, Lausten GS, Arnoldi CC. Microvascular obstruction in avascular necrosis. Immunohistochemistry of 14 femoral heads. Acta Orthop Scand. 1995;66(1):9–12.
Laroche M, et al. Histological appearance of the intra-osseous vessels of the femoral head in aseptic osteonecrosis of the hip, with or without antiphospholipid antibodies. Clin Rheumatol. 1997;16(4):367–71.
Saito S, Ohzono K, Matsui M. Early arteriopathy and hemorrhage in osteonecrosis of the femoral head. In: Urbaniak JR, Jones JPJ, editors. Osteonecrosis: etiology, diagnosis, and treatment. Rosemont: AAOS; 1997. p. 81–5.
Chotanaphuti T, et al. The prevalence of thrombophilia in idiopathic osteonecrosis of the hip. J Med Assoc Thai. 2009;92 Suppl 6:S141–6.
Aaron R. Osteonecrosis: etiology, pathophysiology, and diagnosis. In: Callaghan T, editor. The adult hip. Philadelphia: Lippincott Raven; 1998. p. 451–66.
Jones Jr JP. Fat embolism and osteonecrosis. Orthop Clin N Am. 1985;16(4):595–633.
Atsumi T, Kuroki Y, Yamano K. A microangiographic study of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 1989;246:186–94.
Bjorkman A, et al. Factor V leiden and prothrombin gene mutation: risk factors for osteonecrosis of the femoral head in adults. Clin Orthop Relat Res. 2004;425:168–72.
Bjorkman A, et al. Factor V Leiden and the prothrombin 20210A gene mutation and osteonecrosis of the knee. Arch Orthop Trauma Surg. 2005;125(1):51–5.
Cenni E, et al. Idiopathic and secondary osteonecrosis of the femoral head show different thrombophilic changes and normal or higher levels of platelet growth factors. Acta Orthop. 2011;82(1):42–9.
Glueck CJ, et al. Hypofibrinolysis: a common, major cause of osteonecrosis. Am J Hematol. 1994;45(2):156–66.
Glueck CJ, et al. Thrombophilia and hypofibrinolysis: pathophysiologies of osteonecrosis. Clin Orthop Relat Res. 1997;334:43–56.
Glueck CJ, et al. The plasminogen activator inhibitor-1 gene, hypofibrinolysis, and osteonecrosis. Clin Orthop Relat Res. 1999;366:133–46.
Glueck CJ, et al. Thrombophilia, hypofibrinolysis, the eNOS T-786C polymorphism, and multifocal osteonecrosis. J Bone Joint Surg Am. 2008;90A(10):2220–9.
Glueck CJ, et al. Hypofibrinolysis, thrombophilia, osteonecrosis. Clin Orthop Relat Res. 2001;386:19–33.
Glueck CJ, Freiberg RA, Wang P. Heritable thrombophilia-hypofibrinolysis and osteonecrosis of the femoral head. Clin Orthop Relat Res. 2008;466(5):1034–40.
Gruppo R, et al. The pathophysiology of alveolar osteonecrosis of the jaw: anticardiolipin antibodies, thrombophilia, and hypofibrinolysis. J Lab Clin Med. 1996;127(5):481–8.
Jones LC, et al. Procoagulants and osteonecrosis. J Rheumatol. 2003;30(4):783–91.
Korompilias AV, et al. Anticardiolipin antibodies and osteonecrosis of the femoral head. Clin Orthop Relat Res. 1997;345:174–80.
Korompilias AV, Ortel TL, Urbaniak JR. Coagulation abnormalities in patients with hip osteonecrosis. Orthop Clin N Am. 2004;35(3):265–71, vii.
Tan X, et al. Comparative analysis of serum proteomes: discovery of proteins associated with osteonecrosis of the femoral head. Trans Res. 2006;148(3):114–9.
Zalavras C, et al. Potential aetiological factors concerning the development of osteonecrosis of the femoral head. Eur J Clin Invest. 2000;30(3):215–21.
Petri M. Thrombosis and systemic lupus erythematosus: the Hopkins Lupus Cohort perspective. Scand J Rheumatol. 1996;25(4):191–3.
Gertler SL, et al. Mesenteric venous thrombosis as sole complication of decompression sickness. Digest Dis Sci. 1984;29(1):91–5.
