Abstract
Experimental sebaceous gland models are essential for a better understanding of the pathophysiology of human skin disorders involving the sebaceous gland, such as sebostasis, seborrhea, and acne, for thorough research and development of cosmetics and drugs, and for investigation of drug pharmacokinetics. So, the need for an established model for studies of sebocyte differentiation and for pharmacologic assays has led into considerable advances in this field (Table 6.1).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara Core Messages-
Seborrhea and acne are exclusively human disorders and sebaceous gland differentiation is species-specific, thus posing the need for human in vitro models.
-
Human sebaceous gland cell lines (SZ95 as well as SEB-1, Seb-E6E7) have been used in monolayer cultures as models to study specific functions involved in development, growth, and differentiation of sebaceous gland cells.
-
Maintenance of sebaceous gland cells in certain culture conditions has helped to investigate the physiology of the sebaceous gland, including its changes in acne.
-
Sebocyte culture models have provided insight in the mechanism of action of acne treatments, including retinoids, anti-androgens, and PPAR ligand antagonists.
-
More complex culture systems, including three-dimensional models are under development.
-
Sebocyte culture models provide new chances for further research on biologically active ingredients, new pharmaceutical and cosmetic drugs for antiaging, and acne treatment.
1 Introduction
Experimental sebaceous gland models are essential for a better understanding of the pathophysiology of human skin disorders involving the sebaceous gland, such as sebostasis, seborrhea, and acne, for thorough research and development of cosmetics and drugs, and for investigation of drug pharmacokinetics. So, the need for an established model for studies of sebocyte differentiation and for pharmacologic assays has led into considerable advances in this field (Table 6.1).
Several attempts were made to cultivate animal [1, 2] or human sebaceous gland cells, using mechanical dissociation of isolated sebaceous glands or enzymatic separation of sebocytes from skin sections with a keratotome [3, 4]. However, seborrhea and acne are exclusively human diseases and sebaceous gland differentiation is species-specific, and no animal model was found to be predictive in assessing antiacne drug effects in humans. So, basic research on human sebaceous gland function and control requires human in vitro models.
Initial studies have been reported on experimental models carried out on whole human skin plugs, either incubated in vitro [5–7] or grafted on to nude mice [8]. However, it was not until the isolation of viable human sebaceous glands and pilosebaceous units [9, 10] and the establishment of the human sebocyte culture model in vitro [11] that fundamental research on human sebocyte activity and its regulation begun [12].
Human sebaceous gland experimental models have shed light on a plethora of functions of the sebaceous gland, highlighting its role in skin homeostasis [13]. Apart from acne, sebaceous glands are involved in embryology, development, and differentiation; in skin protection; and in inflammation and immunity and display complex endocrine properties (Table 6.2) [13]. Also, sebocytes, despite their programming for terminal differentiation, preserve characteristics of stem-like cells, as they present a remarkable potential of dual differentiation. The interactions between β-catenin and Sonic hedgehog promote proliferation of progenitors of the hair lineages, while Indian hedgehog stimulates proliferation of sebocytes precursors [14]. Overexpression of myc stimulates sebocyte differentiation, whereas overexpression of β-catenin stimulates interfollicular epidermal differentiation in vitro [15].
2 Human Experimental Models of the Pilosebaceous Unit
Karasek and Charlton [3, 4] first described the cultivation of human sebocytes in collagen after enzymatic dissociation of isolated sebaceous glands and in monolayers after enzymatic digestion of sebaceous-gland-rich dermal slices obtained with a Castroviejo keratotome. Cells obtained by the first technique exhibited a significant loss of sebocyte characteristics in vitro. The latter method was modified later and further developed by Doran et al. [16] who removed the top 0.4-mm facial skin section containing the epidermis and some of the dermis and used the second 0.4-mm dermal section as the source of human sebocytes.
