Abstract
Despite the development of improved protective personal equipment, orthopedic injury patterns remained unchanged from World War I. Orthopedic trauma comprises the vast majority of war injuries, as 70% of casualties involve the musculoskeletal system and extremity injuries represent the most common type. Factors influencing the development of wound infections in a combat theater include wound type and severity, the presence of embedded foreign material, evacuation time from point of injury to medical care, initiation of antimicrobial agents, adequacy of initial wound debridement, immediate wound care, definitive surgical care, rehabilitative care, prior antimicrobial pressure, and the presence of nosocomial pathogens, especially multidrug resistant (MDR) pathogens at treatment facilities. With the possible exception of Acinetobacter baumannii–calcoaceticus complex (ABC), the bacteria infecting combat-related wounds in the past decade are similar to those described in wars of previous periods. The incidence of osteomyelitis in combat-related extremity injuries is between 2% and 15%. Early and aggressive management of extremity wounds starting with interventions near the battlefield have resulted in improved outcomes. The use of antibiotic prophylaxis in an attempt to diminish the rate of infective complications has been considered standard for the last 30 years. However, two major areas of controversies are the use of the best agent and the duration of prophylaxis. Despite its enormous contribution for the understanding and management of open fractures, the Gustilo and Anderson classification has also limitations and recent reviewed data support at least two important and practical conclusions: (1) a short course of first-generation cephalosporins, begun as soon as possible after injury, significantly lowers the risk of infection when used in combination with prompt, modern orthopedic fracture wound management; (2) there is insufficient evidence to support prolonged courses or repeated short courses of antibiotics, the use of antibiotic coverage to gram-negative bacilli or clostridial species, or the use of local antibiotic therapies such as beads. Guidelines recommend the early use of cefazolin or another intravenous first generation cephalosporin at Level I/IIa medical care in the combat zone for all extremity injuries (AII). At Level IV/V medical care, antibiotics should include those agents started earlier in the evacuation chain, but these should be stopped after 24–72 h if there is no evidence of infection upon evaluation of the wound. Level IV/V should be treating only infected wounds and using periprocedure antibiotics as part of routine care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
10.1 Background
As in several other medical fields, there have been remarkable improvements in the twentieth century in decreasing the mortality rate from combat wounds. For instance, existing data indicate a mortality rate of 8% among a total of 153,000 US soldiers wounded in World War I, while mortality rates in World War II and in the Vietnam War were 4.5% (total wounded 599,724) and 3.6% (total wounded 96,811), respectively [28]. Improvements included improved protective personal equipment, better training, the expertise of combat medics enabling life-saving care to be provided at the point of injury, and the rapid evacuation of casualties to surgical care provided in close proximity to the point of injury. These measures have enabled personnel to survive near-catastrophic injuries but, eventually, have placed them at the highest risk for developing wound infections. Sir William Osler, writing on the difficulties of casualty care in 1914, stated: “And here comes in the great tragedy – sepsis everywhere, unavoidable sepsis!… The surgeons are back in the pre-Listerian days and have wards filled with septic wounds. The wound of shrapnel and shell is a terrible affair, and infection is well nigh inevitable.” [38].
Ninety-five years later, his quote remains pertinent because combat-related injuries still carry a great risk of infection. War wounds are distinct from peacetime traumatic injuries because these higher velocity projectiles and/or blast devices cause more severe injury and accompanying wounds are frequently contaminated by clothing, soil, and environmental debris [2]. In addition, the pattern, number, and severity of injuries; presence of devitalized tissue, foreign bodies, clots, and fluid collections; time from injury to evacuation or antimicrobial therapy; and microbiologic contamination introduced during care in the medical system, all these constitute important conditions influencing the outcome of war wounds. Despite the development of improved protective personal equipment, orthopedic injury patterns remained unchanged. From World War I to operations in Somalia, approximately 65% of the total number of injuries suffered by casualties were orthopedic [57] with extremity injuries representing the most common type of injury sustained in combat (∼65%) [22].
