Abstract
Nowadays, permanent prostate brachytherapy (PPB) is a mature treatment option for patients with localised cancer. With the introduction of transrectal ultrasound–guided perineal implantation by Holm et al. in 1983, a new era in prostate brachytherapy was started. The technique was refined by the Seattle group of Ragde and Blasko, and this technique is still used in many centres over the world. Around the millennium-change guidelines were published for the selection of patients according to their T stage, PSA level and Gleason score. Patients with low-risk features have excellent clinical outcome with tumour control at 10 years of more than 90%, as shown in this chapter.
Also, patients with intermediate-risk features (T2b; PSA 10–20 ng/ml; Gleason sum 7) can be cured with PPB, with a 10-year tumour control of 80–90%.
There is a substantial improvement in technique of implantation over the past 30 years. From loose seeds, using a Mick applicator, we moved to stranded seeds and later also again back to loose seeds with complete afterloading using the FIRST system. Also, treatment planning was more and more refined. It started with a nomogram, followed by preplanning some weeks before the implant procedure and now intraoperative planning at the beginning of the procedure, interactive planning with position feedback from the needle position and inverse planning, using dose constraints for normal tissues.
Not only is tumour control high, but at the same time toxicity is very low. Major incidents are seldom and almost always temporarily. The most experienced complication is acute retention some weeks after implantation. Careful selection of patients, excluding men with large prostates and high IPSS levels reduces the chance of acute retention.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Gleason Score
- Prostate Volume
- International Prostate Symptom Score
- Seed Implantation
- Prostate Brachytherapy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
10.1 Introduction
Prostate cancer is the most frequent male malignant tumour in the Western world and affects about 10% of all men. In localised prostate cancer, various treatment options are available such as surgery, either by open, laparoscopic or robot-guided surgery, external beam irradiation, brachytherapy with low dose Iodine-125 seeds or an HDR Iridium-192 source, cryotherapy, HIFU and active surveillance.
Brachytherapy for the treatment of prostate cancer is already mentioned in 1913 by Pasteau and Degrais using radium in a silver tube in the urethra (Pasteau and Degrais 1914). Other techniques were executed as well, such as radium needles inserted into the prostate through the rectum, via the perineum or bladder. These techniques with radium resulted in severe rectal and bladder complications including ulceration and fistulae. Flocks used radioactive gold (Au-198) colloidal solution injections (Flocks et al. 1954). Au-198 has a short half-life of 2.7 days and emits short-range beta radiation plus gamma radiation. Due to difficulties with the use of colloidal gold, Au-198 gold seeds were developed for insertion into the prostate, either alone or in combination with EBRT. The radiation exposure hazard associated with the high energy of Au-198, however, made these techniques unpopular. The high morbidity rate of early brachytherapy techniques and the advent of megavoltage radiation with Cobalt and somewhat later linear accelerators reduced interest in brachytherapy in the 1960s.
Hilaris and Whitmore at the Memorial Sloane Kettering Cancer Centre in New York introduced Iodine-125 seeds in 1970 (Whitmore et al. 1972). I-125 has a half-life of 60 days and emits low energy photons (28 keV). Due to the low energy, there are nearly any radiation exposure problems. The seeds were implanted in the prostate by a retropubic approach in combination with bilateral regional lymph node dissection. They found a 5-year survival of 79% in a population of 606 patients treated from 1970 to 1980, strongly related to T stage (T1 96%, T2 76%, T3 69% and T4 13%). Recurrence rate was highly related to tumour grade (Fuks et al. 1991). A small series from the Netherlands Cancer Institute showed similar results with 52% versus 48% local recurrences for the Whitmore series (Roeleveld et al. 1996). We know now that the retropubic approach is inadequate for a proper implant due to the poor guidance of the needles by the index finger in the rectum.
In 1980, Charyulu already described a perineal technique where patients received EBRT and a boost dose with Radon-222 (Charyulu 1980). The position of the needles was guided by a template, and the tip of the needle was checked with radiography of the Foley balloon. Kumar improved this technique, using C-arm fluoroscopy to guide the needles (Kumar and Bartone 1981).
A breakthrough was the introduction of the transrectal ultrasound (TRUS)–guided perineal technique by Holm et al. (1983). A perspex template was attached to the ultrasound probe to guide the needles into the prostate. This technique was refined by the Seattle group and is still the most common way to perform permanent prostate brachytherapy (Blasko et al. 1987).
Because of better staging modalities such as TRUS and magnetic resonance imaging (MRI) and the awareness by men of prostate cancer, the majority of patients are nowadays diagnosed with a low-risk prostate cancer, resulting in a high cure rate for most patients.
10.2 Patient Selection
Guidelines for permanent prostate brachytherapy (PPB) are published by ASTRO (Nag et al. 1999, 2000) and by ESTRO (Ash et al. 2000). According to T stage, Gleason sum and PSA value patients can be categorised in three risk groups (Table 10.1). Besides tumour characteristics, also functional characteristics are taken into account. International prostate symptom score (IPSS), urodynamic parameters such as bladder volume, maximum flow rate and residue are considered to be also important. In the low risk group patients are included with T1c–T2b tumours, Gleason sum < 7 and PSA < 10 ng/ml. These are excellent patients for PPB, with cure rates of over 90% at 10 years (see results). The opposite is the high-risk group with T3, or Gleason > 7, or PSA > 20, or Gleason =7 and PSA 10–20 ng/ml. These patients in general are not treated by PPB, although it is not clear whether other modalities show better outcome. The intermediate group consists of T2c, or Gleason 7, or PSA 10–20 ng/ml. These patients in general are still candidates for PPB, with somewhat lower cure rate than low-risk patients as will be described in the results.
Preoperative work-up includes PSA, digital rectal examination, TRUS of the prostate, CT or (preferably) MRI of the pelvis. Bone scan and other imaging modalities are not recommended for low-risk and (low tier) intermediate-risk patients. A previous TURP is a relative contraindication since a large TURP defect will result in the loss of seeds while urinating. Furthermore, these patients are at higher risk for urethral necrosis, strictures and incontinence (McElveen et al. 2004). It is advised to wait for 6–12 months after TURP to perform PPB. Even so, TURP after PPB should be postponed for several months to reduce complications.
Patients with prostate volumes more than 50 cc are not good candidates for PPB. Pubic arch interference may hinder the placing of the needles close to the bony structures. Further, the contour may not fit in the template and the TRUS image quality is worse than in smaller prostates. Also, a large number of seeds are needed, resulting in more complications such as acute retention. Androgen ablation therapy (ADT) may reduce the prostate volume with approximately 30% and can be used to downsize the prostate (Lee 2002). However, in volumes over 80 cc, the volume reduction still will be insufficient for PPB in most of these patients.