The first successful human sebocyte culture was introduced in 1989 by Xia et al. [11] with the in vitro subcultivation of human sebaceous gland-derived cells. Intact sebaceous glands were isolated from full-thickness human skin after incubation in dispase and deoxyribonuclease. Human sebocyte monolayer cultures as outgrowths from the periphery of sebaceous gland organ cultures were obtained. The ducts of the glands were removed; the isolated gland lobules were seeded on a 3 T3-cell feeder layer in Dulbecco’s modified Eagle’s medium and Ham’s F 12 medium (3:1) supplemented with fetal calf serum (10 %), l-glutamine, antibiotics, epidermal growth factor (10 ng/ml), hydrocortisone (0.4 μg/ml), and cholera toxin (10-9 M), and were then cultivated in a CO2 incubator at 37° C. After 2–3 weeks, cell outgrowths resulted from the periphery of the gland lobules, and dispersed cells were subcultured thrice with or without 3 T3-cell feeder layer. The cultured cells preserved in vitro morphologic characteristics and differentiation patterns comparable to those described for normal human sebocytes in vivo with a high rate of viable cells. Their labeling pattern with monoclonal antibodies showed close similarities to the pattern of keratinocytes in vivo and in vitro. In their cytoplasm oil red- and nile red-stained droplets were detected, and the observed density and distribution evidenced in vitro lipogenesis. This technique demonstrated the growth of cells originating from intact human sebaceous glands and their long-term differentiation into lipid-producing cells in vitro [11]. Also, sebocyte cultures could be obtained not only from sebaceous-gland-rich skin areas but also from other areas of the human skin [17]. Disadvantages of the method included the fact that the exact separation of glands from the skin was time consuming and required skillful preparation and that the rather low number of proliferating cells in the intact sebaceous gland lobules did not provide optimal conditions for their in vitro growth.
Over the years, modifications of the technique of Xia and al [11]. have improved the culture of human sebocytes in vitro. Zouboulis et al. [18] modified the culture medium including 2 % human serum, 8 % fetal calf serum, and omitting hydrocortisone. Lee [19] treated sebaceous glands with collagenase before cultivating them in serum-free William’s E medium supplemented with 10 μg/ml insulin, 10 μg/ml transferring, 10 μg/ml hydrocortisone, 10 ng/ml epidermal growth factor, 10 ng/ml sodium selenite, 2 nmol/l l-glutamine, and penicillin/streptomycin [19]. Primary sebocyte cultures could also be obtained by omitting the 3 T3 fibroblast layer, and secondary cultures could be grown in a medium supplemented with delipidized serum and serum-free keratinocyte basal medium. [20–22]
Fujie et al. [23] cultured primary sebocytes after the technique of Xia et al. [11] for at least three passages in serum-free keratinocyte growth medium without a feeder cell layer. Keratinocyte growth factor, shown to be a mitogen for primary cultures of mammary epithelium alone or combined with epidermal growth factor and/or bovine serum albumin, was found to significantly improve yield rates and proliferation of human sebocytes [24–26].
Human sebocytes however, are predestined to differentiate by accumulating neutral fat droplets until they burst and die. Therefore, adequate cell amounts for large-scale experiments could only be obtained from multiple donors, whereas prolonged experiments were hindered by the short life spans of the cells, as normal human sebocytes could only be grown for 3–6 passages.
These drawbacks were overcome by the generation of an immortalized sebocyte cell line (SZ95) by Zouboulis et al. [27] by transfecting cultured human facial sebocytes from a 87-year old woman with the Simian virus 40 large T antigen. The SZ95 sebaceous gland cell line is nowadays protected by national and international patents as well as priority submissions [28]. SZ95 sebocytes exhibit similar morphologic, phenotypic, and functional characteristics of normal human sebocytes. Several studies have shown that SZ95 sebocytes retain major characteristics of normal human sebocytes, such as progressing differentiation with increasing cell volume and lipid synthesis, expression of markers of sebaceous lineage and terminal sebocyte differentiation, such as keratin 7 and epidermal membrane antigen (EMA), respectively [18], and can subsequently undergo apoptosis [29]. SZ95 sebocytes also express characteristic organ- and function-specific proteins of human sebaceous glands and exhibit expected biological responses to androgens and retinoids [27, 29].