10.2 The Nature of the Problem
Historically, surgeons and hospital epidemiologists have stratified operations into clean, clean–contaminated, and contaminated procedures on the basis of the expected quantity of bacteria introduced into the operative site during surgery. Although the magnitude of bacterial inoculation into the wound still has some predictive value regarding the risk of developing a wound infection, patient- and procedure-related risk factors also contribute greatly to this risk. Wounds caused by weapons are characterized by extensive tissue destruction, and often there is deep penetration of metal fragments, dirt, and debris into wounds that may not be detected at time of surgery. Therefore, traumatic wounds are classified as contaminated or dirty wounds. Anatomical variations in regional blood flow and skin flora also play a part in determining the likelihood of infection. Wounds on the highly vascularized face or scalp are less likely to be infected than wounds in less vascularized areas [21]. Combat-related injuries are caused by shear forces; however, compressive forces cause more devitalization of tissue and, therefore, crush wounds are more susceptible to infection [50]. Because of the nature of the injuries (wounds caused by improvised explosive devices, mortars, rocket-propelled grenades, and gunshots) and protective gear, extremity wounds are prevalent [1]. Patients typically suffer multiple injuries, involving on average 1.6 different body parts [59]. Explosive devices typically result in a greater number of injury sites and greater severity of injuries [34]. Factors influencing the development of wound infections in a combat theater include wound type and severity, the presence of embedded foreign material or fragments (such as soldier’s clothing, dirt, and debris), evacuation time from point of injury to medical care, initiation of antimicrobial agents, adequacy of initial wound debridement, immediate wound care, definitive surgical care, rehabilitative care, prior antimicrobial pressure, and the presence of nosocomial pathogens, especially multidrug resistant (MDR) pathogens at treatment facilities.
10.3 The Wound Microenvironment
The bacteriology combat-related wound has been a significant factor in determining antibiotic treatment guidelines. The epidemiology of these wounds has changed significantly since Alexander Fleming characterized bacteria-infecting wounds during World War I [15, 52]. This includes a shift from Clostridia species in World War I, to Streptococcus pyogenes and Staphylococcus aureus in World War II, to gram-negative bacilli (Pseudomonas aeruginosa, Enterobacter species, Escherichia coli, and Klebsiella species) since the Vietnam War [27, 29, 46, 54]. During the Korean conflict, it was noted that the bacteria responsible for infecting wounds varied with the seasons, with more staphylococci, streptococci, and Clostridium in winter months and fecal pathogens in summer months [35]. Seasonal variation in bacteria-infecting wounds was also noted during the Vietnam conflict [30]. It was observed that bacteria transitioned over time within a combat-related injury. Typically, an even representation of gram-positive bacteria such as Staphylococcus spp. and gram-negative bacteria such as Pseudomonas aeruginosa, Enterobacter aerogenes, Proteus spp., and E. coli existed at the time of injury but, over the course of therapy, resistant gram-negative bacteria were responsible for the majority of infections, especially further back in the evacuation chain [35]. During Operation Iraqi Freedom (OIF), samples from war wounds were obtained shortly after injury for aerobic culture [1]. Approximately one-half of the culture results were positive, with most cultures yielding gram-positive skin flora. Similar to the Vietnam War experience, gram-negative rods accounted for the majority of wound infections during OIF. Among 56 patients evacuated to US Navy hospital ship between March and May 2003, and meeting a criteria for infection (84% wound infections and 38% bloodstream infections), Acinetobacter species (36%) were the predominant organisms, followed by Escherichia coli and Pseudomonas species (14% each) [45].
One of the primary lessons learned during World War II was the role of nosocomial transmission of disease, with up to 86% of patients having hospital-associated infections [31, 33, 48]. Similar to previous wars, wound infections developed days after injury during OIF and were usually acquired in the hospital setting [1]. It was proposed that initial antimicrobial agents used at the time of injury were responsible for drug pressure leading to increasingly resistant bacteria. A study from the Yom Kippur War [26] reported that 80 of 88 episodes of wound infection (91%) diagnosed among 624 consecutively admitted battlefield casualties occurred during administration of antibiotic therapy.
