Abstract
Implantation is a complex process involving an intricate cascade of molecular interactions between the implanting blastocyst and the receptive endometrium. The molecular basis of endometrial receptivity and the mechanisms by which the blastocyst first adheres to the luminal epithelium and then penetrates into the stroma are only just beginning to be resolved. Advances in “omics” technologies, particularly proteomics and metabolomics, are set to have a major impact on the development of this field. In the wake of this information, novel targets for contraceptive intervention may become apparent.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Implantation of the developing blastocyst is an absolute requirement for reproduction. From the embryo’s viewpoint, its goal is to invade the maternal tissue and gain access to nutrients that are essential for survival and development. Implantation is a complex process in which a semiallogeneic embryo needs to be accepted by the maternal endometrium. For this to occur, a bi-directional communication between the blastocyst and the endometrium is required. This dialog enables a synchronous development of the viable embryo and the development of endometrial receptivity followed by embryo apposition, adhesion, and invasion into the stroma (Dominguez et al. 2002).
Endometrial receptivity is a self-limited period in which the endometrium acquires a functional and transient ovarian steroid-dependent status that allows a blastocyst to be received and which further supports implantation through the mediation by immune cells, cytokines, growth factors, chemokines, and adhesion molecules (Kämmerer et al. 2004; Giudice 1999a; Dimitriadis et al. 2005). This specific period, known as “the window implantation,” opens 4–5 days after endogenous or exogenous progesterone stimulation and closes 9–10 days afterwards (Finn and Martin 1974; Martín et al. 2002).
Implantation itself is governed by a collection of endocrine and autocrine signals of embryonic and maternal origins as well as by the corresponding embryo– endometrial dialog. Understanding the activity and function of the molecules involved in this dialog will enable us to use them as predictors of either endometrial receptivity or embryo quality.
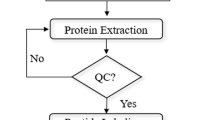
Recently, major advances in the genomics of the endometrium (Horcajadas et al. 2007) and oocytes (Bermúdez et al. 2004) have been achieved with the microarray and bioinformatics technologies available, to provide a vast amount of information regarding gene expression in these tissues and cells. However, gene expression is only one aspect of the complex regulatory network that allows cells to respond to intracellular and extracellular signals. Unlike the genome, the proteome itself is dynamic, complex, and variable. Furthermore, it depends upon the developmental stage of the cells, reflecting the impact of both internal and external environmental stimuli. Proteomics is often considered the next step in the study of biological systems (Fig. 1) and is more complicated than genomics, mostly because the proteome differs from cell to cell, while an organism’s genome is constant, albeit with exceptions. To date, lack of sensitivity has been a stumbling block for the global introduction of proteomics into the field of human reproduction. However, new developments in mass spectrometry using protein profiling and peptide sequencing have been implemented to elucidate the underlying biological processes. In this chapter, we will review the state-of-the-art of proteomics during embryonic implantation (Fig. 2).
Strategies of proteomic analysis. Proteins are extracted from biological samples, fractionated, separated, and analyzed by differential techniques. In gel-based methods (left), different protein samples are labeled with different fluorescent dyes and are then mixed together. Next, proteins are separated into two-dimensional difference gel electrophoresis (2D-DIGE) according to their isoelectric point and molecular mass. Gels are scanned by lasers and those spots corresponding to proteins with a differential pattern of expression are identified. Finally, these proteins are identified by mass spectrometry (MALDI-TOF/TOF). In the chromatographic separation methods (center), protein extracts, protein fractions (SELDI), or one-dimensional gel bands (SDS-PAGE) are digested enzymatically, and the peptide mixture is separated by liquid chromatography (HPLC). Usually, peptides are analyzed and typically identified by an electrospray ionization mass spectrometer coupled with a linear ion trap. Other methods are based on proteins arrays (right). These arrays are membranes that contain a certain number of preabsorbed antibodies that correspond to different proteins
Application of proteomic technologies to the study of embryo implantation. This figure shows the proteomics approaches that can be used to study the embryo implantation process. The identification of differentially expressed proteins will allow us to understand this complex biological process and to use them as key interceptive markers, to prevent embryo implantation, as markers of endometrial receptivity, embryo viability or as causes of disease
2 Proteomic/Secretomics of the Human Embryo
A crucial aspect in implantation is the concept of “embryo viability,” that is, acquisition of the ability to recognize, adhere, and invade the endometrial tissue. The selection of appropriate embryos for their transfer to the uterus is a critical issue in the field of reproductive medicine. Morphological evaluation remains the primary method of embryo assessment during IVF cycles, but its limited predictive power and inherent inter- and intraobserver variability limits its value (Guerif et al. 2007). Consequently, there is a need to objectively identify those embryos with the highest implantation potential based on specific genomic, proteomic, and/or metabolomic profiles.