In 2003, Thiboutot et al. [30] applied the transfection system administered by Zouboulis et al. [27] to develop a second immortalized human sebaceous gland cell line, termed SEB-1. SEB-1 was established from sebaceous glands of normal skin of the preauricular area of a 55-year-old male. Like SZ95 sebocytes, SEB-1 sebocytes also express characteristic sebaceous gland proteins and their cytoplasm-induced oil red O-positive lipid droplets. In gene array studies, genes characteristic for the sebaceous gland and such involved in lipid and steroid metabolism were expressed in SEB-1 sebocytes.
A third immortalized sebaceous gland cell line, Seb-E6E7, has been generated from adult human facial skin following a facelift procedure. Human sebocytes were immortalized by introduction of HPV16 E6 and E7 genes. Seb-E6E7 sebocytes were transduced by coculture with mitomycin C-treated packaging cells in the presence of 3 T3-J2 cells. Seb-E6E7 sebocytes, like SZ95 sebocytes, express both K7 and involucrin. In first experiments, Seb-E6E7 seem to respond to chemicals in a similar manner with SZ95 sebocytes despite their different transfection methods [15].
3 Acne Treatments Investigated in Experimental Sebocyte Culture Models
Cell culture models, especially the SZ95 sebaceous gland cell line, have advanced in excellent models to investigate new ingredients against seborrhea, acne, and aging skin.
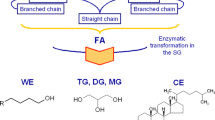
Antiacne therapies investigated in vitro include retinoids, anti-androgens, and zileuton, a potent peroxisome proliferator-activated (PPAR)-α ligand antagonist [31, 32] (Table 6.3). Among these, the most investigated therapy in vitro is 13cis retinoic acid. Its mechanism of action has been elucidated by in vitro sebocyte research revealing that 13cis retinoic acid and all-trans retinoic acid inhibit the proliferation of cultured sebocytes in a dose- and time-dependent manner [22, 33, 34]. Marked decreases in wax esters, a slight decrease in squalene, and a relative increase in cholesterol level have been measured. It has been shown that 13cis retinoic acid undergoes intracellular isomerization to all-trans retinoic acid in human sebocytes, which then exerts its antiproliferative effect on sebocytes via binding to retinoic acid receptors (RAR) [35]. Also, 13cis retinoic acid causes cell cycle arrest and induced apoptosis in cultured sebocytes by a RAR independent mechanism [36] and may reduce the mRNA expression of pro-matrix metalloproteinase (MMP)-2, proMMP-9, proMMP-13, which are increased in acne [37].
Anti-androgens have been studied regarding their mechanism of action in acne. Anti-androgens, like spironolactone, inhibit the stimulatory effect of testosterone and 5α-dihydrotestosterone on sebocyte proliferation. They inhibit lipogenesis under the presence of peroxisome proliferator-activated receptor (PPAR) ligands [21]. Cyproterone acetate inhibits the activity of 3β-hydroxy-steroid dehydrogenase and blocks the androgen receptor [38].
Zileuton, the only known potent PPARα ligand antagonist, inhibits leukotriene B4 synthesis, thus reducing lipid synthesis [31, 32, 39]. Also, ectopeptidase inhibitors reduce proliferation and cytokine production in SZ95 sebocytes as well as the topical function of human peripheral T cells in vivo and in vitro [40].
Conclusions
Mammal sebocytes and sebocyte-like cells (human, mouse, hamster, rat) and human sebaceous gland cell lines (SZ95, SEB-1, Seb-E6E7) have been used in monolayer cultures as models to study specific functions involved in development, growth, and differentiation of sebaceous gland cells.
Maintenance of these cells in certain culture conditions has helped investigate the physiology of the sebaceous gland, including its changes in acne. Also, sebocyte culture models provide new chances for further research on biologically active ingredients, new pharmaceutical and cosmetic drugs for antiaging, and acne treatment. More complex culture systems, including three-dimensional models, are under development.
References
Carpenter WR, Goodridge AG. Cells isolated from duck sebaceous glands undergo partial differentiation in primary culture. Fed Proc. 1986;45:1579.
Kanaar P, Plameijer HS. An investigation of the influence of testosterone on a sebaceous gland model in organ-culture. Preliminary communication. Dermatologica. 1972;144:353–4.
Karasek MA, Charlton ME. In vitro growth and serial cultivation of normal human sebaceous gland cells. Clin Res. 1982;30:263A.
