Abstract
Placement of dental implants has become the standard of care for replacement of missing teeth when indicated. Implant surgery is now performed by several of the dental specialties, including oral and maxillofacial surgery. Injuries to the inferior alveolar nerve (IAN) and the mental nerve (MN) are known risks for the placement of dental implants in the mandible. Upon diagnosis of a nerve injury, prompt evaluation of the patient’s sensory function, assessment of the position of the implant with relation to the inferior alveolar canal, and timely decisions regarding the fate of the implant and management of the nerve injury will maximize the likelihood of a favorable outcome.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Placement of dental implants has become the standard of care for replacement of missing teeth when indicated. Implant surgery is now performed by several of the dental specialties, including oral and maxillofacial surgery. Injuries to the inferior alveolar nerve (IAN) and the mental nerve (MN) are known risks for the placement of dental implants in the mandible. Upon diagnosis of a nerve injury, prompt evaluation of the patient’s sensory function, assessment of the position of the implant with relation to the inferior alveolar canal, and timely decisions regarding the fate of the implant and management of the nerve injury will maximize the likelihood of a favorable outcome.
6.1 Background
Since the introduction of dental implants in the 1980s in the USA, the last three decades have seen an exponential increase in the number of implants placed, with many choices of implant type. Many dental professionals, including several specialists, provide this service, and although there have been groundbreaking advances in materials science, bone grafting, tissue management, imaging, and treatment planning, the basic concept of osseointegration [9] remains pivotal for the success of modern implantology. Expertise in the regional soft and hard tissue anatomy of the maxillomandibular region is a prerequisite for the minimization of risk of untoward sequelae from dental implant placement. Prompt recognition and management of acute and chronic complications of surgery is paramount for optimal patient outcome [19, 22, 36].
The risks of injury to the inferior alveolar nerve (IAN), lingual nerve (LN), mental nerve (MN), and long buccal nerve (LBN) are uncommon, but known, complications of implant restoration of the mandible and demand specialized attention [2]. Although not routine, the preoperative use of advanced imaging modalities such as cone-beam computerized tomography (CBCT) scans can assist in localization of the inferior alveolar canal (IAC) and the position of the mental foramen in preparation for implant surgery [30]. With careful planning, the possibility of nerve injury is significantly reduced, although not eliminated completely, even with the best of planning and treatment. Sensory dysfunction of the IAN, especially if persistent or painful, can be distressing to both the patient and the clinician. Most of these injuries resolve spontaneously [7]; however, surgical intervention to repair the nerve is of benefit to selected patients whose sensory dysfunction is persistent and unacceptable [15]. Altered sensation after implant surgery continues to bear medicolegal implications that further warrant the attention of the implantologist [10]. The occurrence of neurosensory dysfunction associated with implant surgery does not necessarily imply a breach of the standard of care. In essence, a nerve injury can result from surgeon-related factors (e.g., diagnosis, surgical technique), patient-related factors (e.g., anatomic variations, undisclosed or uncontrolled medical conditions such as diabetes mellitus), factors not known at the time of the procedure, or combinations of these factors. This differentiation of cause and effect is not always easily discerned from a retrospective review of any given clinical situation.
In the treatment of IAN injuries associated with dental implant surgery, it is most important that there be prompt recognition and acknowledgment of the patient’s sensory complaints and timely decisions regarding management in order to maximize the recovery of nerve function. The clinician will be faced with several issues including treatment of the neurosensory disturbance (NSD) of the affected region, how best to proceed with dental restoration of the affected area, management of a distressed and disappointed patient, and communication with other involved dental professionals. The patient’s concerns are best addressed by a continuing supportive relationship with the patient and appropriate recommendations for further treatment in conjunction with the restorative dentist.
This chapter will cover the etiology, diagnosis, and current management of injuries to the mandibular division (MdN) of the trigeminal nerve from dental implant surgery.
6.2 Etiology of Implant-Related Nerve Injury
The etiology and location of mandibular nerve (MdN) injury from dental implant surgery may be obvious in some clinical situations. However, it is imperative that when planning any microsurgical intervention the site of nerve injury must be identified preoperatively, if at all possible, in order to minimize manipulation of the nerve during surgical intervention. Consideration should be given to the possible anatomic locations of the injury site other than the site of implant placement. This would include the site of local anesthetic injection, incision design, and possible retraction (i.e., stretch) injury at a site distant from the implant location.
Anatomic variations aside, the five most frequent possible causes of injury to the mandibular nerve (MdN) related to dental implant surgery are (1) preoperative errors in evaluation, diagnosis, and treatment planning; (2) local anesthetic injection; (3) excessive implant osteotomy preparation (drilling) or overheating due to drilling; (4) impingement of the implant on the inferior alveolar canal and neurovascular bundle; and (5) other causes such as inadvertent transection of the mental, lingual, or long buccal nerve during incision and/or soft tissue flap retraction.
6.2.1 Errors in Diagnosis and Treatment Planning
The radiographic planning identifies the position of the inferior alveolar canal, which coincides with the anatomic boundaries of the inferior alveolar neurovascular bundle. Anatomical analysis of the neurovascular bundle demonstrates that the IAN is the dominant structure occupying over 80 % of the cross-sectional area, while the remaining 20 % contains the inferior alveolar artery and vein. The location of the vascular structures in relation to the nerve is unpredictable with individual variability.