Katz-Jaffe et al. (2006a) developed a method to analyze the proteome of individual human blastocysts and to identify differentially expressed proteins prior to implantation. Cryopreserved individual embryos for research were obtained from couples undergoing infertility treatment and were donated with consent and analyzed by time-of-flight mass spectrometry. Differential protein expression profiles were observed between early and expanded blastocysts, and also by developing blastocysts as opposed to degenerate embryos. Significantly, several up-regulated and down-regulated proteins were detected in degenerating embryos. A search in the protein databases highlighted several candidates, including an inhibitor of Tcf-4 (transcription factor mediating Wnt signaling) and an apoptotic protease-activating factor. Degenerating embryos displayed a significant up-regulation of several potential biomarkers which may be involved in apoptotic and growth-inhibiting pathways. Therefore, these data linked the proteomic profiles to embryo morphology.
Given the technical and ethical difficulties implied in handling human embryos, research is progressing through the application of noninvasive proteomics to study the molecules both produced by the embryo and secreted into the surrounding medium to identify novel biomarkers of embryo development and viability. In this perspective, little is known about the peptide/protein production and consumption of human embryos.
Several groups have focused on the identification of the specific molecules secreted by the embryo into conditioned media, which are considered critical for embryo viability, such as IL-1α and IL-6 (Baranao et al. 1997), IL-1α (Sheth et al. 1991), or soluble human leukocyte antigen G (HLA-G) (Desai et al. 2006; Fuzzi et al. 2002). These later studies revealed higher pregnancy rates when soluble HLA-G was detected in the conditioned media of day 3 embryos. However, the results were not consistent as pregnancies were obtained from HLA-G negative embryos. Since individual mammalian embryos have very different developmental potentials, even within the same cohort, it will be necessary to evaluate several parameters for the definitive indication of developmental competence and embryonic viability.
The proteomics platform has been successfully employed to analyze the secretome of mammalian embryos throughout preimplantation development, and a database of secretome profiles representing preimplantation development has been created (Katz-Jaffe et al. 2006b). This work revealed that human embryos produce distinctive protein profiles every 24 h of their development (P<0.05) with proteins that are differentially expressed, while others remain constant across the different embryonic stages. The correlation of day 5 secretome data with ongoing blastocyst development revealed an 8.5 kDa protein biomarker that was significantly up-regulated (P<0.05). The best candidate for this biomarker was ubiquitin, which has been implicated in the implantation process in some mammalian species. Ongoing research focuses on the identification of other proteins and also on the correlation of these unique protein profiles with both viability and ongoing successful pregnancy.
Recently, our group reported the partial embryonic secretome (proteins secreted/consumed) by the human blastocyst related to their implantation ability (Domínguez et al. 2008). The aim of this work was to identify changes in the protein profile of the culture media from human blastocyst cultured for 24 h, which either implanted or did not implant, using protein-array technology. Furthermore, a statistical approach was performed to compare each of these media with a medium that did not contain blastocysts (control medium). When the protein profile of the blastocyst culture medium was compared with the controls, soluble TNF receptor 1 and IL-10 increased significantly, whereas MSP-a, SCF, CXCL13, TRAILR3, and MIP-1b decreased significantly. Specifically, CXCL13 and GM-CSF also decreased significantly in the implanted blastocyst media compared with the media from nonimplanted counterparts with a similar morphology.