10.4 Epidemiology of Combat-Related Wound Infections Caused by Multidrug-Resistant Organisms
With the possible exception of Acinetobacter baumannii–calcoaceticus complex (ABC), the bacteria-infecting combat-related wounds in the past decade are similar to those described in wars of previous periods [35]. The major change in the recent epidemiology of combat-related wound infections is the development of infections due to MDR bacteria, notably ABC, but also with extended spectrum beta-lactamase-producing bacteria such as Klebsiella pneumoniae, methicillin-resistant Staphylococcus aureus, and MDR Pseudomonas aeruginosa [1, 5, 10]. A. baumannii is a well-known cause of health-care-associated infections, particularly among intensive care unit patients. Because the organism has developed substantial antimicrobial resistance, treatment of infections attributed to A. baumannii has become increasingly difficult [55]. Since 2003, the incidence of MDR Acinetobacter infection in military treatment facilities has increased significantly [1, 10]. The majority of isolates are cultured from wound specimens; however, the increase in incidence has involved all culturable sites, including blood. Of 45 patients with A. baumannii bloodstream infections at Walter Reed Army Medical, 29 (64%) patients sustained traumatic injuries in the Iraq/Kuwait region. Of these, 18 (62%) had bloodstream infections detected from blood cultures obtained within 48 h of hospital admission after transfer from a combat theater medical or other military medical facility [5]. The majority of Acinetobacter isolates cultured from hospitalized, injured personnel have been MDR, unlike isolates cultured before the war. Although some of the patients identified in this report had evidence of bloodstream infections at the time of admission to military medical facilities, whether the infections were acquired from environmental sources in the field or during treatment at (or evacuation from) other military medical facilities (e.g., field hospitals) is unknown [5]. Nevertheless, it is unlikely that wounds are colonized at the time of injury with dirt and debris containing MDR gram-negative bacteria. Based on cumulative data, nosocomial transmission is likely propagating infections with these bacteria [35].
Whole-genome sequencing of a resistant, epidemic strain showed that A. baumannii was able to switch genomic structures, likely accounting for the rapid resistance mutation acquisition under antibiotic pressure [16]. The original source of A. baumannii is not clear; however, countries in the Middle East at the onset of OIF had MDR gram-negative bacteria, including ABC, complicating the care of patients in their intensive care units [24, 25, 47].
10.5 Combat-Related Extremity Injuries and Open Fractures
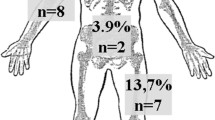
Open fractures, defined as those communicating with the outside environment through a skin wound, are a major source of morbidity after trauma. Orthopedic trauma comprises the vast majority of war injuries, as 70% of casualties involve the musculoskeletal system; 26% are fractures and 82% of the fractures are open [8, 9, 39, 40]. There is a relatively even distribution between the upper and lower extremities, with hand trauma representing 36% of upper extremity injuries and tibia and fibula injuries constituting 48% of lower extremity injuries [9]. Thus, it is not surprising that the incidence of osteomyelitis in combat-related extremity injuries is from 2% to 15% [5, 37, 58]. Prior to World War I, the mortality rate associated with open fractures ranged from 80% to 90% [20]. However, modern trauma systems have led to greater early survival rates, and chronic osteomyelitis, nonunion, loss of function, or even limb loss represent the most important long-term morbidity of open fractures. High-energy, high-grade open fractures of the lower extremities, especially of the tibia, are considered to be at especially high risk of infection [11, 12, 19, 44]. These wounds often harbor bone fragments or soft tissues with a marginal blood supply and may have soft-tissue envelopes that are inadequate to cover the bone. Such injuries constitute a culture medium with an almost permanent exposure to the bacterial hospital flora. Moreover, antibiotics poorly penetrate devascularized tissues, which are also an unfavorable environment for phagocytes’ action. In a recent retrospective cohort study of 110 cases of osteomyelitis among casualties of the OIF and Enduring Freedom, infection involving the lower extremities was more than twice as frequent as osteomyelitis of the upper limbs in both the initial and recurrent episodes [58].