The panoramic radiograph is useful as the primary imaging study to assess the vertical distance from the crest of the mandibular alveolar ridge to the superior aspect of the inferior alveolar canal (IAC). The panoramic machine should be calibrated for distortion or magnification to allow for accurate determination of dimensions from each panoramic film. There is generally a magnification factor varying between 10 and 40 % on the panoramic radiograph with more magnification in the areas where the imaged bone falls out of the focal trough of the beam. Typically, 20–30 % magnification should be expected in the mandible, and this must be accounted for in the planning. Many implant companies provide radiographic guides with varying percentages of magnification that are helpful in the treatment planning process. If the panoramic film shows inadequate distance from the alveolar crest to the IAC to support an implant, the mediolateral position of the IAC will need to be determined in order to decide whether an implant can be placed without repositioning of the IAN or MN (see below). In such patients, a computed tomographic (CT) or cone-beam scan (CBCT) will be a necessary part of the evaluation process.
Regardless of the radiographic modality (CT or panorex) used for implant planning, errors in interpretation and application of the radiograph can lead to errors in implant positioning. The CT scans have improved resolution and allow visualization of the nerve in three dimensions; however, errors in software planning can be transferred into the surgical procedure. With respect to surgical guides, attention should be given to the accuracy of the guides and the stability of seating onto the alveolar ridge. Placement of the surgical guide on a totally edentulous mandible will have a significant inherent margin of error related to the soft tissue despite correct 3D planning. It is important to allow an additional reasonable distance (i.e., 2–3 mm) from the superior aspect of the IAC during CT planning to accommodate for this margin of error. Although the use of flapless surgery with a mucosal-borne surgical guide (Fig. 6.1) for implant placement is popular, the surgeon should not hesitate to raise a mucoperiosteal flap to better visualize and confirm anatomic landmarks as needed. It is accepted that there is more accuracy with bone-borne (and tooth-borne) surgical guides than with mucosal-borne guides due to the inherent mobility of the soft tissues and lack of fixed landmarks, despite the use of stabilization screws.
6.2.2 Local Anesthetic Injection
The IAN or LN can be injured by needle contact secondary to the injection of a local anesthetic into the pterygomandibular space [27, 28] or the MN when injecting in the area of the mental foramen. Although the exact pathophysiology of this injury remains unknown, there are three possible causes: (1) direct intraneural injection with mechanical injury to the nerve (i.e., severance of axons, partial or total, scar tissue or neuroma formation, Wallerian degeneration), (2) interruption of vessels of the mesoneurium with peri- and intraneural hemorrhage and secondary scar formation, and (3) chemical toxicity of the anesthetic solution, or from a contaminant (sterilizing solution in a storage container) that is able to enter into a leaky anesthetic cartridge [13]. Regardless of the cause, it is recommended that aspiration be performed prior to all local anesthetic injections. If there is a bloody aspirate, or the patient complains of a paresthesia (typically, an “electric shock-like” sensation), the needle is withdrawn a few millimeters and aspiration is repeated. If there is now no bloody aspirate, it can be assumed that the needle tip is no longer in contact with a blood vessel or nerve, and the injection is completed. A note of such an occurrence should be routinely entered in the patient’s chart. This technique may prevent direct injection into a vascular space, but does not necessarily prevent deposition of the anesthetic within the epineurium (the diameter of the IAN is four to five times greater than the associated inferior alveolar artery or vein). Nerve injury secondary to local anesthetic injection, although uncommon, has a reported incidence of 1:26,762 to 1:160,571. It can be difficult to differentiate from injury related to the placement of the dental implants, especially if sedation or general anesthesia was used and, therefore, the patient was unable to report a paresthesia at the time of the injection(s). Without obvious clinical or radiographic signs of injury to the nerve from the dental implant procedure itself, the possibility of needle injection injury cannot be eliminated. Unfortunately, a small number of patients who have suffered an injection-related injury can be misdiagnosed with injury related to the dental implant surgery and subsequently undergo either inappropriate removal of the implant or fruitless exploratory surgical procedures that reveal no visible nerve injury at the implant location.
6.2.3 Osteotomy Preparation
Injury to the IAN as a consequence of bone preparation or implant placement can be due to errors in radiographic planning, drilling, or direct contact of the implant with the nerve. Drilling injuries to the IAN can be difficult to diagnose. Despite correct position of the implant vis-a-vis the IAC on the postoperative radiograph appearance of the implant, osseous preparation with the drill may have been performed beyond the planned implant depth causing injury to the nerve (Fig. 6.2). In addition to the possibility that one of the implant drills entered the IAC and injured the IAN, it is also possible that the drill caused vascular trauma to the inferior alveolar artery (IAA) or inferior alveolar vein (IAV) and resulted in intra-canal bleeding. This bleeding may be noted during the osteotomy preparation by visualization of oozing that is more significant than normal marrow oozing. Once the implant is placed, the bleeding is tamponaded with resultant pressure placed upon the IAN, resulting in paresthesia, and even dysesthesia. This error can be prevented by measurement from correctly calibrated radiographs of the distance from the alveolar ridge crest to the superior aspect of the IAC, the use of drilling equipment with predetermined depth stops, and careful technique to prevent drilling beyond the planned depth. Irrigation with adequate coolant to dispel heat generated by bone drilling may also prevent a thermal injury in the absence of direct contact with the nerve. Frequent intraoperative reverification of the drill dimensions (diameter and length) is also helpful.