In Europe mainly iodine seeds are used for PPB. In the USA, still a substantial number of patients are treated with Palladium-103. The energy is similar, but the half-life is 17 days in place of 60 days and therefore delivers a much higher dose rate than iodine. Although palladium is advocated for fast growing tumours (Gleason > 7), there is no clinical confirmation of this hypothesis.
10.3 Treatment Planning
10.3.1 Preplanning
Preplanning is performed to measure the size of the prostate to order the number of seeds and making a preplan for seed implantation. This is in general done by TRUS. With the stepping unit of the support frame (Fig. 10.1), transversal slices are made at increments of 5 mm through the prostate from base to apex. In general, the prostate volume will be larger with this method than with routine transaxial measurement using the equation L × W × H × 0.52. The prostate should be in the middle of the template; this means that the urethra is not always in the middle of the gland in case of hyperplasia.
From this volume study, the contour of the prostate is depicted on each slice (Fig. 10.2). The images are digitised and fed into a dedicated planning computer. The planning treatment volume is routinely with a margin of 5 mm outside the depicted contour in lateral and ventral direction. However, for the dorsal side close to the rectum, often, a smaller margin is used to avoid rectal damage as stated in the update of the GEC-ESTRO guidelines (Salembier et al. 2007). Teh (Table 10.2) found in prostatectomy material of 712 patients that the majority of extracapsular extension is within a few millimetres from the capsule (Teh et al. 2003). Schwartz describes the association of extraprostatic extension with preoperative PSA, percentage of cancer in biopsy cores, and clinical tumour stage (Schwartz et al. 2007).
10.3.2 Needle Loading
Per definition the dose in brachytherapy is inhomogeneous. To exploit this inhomogeneity further, differential loading of the needles can avoid high dose to the prostatic urethra and rectum. With differential loading (that is not filling a needle with seeds at a fixed distance from each other, but placing less seeds and extra spacers to reduce dose, or place extra seeds without spacers to increase the dose), one can more or less paint the dose over the prostate volume. Typically, the highest dose will be in the peripheral zone with areas of 200% and more of the prescription dose. For the urethra dose, 100–150% of the reference dose is acceptable and will not lead to severe urethral complications. For the rectum dose, 100% should be the limit to avoid rectal injury. The planning system will also give dose volume histograms (DVH), a very helpful tool in determining the best configuration of the seed placement and the quality of the implant, avoiding overdoses in critical parts.
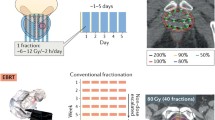
The prescription dose for iodine seeds is 145 and 120 Gy for palladium for monotherapy. In combination with EBRT the doses are reduced with 25–40%. The required number of seeds depends on the volume of the prostate and the activity of the seeds. In general, the activity is 0.4–0.5 mCurie and the number of seeds lower with higher active seeds.
10.3.3 Other Planning Strategies
In place of preplanning, several other planning strategies can be performed. One can use intraoperative planning. In this situation, a preplan is made before the implant procedure with the patient already anaesthetised on the treatment table in lithotomy position and immediately execution of the plan. Also one can perform interactive planning, that is, stepwise refining the plan using computerised dose calculations according to the actual needle positions. With this planning technique variation in patient set-up, swelling and gland movement can be accounted for. Even more accurate would be dynamic dose calculation using continuous seed position feedback. However, this is still not available because the seeds are difficult to identify on TRUS. Several centres perform inverse planning, using constrains for critical tissues in and around the prostate (Martin et al. 2007).
10.4 Treatment Techniques
10.4.1 Patient Preparation
The procedure is performed on an outdoor basis or with one night of hospitalisation. Patients should have an empty rectum to optimise TRUS. This means a diet and laxative for 1 week and a rectal enema about 1 hour before the procedure will start. The treatment can be done with spinal/saddle block or general anaesthesia. Most centres give prophylactic antibiotics, either for several days or in one bolus before the implant. Since the needles are placed transperinealy, in contrast to the transrectal route for biopsies, there is hardly any infection.
The patient is placed in lithotomy position on the edge of the table in the same position as during the preplanning. A Foley catheter is introduced to visualise the urethra. Aerated gel (lubricating gel plus air to make small bubbles) can help to visualise the urethra. The scrotum is displaced from the operating field and fixed with adhesive dressing, and the perineum is washed with antiseptic solution.
The ultrasound probe is inserted and positioned under the prostate. A new volume study is performed and verified with the preplan (if done earlier). A volume study can also be done with a rotating probe in the rectum, making a 3D scan of the prostate.
10.4.2 Implant Procedure
Although there are several techniques for prostate implantation, in essence, the technique is the same, viz. the insertion of needles in the prostate guided by TRUS and the placing of the sources at the right position.
Needles can be preloaded according to the preplanning or can be afterloaded when the configuration for each needle is established. With the Mick applicator (see Fig. 10.3), single seeds are placed in the prostate according to the dose plan. One can also use strands, with seeds connected at a distance of 5 mm and embedded in a stiff polyglactin suture. In both situations, the seeds are inserted manually into the prostate. In Utrecht, we developed strand holders to facilitate the insertion of a strand into the needle and subsequently into the prostate using the obturator of the needle (Fig. 10.4). Also, the holder gives radiation protection while inserting the seeds. With the Fully Integrated Radiotherapy Seed Treatment (FIRST) system (Fig. 10.5) single seed configurations are composed by a computer and inserted automatically into the prostate. With all systems differential loading can be performed. The Bard company created a special system to link seeds with spacers according to the plan (Fig. 10.6). In literature, there are publications that single seeds may result in a better dose distribution and even a better clinical outcome. Moerland found a significant larger decline of post-implant D90 (dose received by 90% of prostate volume) for stranded seeds as opposed to loose seeds (Moerland et al. 2009). Saibishkumar described a greater loss of seeds with strands compared with loose seeds (Saibishkumar et al. 2009). However, prostate dosimetry on days 7 and 30 was similar between both types of seeds. Reed found in the only two data-randomised comparison a higher post-implant D90 and V100 value for loose seeds. The results were based on only 62 men. In some cases, loose seeds were added to the stranded seed treatment (Reed et al. 2007). Hinnen assessed the clinical outcome in terms of biochemical no evidence of disease (bNED) from PPB for loose seeds (358 patients) and stranded seeds (538 patients) (Hinnen et al. 2010 b). He found 5-year bNED of 86% and 90% (95% confidence interval) for strands and loose seeds, respectively, and an associated biochemical failure reduction of 43% for loose seeds.