Studies of antibiotic use in open fractures became more standardized following the important study by Gustilo and Anderson [18], which revised the grading of open fractures, especially among “Grade III” fractures with extensive soft-tissue damage (Table 10.1). That and later studies showed that fracture grade and the degree of associated soft-tissue damage are independent determinants of infection risk [12, 19]. Despite its enormous contribution to the understanding and management of open fractures, the Gustilo–Anderson classification has limitations recently summarized by Hauser et al. [20]. Fracture grades can be modified on the basis of operative findings, and the classification is subjective and suffers from a high degree of interobserver variability [53]. Also, retrospective discrimination between Grades IIIb and IIIc fractures was clearly arbitrary. Successful vascular reconstructions appear to have converted Grade IIIc to functional IIIb fractures, while a failure of revascularization led to primary amputations and elimination from the study group. Thus, the rates of infection found by Gustilo et al. in their original studies were nearly identical for Grade IIIb and IIIc fractures [19]. Moreover, although Grade IIIc fractures were defined as those requiring vascular reconstruction, many Grade IIIb fractures distal to the knee clearly harbored vascular injuries. Lastly, both ischemia/reperfusion injuries and compartment syndromes are frequent after vascular repairs and may contribute to secondary vascular insufficiency at the fracture wound. Thus, vascular repairs are inaccurate surrogates for wound ischemia. These considerations mandate that analyzes of antibiotic use in high-grade (Gustilo IIIb–IIIc) fractures be approached with the greatest care. Inadequate revascularization of Grade IIIc fractures will lead to infection and limb loss [49], but no study has looked at the success of revascularization per se as a predictor of the success of fracture wound prophylaxis. Nonetheless, some sort of grading system must be used if antibiotic prophylaxis study groups are to be compared in an interpretable fashion. The relative increase in infection between Gustilo Grades IIIa and IIIb fractures was initially estimated at 10- to 15-fold [19]. Later studies reported infection rates ranging from 0% to 9% for Grade I fractures, from 1% to 12% for Grade II fractures, and from 9% to 55% for Grade III fractures [3, 6, 7, 11, 18, 19, 43, 44].
Paralleling the increasing risk of infection is the rising hazard of gram-negative infections in patients with severe soft-tissue injuries and prolonged intervals to wound closure [3, 11, 12, 18, 44].
10.6 Prevention of Infections Associated with Combat-Related Extremity Injuries
Early and aggressive management of extremity wounds, starting with interventions near the battlefield, have resulted in improved outcomes [37]. The major objectives of the management of extremity injuries, whether in the civilian community or in the military setting, are to prevent infection, promote fracture healing, and restore function. Current methods to prevent infections in these types of injuries are derived primarily from controlled trials of elective surgery and civilian trauma as well as retrospective studies of civilian and military trauma interventions. Recently, a committee consisting of military and civilian experts in infectious disease, trauma, preventive medicine, infection control, critical care, and several surgical specialties including general and orthopedic surgery reviewed the relevant civilian and military trauma literature to draft recommendations for the treatment of casualties based on the available evidence. The committee experts were asked to develop recommendations for the reduction or prevention of infections in combat-related injuries. The conference was sponsored by the United States Army Office of the Surgeon General and hosted by the United States Army Institute of Surgical Research at Fort Sam Houston, Texas, on June 11–12, 2007. An attempt was made to assign a level to denote both the strength of recommendations and quality of evidence available to support those recommendations. The Infectious Diseases Society of America/US Public Health Service rating system was utilized (Table 10.2). Limitations in using a rating system in the guidelines included the fact that randomized, controlled trials have not been performed in combat zones and that generalizing civilian trauma care data to combat trauma care may not be valid because of the differences in mechanisms of injury, time to access, diagnostic capabilities at initial receiving facilities, the austere nature of many of those facilities, and access to and type of medical care systems. The guidelines were eventually published [22] and they integrate the most recent available evidence and expert opinion, from within and outside the US military medical community, to provide guidance to US military health-care providers in the diagnosis, treatment, and prevention of infections in those individuals wounded in combat. Table 10.3 summarizes the major recommended clinical practice guidelines for the prevention of infection after combat-related extremity injuries.