We have also investigated the secretome profile of implanted blastocysts which developed after performing an embryo biopsy for preimplantation genetic diagnosis and were subsequently grown in a sequential system or cocultured with endometrial epithelial cells (EEC) (Dominguez et al. 2008a). The results after having applied protein-array technology showed a different protein pattern in these two culture systems. Interestingly, IL-6 was the most abundantly secreted protein in the EEC coculture, which enables us to conclude that the IL-6 present in the media is consumed/metabolized by the blastocyst and could be necessary for the developmental process. Furthermore, IL-6 could be considered a potential predictor of blastocyst selection, as an alternative to the usual morphological criteria.
Definitive identification of the key development proteins will provide insights into the cellular and biochemical processes occurring during human embryonic development. In addition, these data could contribute to the development of a noninvasive viability assay to be used in both clinical IVF and animal biotechnology. The identified differences in the protein profile of the culture media in the presence of implanted vs. nonimplanted blastocysts could be used as a potential marker of embryo viability and, therefore, a useful tool other than morphology to select the more appropriate blastocysts to be transferred.
3 Proteomics of the Human Endometrium
The dynamics of the endometrial transition from the nonreceptive stage to the receptive stage at the proteomic level deserves further attention to understand endometrial receptivity and to identify potential molecules for interception. DeSouza et al. (2005) employed a quantitative approach to assess the proteomic repertoire using isotope-coded affinity tags (ICAT), affinity purification and liquid chromatography coupled online to Mass Spectrometry (LC-MS) between proliferative and secretory endometria. Only five proteins showed a consistent differential expression, of which the glutamate NMDA receptor subunit zeta 1 precursor and FRAT1 were the most interesting proteins. The utility of these proteins as indicators of receptivity endometrial is open to further research.
Our group compared the proteomes of prereceptive (day LH+2) vs. receptive (LH+7) endometrial biopsies obtained from the same fertile woman (n=6) in the same menstrual cycle. Biopsies were analyzed using two-dimensional fluorescence difference gel electrophoresis (2D-DIGE) and matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF-MS). Seventy-eight differentially expressed proteins were found in the receptive vs. prereceptive endometrium, with 44 and 34 up- and down-regulated spots, respectively. It is interesting to emphasize two of the most consistently and differentially expressed proteins, Annexin A2 and Stathmin 1, which may prove important in predicting the receptivity status and could, therefore, be possible targets for interception (Dominguez et al. 2008b).
Proteomic techniques have been also used to search for proteins which are differentially expressed in endometriosis. This gynecological condition occurs when endometrial tissue becomes implanted in ectopic sites outwith the uterus, usually within the peritoneal cavity (Kitawaki et al. 2002; Donnez et al. 2002). Tabibzadeh et al. compared the 2D-PAGE of peritoneal fluid (PF) of women with and without endometriosis. However, the gels exhibited a limited number of protein spots, and the identity of the majority of the protein spots with an abnormal expression in endometriosis was neither determined by immunoblotting nor mass spectrometry (Tabibzadeh et al. 2003). Instead, they showed marked differences in the amount and type of the PF proteins present in six women with mild endometriosis, in six women with severe endometriosis, in six women with infertility and no endometriosis, and in six fertile controls using 2-DE. The proteins observed in women with infertility and without endometriosis did not differ from those of healthy controls, and mild endometriosis was associated only with a mild reduction of proteins in the 35–40 kDa and pI 5.7–6.0 ranges when compared with controls. However, a more marked decrease in the same protein spots was observed in women with severe endometriosis, which also presented a two- to fourfold increase in the amount of other numerous proteins seen in severe endometriosis when compared with controls.