Karasek MA. Growth characteristics of human sebaceous gland cells in cell culture. Clin Res. 1986;34:416A.
Cooper MF, McGrath H, Shuster S. Sebaceous lipogenesis in human skin. Variability with age and severity of acne. Br J Dermatol. 1976;94:165–72.
Hsia SL, Fulton JE, Fulgham D, et al. Lipid synthesis from acetate-1-C by suction blister epidermis ad other skin components. Proc Soc Exp Biol Med. 1970;135:285–91.
Sharp F, Hay JB, Hodgins MB. Metabolism of androgens in vitro by human fetal skin. J Endocrinol. 1976;70:491–9.
Petersen MJ, Zone JJ, Krueger GG. Development of a nude mouse model to study human sebaceous gland physiology and pathophysiology. J Clin Invest. 1984;74:1358–65.
Kealey T, Lee CM, Thody AJ, et al. The isolation of human sebaceous glands and apocrine sweat glands by shearing. Br J Dermatol. 1986;114:181–8.
Sanders DA, Philpott MP, Nicolle FV, et al. The isolation and maintenance of the human pilosebaceous unit. Br J Dermatol. 1994;131:166–76.
Xia L, Zouboulis C, Detmar M, et al. Isolation of human sebaceous glands and cultivation of sebaceous gland-derived cells as an in vitro model. J Invest Dermatol. 1989;93:315–21.
Zouboulis CC, Xia L, Akamatsu H, et al. The human sebocyte culture model provides new insights into development and management of seborrhea and acne. Dermatology. 1998;196:21–31.
Zouboulis CC, Malte Baron J, Bohm M, et al. Frontiers in sebaceous gland biology and pathology. Exp Dermatol. 2008;17:542–51.
Niemann C, Unden AB, Lyle S, et al. Indian hedgehog and β-catenin signaling: Role in the sebaceous lineage of normal and neoplastic mammalian epidermis. Proc Natl Acad Sci U S A. 2003;100 Suppl 1:11873–80.
Lo Celso C, Berta M, Braun K, et al. Characterisation of bipotential epidermal progenitors derived from human sebaceous gland: contrasting roles of c-Myc and β-catenin. Stem Cells. 2008;26:1241–52.
Doran TI, Baff R, Jacobs P, et al. Characterization of human sebaceous cells in vitro. J Invest Dermatol. 1991;96:341–8.
Doran TI, Baff R. The inhibition of proliferation of human sebaceous cells in vitro as a predictive assay for anti-acne activity. J Invest Dermatol. 1988;90:554.
Zouboulis CC, Xia L, Detmar M, et al. Culture of human sebocytes and markers of sebocytic differentiation in vitro. Skin Pharmacol. 1991;4:74–83.
Lee CM. Cell culture systems for the study of human skin and skin glands. In: Jones CJ, editor. Epithelia: advances in cell physiology and cell culture. Dordrecht: Kluwer; 1990. p. 333–50.
Akamatsu H, Zouboulis CC, Orfanos CE. Control of human sebocyte proliferation in vitro by testosterone and 5-alpha-didydrotestosterone is dependent on the localization of the sebaceous glands. J Invest Dermatol. 1992;99:509–11.
Akamatsu H, Zouboulis CC, Orfanos CE. Spironolactone directly inhibits proliferation of cultured human facial sebocytes and acts antagonistically to testosterone and 5-alpha-dihydrotestosterone in vitro. J Invest Dermatol. 1993;100:660–2.
Zouboulis CC, Korge BP, Mischke D, et al. Altered proliferation, synthetic activity and differentiation of cultured human sebocytes in the absence of vitamin A and their modulation by synthetic retinoids. J Invest Dermatol. 1993;101:628–33.
Fujie T, Shikiji T, Uchida N, et al. Culture of cells derived from the human sebaceous gland under serum-free conditions without a biological feeder layer or specific matrices. Arch Dermatol Res. 1996;288:703–8.
Chen W, Zouboulis CC, Fritsch M, et al. Evidence of heterogeneity and quantitative differences of the type 1 5a-reductase expression in cultured human skin cells: Evidence of its presence in melanocytes. J Invest Dermatol. 1998;110:84–9.