10.7 The Use of Antibiotics in the Management of Combat-Related Extremity Injuries
Antibiotics were introduced toward the end of World War II, when open fractures were treated on the battlefield with topical sulfonamides and definitive care was given at forward medical facilities. Reliance on antibiotics proved unsuccessful in open fractures that were closed primarily, while delayed closure of open fractures was successful in nearly all cases despite bacterial wound contamination [14]. Nevertheless, the use of antibiotic prophylaxis in an attempt to diminish the rate of infective complications, particularly after open fractures, has been considered standard for the last 30 years. Since there have been no randomized, controlled trials on the use of antibiotics in combat-related injuries, many recommendations are based on a number of expert opinion publications. Two major areas of controversies are the use of the best agent and the duration of prophylaxis. The role of antibiotics at the time of injury on the battlefield is also debatable. For instance, the British military uses relatively narrow-spectrum agents, typically penicillin with a beta-lactamase agent, similar to agents recommended by the International Committee of the Red Cross at the time of initial surgical evaluation [13], while the US military, at least for those unable to receive surgical care in a rapid manner, has proposed broader spectrum agents [4, 36]. Given the concern of antimicrobial resistance with broad-spectrum therapy, narrow-spectrum antibiotic therapy might be of greater long-term benefit, but this remains to be answered.
The use of antibiotics in the management of open fractures in the civilian community has been extensively analyzed. A Cochrane review published in 2004 revealed that antibiotics had a protective effect against early infection compared with no antibiotics (relative risk 0.41; 95% confidence interval [CI], 0.27–0.63; absolute risk reduction of 0.08; 95% CI, 0.04–0.12 and number needed to treat 13; 95% CI, 8–25) [17]. This effect was solely because of the high activity of β-lactams against streptococci and staphylococci. Prolonged courses of broad-spectrum antibiotics are often cited as the standard of care for prevention of infective complications of open fractures. The origins of these recommendations are obscure, but probably relate to the seminal study of Patzakis et al. from 1974 [42]. This randomized, placebo-controlled study was the first to examine infection rates in open fractures as a specific function of antibiotic use and included 310 patients over a two-year period, most with tibial fractures. Fractures with associated vascular injuries were excluded and all wounds were closed primarily, an atypical surgical method by modern standards. The groups appeared to be comparable in their surgical management. Patients were randomized into three groups to receive no antibiotics, penicillin and streptomycin, or cephalothin. All patients were treated for 10–14 days, a regimen that currently would be regarded as therapeutic rather than prophylactic. The study groups had infection rates of 13.9%, 9.7%, and 2.3%, respectively, a difference that was significant only between the cephalothin and placebo groups. These data provided strong evidence of the efficacy of first-generation cephalosporins in managing open long-bone fractures. In the same article, however, Patzakis et al. retrospectively reviewed the bacteriology of the fractures that became infected [42]. In the placebo group, the infecting organisms included gram-positive, gram-negative, and, rarely, clostridial species. The penicillin/streptomycin-treated group developed infections with Staphylococcus aureus and Enterobacteriaceae, including Pseudomonas, while infections in the group that received cephalothin typically yielded gram-negative species. These ancillary findings led the authors to suggest that combining streptomycin with a cephalosporin would reduce infection rates further, but that hypothesis was not tested. In a posterior study in 2000, Patzakis et al. compared single-agent ciprofloxacin prophylaxis with the combination of cefamandole and gentamicin in a randomized, double-blind study in 163 patients with open fractures well stratified as to grade [41]. The groups appeared equivalent. The overall infection rates in this study were high, which probably is related to delays in management because patients were only started on antibiotics within “12 h postinjury” (reported mean time from injury to surgery was 24 h). Ciprofloxacin monotherapy had higher failure rates in comparison to cephalosporin in combination with an aminoglycoside for type III fractures (8 of 26 cases vs. 2 of 26 cases, respectively), but this difference was not statistically significant.
The optimal duration of antibiotics is also not clear. There is a major misconception among many surgeons about the need for prolonged antibiotic prophylaxis. Prospective studies have revealed therapy as short as one day may be as effective as the traditionally recommended 5 days of therapy [11, 32, 51]. There are data suggesting that prolonged courses of antibiotics are complicated by systemic infections due to resistant organisms [23, 56]. A recent systematic review of the literature on the effects of prophylactic antibiotic administration on the incidence of infections complicating open fractures was performed by the Surgical Infection Society [20]. The data reviewed by that group supported several important and practical conclusions: (1) a short course of first-generation cephalosporins begun as soon as possible after injury significantly lowers the risk of infection when used in combination with prompt, modern orthopedic fracture wound management; (2) there is insufficient evidence to support other common management practices, such as prolonged courses or repeated short courses of antibiotics, the use of antibiotic coverage extending to gram-negative bacilli or clostridial species, or the use of local antibiotic therapies such as beads; (3) large, randomized, blinded trials are needed to prove or disprove the value of these traditional approaches.