6.2.4 Direct Implant Placement Injury
In addition to injury caused by drilling, the extent of injury to the IAN due to the implant itself is related to the degree of encroachment of the implant into the IAC or its direct contact with the IAN (Fig. 6.3). Nerve injury due to implant placement may occur despite proper osseous preparation, when the implant is inserted beyond the vertical confines of the prepared bone, compressing or breaching the superior wall of the IAC and forcing bone into the canal (Fig. 6.4a). Alternately, extension of drilling into the IAC may facilitate overinsertion of the implant beyond its intended depth and into the IAC, making direct contact between the implant and the IAN (Fig. 6.4b, c). Finally, delayed osseous healing and remodeling from localized injury can cause excessive bone formation during the healing phases and compromise the IAC cross-sectional diameter resulting in nerve compression (Fig. 6.4d) [8].
(a) Collapse of the superior aspect of the IAC due to implant placement beyond the planned osteotomy causing injury to the nerve (compartment syndrome). (b) Direct injury to the IAN by implant contact. (c) Direct injury to the cortical rim of the IAC with deformation of the neurovascular bundle. (d) Remodeling of the IAC cortical rim causing narrowing of canal
6.2.5 Other Causes of Injury
The mental nerve (MN) lies in the mandibular buccal soft tissues and is at risk for iatrogenic injury during a vestibular incision. Recognition of the changing anatomy of the edentulous mandible is particularly helpful in minimizing the risk of injury to the MN. As the patient ages, the alveolar bone in an edentulous area resorbs, and the position of the mental foramen becomes closer to the crest of the alveolar ridge (Fig. 6.5a). In some patients there is actual dehiscence of the IAC, and the IAN and the MN come to lie on the alveolar ridge crest (Fig. 6.5b). Placement of an incision must, therefore, take these anatomic changes into consideration. During the retraction of a mucoperiosteal flap, it is possible to exert continuous, undue pressure on the underlying MN. Gentle soft tissue retraction with frequent brief relaxation of retraction pressure is suggested (Fig. 6.5c).
(a) Superior position of the mental foramen due to resorption of the alveolar bone in the partially edentulous mandible. (b) Dehiscence of the IAC, where the IAN and the MN come to lie on the alveolar ridge crest. (c) Exposure of the MN with gentle traction and frequent relaxation minimizes the chance of nerve injury
Less common causes of nerve injury are related to placement of bone grafts (autologous, allogeneic, xenogeneic) during simultaneous implant placement. In cases of complex implant reconstruction, the bone graft material may be placed into the donor site with excessive force, thus severely compressing or even crushing the IAN. It is also possible that particulate bone materials placed in the vicinity of the mental foramen may migrate or become dislodged to impinge upon the MN as it exits the foramen, and this may cause significant scarring around the nerve and resultant paresthesia, including dysesthesia.
6.3 Evaluation of Implant-Related Nerve Injury
6.3.1 Evaluation of Nerve Injuries
Neurosensory disturbances are evaluated and documented in a standard fashion using the Medical Research Council Scale (MRCS) guidelines, as modified for the oral and maxillofacial regions, regardless of the etiology of the sensory nerve injury. The evaluation of nerve injuries is discussed in Chap. 10. Since many of these implant-related injuries result in dysesthesia, specific attention should be directed towards the time frame of the injury and the likelihood that pharmacologic management may be indicated.
6.3.2 Treatment
Timely repair of peripheral nerve injuries has always been the sine qua non for successful recovery of nerve function, especially since Seddon’s extensive experience with treatment of missile injuries to extremities during and following WWII. His comment [31], “(i)f a purely expectant policy is pursued, the most favorable time for operative intervention will always be missed…,” is as pertinent today as it was more than 60 years ago. As in all other causes of nerve injury, treatment of the patient with a dental implant-associated nerve injury is dependent upon the correct diagnosis of the injury and its timely management.
The perioperative administration of supportive medications has been advocated for patients undergoing procedures such as dental implants, mandibular osteotomies, and lower third molar removal that are associated with a significant risk of nerve injury. There is conflict in the literature between those who recommend beginning corticosteroids preoperatively [1] and others who advise waiting postoperatively for several days before initiating administration to allow for edema resolution and tissue perfusion of the medication [32]. Many surgeons routinely administer a single preoperative intravenous dose of a steroid (dexamethasone or hydrocortisone). Whether or not it is beneficial to initiate corticosteroid or anti-inflammatory (NSAID) medications after a nerve injury has occurred is questionable. Previous studies have documented the lack of benefit of corticosteroids administered to reduce cerebral edema in patients who have sustained closed head injuries. That the IAN, in a similar “closed box” situation, confined within the IAC, could benefit from a retroactively administered corticosteroid seems unlikely as well, although that data is conflicting.
An algorithm for the management of nerve injuries from dental implant surgery is shown in Table 6.1. The patient who complains of decreased or painful sensation following placement of dental implants should be requested to return to the office for evaluation. In some patients a nerve injury might have been suspected, if the patient complained of a paresthesia during local anesthetic injection or during the bone drilling preparation for implant placement. In most cases, however, the patient may be under intravenous sedation, and there is typically no indication during the procedure of a nerve injury. It is recommended that the patient be seen as soon as possible and convenient for the patient, preferably within 24 h, or the same day, if painful sensation is the chief complaint, so that adequate pain control can be established and rapport with the patient maintained. The exact nature of the complaint(s) should be ascertained. A general oral exam is performed to assess the healing status of the surgical site. Neurosensory testing (NST) is done to establish an objective baseline determination of the level of sensory dysfunction for further follow-up, as indicated.