Stabilising needles are helpful to reduce movement of the gland during the insertion of the needles. One can introduce all needles first, afterloading the needles with the appropriate number of seeds or one can insert a needle and insert the seeds, or use preloaded needles prepared by the vendor according to the configuration of the preplan. During the procedure, the planning can be adjusted to the exact position of the needle, taking into account a different route of the needle than planned (interactive planning). When all seeds are placed in the prostate, fluoroscopy can be done to verify the number of seeds in the prostate (Fig. 10.7). Also a C-arm with CT option can be used, to get a better insight of the position of the seeds over the prostate volume. If necessary, extra seeds might be placed (Westendorp et al. 2011).
After recovering from the anaesthesia, the Foley catheter can be removed. When the patient urinates spontaneously, he can return back home. Patients receive an alpha blocker to increase the urinary flow. Pain medication is seldom required. Physical exercise is allowed, but the patient should refrain from bicycling for one or more months depending on the urinary symptoms because this gives extra irritation of the prostatic urethra.
10.4.3 Postplanning
It is recommended to do a postplanning approximately 1 month after the brachytherapy procedure. Swelling as result of the insertion of all needles will have disappeared by that time. CT or MRI can be used for imaging of the prostate and the seeds, with CT the seeds are better visualised, with MRI the prostate is better imaged and fusion of both modalities is the most appropriate (Villeirs et al. 2005). From the post planning the dosimetric parameters can be calculated by the planning computer. DVHs are useful indices considering the implant quality. What exactly is a good implant is still under debate. A D90 (dose of 90% of the prostate) value of more than 140Gy is recommended (Stock et al. 1998). Kao evaluated 643 patients after PPB with D90s of 180 Gy or greater and found excellent 5-year bNED of 96.5% for the whole group with 97.3% for low-risk patients and 92.8% for intermediate-/high-risk patients (Kao et al. 2008). However, Ash showed also good results with lower D90s (Ash et al. 2006).
10.4.4 Radiation Safety
Safety procedures include exposure measurement before discharge, information to the general practitioner and information for the patient and his relatives. Although the radiation exposure to other persons is very limited, it is advised that patients should not have close contact with young children and pregnant women for 2 months. The wife of the patient can sleep in the same bed with the patient. Measurements from South Africa with radiation monitors for the family and pets did not show any radiation, except for the wife sleeping in the same bed. However, still the radiation exposure was well below the International Commission on Radiological Protection (ICRP) limits with a lifelong dose of 0.1 mSv for iodine-125 and 0.02 mSv for palladium-103 (Michalski et al. 2003). Sexual intercourse is permitted, but a condom should be used during the first ejaculations since an iodine seed may be lost through this way. Seeds might disappear with the urine or can migrate within the body, mainly into the lung or regional lymph nodes. Although second primary cancer (SPC) such as bladder cancer may appear, the incidence is very low and should not be used as an excuse to refrain from brachytherapy (Singh et al. 2010). The ICRP considers the risk of SPCs after PPB negligible (Cosset et al. 2004).
Safety monitors in shops and warehouses are not triggered by the seeds. However, at some airports in the USA and in Russia, radiation monitors are used, and patients might be stopped up till 6 months after seed implantation. These patients should have a declaration from the hospital to enter the country.
10.5 Combined Treatment
Combination of PPB and EBRT is advocated for intermediate-risk patients with a higher chance for extracapsular extension (Blasko et al. 2000). The same group from Seattle reported on the 15-year bNED in clinical T1–T3 following combined EBRT and PPB. At 15 years, the bNED results were 88% for low-risk, 80% for intermediate-risk and 53% for high-risk patients (Sylvester et al. 2007). Critz shows also good results with the combined approach, but results are not better than with seeds alone, both in clinical outcome and side effects (Critz and Levinson 2004). However, there are no randomised studies to prove this. Several arguments are mentioned in favour for combined treatment. A higher dose outside the prostate capsule can be achieved to eradicate tumour cells outside the prostate. It also may eradicate tumour in lymph nodes and it results in a higher total dose to the prostate. Contra-arguments are that a dose of 40–55Gy with EBRT is too low to eradicate significant tumour, especially more than 5 mm outside the prostate contour. According to Teh, the majority of extracapsular growth is within 2 mm from the capsule, and if more it should be visible on MRI and TRUS, making the patient not suitable for PPB (Teh et al. 2003). In general, PPB will give such a high dose to prostate and margin that extra dose is not necessary. Finally the combined approach is more expensive and may result in more side effects. Blasko stated that combined therapy is perhaps indicated in centres with limited experience, to homogenise the total dose within the prostate (Blasko et al. 2000).
10.6 Results
According to a combination of PSA value, Gleason score and sum, and T-stage patients can be categorised in three risk groups, low, intermediate and high risk (Table 10.1), although systems in use in Europe and the USA may differ in criteria (Table 10.3). In general, only low- and intermediate-risk patients are considered candidates for PPB.
It is recommended to use the classification as published by GEC-ESTRO (Ash et al. 2000).
10.6.1 Low-Risk Patients
Low-risk patients are defined as T1c-2b, PSA < 10 ng/ml and Gleason sum ≤6. Because randomised studies are not available, data of clinical outcome are results from single institutions or combined from several centres. Follow-up time in large series is often more than 5 and even 10 years. Table 10.4 is showing excellent outcomes with percentages from 82% to 89% for bNED and around 95% for disease-specific survival (Beyer and Brachman 2000; Grimm et al. 2001; Battermann et al. 2004; Sharkey et al. 2005; Potters et al. 2005; Zelefsky et al. 2007; Hinnen et al. 2010a; Henry et al. 2010; Taira et al. 2011). In some articles, PPB is compared with other treatment modalities such as prostatectomy and EBRT (Pickels et al. 2010; Kupelian et al. 2004; Tward et al. 2006; Colberg et al. 2007; Jabbari et al. 2010). From these data, it is clear there is no significant difference in tumour control after PPB and prostatectomy. Only in the Kupelian paper, there is a significant lower outcome for patients irradiated with and insufficient external beam dose of < 72 Gy (Kupelian et al. 2004). Pickles and Morris describe a match-pair analysis of 601 patients treated with PPB or 3D conformal EBRT. The 5-year results of bNED were 95% for PPB and 85% for EBRT and after 7 years, still 95% for PPB, but only 75% for EBRT. Higher late toxicity was found for PPB for urinary symptoms and worse for bowel symptoms after EBRT. Colberg reported on 741 patients from one institution treated with prostatectomy (391 patients) or PPB (350 patients, 35% with 125-I and 65% with 103Pd). Only 8% were treated with combined PPB plus EBRT; 25 patients received ADT to downsize the prostate. At a median follow-up of 42 months, bNED was identical for the favourable group (93% vs. 92%), the intermediate group (70% vs. 70%) and poor group (50% vs. 52%) (Colberg et al. 2007). Tward looked at 60,290 patients from the SEER program with low and intermediate prostate cancer for prostate-cancer specific mortality (PCSM) and any-cause mortality (ACM). Median follow-up was 46 months. For patients age <60, PCSM at 10 years was 1.3% for surgery, 0.5% for PPB and 3.75% for no definitive treatment. Men over 60 had PCSM of 3.8%, 5.3% and 8.4%, respectively. On univariate and multivariate analysis, both prostatectomy and PPB had statistically equivalent PCSM and CSM (Tward et al. 2006). In the paper by Jabbari, also proton boost was included, but the conclusion of the paper was the finding of excellent results for PPB, suggesting at least equivalent 5-year bNED rates and a greater proportion of men achieving lower PSA nadirs compared with 3D-CRT or CPBRTB (Jabbari et al. 2010).