Fowler et al. (2007) investigated the effects of endometriosis on the proteome of the human eutopic endometrium by using 2D-PAGE and mass spectrometry. Several deregulated proteins were identified including (1) molecular chaperones such as heat shock protein 90 and annexin A2, (2) proteins involved in the cellular redox state, such as peroxiredoxin 2, (3) molecules involved in protein and DNA formation/breakdown, including ribonucleoside-diphosphate reductase, prohibitin and prolyl 4-hydroxylase, and (4) secreted proteins, such as apolipoprotein A1.
In a similar work, Zhang et al. (2006) designed a study to search for endometriosis-specific proteins using 2-DE, and mass spectrometry. The 2-DE protein patterns of the average gels of the sera samples from women with or without endometriosis were compared, and different protein spots were detected with a discrepancy that was at least threefold. After the comparative proteomic study, the authors found 13 protein spots from serum that correlated with 11 known proteins which were expressed differently between women with and without endometriosis. While some of the differentially expressed proteins originated from the cytoskeleton, others were regulatory proteins of the cell cycle, associated with signal transduction, or with immunological function. Such proteins include the G antigen family B1 protein, actin-related protein 6, actin like-7-anhydrase I, Dentin matrix acidic phosphoprotein I, CD166 antigen, and cyclin A1, among others.
4 Proteomics of Human Endometrial Fluid
The viscous fluid secreted by the endometrial glands provides nutrients for blastocyst formation and constitutes a microenvironment where the embryo–endometrial dialog occurs prior to implantation. It is also an important compartment for the assessment of endometrial maturation (Beier-Hellwig et al. 1989; Giudice 1999b; Lindhard et al. 2002; Herrler et al. 2003; Beier 1974; Maathuis and Aitken 1978; Beier and Beier-Hellwig 1998). Furthermore, uterine secretions are less complex in terms of their protein repertoire and may serve as a pool of biomarkers for functional endometrial operation.
Endometrial secretion has been shown to contain (1) proteins originating from the transudation of serum, (2) leakage products of apoptotic epithelial cells, and (3) proteins secreted from the glandular epithelium. This secretion undergoes significant changes in protein content during the transition from the proliferative phase to the secretory phase (Maathuis and Aitken 1978). Endometrial secretion composition varies during the menstrual cycle as a result of the changes in the ovarian steroid serum concentration (Beier and Beier-Hellwig 1998). Estradiol (E2) regulates transudation by blood vessel dilatation and permeability, and progesterone (P) controls the secretory activity of the endometrial glands. Furthermore, endometrial secretion contains cytokines such as leukemia inhibitory factor (LIF) (Laird et al. 1997), glycodelin (PP14) (Li et al. 1993a), macrophage colony-stimulating factor (M-CSF), epidermal growth factor (EGF), vascular endothelial growth factor (VEGF) (Classen-Linke et al. 2000), insulin-like growth factor binding protein 1 (IGFBP-1), interleukins (Simon et al. 1996; Makkar et al. 2006), as well as steroid and nonsteroid hormones (estrogen, progesterone, prolactin, human chorionic gonadotrophin, and precursors) (Stone et al. 1986; Licht et al. 1998).
In the past, the protein patterns of uterine secretions throughout the menstrual cycle have been analyzed by electrophoresis. These analyses revealed three different protein patterns that are typical of the equivalent phases of the menstrual cycle: intermediate phase, proliferative phase, and secretory phase. The results showed characteristic “families” of proteins bands, corresponding to 63 proteins, and some of them were identified by their molecular mass (Beier-Hellwig et al. 1989).