A panoramic radiograph is obtained to determine the position of the implant(s) in relation to the IAN. If there is no close relationship of the implant and the IAC on the panoramic film, no repositioning or removal of the implant is indicated and should be done. The patient is followed expectantly with frequent repeat NST to assess progress of recovery of sensation. Those patients who go on to acceptable (to the patient) spontaneous recovery require no further active treatment. Patients who fail to regain acceptable sensory function within 3 (anesthesia) or 4 (hypoesthesia ± pain) months are referred to a microneurosurgeon for possible nerve exploration and repair. On the other hand, if there is superimposition of the implant over the IAC on the panoramic film, a CT or CBCT scan is obtained to determine whether this represents an encroachment upon the IAN or IAC, or simply a two-dimensional radiographic overlap that cannot be distinguished on the panoramic radiograph. If the CT demonstrates that the implant is not in contact with the IAC, the implant can be maintained and the patient is followed expectantly with serial NST to determine if spontaneous recovery occurs (see above) (Fig. 6.6a–e).
(a) CT-generated panoramic radiograph demonstrating the position of the implant #29 to the IAC in a patient with severe dysesthesia of the IAN following implant placement. (b) Cross-sectional view (coronal) of the same patient demonstrating impingement of the implant on the IAN within the IAC. (c) 3D reconstruction image with transparency of the osseous structures showing the IAC and the implant. (d) 3D reconstruction in cross-section. (e) 3D reconstruction in cross-section with digital removal of the osseous structures
On the contrary, if the implant is in direct contact with the IAC, then the implant should be repositioned immediately (prior to osseointegration) to create at least a 2-mm separation between the apical aspect of the implant and the IAC. If this implant repositioning encroaches unacceptably on the interocclusal clearance, then the implant should be removed and replaced with a shorter implant. This may allow the patient to maintain the implant despite the outcome of nerve injury. If the implant cannot be repositioned without compromising its stability, then it should be removed; consideration could be given towards the use of a shorter implant with a wider diameter to engage the bone for primary implant stability. The patient should be reevaluated with NST within 1 week. If there are signs of neurosensory recovery, no further treatment may be necessary, except for interval NST to document progress to satisfactory return of sensation (“useful sensory function,” or better). The implant can be restored if it has adequate stability and meets acceptable prosthodontic criteria for restoration. It should be remembered that if the implant was close to the IAC, that once the implant is restored and placed into function that neurosensory symptoms may occur during mastication whereby pressure is placed within the closed environment of the IAC. In this case either occlusal adjustment of the implant restoration or removal or “sleeping” the implant may be necessary depending upon the individual patient and clinical symptoms.
If, upon removal or repositioning of the implant, the patient does not show acceptable signs of recovery within 3 (anesthesia) or 4 (hypoesthesia/pain) months by serial NST, microsurgical consultation is indicated. Since the IAN lies within a bony canal, spontaneous recovery might occur due to “guided regeneration” of the nerve provided by the confines of the canal. In such a case, recovery of sensory function should begin (onset of symptoms, responses to NST) within 3 months after nerve injury. Microsurgical consultation can be considered earlier if there is a diagnosis of nerve transection (i.e., by direct visualization at the time of surgery). The so-called 12-week rule for the anesthetic patient has subsequently come to be recognized by many of those surgeons who care for nerve injuries as the standard for timely decision-making for the nerve injury patient who has an unacceptable persistent total loss of sensory function [3–6]. The patient who still has partial, but unacceptable, recovery of sensation at 3 months after nerve injury can be followed at regular (1-month) intervals as long as there is progressive improvement in subjective symptoms and NST at each visit. Once improvement ceases, it will typically not resume at some indeterminate time in the future, and a treatment decision is made at that time, depending upon the level of the sensory deficit according to the NST, the patient’s subjective assessment of his status, and any associated functional impairment.
6.4 Surgical Procedures for IAN Injuries from Dental Implants
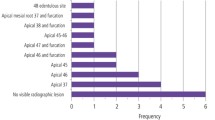
A list of microneurosurgical procedures that can provide surgical management of IAN injuries from dental implants is provided in Table 6.2. Figure 6.7 shows various microneurosurgical operations (note: these should include only nerve repairs secondary to dental implant-associated injuries). Although it is beyond the scope of this chapter to discuss all the techniques listed in Table 6.2, in a review of 167 IAN injuries [6], the most commonly performed operation was autogenous (sural or great auricular) nerve grafts (n = 71, 38.2 %) for reconstruction of a nerve gap, followed by internal neurolysis (n = 60, 32.3 %) when the nerve was not discontinuous. The need for reconstruction of a nerve gap was much more frequent with the IAN than that of the LN [4]. This has to do with the greater ease with which the proximal and distal stumps of the LN, contained within soft tissue, are able to be mobilized and brought into approximation for suturing without tension, than is the case with the IAN contained within a bony canal. This certainly has implications for the dental implant patient with a nerve injury, the majority of which are related to the IAN, and not the LN.