10.6.2 Intermediate-Risk Patients
Intermediate-risk patients (T1c-2c; Gleason 7; PSA 10–20 ng/ml) show good results as well, as can be seen in Table 10.5. Definitions of intermediate-risk cases and selection criteria may be different from series to series, and PPB may be combined with external beam radiotherapy and/or androgen deprivation therapy (Kupelian et al. 2004; Merrick et al. 2005a; Datolli et al. 2007; Morris et al. 2009; Munro et al. 2010). Both for the combination of EBRT plus seeds and the use of seeds plus ADT, it is not proven to be better than PPB alone (Merrick et al. 2005a). Henry described 1,298 patients, of whom 44.2% received ADT and found an association with poorer overall biochemical control rates, particularly in the intermediate risk group. She explained this difference that in patients with higher percent positive biopsy scores, the presence of perineural invasion, or Gleason 4 + 3 histology received ADT (Henry et al. 2010).
Hinnen reported an improvement in outcome for patients in the past decade compared with earlier experience in Utrecht for intermediate-risk patients since the use of intraoperative planning. This might not only be attributed to intraoperative planning but also to better patient selection by better (MRI) imaging, improved guidelines for implantation or greater consistency in biopsy Gleason score. However, for low-risk patients, there was no improvement, probably because the results for these patients already are very favourable (Hinnen et al. 2010a).
As was discussed earlier, outcome after PPB was found related to the D90 (dose to 90% of the prostate) over or under 180Gy and implantation technique using stranded or loose seeds (Ash et al. 2006; Piña et al. 2010; Hinnen et al. 2010b).
10.6.3 Gleason Sum 3 + 4 or 4 + 3, Does It Matter?
Results from literature concerning results in Gleason 3 + 4 and 4 + 3 give either a poorer prognosis for 4 + 3 tumours or not for all treatment modalities. Wright looked at prostate cancer–specific mortality for these groups of patients after surgery and radiotherapy and found an increased risk of recurrence or progression and specific mortality in those with Gleason 4 + 3 versus 3 + 4 (Wright et al. 2009). Merrick described a series of 530 patients with Gleason 3 + 4 (300 patients) or 4 + 3 (230 patients). At 10 years, primary Gleason score did not impact survival, while deaths from cardiovascular disease or second malignancies were 9.6 times more common than death from prostate cancer (Merrick et al. 2007).
10.6.4 High-Risk Patients
A significant lower cure rate is found in high-risk patients (≥T2c; Gleason > 7; PSA > 20 ng/ml) after all treatment options. This may be due to the fact that a substantial number of them will have microscopic metastases. In the treatment of patients without traceable metastases brachytherapy can be used, either as monotherapy or in combination with EBRT and/or ADT. Many of these combined treatments are performed successfully using HDR brachytherapy (Galalae et al. 2002; Martinez et al. 2010). For patients categorised as high risk due to a PSA value over 20 ng/ml and/or Gleason sum higher than 7, PPB might still be an option. Stone reports good results for these patients with PPB at a D90 of more than 200 Gy (Stone et al. 2010).
10.6.5 Does Age Matter?
Patients before 60 years of age should not withhold PPB according to data in literature (Merrick et al. 2006; Shapiro et al. 2009; Burri et al. 2010a, b). Shapiro found freedom from progression at 10 years after PPB, in patients with low, intermediate and high risk of 91.3%, 80.0% and 70.2% compared to 91.8%, 83.4% and 72.1%, respectively, for men before 60 years versus men of 60 years or older. Interestingly, high rates of cause-specific and biochemical progression- free survival after PPB in 145 consecutive men over 74 years of age were reported. Overall survival and non-cancer deaths were best predicted by tobacco status (Merrick et al. 2008).
Second primary tumours do occur, but still the number is negligible as mentioned earlier in this chapter (Liauw et al. 2006). Hinnen found in a series of 136 PPB patients, compared with 87 patients after prostatectomy with a median follow-up of 5 years for both a low incidence of second primary cancers. However, in patients under 60, there was a higher chance for bladder cancer after PPB (Hinnen et al. 2011b). Moon looked at the SEER registry for men with incident prostate cancer and evaluated type of treatment, tumour stage and grade, and age at diagnosis. Data were evaluated for second primary cancers beginning 5 years after treatment. Patients after EBRT had significantly higher odds of developing second cancers compared with men without radiation therapy, both in the treated area (bladder, rectum) but also in areas not potentially related to radiation. Lowest odds of developing cancers were found with men after PPB (Moon et al. 2006).
10.7 Morbidity
The majority of patients will experience some degree of urinary irritation with complaints of higher frequency, reduced flow, urge and burning while urinating. These symptoms are the result of swelling of the prostate because of the needles that have been placed. After a few weeks prostate radiation inflammation will take over the symptoms. Although many men will recover in weeks or months, in a small number of men, symptoms become worse and may result in urinary obstruction. The incidence rate varies in literature from 5% to 20% and is related to prostate volume and initial voiding problems with high IPSS (Terk et al. 1998; Blasko et al. 2002; Crook et al. 2002; Martens et al. 2006). Also after combined treatment, a similar rate of obstruction is found. The majority of obstructed patients can be helped with a Foley catheter for some weeks. Occasionally, the problems remain and a suprapubic catheter should be placed to drain the bladder. This is more comfortable and the patient himself can monitor his voiding pattern. It is advised to wait at least 6 months and better 12 months before surgical procedures are performed to reduce the chance for incontinence. If surgery is performed, the procedure should be as minimal as possible (median incision, bladder neck incision, or mini TURP). Incontinence rate is less than 1%, only patients who had previous TURP have a higher chance for incontinence (Blasko et al. 2002; Stone and Stock 2002; McElveen et al. 2004). Keyes presented a paper on predictive factors for acute and late urinary toxicity in 712 patients. IPSS returned to baseline at a median of 12.6 months. On multivariate analysis, higher baseline IPSS resulted in a quicker resolution of their IPSS. Higher D90, maximal post-implant IPSS, and urinary retention slowed IPSS resolution time. Actuarial 5-year late urinary toxicity Grade 3 and 4 was reported 6.2% and 0.1% (Keyes et al. 2009a). The same group also report on urinary flare in the same group of patients. Typically, this is found 16–24 months after implant with an incidence of 52% (flare definition of an IPSS increase ≥5) and 30% (flare ≥8). Patients with symptoms had a resolution of these symptoms within 6 months of 65% and at 12 months of 91% (Keyes et al. 2009b).