In another work (Van der Gaast et al. 2003), endometrial fluid obtained transcervically by aspiration immediately prior to embryo transfer was analyzed and the protein profile in each sample was determined. Although uterine fluid aspiration is a safe method, sometimes the material obtained is not enough for analysis or it may be diluted as a result of uterine washing, making the results difficult to consider. These studies also demonstrated that endometrial secretion can be obtained for analysis immediately prior to embryo transfer in IVF cycles without disrupting implantation (Li et al. 1993b; Olivennes et al. 2003).
More recently, Van der Gaast et al. (2008) investigated the effect of ovarian stimulation in IVF on endometrial secretion and markers of receptivity in the midluteal phase. The endometrial fluids obtained during this period in the stimulated cycle were compared with the spontaneous cycle. Protein composition was analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), and gels were stained with Coomassie brilliant blue. The protein pattern was obtained by measuring the relative density of each band by means of scanning laser densitometer and the GelScan XL software package. In this pilot study, ovarian stimulation did not alter the investigated markers of endometrial maturation in the midluteal phase.
Classically, two-dimensional electrophoresis, based on a combination of isoelectric focusing and SDS-PAGE, was the only method available to analyze the protein complement in a sample with high resolution. The introduction of protein chips and mass spectrometry has facilitated protein identification. Presently, our group is working on the proteomic analysis of endometrial fluid from natural cycles using liquid chromatography online with electrospray ionization-ion trap mass spectrometry (ESI-LC-MS) techniques. This approach circumvents one of the major challenges of endometrial research, that of investigating endometrial performance during the window of implantation without disrupting endometrial function and the subsequent process of implantation.
The current technical limitations of applying proteomics to the study of protein patterns in endometrial fluid is that the majority of identified proteins correspond to serum proteins, thus masking the identification of proteins present at low concentrations which may be of great interest, such as biomarkers for endometrial receptivity, embryo development, diseases, and/or contraceptive intervention.
5 Conclusions
The significant histological, biological, and physiological events that occur during implantation are ultimately the result of regulated changes in gene transcription, together with posttranscriptional, posttranslational, and epigenetic modifications that ultimately control expression the embryonic and endometrial proteomes (Fig. 3). In recent years, “omics” techniques have advanced to the point that rapid identification of genes or proteins of interest can be readily secured. However, technical limitations still exist which complicate the unification of the results obtained.
Proteomics together with genomics and metabolomics are complementary approaches that provide diverse but comparable perspectives, which will improve our understanding of the complexity of the implantation process, including the identification of key biomarkers. The next step will be to integrate this information into a system biology approach to develop models for functions of interest, such as embryo viability, endometrial receptivity, and the embryo–endometrial dialog.
References
Baranao RI, Piazza A, Rumi LS, Polak de Fried E (1997) Determination of IL-1 and IL-6 levels in human embryo culture-conditioned media. Am J Reprod Immunol 37:191–194
Beier HM (1974) Oviducal and uterine fluids. J Reprod Fertil 37:221–237
Beier HM, Beier-Hellwig K (1998) Molecular and cellular aspects of endometrial receptivity. Hum Reprod Update 4:448–458