Microneurosurgical procedures: (a) External decompression of the IAN. (b) Internal neurolysis of IAN. Arrow shows intact fascicles. (c) Neuroma-in-continuity of the IAN. (d) IAN after excision of a neuroma-in-continuity. (e) Diagram of a direct neurorrhaphy. (f) Sural nerve graft for IAN reconstruction. Areas of microanastamosis (arrows). (g) Decellularized human nerve graft (Axogen Avance, Alachua, FL) for IAN reconstruction. (h) Diagram of guided tissue regeneration with conduit repair (entubulation). (i) Neurectomy and epineurial nerve capping. (j) Nerve redirection procedure
6.4.1 Nerve Exploration
High-resolution CT imaging can provide extensive detail of the bony anatomy, including the IAC. Although high-resolution magnetic resonance imaging (MRI) may be able to provide adequate visualization of the LN or MN [23], the ultimate view of the injured nerve requires visualization provided only by surgical exploration. Exploration of the IAN will reveal any gross anatomic abnormalities, the presence of bony fragments or foreign bodies (e.g., bone graft materials) that may be impinging upon the nerve, any contact of the nerve with the implant (Fig. 6.8), or the formation of scar tissue associated with the nerve (Fig. 6.9).
6.4.2 Dental Implant Removal
The technique of implant removal will depend upon whether the implant has achieved osseointegration. If the implant is fully osseointegrated, it is best removed using a trephine bur that cuts circumferentially around the implant allowing implant removal with minimal sacrifice of surrounding bone. A recently placed implant that has not osseointegrated can be removed using a torque wrench or handpiece. Appropriate bone preservation techniques should be used for possible future implant replacement. However, care must be taken not to further injure the nerve by compressing bone graft material onto the exposed nerve through the superior aspect of the IAC as described above. Additionally, it may be preferred to remove the involved implant and replace it immediately with a shorter implant. In the event that there is not adequate primary implant stability of the same diameter but shorter implant, a wider diameter and shorter implant can be used for immediate replacement.
6.4.3 Nerve Repositioning
CT imaging and navigation-guided implant placement have provided some protection against IAN injury since there is no magnification error associated with these imaging techniques, but proper planning is still essential. However, when preoperative imaging studies indicate an unfavorable location of the IAC either inferosuperiorly or mediolaterally, the implants cannot be placed without a high risk of injury to the IAN. It may be possible to place the implant in a position buccal or lingual to the IAC, but this may place the IAN at further risk for injury. Additionally, in such cases a nerve repositioning procedure may be indicated [11, 14, 18]. In this procedure the lateral cortex of the mandible is removed at the desired location for implant placement. The mental nerve can be freed from the foramen if the implants are planned in close proximity to this area. If necessary, the incisive nerve is transected at its junction with the mental nerve to allow lateralization of the IAN. The nerve is carefully lateralized from the canal to allow placement of the implant(s) medial to the lateralized IAN as needed (Fig. 6.10). An autogenous bone graft, either from the bone removed to unroof the IAC, or elsewhere, or freeze-dried bone allograft, is always placed between the repositioned nerve and the associated implants in order to prevent direct contact of the IAN and thermal transmission with the implant(s). Also, artificial material, such as calcium hydroxyapatite, should never be placed in direct contact with the nerve. A severe inflammatory reaction in the nerve, similar to a chemical burn with dense scarring, accompanied by considerable pain, is often the unfortunate result. Surgical treatment of such injuries is problematic. For further discussion of nerve repositioning, see Chap. 7.
(a) Schematic representation of anticipated implant placement in the posterior right mandible. (b) IAN lateralization. (c) Placement of two dental implants beyond the IAC. (d) Preoperative panoramic radiograph of failing dental fixed prosthesis and edentulous posterior mandible. (e) Placement of two dental implants lingual to the IAC after nerve lateralization. Bu Buccal; Li Lingual
6.4.4 Excision of Neuroma
Neuroma formation can be the result of direct drill injury, or direct or indirect implant injury to the IAN (Fig. 6.11a). A neuroma-in-continuity usually represents a partial nerve transection with subsequent healing predominated by scar formation and the presence of nonconducting nerve tissue. The vast majority of these injuries are repaired using nerve grafts (see next section) to restore the continuity of the defect following neuroma excision to healthy nerve tissue proximally and distally from the site of injury (Fig. 6.11b).
6.4.5 External Neurolysis (Decompression) and Internal Neurolysis
Compression of the IAN can be seen with collapse of the IAC, or impingement on the nerve by the implant or other foreign bodies (e.g., bone graft material). External neurolysis, or decompression, is the removal of surrounding bone, soft tissue structures, and/or foreign material around the nerve (Fig. 6.7a). In cases where the implant is found to compress the nerve (Fig. 6.8), repositioning of the nerve is an option for decompression (see previous section). Internal neurolysis is the opening of the epineurium to inspect the internal neural structures and decompress the individual nerve fascicles (Fig. 6.7b). If there is a continuity defect of one or more of the fascicles, then neurorrhaphy or nerve graft reconstruction is indicated. If the nerve is found to be intact, an external decompression and internal neurolysis are sufficient. Extensive or aggressive attempts at internal neurolysis carry the risk of scar formation and iatrogenic injury to the fascicles, so this technique must be performed with great care and precision.
6.4.6 Neurorrhaphy
Unlike the lingual nerve, injuries to the IAN are difficult to repair by direct neurorrhaphy due to the relative inability to mobilize and advance the IAN into approximation across a nerve gap without tension, unless the incisive nerve (IN) is transected to allow increased mobility of the nerve stumps. However, release of the IN leaves the patient with sensory loss in the lower incisor teeth and the mandibular labial gingiva. The stump of the transected IN may develop a stump neuroma, with the potential for neuropathic pain. These disadvantages should be weighed against considerations to attempt tension-free approximation of the IAN without interposition of an autogenous nerve graft.