Yang P, Kruh JN, Foster CS. Antiphospholipid antibody syndrome. Curr Opin Ophthalmol. 2012;23(6):528–32.
Taraborelli M, Andreoli L, Tincani A. Much more than thrombosis and pregnancy loss: the antiphospholipid syndrome as a ‘systemic disease’. Best Pract Res Clin Rheumatol. 2012;26(1):79–90.
Lund KS, et al. Increased risk of venous thromboembolism and arterial cardiovascular events in patients with inflammatory bowel disease. Ugeskr Laeger. 2012;174:3003–6.
Papa A, et al. Vascular involvement in inflammatory bowel disease: pathogenesis and clinical aspects. Digest Dis. 2008;26(2):149–55.
Hall JE, Guyton AC. Guyton and Hall textbook of medical physiology. 12th ed. Philadelphia: Saunders/Elsevier; 2011. xix, 1091 p.
Hoffbrand AV, Moss PAH, Pettit JE. Essential haematology. 6th ed. Malden: Wiley-Blackwell; 2011. xi, 454 p.
Aaron RK, Ciombor DM. Coagulapathies and osteonecrosis. Curr Opin Orthop. 2001;12:378–83.
Hoffbrand AV, Moss PAH, Pettit JE. Essential haematology. 5th ed. Malden/Oxford: Blackwell; 2006. ix, 380 p.
Castoldi E, Rosing J. APC resistance: biological basis and acquired influences. J Thromb Haemostasis JTH. 2010;8(3):445–53.
Lijnen HR. Role of fibrinolysis in obesity and thrombosis. Thromb Res. 2009;123 Suppl 4:S46–9.
Lijnen HR. Elements of the fibrinolytic system. Ann N Y Acad Sci. 2001;936:226–36.
Tran-Thang C, et al. Plasminogen activators and plasminogen activator inhibitors in liver deficiencies caused by chronic alcoholism or infectious hepatitis. Thromb Haemostasis. 1989;62(2):651–3.
Johannesdottir SA, et al. Use of glucocorticoids and risk of venous thromboembolism: a nationwide population-based case–control study. JAMA Int Med. 2013;173(9):743–52.
van Zaane B, et al. Systematic review on the effect of glucocorticoid use on procoagulant, anti-coagulant and fibrinolytic factors. J Thromb Haemostasis JTH. 2010;8(11):2483–93.
Elishkewich K, et al. Idiopathic osteonecrosis in an adult with familial protein S deficiency and hyperhomocysteinemia. Blood Coagul Fibrinolysis. 2001;12(7):547–50.
Glueck CJ, et al. Idiopathic osteonecrosis, hypofibrinolysis, high plasminogen activator inhibitor, high lipoprotein(a), and therapy with Stanozolol. Am J Hematol. 1995;48(4):213–20.
Glueck CJ, et al. Estrogen replacement in a protein S deficient patient leads to diarrhea, hyperglucagonemia, and osteonecrosis. JOP J Pancreas. 2001;2(5):323–9.
Glueck CJ, et al. Thrombophilia, hypofibrinolysis, the eNOS T-786C polymorphism, and multifocal osteonecrosis. J Bone Joint Surg Am. 2008;90(10):2220–9.
Kubo T, et al. Antithrombin III deficiency in a patient with multifocal osteonecrosis. Clin Orthop Relat Res. 2000;378:306–11.
Moore J, et al. Bilateral knee osteonecrosis in a patient with thrombotic thrombocytopenic purpura. Aust N Z J Med. 1999;29(1):88–9.
Pierre-Jacques H, et al. Familial heterozygous protein-S deficiency in a patient who had multifocal osteonecrosis. A case report. J Bone Joint Surg Am. 1997;79(7):1079–84.
Shahin AA. Arthritis and osteonecrosis in a patient with thrombophilia. Rheumatol Int. 2001;20(6):243–5.
Ureten K, et al. Atraumatic osteonecrosis after estrogen replacement therapy associated with low protein S level in a patient with Turner syndrome. Clin Appl Thromb/Hemostasis. 2010;16(5):599–601.
Vairaktaris E, et al. Bisphosphonate-induced avascular osteonecrosis of the mandible associated with a common thrombophilic mutation in the prothrombin gene. J Oral Max Surg. 2009;67(9):2009–12.
Wermes C, et al. Severe protein C deficiency and aseptic osteonecrosis of the hip joint: a case report. Eur J Pediatr. 1999;158 Suppl 3:S159–61.