Late complications are pain in the perineum, urethra strictures and rectal bleeding. Since the use of intraoperative dose planning, the rate of these complications is reduced considerably (Salembier et al. 2007). All these complications are rare nowadays and recover often spontaneously with pain medication, alpha blockers or in severe and persisting situations a treatment session of hyperbaric oxygen. Fistulae and other grade 4 toxicity are reported 0–2% in experienced hands (Stone and Stock 2002).
Erectile dysfunction is found in 20–50% of men, depending on age, sexual activity, smoking, diabetes and use of medication, e.g. β-blockers (Robinson et al. 2002; Merrick et al. 2005b). Sildenafil and other stimulating drugs can help to improve erections. Especially in younger patients, a decrease of erection may appear a few months after seed implantation and in general will recover spontaneously.
From a study in Utrecht, it was shown that patients after 6 years had the same quality of life score as before iodine implantation (Roeloffzen et al. 2010). Malcolm found after 2 years from open or RALP prostatectomy, cryosurgery or PPB in all domains (bother score, urinary and sexual function) higher scores after PPB (Malcolm et al. 2010). Crook reported on the outcome of the SPIRIT study on the comparison of health-related quality of life 5 years after treatment. Of 168 survey responders 60.7% had PPB and 39.3% surgery. Median follow-up was 5.2 years. There was no difference in bowel or hormonal domains, but patients after PPB scored better in urinary and sexual domain, and in patient satisfaction (Crook et al. 2011).
10.8 Management of Recurrences
After PPB, patients are followed by both the radiation-oncologist and the urologist. PSA levels are closely monitored. If PSA levels are rising, this indicates local recurrence, distant recurrence, local plus distant recurrence and most common PSA bounce. In the last case, it means there is a temporary PSA increase about 1.5 years after seed implantation. PSA can increase with up to 2 ng/ml. Kirilova examined patients with a bounce after iodine seed implantation with 3D MRI spectroscopy and found diffuse metabolic activity during an ordinary bounce, whereas in case of recurrence, there was more focal activity (Kirilova et al. 2011). This rise is most likely caused by death of many normal prostate cells due to hypoxia. It was found that this phenomenon is related to a better outcome than in patients without this rise (Crook et al. 2007; Hinnen et al. 2012). PSA levels should come down to non-measurable levels, but this might take several years. Grimm observed a period of 6 years before 80% of the patients had reached their nadir of <0.2 ng/ml (Grimm et al. 2001). If PSA remains to increase, further diagnostic examination is mandatory to differentiate between distant or local recurrence. However, in many cases, it is not possible to find either a local or distant tumour recurrence. MRI, especially dynamic contrast-enhanced (DCE) MRI can help to locate local recurrence by showing a higher blood perfusion (Futterer et al. 2006). Of course, histological proof is needed before calling the finding a local recurrence. Although the possibilities are limited, still some options are open for the patient. This is highly related to the initial risk group and the delay between the first implantation and the onset of recurrence. In general, PSA increases soon after brachytherapy indicates distant spread, especially when the PSA doubling time is less than 6 months. Second brachytherapy is an option as described by (Moman et al. 2010). She advocates only doing this second treatment if the recurrence is located in one lobe. Then a seed implant of that lobe is performed with much lower toxicity than with a full implant. In a previous paper, Moman found in a series of 31 local recurrences after initial brachytherapy (11 patients) or EBRT (20 patients) freedom for biochemical recurrence of 51% after 1 year and 20% after 5 years. Toxicity was high with genitourinary tract grades 1, 2, and 3 of 29%, 58% and 3% in the acute phase and 16%, 39% and 19% in the late phase, respectively. For gastrointestinal toxicity, this was 45%, 10% and 0% in the acute phase and 48%, 3% and 6% in the late phase, respectively (Moman et al. 2009). Nguyen showed a similar major toxicity of 30% versus 29% but with a much better tumour outcome with 70% failure free after 4 years. However, in this series only low-risk patients were candidates for salvage brachytherapy (Nguyen et al. 2007). Burri published the results from the Mount Sinai group on 37 patients (32 EBRT and 5 PPB) with a median follow-up of 86 months. Salvage brachytherapy was associated with a 10-year bNED of 54% and cause-specific survival of 96%. Presalvage PSA < 6 ng/ml was significantly associated with improved bNED. Toxicity was low, but with three Grade 3 toxicities and one Grade 4. Toxicity was correlated with pelvic lymph node dissection (Burri et al. 2010 b). Another option is salvage surgery. In case of prostatectomy, the same criteria can be used to consider a patient candidate for salvage surgery and might be successful in well-selected patients. Bianco reports on 100 consecutive patients with local recurrence after EBRT (58 patients) and after PPB (42 patients). The overall 5-year progression-free probability was 55%. Preoperative PSA was the only significant predictor of disease progression with probability of 86%, 55% and 37% for PSA level of <4, 4–10, and >10, respectively (Bianco et al. 2005). In an earlier paper by the same group, toxicity was described. In patients operated after 1993, the major complication rate was 13%, significantly less than the 33% from previous experience. Urinary incontinence was reported in 68% of patients, requiring one pad a day or less, while 23 patients needed an artificial urinary sphincter (Stephenson et al. 2004). External beam irradiation with IMRT can be a possibility, although there is not much literature available. Salvage seed implantation after failure of EBRT is an option, again with the same criteria as mentioned above (Beyer 2004; Lee et al. 2008).
10.9 Discussion and Conclusions
Early experience with permanent prostate brachytherapy was rather dismal. However, the rationale to deliver a high local dose with sparing of normal tissues remained appealing. With the introduction of the perineal technique, using TRUS for guidance of the needles, much better results were obtained and gave PPB a solid place in the armamentarium for the treatment of localised prostate cancer. Long-term results are available and show outcomes equivalent to radical prostatectomy and beam irradiation.
With modern imaging techniques such as MRI with or without endorectal coil, multi-slice CT, choline-PET-CT a further improvement in staging will result in better patient selection and hence better outcome for all treatment modalities. But we should remember the phrase from Whitmore on patient selection: ‘Is prostate brachytherapy necessary for those who want it and is prostate brachytherapy possible for those who need it’.