6.4.7 Nerve Grafts
The sine qua non of a successful neurorrhaphy is to bring the proximal and distal stumps of a transected nerve together and suture them in this position without tension. When the surgeon is unable to accomplish this, reconstruction of the space between the two nerve stumps (the nerve gap) can be performed with an interpositional nerve graft [20]. Both autologous and allogeneic nerve grafts are can be utilized. The sural (SN) and greater auricular nerve (GAN) are the most commonly used autogenous grafts for maxillofacial nerve repairs (Fig. 6.12a, b). The SN provides a better size match and longer length than the GAN. The disadvantages of this graft are the vertical scar just posterior and superior to the lateral malleolus of the ankle, although a transverse incision could be used [24]; the added operative time to reposition the patient and access a distant surgical site; and the associated donor site morbidity (anesthesia of the lateral foot, temporary gait disturbance, pain) (Fig. 6.12c). The GAN is easily harvested along its superficial course lateral to the sternocleidomastoid muscle approximately 6 cm inferior to the ear lobe. The main disadvantages of the GAN are the neck scar, ear lobe anesthesia, and its smaller (than the recipient IAN or LN) diameter. The incision for harvesting the GAN is usually made in a natural skin crease in the lateral neck, and a careful closure usually results in an inconspicuous scar (Fig. 6.13). Loss of sensation in the lower part of the earlobe is seldom a concern to patients. When the diameter of the GAN is smaller than that of the recipient nerve, a cable graft (using multiple strands of GAN) can correct this discrepancy.
(a) One-year postoperative view of a healed Risdon incision in an 18-year-old female demonstrating minimal scar visibility. (b) Surgical scars (arrows) from submandibular incision to expose the IAN and neck incision to harvest a great auricular nerve graft in a 21-year-old African-American female 1 year after the operation
In addition, decellularized human nerve allografts (Axogen Avance, Alachua, Florida) are readily available for trigeminal nerve reconstruction (Fig. 6.7g). Ongoing studies to determine the success of this nerve in the maxillofacial area is pending, although the initial results are promising. It is another option to avoid donor site morbidity of autogenous nerve grafting.
6.5 Complications of Surgical Treatment
The main complications associated with microsurgical repair of nerve injuries from dental implants are related to the specific surgical procedure, expected sensory outcomes, timing of surgery, patient age and medical status, and risks of general anesthesia.
6.5.1 Specific Surgical Procedures
Surgical access to the IAN is dependent upon the location of the nerve injury, the planned procedure, and the surgeon’s preference. The IAN has a long course, branching from the mandibular nerve in the pterygomandibular space, traveling anteriorly until it enters the mandibular foramen on the medial mandible, continuing within the IAC, and, just before exiting at the mental foramen, dividing into its two terminal branches, the IN and the MN. Injuries to the IAN in the IAC and more proximally in the pterygomandibular space (needle injuries) are difficult to visualize and repair without performing a mandibular ramus osteotomy for additional access. Such operations are seldom done for nerve repair unless as part of tumor resection. However, when the proximal IAN is not accessible, or otherwise unrepairable, a nerve-sharing procedure can be done without the requirement of a mandibular ramus osteotomy [16]. In this operation, an autogenous sural nerve graft is used to connect the proximal great auricular nerve to the distal IAN. The IAN in the area of the third molar can be accessed via both transoral and transcutaneous incisions. The standard Risdon incision allows excellent access to the entire nerve from the area of the mandibular canal to the mental foramen. The main disadvantage of this access is the small possibility of permanent injury to the marginal mandibular branch of the facial nerve (less than 1 %) and the facial neck scar (especially in younger individuals that do not have a naturally visible neck crease). However, placement of the incision along the relaxed skin tension lines (RSTL), meticulous attention to closure, continued support of the healing incision with adhesive strips, proper skin care, and protection with sunscreens for up to 1 year after operation will enhance the likelihood of an inconspicuous scar (Fig. 6.13a). In African-Americans, the injection of the incision margins with a corticosteroid (e.g., triamcinolone) before closure, and on a monthly basis thereafter as indicated, reduces the risk of formation of a hypertrophic scar or keloid (Fig. 6.13b).
The IAN can also be exposed transorally via a variety of techniques including a modified sagittal split ramus osteotomy or by decortication (removal of the lateral cortex to create a window of exposure) (Fig. 6.14). The main disadvantage of the transoral approach is the reduced visibility and access, mainly posterior to the mandibular first molar. Although technically more difficult, successful nerve repairs, including interpositional grafting, may be accomplished via this approach.
6.5.2 Expected Sensory Outcomes
The fact that microsurgical repair of injured peripheral nerves achieves some degree of successful improvement in sensory function and reduction of pain in some patients has been established [12, 17, 29]. However, as in all operations on sensory nerves, the failure to improve sensation or relieve dysesthesia does occur in some patients. In our study of 167 patients who underwent IAN repair and returned for at least 1-year follow-up, the majority of patients complained preoperatively of numbness (n = 62, 33.3 %) or numbness with pain (n = 91, 48.9 %). Recovery from neurosensory dysfunction of the IAN (defined by the MRSC as ranging from “useful sensory function” to “complete return of sensation”) was achieved in 152 IANs (81.7 % with complete recovery or recovery to “useful sensory function”), while 18.3 % of nerves showed no or inadequate improvement [6].