Zhang H, et al. Proteomic analysis of bone tissues of patients with osteonecrosis of the femoral head. Omics J Integr Biol. 2009;13(6):453–66.
Benbih M, et al. Multiple osteonecroses and venous thrombosis: one case of patient with a novel mutation of protein C (N102S) and heterozygous for FV Leiden. Ann De Biol Clin. 2008;66(4):437–40.
Varga EA, et al. Cardiology patient pages. Homocysteine and MTHFR mutations: relation to thrombosis and coronary artery disease. Circulation. 2005;111(19):e289–93.
Ferrari P, et al. Association of plasminogen activator inhibitor-1 genotype with avascular osteonecrosis in steroid-treated renal allograft recipients. Transplantation. 2002;74(8):1147–52.
Kim H, et al. Significant associations of PAI-1 genetic polymorphisms with osteonecrosis of the femoral head. BMC Musculoskelet Disord. 2011;12:160.
Glueck CJ, et al. The role of the factor V Leiden mutation in osteonecrosis of the hip. Clin Appl Thromb Hemost. 2012;19(5):499–503.
Gillespie DL, et al. Resistance to activated protein C: a common inherited cause of venous thrombosis. Ann Vasc Surg. 1996;10(2):174–7.
Kerachian MA, et al. Avascular necrosis of the femoral head: vascular hypotheses. Endothelium. 2006;13(4):237–44.
Shang XF, et al. Association between MTHFR C677T polymorphism and osteonecrosis of the femoral head: a meta-analysis. Mol Biol Rep. 2012;39(6):7089–94.
Orth P, Anagnostakos K. Coagulation abnormalities in osteonecrosis and bone marrow edema syndrome. Orthopedics. 2013;36(4):290–300.
Lykissas MG, et al. The role of hypercoagulability in the development of osteonecrosis of the femoral head. Orthop Rev (Pavia). 2012;4(2):e17.
Adams MJ, Palatinus AA, Harvey AM, Khalafallah AA. Impaired control of the tissue factor pathway of blood coagulation in systemic lupus erythematosus. Lupus. 2011;20(14):1474–83.
Palatinus A, Adams M. Thrombosis in systemic lupus erythematosus. Semin Thromb Hemost. 2009;35(7):621–9.
Nsiri B, et al. Abnormalities of coagulation and fibrinolysis in homozygous sickle cell disease. Hematol Cell Ther. 1996;38(3):279–84.
Candito M, et al. Homocysteinemia and thrombophilic factors in unexplained decompression sickness. Rev Neurol (Paris). 2006;162(8-9):840–4.
Tran-Thang C, et al. Plasminogen activators and plasminogen activator inhibitors in liver deficiencies caused by chronic alcoholism or infectious hepatitis. Thromb Haemost. 1989;62(2):651–3.
Koutroubakis IE, Tsiolakidou G, Kouroumalis EA. Inherited thrombophilia and thrombosis in inflammatory bowel disease. Am J Gastroenterol. 2006;101(2):403; author reply 403–4.
Klai S, et al. Thrombophilic disorders: a real threat to patients with end-stage renal disease on hemodialysis and at the time of renal transplantation. Blood Coagul Fibrinolysis. 2012;23(5):406–10.
Reshetniak TM, Seredavkina NV, Nasonov EL. Cardiovascular aspects of antiphospholipid syndrome. Klin Med (Mosk). 2008;86(9):4–12.
Glueck CJ, et al. The 4G/4G polymorphism of the hypofibrinolytic plasminogen activator inhibitor type 1 gene: an independent risk factor for serious pregnancy complications. Metabolism. 2000;49(7):845–52.
Tan X, et al. Comparative analysis of serum proteomes: discovery of proteins associated with osteonecrosis of the femoral head. Transl Res. 2006;148(3):114–9.
Glueck CJ, et al. Plasminogen activator inhibitor activity: an independent risk factor for the high miscarriage rate during pregnancy in women with polycystic ovary syndrome. Metabolism. 1999;48(12):1589–95.
Hirata T, et al. Low molecular weight phenotype of Apo(a) is a risk factor of corticosteroid-induced osteonecrosis of the femoral head after renal transplant. J Rheumatol. 2007;34(3):516–22.