Beier-Hellwig K, Sterzik K, Bonn B, Beier HM (1989) Contribution to the physiology and pathology of endometrial receptivity: the determination of proteins patterns in human uterine secretions. Hum Reprod 4:115–120
Bermúdez MG, Wells D, Malter H, Munné S, Cohen J, Steuerwald NM (2004) Expression profiles of individual human oocytes using microarray technology. Reprod Biomed Online 8:325–337
Classen-Linke I, Alfer J, Krusche CA et al (2000) Progestins, progesterone receptor modulators, and progesterone antagonist change VEGF release of endometrial cells in culture. Steroids 65:763–771
Desai N, Filipovits J, Goldfarb J (2006) Secretion of soluble HLA-G by day 3 human embryos associated with higher pregnancy and implantation rates: assay of culture media using a new ELISA kit. Reprod Biomed Online 13:272–277
DeSouza L, Diehl G, Yang E, Guo J, Rodrigues MJ, Romaschin AD, Colgan TJ, Siu M (2005) Proteomic analysis of the proliferative and secretory phases of the human endometrium: Protein identification and differential protein expression. Proteomics 5:270–281
Dimitriadis E, White CA, Jones R, Salamonsen LA (2005) Cytokines, chemokines and growth factors in endometrium related to implantation. Hum Reprod Update 11:613–630
Dominguez F, Pellicer A, Simon C (2002) Paracrine dialogue in implantation. Mol Cell Endocrinol 186:175–181
Dominguez F, Gadea B, Mercader A, Esteban F, Pellicer A, Simon C (2008) Embryological outcome and secretome profile of implanted blastocyst obtained. Fertil Steril. doi:10.1016/j.fertnstert.2008.10.019. PMID 19062008
Dominguez F, Garrido-Gomez T, Lopez JA, Camafeita E, Quiñonero A, Pellicer A, Simon C (2009) Proteomic analysis of the human receptive versus non-receptive endometrium using differential in-gel electrophoresis and MALDI-MS unveils stathmin I and annexin A2 as diffrentially regulated. Hum Reprod 24:2607–2617
Domínguez F, Gadea B, Esteban FJ, Horcajadas JA, Pellicer A, Simón C (2008) Comparative protein-profile analysis of implanted versus non-implanted human blastocyst. Hum Reprod 23:1993–2000
Donnez J, Van Langendonckt A, Casanas-Roux F, Van Gossum JP et al (2002) Current thinking on the pathogenesis of endometriosis. Gynecol Obstet Invest 54:52–58
Finn CL, Martin L (1974) The control of implantation. J Reprod Fertil 39:195–206
Fowler PA, Tattum J, Bhattacharya S, Klonisch T, Hombach-Klonish S, Gazvani R, Lea RG, Miller I, Simpson WG, Cash P (2007) An investigation of the effects of endometriosis on the proteome of human eutopic endometrium: a heterogeneous tissue with a complex disease. Proteomics 7:130–142
Fuzzi B, Rizzo R, Criscuoli L, Noci I, Melchiorri L, Scarselli B et al (2002) HLA-G expression in early embryos is a fundamental prerequisite for the obtainment of pregnancy. Eur J Immunol 32:311–315
Giudice LC (1999) Implantation and endometrial function. In: BCJM Fauser (ed) Molecular biology in reproductive medicine. Parthenon Publishing Group, New York, NY, USA, London, UK
Giudice LC (1999b) Potencial biochemical markers of uterine receptivity. Hum Reprod 14:3–16
Guerif F, Le Gouge A, Giraudeau B, Poindron J, Bidault R, Gasnier O, Royere D (2007) Limited value of morphological assessment at days 1 and 2 to predict blastocyst development potential: a prospective study based on 4042 embryos. Hum Reprod 22:1973–1981
Herrler A, von Rango U, Bier HM (2003) Embryo-maternal signalling: how the embryo starts talking to its mother to accomplish implantation. Reprod Biomed Online 6:244–256
Horcajadas JA, Pellicer A, Simón C (2007) Wide genomic analysis of human endometrial receptivity: new times, new opportunities. Hum Reprod Update 13:77–86
Kämmerer U, von Wolff M, Markert UR (2004) Inmunology of human endometrium. Inmunobiology 209:569–574
Katz-Jaffe MG, Gardner DK, Schoolcraft WB (2006a) Proteomic analysis of individual human embryos to identify novel biomarkers of development and viability. Fertil Steril 85:101–107
Katz-Jaffe MG, Schoolcraft WB, Gardner DK (2006b) Analysis of protein expression (secretome) by human and mouse preimplantation embryos. Fertil Steril 86:678–685