Prostate brachytherapy appears to be the treatment of choice for low and intermediate cancers and can be used in combined therapy as a boost with or without androgen deprivation for patients with less favourable criteria. Whether HDR monotherapy will be used routinely for early-stage lesions is not clear but has a major advantage in the costs of treatments due to the high price of iodine seeds in Europe. Also, the radiobiology with low α/β ratio for prostate cancer could be in favour of HDR.
Urologists are considering using focal therapy in selected patients. In place of cryosurgery and HIFU, prostate brachytherapy with seeds or HDR can be a more appropriate technique in these cases. However, Isban published up to 60% multifocal tumour apart from the diagnosed unilateral tumour in biopsies (Isban et al. 2010).
Finally, we have to keep in mind that more men after permanent prostate brachytherapy will not die of their cancer but of other causes (Bittner et al. 2008).
References
Ash D, Flynn A, Battermann JJ et al (2000) ESTRO/EAU/EORTC recommendations on permanent seed implantation for localised prostate cancer. Radiother Oncol 57:315–321
Ash D, Al-Qaisieh B, Bottomley D et al (2006) The correlation between D90 and outcome for I-125 seed implant monotherapy for localised prostate cancer. Radiother Oncol 79:185–189
Battermann JJ, Boon TA, Moerland RA (2004) Results of permanent prostate brachytherapy, 13 years of experience at a single institution. Radiother Oncol 71:23–28
Beyer DC, Brachman DG (2000) Failure free survival following brachytherapy alone for prostate cancer: comparison with external beam radiotherapy. Radiother Oncol 57:263–267
Beyer DC (2004) Salvage brachytherapy after external-beam irradiation for prostate cancer. Oncology 18:151–158
Bianco FJ Jr, Scardino PT, Stephenson AJ et al (2005) Long-term oncologic results of salvage radical prostatectomy for locally recurrent prostate cancer after radiation therapy. Int J Radiat Oncol Biol Phys 62:448–453
Bittner N, Merrick GS, Galbreath R et al (2008) Primary causes of death after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 72:433–440
Blasko JC, Radge H, Schumacher D (1987) Transperineal percutaneous iodine-125 implantation for prostatic carcinoma using transrectal ultrasound and template guidance. Endocurie/Hypertherm Oncol 3:131–139
Blasko JC, Grimm PD, Sylvester JE et al (2000) The role of external beam radiotherapy with I-125/Pd-103 brachytherapy for prostate carcinoma. Radiother Oncol 57:273–278
Blasko JC, Mate T, Sylvester JE et al (2002) Brachytherapy for carcinoma of the prostate: techniques, patient selection, and clinical outcomes. Semin Radiat Oncol 12:81–94
Burri RJ, Ho AY, Forsythe K et al (2010a) Young men have equivalent biochemical outcomes compared with older men after treatment with brachytherapy for prostate cancer. Int J Radiat Oncol Biol Phys 77:1315–1321
Burri RJ, Stone NN, Unger P et al (2010b) Long-term outcome and toxicity of salvage brachytherapy for local failure after initial radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 77:1338–1344
Charyulu KKN (1980) Transperineal interstitial implantation of prostate cancer. A new method. Int J Radiat Oncol Biol Phys 6:1261–1266
Colberg JW, Decker RH, Khan AM et al (2007) Surgery versus implant for early prostate cancer: results from a single institution, 1992–2005. Cancer J 13:229–232
Cosset JM, Pinillos-Ashton L, Mettler F (2004) The recommendations of the International Commission on Radiological Protection (ICRP) for high-dose-rate brachytherapy and for permanent prostatic implants. Cancer 8(Suppl 1):S50–S55
Cosset JM, Flam T, Thiounn N et al (2008) Selecting patients for exclusive permanent prostate brachytherapy: the experience of the Paris Insitut Curie/Cochin hospital/Necker hospital group on 809 patients. Int J Radiat Oncol Biol Phys 71:1042–1048
Critz FA, Levinson K (2004) 10-year disease-free survival rates after simultaneous irradiation for prostate cancer with a focus on calculation methodology. J Urol 172:2232–2238
Crook J, McLean M, Catton C et al (2002) Factors influencing risk of acute urinary retention after TRUS guided permanent prostate seed implantation. Int J Radiat Oncol Biol Phys 52:453–460
Crook J, Gillan C, Yeung I et al (2007) PSA kinetics and PSA bounce following permanent seed prostate brachytherapy. Int J Radiat Oncol Biol Phys 69:426–433
Crook J, Gomez-Iturriaga A, Wallace K et al (2011) Comparison of health-related quality of life 5 years after SPIRIT: surgical prostatectomy versus interstitial radiation intervention trial. J Clin Oncol 29:362–368
Datolli M, Walner K, True L et al (2007) Long-term outcomes after treatment with brachytherapy and supplemental conformal radiation for prostate cancer patients having intermediate and high-risk features. Cancer 110:551–555
Flocks RH, Kerr HD, Elkins HB et al (1954) Treatment of carcinoma of the prostate by interstitial radiation with radioactive gold (Au-198): a follow-up report. J Urol 71:628–633
Fuks Z, Leibel SA, Wallner KE et al (1991) The effect of local control on metastatic dissemination in carcinoma of the prostate: long term results in patients treated with I-125 implantation. Int J Radiat Oncol Biol Phys 21:537–547
Futterer JJ, Heijmink SW, Scheenen TW et al (2006) Prostate cancer localization with dynamic contrast-enhanced MR imaging and proton MR spectroscopic imaging. Radiology 241:449–458
Galalae RM, Kovacs G, Schultze J et al (2002) Long-term outcome after elective irradiation of the pelvic lymphatics and local dose escalation using high dose rate brachytherapy for locally advanced prostate cancer. Int J Radiat Oncol Biol Phys 52:81–90
Grimm PD, Blasko JC, Sylvester JE et al (2001) 10-Year biochemical (prostate-specific antigen) control of prostate cancer with I125 brachytherapy. Int J Radiat Oncol Biol Phys 51:31–40
Henry AM, Al-Qaisieh B, Gould K et al (2010) Outcomes following iodine-125 monotherapy for localized prostate cancer: the results of Leeds 10-year single-center brachytherapy experience. Int J Radiat Oncol Biol Phys 76:50–56
Hinnen KA, Battermann JJ, van Roermond JGH et al (2010a) Long term biochemical and survival outcome of 921 patients treated with I-125 permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 76:1433–1438