Asano T, et al. Relationship between postrenal transplant osteonecrosis of the femoral head and gene polymorphisms related to the coagulation and fibrinolytic systems in Japanese subjects. Transplantation. 2004;77(2):220–5.
Mehsen N, et al. Coagulopathies frequency in aseptic osteonecrosis patients. Joint Bone Spine. 2009;76(2):166–9.
Seguin C, et al. Non-traumatic necrosis of bone (osteonecrosis) is associated with endothelial cell activation but not thrombophilia. Rheumatology. 2008;47(8):1151–5.
Dromer C, et al. No link between avascular necrosis of the femoral head and antiphospholipid antibodies. Rev Rhum Engl Ed. 1997;64(6):382–5.
Alarcon-Segovia D, et al. Antiphospholipid antibodies and the antiphospholipid syndrome in systemic lupus erythematosus. A prospective analysis of 500 consecutive patients. Medicine (Baltimore). 1989;68(6):353–65.
Celik A, et al. Association of corticosteroids and factor V, prothrombin, and MTHFR gene mutations with avascular osteonecrosis in renal allograft recipients. Transplant Proc. 2006;38(2):512–6.
Kim TH, et al. Lack of association of MTHFR gene polymorphisms with the risk of osteonecrosis of the femoral head in a Korean population. Mol Cells. 2010;29(4):343–8.
Sun W, et al. Hematological changes and related gene mutation of post-severe acute respiratory syndrome patients with osteonecrosis. Zhonghua Yi Xue Za Zhi. 2006;86(7):442–5.
Jones JPJ, Sakovich L, Andersen CE. Dysbarism-related osteonecrosis. Washington, DC: E. Department of Health, and Welfare, Editor; 1974. p. 117–32.
Jones Jr JP. Risk factors potentially activating intravascular coagulation and causing nontraumatic osteonecrosis. In: Urbaniak JR, Jones Jr JP, editors. Osteonecrosis: etiology, diagnosis, and treatment. Rosemont: AAOS; 1997. p. 89–96.
Jones Jr JP. Coagulopathies and osteonecrosis. Acta Orthop Belg. 1999;65 Suppl 1:5–8.
Kabata T, et al. Onset of steroid-induced osteonecrosis in rabbits and its relationship to hyperlipaemia and increased free fatty acids. Rheumatology (Oxford). 2005;44(10):1233–7.
Jacobs B. Epidemiology of traumatic and nontraumatic osteonecrosis. Clin Orthop Relat Res. 1978;130:51–67.
Slichter SJ, et al. Dysbaric osteonecrosis: a consequence of intravascular bubble formation, endothelial damage, and platelet thrombosis. J Lab Clin Med. 1981;98(4):568–90.
Li Y, et al. The experimental study on treatment of glucocorticoid-induced ischemic necrosis of femoral head by gu fu sheng capsule. J Tradit Chin Med. 2004;24(4):303–7.
Nishimura T, et al. Histopathologic study of veins in steroid treated rabbits. Clin Orthop Relat Res. 1997;334:37–42.
Boss JH, Misselevich I. Osteonecrosis of the femoral head of laboratory animals: the lessons learned from a comparative study of osteonecrosis in man and experimental animals. Vet Pathol. 2003;40(4):345–54.
Kerachian MA, Seguin C, Harvey EJ. Glucocorticoids in osteonecrosis of the femoral head: a new understanding of the mechanisms of action. J Steroid Biochem Mol Biol. 2009;114(3–5):121–8.
van Zaane B, et al. Systematic review on the effect of glucocorticoid use on procoagulant, anti-coagulant and fibrinolytic factors. J Thromb Haemost. 2010;8(11):2483–93.
Kenzora JE, Glimcher MJ. Accumulative cell stress: the multifactorial etiology of idiopathic osteonecrosis. Orthop Clin North Am. 1985;16(4):669–79.
Cosgriff SW. Thromboembolic complications associated with ACTH and cortisone therapy. J Am Med Assoc. 1951;147(10):924–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Jones, L.C., Ciombor, D.M. (2014). Osteonecrosis and Intravascular Coagulation Revisited. In: Koo, KH., Mont, M., Jones, L. (eds) Osteonecrosis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-35767-1_10
Download citation
DOI: https://doi.org/10.1007/978-3-642-35767-1_10
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-35766-4
Online ISBN: 978-3-642-35767-1
eBook Packages: MedicineMedicine (R0)