Kitawaki J, Kado N, Ishihara H, Koshiba H et al (2002) Endometriosis: the pathophysiology as an estrogen-dependent disease. Steroid Biochem Mol Biol 83:149–155
Laird SM, Tuckerman EM, Dalton CF (1997) The production of leukaemia inhibitory factor by human endometrium: presence in uterine flushings and production by cells in culture. Hum Reprod 12:569–574
Li TC, Dalton C, Hunjan KS et al (1993a) The correlation of placental protein 14 concentrations in uterine flushings and endometrial morphology in the peri-implantation period. Hum Reprod 8:1923–1927
Li TC, MacKenna A, Roberts R (1993b) The techniques and complications of out-patient uterine washing in the assessment of endometrial function. Hum Reprod 8:343–346
Licht P, Losch A, Dittrich R et al (1998) Novel insights into human endometrial paracrinology and embryo-maternal communication by intrauterine microdialysis. Hum Reprod Update 4:532–538
Lindhard A, Bentin-Ley U, Ravn V (2002) Biochemical evaluation of endometrial function at the time of implantation. Fertil Steril 78:221–233
Maathuis JB, Aitken RJ (1978) Protein patterns of human uterine flushings collected at various stages of the menstrual cycle. J Reprod Fertil 53:343–348
Makkar G, Ng EH, Yeung WS, Ho PC (2006) Reduced expression of interleukin-11 and interleukin-6 in the peri-implantation endometrium of excessive ovarian responders during in-vitro fertilization treatment. J clin Endocrin Metab 91:3181–3188
Martín J, Dominguez F, Avila S, Castrillo JL, Remohí J, Pellicer A, Simón C (2002) Human endometrial receptivity: gene regulation. J Reprod Immunol 55:131–139
Olivennes F, Ledee-Bataille N, Samama M, Kadoch J, Taupin JL, Dubanchet S et al (2003) Assessment of leukemia inhibitary factor levels by uterine flushing at the time of egg retrieval does not adversely affect pregnancy rates with in vitro fertilization. Fertil Steril 79:900–904
Sheth KV, Roca GL, al-Sedairy ST, Parhar RS, Hamilton CJ, al-Abdul Jabbar F (1991) Prediction of successful embryo implantation by measuring interleukin-1-alpha and immunosuppressive factor(s) in preimplantation embryo culture fluid. Fertil Steril 55:952–957
Simon C, Mercader A, Frances A et al (1996) Hormonal regulation of serum and endometrial IL-1α, IL-1β and IL-1ra: IL-1 endometrial microenvironment of the human embryo at the apposition phase under physiological and supraphysiological steroid level conditions. J Reprod Inmunol 31:165–184
Stone BA, Petrucco OM, Seamark RF, Godfrey BM (1986) Concentrations of steroid hormones, and of prolactin, in washings of the human uterus during the menstrual cycle. J Reprod Fertil 78:21–25
Tabibzadeh S, Becker JL, Parsons AK (2003) Endometriosis is associated with alterations in the relative abundance of proteins and IL-10 in the peritoneal fluid. Front Biosci 8:70–78
Van der Gaast MH, Beier-Hellwig K, Fauser BC, Beier HM, Macklon NS (2003) Endometrial secretion aspiration prior to embryo transfer does not reduce implantation rates. Reprod Biomed Online 7:105–109
Van der Gaast MH, Classen-Linke I, Krusche CA, Beier-Hellwig K, Fauser BCJM, Beier HM, Macklon NS (2008) Impact of ovarian stimulation on mid-luteal endometrial tissue and secretion markers of receptivity. RBM Online 4:553–563
Zhang H, Niu Y, Fend J, Guo H, Ye X, Cui H (2006) Use of proteomic analysis of endometriosis to identify different protein expression in patients with endometriosis versus normal controls. Fertil Steril 86:274–282
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Garrido-Gómez, T., Dominguez, F., Simón, C. (2010). Proteomics of Embryonic Implantation. In: Habenicht, UF., Aitken, R. (eds) Fertility Control. Handbook of Experimental Pharmacology, vol 198. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-02062-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-642-02062-9_5
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-02061-2
Online ISBN: 978-3-642-02062-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)