6.5.3 Timing of Surgery and Age of Patient
The results of microsurgical intervention are related statistically to the length of time between nerve injury and microsurgical repair, as shown in previous studies. In our report of 222 repaired LN injuries, using the logistic regression model, the shorter the duration of time (in months) between nerve injury and repair, the higher the odds of improvement. This work is in agreement with that of Susarla who found a relationship between early repair of LN injuries and a more favorable outcome as judged by the patient [33]. In our series of 167 IAN repairs, the likelihood of functional sensory recovery decreased with increasing duration from nerve injury to its repair, and favorable surgical outcome was decreased with increased age of the patient [6]. It should be remembered that some studies have shown that time from injury to repair is not a significant factor, however. The significance of age and length of time from nerve injury to its repair is especially pertinent to the dental implant patient. Most of the patients who sustain dental implant-associated nerve injuries that failed to improve or resolve spontaneously and are referred for evaluation and treatment are greater than 50 years of age and had suffered their nerve injury more than 9 months prior to the initial consultation. These factors all potentially impact negatively on neurosensory recovery following any form of treatment.
6.5.4 Patient’s Medical Status and Risk of General Anesthesia
Preoperative evaluation of the patient’s medical status and risk assessment for general anesthesia for a microneurosurgical operation is performed as needed in consultation with other medical specialties. The risks of general anesthesia for a prolonged procedure include deep vein thrombosis with potential for embolization, pulmonary atelectasis with development of pneumonitis, and urinary tract infection from catheterization. These risks may be greater in the older patient population that most often presents for treatment of dental implant-associated nerve injuries. Measures to prevent these risks should be part of the routine care of the patient.
6.6 Postoperative Rehabilitation
Care of the nerve-injured patient does not end with the operation, provision of the usual pain relief, attention to incision care, and recommendations for resumption of normal activities and diet. Measures to enhance sensation and restore related orofacial functions must be included in the rehabilitation of the nerve-injured patient to achieve optimal results.
Younger individuals have better functional recovery after peripheral nerve injury than mature adults (those most likely to have dental implants and, therefore, more at risk of associated nerve injuries). Observations in the human patient are limited, but clinical experience indicates that the efficiency of neural regeneration is less in later life [26, 34]. Neuropsychological factors also influence the ability of the patient to recover successfully from a peripheral nerve injury following surgical repair. There is the need to learn new axonal connections with referral of sensory input to different areas of the CNS. Early in the recovery process, axons exhibit slower conduction time making interpretation more difficult for the CNS until accommodations can be achieved; this is a situation analogous to a baseball batter having to adjust to a change-up (dramatically slower speed) pitch. Although the older patient is slower to adapt to these changes imposed by recovery from a peripheral nerve injury, neuroplasticity (the ability of the brain to adapt) is still viable even into advanced age.
The concept of “sensory reeducation,” first developed by Wynn Parry [35] for rehabilitation of hand and upper extremity injuries, has been modified for the maxillofacial regions and shown to be successful in improving sensory function, once responses to pain and static light touch have returned [21, 25]. The goals of sensory reeducation for peripheral trigeminal nerve injuries are to improve or resolve synesthesia (failure to recognize the location of a stimulus), decrease hyperesthesia, improve recognition of the character and amplitude of stimuli (e.g., moving or stationary, sharp or dull, light or forceful application, size of area of contact), and decrease subjective differences (e.g., numbness) between the affected area and the corresponding normal contralateral area. Following microneurosurgery, sensory reeducation exercises are begun as soon as the area supplied by the repaired nerve begins to respond to painful stimuli and static light tough (usually within 3–6 months after surgery). The exercises are performed by the patient several times daily for a minimum of 12 months, or longer as needed. During this time the patient is monitored with NST to assess progress. Sensory reeducation can contribute to the nerve-injured patient’s ability to improve his level of sensory function and associated orofacial activities.
6.7 Conclusions
Treatment of the patient who has sustained a nerve injury from dental implant procedures involves prompt recognition of this complication, evaluation of sensory dysfunction and the position of the implant, and timely management of the injured nerve. In some patients, removal or repositioning of the implant, or replacement with a shorter implant, and surgical exploration and repair of the injured nerve will maximize the implant patient’s potential for a successful recovery from nerve injury.