The recently published guidelines for the prevention of infection after combat-related injuries reached practically the same conclusions [22, 37]. Accordingly, these guidelines recommend the early use of cefazolin or another intravenous first-generation cephalosporin at Level I/IIa medical care in the combat zone for all extremity injuries (AII) (Table 10.3), although substitutions should be considered if other injuries, including central nervous system or abdominal/thoracic injury, necessitate alternative agents with enhanced gram-negative and anaerobic activity. Enhanced gram-negative therapy even for type III fractures is discouraged (DII) (Table 10.3). At Level IV/V medical care, antibiotics should include those agents started earlier in the evacuation chain but these should be stopped after 24–72 h if there is no evidence of infection upon evaluation of the wound. Overall, Level I/IIa/IIb/III should emphasize wound preemptive therapy, while Level IV/V should be treating only infected wounds and using periprocedure antibiotics as part of routine care. There is also no evidence to support continuing antibiotics during evacuation or continuing antibiotics until the wound is covered or until all drains are removed.
References
Aronson, N.E., Sanders, J.W., Moran, K.A.: In harm’s way: infections in deployed American military forces. Clin. Infect. Dis. 43, 1498 (2006)
Bellamy, R., Zajtchuk, R.: The management of ballistic wounds of soft tissue. In: Bellamy, R.F., Zajtchuk, R. (eds.) Textbook of Military Medicine: Conventional Warfare – Ballistic, Blast and Burn Injuries, Part 1, vol. 3, pp. 163–220. U.S. Government Printing Office, Washington, DC (1991)
Braun, R., Enzler, M.A., Rittmann, W.W.: A double-blind clinical trial of prophylactic cloxacillin in open fractures. J. Orthop. Trauma 1, 12–17 (1987)
Butler, F., O’Connor, K.: Antibiotics in tactical combat casualty care 2002. Mil. Med. 168, 911–914 (2003)
Centers for Disease Control and Prevention: Acinetobacter baumannii infections among Centers for Disease Control and Prevention. Acinetobacter baumannii infections among patients at military medical facilities treating injured U.S. service members, 2002–2004. MMWR Morb. Mortal Wkly. Rep. 53, 1063–1066 (2004)
Chapman, M.W., Mahoney, M.: The role of early internal fixation in the management of open fractures. Clin. Orthop. 138, 120–131 (1979)
Clancey, G.J., Hansen Jr., S.T.: Open fractures of the tibia: a review of one hundred and two cases. J. Bone Joint Surg. Am. 60, 118–122 (1978)
Covey, D.C.: Combat orthopaedics: a view from the trenches. J. Am. Acad. Orthop. Surg. 14(Suppl), S10–S17 (2006)
Covey, D.C., Aaron, R.K., Born, C.T., et al.: Orthopaedic war injuries: from combat casualty care to definitive treatment: a current review of clinical advances, basic science, and research opportunities. Instr. Course Lect. 57, 65–86 (2008)
Davis, K.A., Moran, K.A., McAllister, C.K., et al.: Multidrug-resistant Acinetobacter extremity infections in soldiers. Emerg. Infect. Dis. 11, 1218–1224 (2005)
Dellinger, E.P., Caplan, E.S., Weaver, L.D., et al.: Duration of preventive antibiotic administration for open extremity fractures. Arch. Surg. 123, 333–339 (1988)
Dellinger, E.P., Miller, S.D., Wertz, M.J., et al.: Risk of infection after open fracture of the arm or leg. Arch. Surg. 123, 1320–1327 (1988)
Dufour, D., Jensen, S.K., Owen-Smith, M., et al.: Surgery for Victims of War, 3rd edn. International Committee of the Red Cross, Geneva (1998)
Epps, C.H.J., Adams, J.P.: Wound management in open fractures. Am. Surg. 27, 766–769 (1961)
Fleming, A.: On the bacteriology of septic wounds. Lancet 2, 638–643 (1915)