Hinnen KA, Moerland MA, Battermann JJ et al (2010b) Loose seeds versus stranded seeds in I-125 prostate brachytherapy: differences in clinical outcome. Radiother Oncol 96:30–33
Hinnen KA, Roeloffzen EMA, Battermann JJ et al (2011a) Survival after prostate brachytherapy in patients aged 60 years and younger. BJU 107:1906–1911
Hinnen KA, Monninkhof EM, Battermann JJ et al (2011b) Prostate specific antigen bounce is related to overall survival in prostate brachytherapy. Int J Radiat Oncol Biol Phys 82:883–888
Hinnen KA, Schaapveld M, van Vulpen M et al (2011c) Prostate brachytherapy and second primary cancer risk: a competitive risk analysis. J Clin Oncol 29:4510–4515
Holm HH, Juul N, Pedersen JF et al (1983) Transperineal 125iodine seed implantation in prostatic cancer guided by transrectal ultrasonography. J Urol 130:283–286
Isban I, Karakiewitcz PI, Vogel S et al (2010) Unilateral prostate cancer cannot be accurately predicted in low-risk patients. Int J Radiat Oncol Biol Phys 77:784–787
Jabbari S, Weinberg VK, Shinohara K et al (2010) Equivalent biochemical control and improved prostate-specific antigen nadir after permanent prostate seed implant brachytherapy versus high-dose three-dimensional conformal radiotherapy and high-dose conformal proton beam radiotherapy boost. Int J Radiat Oncol Biol Phys 76:36–42
Kao J, Stone NN, Lavaf A et al (2008) 125I monotherapy using D90 implant doses of 180 Gy or greater. Int J Radiat Oncol Biol Phys 70:96–101
Keyes M, Miller S, Moravan V et al (2009a) Predictive factors for acute and late urinary toxicity after permanent prostate brachytherapy: long-term outcome in 712 consecutive patients. Int J Radiat Oncol Biol Phys 73:1023–1032
Keyes M, Miller S, Moravan V et al (2009b) Urinary symptom flare in 712 125I prostate brachytherapy patients: long term follow-up. Int J Radiat Oncol Biol Phys 75:649–655
Kirilova A, Damyanovich A, Crook J et al (2011) 3D MR-spectroscopic imaging assessment of metabolic activity in the prostate during the PSA “bounce” following 125Iodine brachytherapy. Int J Radiat Oncol Biol Phys 79:371–378
Kumar PP, Bartone FF (1981) Transperineal percutaneous I-125 implant of prostate. Urology 17:238–240
Kupelian PA, Potters L, Khuntia D et al (2004) Radical prostatectomy, external beam radiotherapy <72 Gy, external beam radiotherapy ≥72 Gy, permanent seed implantation, or combined seeds/external beam radiotherapy for stage T1-T2 prostate cancer. Int J Radiat Oncol Biol Phys 58:25–33
Lee WR (2002) The role of androgen deprivation therapy combined with prostate brachytherapy. Urology 37:565–569
Lee HK, Adams MT, Motta J (2008) Salvage prostate brachytherapy for localized prostate cancer failure after external beam radiation therapy. Brachytherapy 7:17–21
Liauw SL, Sylvester JE, Morris CG et al (2006) Second malignancies after prostate brachytherapy: incidence of bladder and colorectal cancers in patients with 15 years of potential follow-up. Int J Radiat Oncol Biol Phys 66:669–673
Malcolm JB, Fabrizio MD, Barone BB et al (2010) Quality of life after open or robotic prostatectomy, cryoablation or brachytherapy for localized prostate cancer. J Urol 183:1822–1829
Martens C, Pond G, Webster D et al (2006) Relationship of international prostate symptom score with urinary flow studies, and catherization rates following 125I prostate brachytherapy. Brachytherapy 5:9–13
Martin AG, Roy J, Beaulieu L et al (2007) Permanent prostate implant using high activity seeds and inverse planning with fast simulated annealing algorithm: a 12-year Canadian experience. Int J Radiat Oncol Biol Phys 67:334–341
Martinez A, Demanes J, Vargas C et al (2010) High-dose-rate prostate brachytherapy. An excellent accelerated-hypofractionated treatment for favourable prostate cancer. Am J Clin Oncol 33:481–488
McElveen TL, Waterman FM, Hayeon K et al (2004) Dicker AP factors predicting for urinary incontinence after prostate brachytherapy. Int J Radiat Oncol Biol Phys 57:1395–1404
Merrick GS, Butler WM, Wallace KE et al (2005a) Impact of supplemental external beam radiotherapy and/or androgen deprivation therapy on biochemical outcome after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 61:32–43
Merrick GS, Butler WM, Wallner KE et al (2005b) Erectile function after prostate brachytherapy. Int J Radiat Oncol Biol Phys 62:437–447
Merrick GS, Wallner KE, Butler WM et al (2006) Brachytherapy in men aged < or = 54 years with clinically localized prostate cancer. BJU Int 98:324–328
Merrick GS, Galbreath RW, Butler WM et al (2007) Primary Gleason pattern does not impact survival after permanent interstitial brachytherapy for Gleason score 7 prostate cancer. Cancer 110:289–296
Merrick GS, Wallner KE, Galbreath RW et al (2008) Prostate brachytherapy in men ≥75 years of age. Int J Radiat Oncol Biol Phys 72:415–420
Michalski J, Mutic S, Eichling J et al (2003) Radiation exposure to family and household members after prostate brachytherapy. Int J Radiat Oncol Biol Phys 56:764–768
Moerland MA, van Deursen MJ, Elias SG et al (2009) Decline of dose coverage between intraoperative planning and post implant dosimetry for I-125 permanent prostate brachytherapy: comparison between loose seeds and stranded implants. Radiother Oncol 91:202–206
Moman MR, Poel van der, Battermann JJ et al (2009) Treatment outcome and toxicity after salvage 125-I implantation for prostate cancer recurrences after primary 125-I implantation and external beam irradiation
Moman MR, van den Berg CAT, Boeken Kruger AE et al (2010) Focal salvage guided by T2-weighted and dynamic contrast-enhanced magnetic resonance imaging for prostate cancer recurrences. Int J Radiat Oncol Biol Phys 76:741–746
Moon K, Stukenborg G, Keim J et al (2006) Cancer incidence after localized therapy for prostate cancer. Cancer 107:991–998
Morris WJ, Keyes M, Palma D et al (2009) Evaluation of dosimetric parameters and disease response after 125Iodine transperineal brachytherapy for low- and intermediate-risk prostate cancer. Int J Radiat Oncol Biol Phys 73:1432–1438
Munro NP, Al-Qaisieh B, Bownes P et al (2010) Outcomes from Gleason 7, intermediate risk, localized prostate cancer treated with iodine-125 monotherapy over 10 years. Radiother Oncol 96:34–37