Suggested Reading
Al-Bishri A, Dahlin L, Sunzel B et al (2005) Systemic betamethasone accelerates functional recovery after a crush injury to rat sciatic nerve. J Oral Maxillofac Surg 63:973
Bagheri SC, Meyer RA (2011) Microsurgical repair of injuries to the inferior alveolar nerve associated with dental implants. In: Steed MB (ed) Atlas of the oral and maxillofacial surgery clinics of North America
Bagheri SC, Meyer RA, Khan HA et al (2009) Microsurgical repair of peripheral trigeminal nerve injuries from maxillofacial trauma. J Oral Maxillofac Surg 67:1791
Bagheri SC, Meyer RA, Khan HA et al (2010) Retrospective review of microsurgical repair of 222 lingual nerve injuries. J Oral Maxillofac Surg 68(4):715–723
Bagheri SC, Meyer RA, Ali Khan H et al (2010) Microsurgical repair of the peripheral trigeminal nerve after mandibular sagittal split ramus osteotomy. J Oral Maxillofac Surg 68:2770–2782
Bagheri SC, Meyer RA, Cho SH et al (2012) Microsurgical repair of the inferior alveolar nerve: success rate and factors which adversely affect outcome. J Oral Maxillofac Surg 70(8):1978–1990
Bartling R, Freeman K, Kraut R (1999) The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg 57:1408–1410
Boyne PJ (1982) Postexodontia osseous repair involving the mandibular canal. J Oral Maxillofac Surg 40:69–77
Branemark P-I (1983) Osseointegration and its experimental background. J Prosthet Dent 50:399–410
Chaushu G, Taicher S, Haiamish-Shani T, Givol N (2002) Medicolegal aspects of altered sensation following implant placement in the mandible. Int J Oral Maxillofac Implants 17:413–415
Dario LJ, English R (1994) Achieving implant reconstruction through bilateral mandibular nerve reposition. J Am Dent Assoc 123:305–309
Gregg JM, Zuniga JR (2001) An outcome analysis of clinical trials of the surgical treatment of traumatic trigeminal sensory neuropathy. Oral Maxillofac Surg Clin North Am 13:377
Hillerup S (2011) Update on injuries related to injection of local anesthetics. In: Symposium: update on nerve injury, diagnosis and repair. Amer Assoc Oral Maxillofac Surg, 93rd annual meeting, Philadelphia, 19 Sept
Jensen O, Nock D (1987) Inferior alveolar nerve repositioning in conjunction with placement of osseointegrated implants: a case report. Oral Surg Oral Med Oral Pathol 63:263–266
Kraut RA, Chanal O (2002) Management of patients with trigeminal nerve injuries after mandibular implant placement. J Am Dent Assoc 133:1352–1354
LaBanc JP, Epker BN (1992) Trigeminal nerve reconstruction surgery using the great auricular nerve transfer technique. Oral Maxillofac Surg Clin North Am 4:459–463
LaBanc JP, Van Boven RW (1992) Surgical management of inferior alveolar nerve injuries. Oral Maxillofac Surg Clin North Am 4:425
Louis PJ (2001) Inferior alveolar nerve repositioning. Atlas Oral Maxillofac Surg Clin North Am 9:93–128
Meyer RA (1992) Applications of microneurosurgery to the repair of trigeminal nerve injuries. Oral Maxillofac Surg Clin North Am 4:405
Meyer RA (2001) Nerve harvesting procedures. Atlas Oral Maxillofac Surg Clin North Am 9:77–91
Meyer RA, Rath EM (2001) Sensory rehabilitation after trigeminal nerve injury or nerve repair. Clin North Am 13:365
Meyer RA, Ruggiero SL (2001) Guidelines for diagnosis and treatment of peripheral trigeminal nerve injuries. Oral Maxillofac Surg Clin North Am 13:383
Miloro M, Halkias LE, Chakeres DW, Slone W (1997) Assessment of the lingual nerve in the third molar region using magnetic resonance imaging. J Oral Maxillofac Surg 55:134–137
Miloro M, Stoner JA (2005) Subjective outcomes following sural nerve harvest. J Oral Maxillofac Surg 63:1150–1154
Phillips C, Blakey G, Essick GK (2011) Sensory retraining: a cognitive behavioral therapy for altered sensation. Atlas Oral Maxillofac Surg Clin North Am 19:909
Pola R, Aprahamian TR, Bosch-Marce M, Curry C, Gaetani E, Flex A, Smith RC, Isner JM, Losordo DW (2004) Age-dependent VEGF expression and intraneural neovascularization during regeneration of peripheral nerves. Neurobiol Aging 25:1361
Pogrel MA, Bryan J, Regezi J (1995) Nerve damage associated with inferior alveolar nerve blocks. J Am Dent Assoc 126(8):1150–1155
Pogrel MA, Thamby S (2000) Permanent nerve involvement resulting from inferior alveolar nerve blocks. J Am Dent Assoc 131(7):901–907
Pogrel MA (2002) The results of microneurosurgery of the inferior alveolar and lingual nerve. J Oral Maxillofac Surg 60:485
Queresby FA, Savell TA, Palomo JM (2008) Applications of cone beam computed tomography in the practice of oral and maxillofacial surgery. J Oral Maxillofac Surg 66:791–796
Seddon HJ (1947) Nerve lesions complicating certain closed bone injuries. J Am Med Assoc 135:691
Seo K, Tanaka Y, Terumitsu M et al (2004) Efficacy of steroid treatment for sensory impairment after orthognathic surgery. J Oral Maxillofac Surg 62:1193
Susarla S, Kaban L, Donoff RB, Dodson T (2007) Does early repair of lingual nerve injuries improve functional sensory recovery? J Oral Maxillofac Surg 65:1070–1076
Verdu E, Ceballos D, Vilches JJ, Navarro X (2000) Influence of aging on peripheral nerve function and regeneration. J Peripher Nerv Syst 5:191
Wynn Parry CB (1984) Brachial plexus injuries. Br J Hosp Med 32(3):130–132, 134–139
Ziccardi V, Steinberg M (2007) Timing of trigeminal nerve microsurgery: a review of the literature. J Oral Maxillofac Surg 65:1341–1345
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Bagheri, S.C., Meyer, R.A. (2013). Dental Implant-Related Injuries of the Trigeminal Nerve. In: Miloro, M. (eds) Trigeminal Nerve Injuries. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-35539-4_6
Download citation
DOI: https://doi.org/10.1007/978-3-642-35539-4_6
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-35538-7
Online ISBN: 978-3-642-35539-4
eBook Packages: MedicineMedicine (R0)