Fournier, P., Vallenet, D., Barbe, V., et al.: Comparative genomics of multidrug resistance in Acinetobacter baumannii. PLoS Genet. 2, e7 (2006)
Gosselin, R.A., Roberts, I., Gillespie, W.J.: Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst. Rev. 1:CD003764 (2004)
Gustilo, R.B., Anderson, J.T.: Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J. Bone Joint Surg. Am. 58, 453–458 (1976)
Gustilo, R.B., Mendoza, R.M., Williams, D.N.: Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J. Trauma 24, 742–746 (1984)
Hauser, C.J., Adams Jr., C.A., Eachempati, S.R.: Prophylactic antibiotic use in open fractures: an evidence-based guideline. Surg. Infect. 7, 379–405 (2006)
Hollander, J.E., Singer, A.J., Valentine, S., Henry, M.C.: Wound registry: development and validation. Ann. Emerg. Med. 25, 675–686 (1995) [Erratum, 26:532]
Hospenthal, D.R., Murray, C.K., Andersen, R.C., et al.: Guidelines for the prevention of infection after combat-related injuries. J. Trauma 64, S211–S220 (2008)
Hoth, J.J., Franklin, G.A., Stassen, N.A., et al.: Prophylactic antibiotics adversely affect nosocomial pneumonia in trauma patients. J. Trauma 55, 249–254 (2003)
Jerassy, Z., Yinnon, A.M., Mazouz-Cohen, S., et al.: Prospective hospital-wide studies of 505 patients with nosocomial bacteraemia in 1997 and 2002. J. Hosp. Infect. 62, 230–236 (2006)
Kanafani, Z.A., Kara, L., Hayek, S., et al.: Ventilator-associated pneumonia at a tertiary-care center in a developing country: Incidence, microbiology, and susceptibility patterns of isolated microorganisms. Infect. Control Hosp. Epidemiol. 24, 864–869 (2003)
Klein, R.S., Berger, S.A., Yekutiel, P.: Wound infection during the Yom Kippur War: observations concerning antibiotic prophylaxis and therapy. Ann. Surg. 182, 15–21 (1975)
Lindberg, R., Wetzler, B., Marshall, J., et al.: The bacterial flora of battle wounds at the time of primary debridement. Ann. Surg. 141, 369–374 (1955)
Mabry, R.L., Holcomb, J.B., Baker, A.M., et al.: United States Army Rangers in Somalia: an analysis of combat casualties on an urban battlefield. J. Trauma 49, 515–529 (2009)
MacLennan, J.: Anaerobic infection of war wounds in the middle east. Lancet 2, 63–66 (1943)
Matsumoto, T., Wyte, S.R., Moseley, R.V., et al.: Combat surgery in communication zone. I. War wound and bacteriology (preliminary report). Mil. Med. 134, 655–665 (1969)
McKissock, W., Wright, J., Miles, A.A.: The reduction of hospital infection of wounds. A controlled experiment. BMJ 2, 375–377 (1941)
Merritt, K.: Factors increasing the risk of infection in patients with open fractures. J. Trauma 28, 823–827 (1988)
Miles, A.A., Schwabacher, H., Cunliffe, A.C.: Hospital infection of war wounds. BMJ 2, 855–900 (1940)
Murray, C.K.: Epidemiology of infections associated with combat-related injuries in Iraq and Afghanistan. J. Trauma 64, S232–S238 (2008)
Murray, C.K.: Infectious disease complications of combat-related injuries. Crit. Care Med. 36, S358–S364 (2008)
Murray, C.K., Hospenthal, D.R., Holcomb, J.B.: Antibiotics use and selection at the point of injury in tactical combat casualty care for casualties with penetrating abdominal injury, shock, or unable to tolerate an oral agent. J. Spec. Oper. Med. 5, 56–61 (2005)
Murray, C.K., Hsu, J.R., Solomkin, J.S., et al.: Prevention and management of infections associated with combat-related extremity injuries. J. Trauma 64, S239–S251 (2008)
Osler, W.: Medical notes on England at war. J. Am. Med. Assoc. 63, 2303–2305 (1914)
Owens, B.D., Kragh Jr., J.F., Macaitis, J., et al.: Characterization of extremity wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J. Orthop. Trauma 21, 254–257 (2007)