Imagawa W, Cunha GR, Young P, et al. Keratinocyte growth factor and acidic fibroblast growth factor are mitogens for primary cultures of mammary epithelium. Biochem Biophys Res Commun. 1994;204:1165–9.
Seltman H, Ruhl R, Seiffert K, et al. Isotretinoin treatment of human sebocytes in vitro results in low isotretinoin, but considerably elevated tretinoin intracellular levels and its effect is not affected by the presence of retinol. J Invest Deramtol. 1997;108:374.
Zouboulis CC, Seltmann H, Neitzel H, et al. Establishment and characterization of an immortalized human sebaceous gland cell line (SZ95). J Invest Dermatol. 1999;113:1011–20.
Zouboulis CC, Schagen S, Alestas T. The sebocyte culture: a model to study the pathophysiology of the sebaceous gland in sebostasis, seborrhoea and acne. Arch Dermatol Res. 2008;300:397–413.
Wrobel A, Seltmann H, Fimmel S, et al. Differentiation and apoptosis in human immortalized sebocytes. J Invest Dermatol. 2003;120:175–81.
Thiboutot D, Jabara S, McAllister J, et al. Human skin is a steroidogenic tissue: steroidogenic enzymes and cofactors are expressed in epidermis, normal sebocytes, and immortalized sebocyte cell line (SEB-1). J Invest Dermatol. 2003;120:905–14.
Zouboulis CC, Nestoris S, Adler Y, et al. A new concept for acne therapy: a pilot study with zileuton, an oral 5-lipoxygenase inhibitor. Arch Dermatol. 2003;139:668–70.
Zouboulis CC, Saborowski A, Boschnakow A. Zileuton, an oral 5-lipoxygenase inhibitor, directly reduces sebum proliferation. Dermatology. 2005;210:36–8.
Zouboulis CC, Korge B, Akamatsu H, et al. Effects of 13-cis-retinoic acid, all-trans-retinoic acid and acitretin on the proliferation, lipid synthesis and keratin expression of cultured human sebocyte in vitro. J Invest Dermatol. 1991;96:792–7.
Zouboulis CC, Krieter A, Gollnick H, et al. Progressive differentiation of human sebocytes in vitro is characterized by increasing cell size and altering antigen expression and is regulated by culture duration and retinoids. Exp Dermatol. 1994;3:151–60.
Tsukada M, Schroder M, Roos T, et al. 13-cis retinoic acid exerts its specific activity on human sebocytes through selective intracellular isomerization to all-trans retinoic acid and binding to retinoic acid receptors. J Invest Dermatol. 2000;115:321–7.
Nelson A, Gilliland K, Cong Z, et al. 13-cis retinoid acid induces apoptosis and cell cycle arrest in human SEB-1 sebocytes. J Invest Dermatol. 2006;126:2178–89.
Papakonstantinou E, Aletras A, Glass E, et al. Matrix metalloproteinases of epithelial origin in facial sebum of patients with acne and their regulation by isotretinoin. J Invest Dermatol. 2005;125:673–84.
Fritsch M, Orfanos C, Zouboulis CC. Sebocytes are the key regulators of androgen homeostasis in human skin. J Invest Dermatol. 2001;116:793–800.
Zouboulis CC, Seltmann H, Alestas T. Zileuton prevents the activation of the leukotriene pathway and reduces sebaceous lipogenesis. Exp Dermatol. 2010;19:148–50.
Thielitz A, Reinhold D, Vetter R, et al. Inhibitors of dipeptidyl peptidase IV(DP IV) and aminopeptidase N (APN) show strong anti-inflammatory effects on immune cells and therapeutic efficacy in autoimmune disorders. J Invest Dermatol. 2007;127:1042–51.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Zouboulis, C.C., Dessinioti, C. (2014). Experimental Models of the Sebaceous Gland. In: Zouboulis, C., Katsambas, A., Kligman, A. (eds) Pathogenesis and Treatment of Acne and Rosacea. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-69375-8_6
Download citation
DOI: https://doi.org/10.1007/978-3-540-69375-8_6
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-69374-1
Online ISBN: 978-3-540-69375-8
eBook Packages: MedicineMedicine (R0)