Nag S, Beyer D, Friedland J et al (1999) American Brachytherapy Society (ABS) recommendations for transperineal permanent brachytherapy of prostate cancer. Int J Radiat Oncol Biol Phys 44:789–799
Nag S, Bice W, DeWyngaert K et al (2000) The American Brachytherapy Society recommendations for permanent prostate brachytherapy postimplant dosimetric analysis. Int J Radiat Oncol Biol Phys 46:221–230
Nguyen PL, Chen MH, D’Amico AV et al (2007) Magnetic resonance image-guided salvage brachytherapy after radiation in select men who initially presented with favourable-risk prostate cancer. Cancer 110:1485–1492
Pasteau O, Degrais D (1914) The radium treatment of cancer of the prostate. Arch Roentgen Ray 28:396–410
Pickels T, Keyes M, Morris WJ (2010) Brachytherapy or conformal external radiotherapy for prostate cancer: a single institution matched-pair analysis. Int J Radiat Oncol Biol Phys 76:43–49
Piña AG-I, Crook J, Borg J et al (2010) Biochemical disease-free rate and toxicity for men treated with iodine-125 prostate brachytherapy with D90 ≥ 180 Gy. Int J Radiat Oncol Biol Phys 78:422–427
Potters L, Morgenstern C, Calugaru E et al (2005) 12-year outcomes following permanent prostate brachytherapy in patients with clinically localized prostate cancer. J Urol 173:1562–1566
Reed DR, Wallner KE, Merrick GS et al (2007) A prospective randomized comparison of stranded vs. loose seeds for prostate brachytherapy. Brachytherapy 6:129–134
Robinson JW, Moritz S, Fung T (2002) Meta-analysis of rates of erectile function after treatment of localized prostate carcinoma. Int J Radiat Oncol Biol Phys 54:1063–1068
Roeleveld TA, Horenblas S, Moonen LMF et al (1996) Inwendige radiotherapie bij prostaatcarcinoom; tegenvallende lange termijn resultaten van retropubische jodium-125 implantatie. Ned Tijdschr Geneeskd 140:1855–1859
Roeloffzen EMA, Lips IM, van Gellekom MPR et al (2010) Health-related quality of life up to six years after I-125 brachytherapy for early-stage prostate cancer. Int J Radiat Oncol Biol Phys 76:1054–1060
Saibishkumar EP, Borg J, Yeung I et al (2009) Sequential comparison of seed loss and prostate dosimetry of stranded seeds with loose seeds in 125I permanent implant for low-risk prostate cancer. Int J Radiat Oncol Biol Phys 73:61–68
Salembier C, Lavagnini P, Nickers P et al (2007) Tumour and target volumes in permanent prostate brachytherapy: a supplement to the ESTRO/EAU/EORTC recommendations on prostate brachytherapy. Radiother Oncol 83:3–10
Schwartz DJ, Sengupta S, Hillman DW et al (2007) Prediction of radial distance of extraprostatic extension from pretherapy factors. Int J Radiat Oncol Biol Phys 69:411–418
Shapiro EY, Rais-Bahrami S, Morgenstern C et al (2009) Long-term outcomes in younger men following permanent prostate brachytherapy. J Urol 181:1665–1671
Sharkey J, Canto A, Solc Z et al (2005) Pd103 brachytherapy versus radical prostatectomy in patients with clinically localized prostate cancer: a 12-year experience from a single group practice. Brachytherapy 4:33–44
Singh AK, Mashtare TL, McCloskey SA et al (2010) Increasing age and treatment modality are predictors for subsequent diagnosis of bladder cancer following prostate cancer diagnosis. Int J Radiat Oncol Biol Phys 78:1086–1094
Stephenson AJ, Scardino PT, Bianco FJ Jr et al (2004) Morbidity and functional outcomes of salvage radical prostatectomy for locally recurrent prostate cancer after radiation therapy. J Urol 172:2239–2243
Stock RG, Stone NN, Lo YC et al (1998) Postimplant dosimetry for I-125 prostate implants. Int J Radiat Oncol Biol Phys 41:101–108
Stone NN, Stock RG (2002) Complications following permanent prostate brachytherapy. Eur Urol 41:427–433
Stone NN, Stock RG, Cesaretti JA et al (2010) Local control following permanent prostate brachytherapy: effect of high biologically effective dose on biopsy results and oncologic outcomes. Int J Radiat Oncol Biol Phys 76:355–360
Sylvester JE, Grimm PD, Blasko JC et al (2007) 15-year biochemical relapse free survival in clinical stage T1-T3 prostate cancer following combined external beam radiotherapy and brachytherapy; Seattle experience. Int J Radiat Oncol Biol Phys 67:57–64
Taira AV, Merrick GS, Butler WM et al (2011) Long-term outcome for clinically localized prostate cancer treated with permanent interstitial brachytherapy. Int J Radiat Oncol Biol Phys 79:1336–1342
Teh BS, Bastasch MD, Wheeler TM et al (2003) IMRT for prostate cancer: defining target volume based on correlated pathologic volume of disease. Int J Radiat Oncol Biol Phys 56:184–191
Terk MD, Stock RG, Stone NN (1998) Identification of patients at increased risk for prolonged urinary retention following radioactive seed implantation of the prostate. J Urol 106:1379–1382
Tward JD, Lee CM, Pappas LM et al (2006) Survival of men with clinically localized prostate cancer treated with prostatectomy, brachytherapy, or no definitive treatment: impact of age at diagnosis. Cancer 107:2392–2400
Villeirs GM, Verstraete KL, De Neve WJ et al (2005) Magnetic resonance imaging anatomy of the prostate and periprostatic area: a guide for radiotherapists. Radiother Oncol 76:99–106
Westendorp R, Nuver T, vd Molen A et al (2011) C-arm cone-beam CT and TRUS guided HDR-boost for prostate treatment. Radiother Oncol 99:S280
Whitmore WF Jr, Hilaris B, Grabstald H (1972) Retropubic implantation of iodine-125 in the treatment of prostatic cancer. J Urol 108:918–920
Wright JL, Salinas CA, Kolb DW et al (2009) Prostate cancer specific mortality and Gleason 7 disease differences in prostate cancer outcomes between cases with Gleason 4 + 3 and 3 + 4 tumors in a population based cohort. J Urol 182:2702–2707
Zelefsky MJ, Kuban DA, Levy LB et al (2007) Multi-institutional analysis of long-term outcome for stages T1-T2 prostate cancer treated with permanent seed implantation. Int J Radiat Oncol Biol Phys 67:327–333
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Battermann, J.J. (2012). Permanent Prostate Brachytherapy. In: Bolla, M., van Poppel, H. (eds) Management of Prostate Cancer. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-27597-5_10
Download citation
DOI: https://doi.org/10.1007/978-3-642-27597-5_10
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-27596-8
Online ISBN: 978-3-642-27597-5
eBook Packages: MedicineMedicine (R0)