Owens, B.D., Kragh Jr., J.F., Wenke, J.C., et al.: Combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J. Trauma 64, 295–299 (2008)
Patzakis, M.J., Bains, R.S., Lee, J., et al.: Prospective, randomized, double-blind study comparing single agent antibiotic therapy, ciprofloxacin, to combination antibiotic therapy in open fracture wounds. J. Orthop. Trauma 14, 529–533 (2000)
Patzakis, M.J., Harvey Jr., J.P., Ivler, D.: The role of antibiotics in the management of open fractures. J. Bone Joint Surg. Am. 56, 532–541 (1974)
Patzakis, M.J., Wilkins, J.: Factors influencing infection rate in open fracture wounds. Clin. Orthop. 243, 36–40 (1989)
Patzakis, M.J., Wilkins, J., Moore, T.M.: Considerations in reducing the infection rate in open tibial fractures. Clin. Orthop. 178, 36–41 (1983)
Petersen, K., Riddle, M.S., Danko, J.R., et al.: Trauma-related infections in battlefield casualties from Iraq. Ann. Surg. 245, 803–811 (2007)
Pettit, R.: Infections of wounds of war. J. Am. Med. Assoc. 73, 494 (1919)
Rotimi, V.O., al Sweih, N.A., Feteih, J.: The prevalence and antibiotic susceptibility pattern of gram-negative bacterial isolates in two ICUs in Saudi Arabia and Kuwait. Diagn. Microbiol. Infect. Dis. 30, 53–59 (1998)
Roy, T.E., Hamilton, J.D., Greenberg, L.: Wound contamination and wound infection. J. R. Army Med. Corps 100, 276–295 (1954)
Seligson, D., Ostermann, P.A., Henry, S.L., Wolley, T.: The management of open fractures associated with arterial injury requiring vascular repair. J. Trauma 37, 938–940 (1994)
Singer, A.J., Hollander, J.E., Quinn, J.V.: Evaluation and management of traumatic lacerations. N Engl J. Med. 337, 1142–1148 (1997) [Correction, 1998;338:474]
Sloan, J.P., Dove, A.F., Maheson, M., et al.: Antibiotics in open fractures of the distal phalanx? J. Hand Surg. Br. 12, 123–124 (1987)
Stoddard, J.L.: The occurrence and significance of B. welchii in certain wounds. J. Am. Med. Assoc. 71, 1400–1402 (1918)
Templeman, D.C., Gulli, B., Tsukayama, D.T., Gustilo, R.B.: Update on the management of open fractures of the tibial shaft. Clin. Orthop. 350, 18–25 (1998)
Tong, M.: Septic complications of war wounds. J. Am. Med. Assoc. 219, 1044–1047 (1972)
Urban, C., Maurer-Segal, R.J.J.: Considerations in control and transmission of nosocomial infections due to multi-drug resistant Acinetobacter baumannii. Clin. Infect. Dis. 36, 1268–1274 (2003)
Velmahos, G.C., Toutouzas, K.G., Sarkisyan, G., et al.: Severe trauma is not an excuse for prolonged antibiotic prophylaxis. Arch. Surg. 137, 537–542 (2002)
Weapons effects and parachute injuries. In: Emergency War Surgery, vol. 1, pp. 1–1.4. 3rd US revision. Borden Institute, Washington, DC (2004)
Yun, H.C., Branstetter, J.G., Murray, C.K.: Osteomyelitis in military personnel wounded in Iraq and Afghanistan. J. Trauma 64, S163–S168 (2008)
Zouris, J.M., Walker, G.J., Dye, J., et al.: Wounding patterns for U.S. Marines and sailors during Operation Iraqi Freedom, major combat phase. Mil. Med. 171, 246–252 (2006)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Berlin Heidelberg
About this chapter
Cite this chapter
Finkelstein, R. (2011). Prevention of Infection and Antibiotic Use in the Management of Armed Conflict Injuries to the Extremities. In: Lerner, A., Soudry, M. (eds) Armed Conflict Injuries to the Extremities. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-16155-1_10
Download citation
DOI: https://doi.org/10.1007/978-3-642-16155-1_10
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-16154-4
Online ISBN: 978-3-642-16155-1
eBook Packages: MedicineMedicine (R0)