Abstract
Maternal cardiovascular disease complicates approximately 0.2–4% of all pregnancies in western industrialized countries, and it is the major cause of maternal death during pregnancy. Women are increasingly seeking pregnancy at a later age, and an increased number of women with congenital problems contemplate pregnancy. Echocardiography is, by far, an important tool during pregnancy providing both qualitative and quantitative information; in addition it can help to stratify maternal risk during pregnancy and consequently to choose the correct management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Echocardiography in pregnancy
- Haemodynamic changes during pregnancy
- Maternal heart during pregnancy
- Valvular heart disease in pregnancy
- Congenital heart disease
- Hypertensive disorders in pregnancy
1 Introduction
Maternal cardiovascular disease complicates approximately 0.2–4% of all pregnancies in western industrialized countries, and it is the major cause of maternal death during pregnancy. Women are increasingly seeking pregnancy at a later age characterized by cardiovascular risk factors (diabetes, obesity, hypertension), resulting in more frequent cardiac events. Furthermore, surgery of congenital heart disease has improved, so as an increased number of women with congenital problems contemplate pregnancy.
2 Haemodynamic Changes/Physiologic Alterations
Pregnancy is a physiological state that induces adaptation of the cardiovascular system to meet the increased metabolic demands of the mother and foetus and to ensure adequate uteroplacental circulation for foetal growth and development. These changes, which occur during labour and delivery and in the postpartum period, can mimic cardiac disease so that an understanding of both haemodynamic alterations and anatomic changes is the key to interpret the echocardiograms in pregnant patients. Further, the normal haemodynamic changes can precipitate cardiac symptoms in previously stable women or may exacerbate symptoms in those with mild baseline symptoms.
Cardiac output increases by about 30–50% by the end of the first trimester, primarily due to an increase in stroke volume and in circulating blood volume. Between the second and third trimesters, cardiac output shows a peak, owing to a 15–20% increase in heart rate and a fall in afterload via decreased total vascular resistance. Arterial blood pressure decreases early in pregnancy, characterized by decreases in DBP exceeding those in SBP. The mean arterial pressure gradually falls, with the largest decrease occurring at 16–20 weeks. BP then begins to rise during the mid-third trimester to levels approaching pre-pregnancy BP values.
During labour and delivery, pain and uterine contractions result in additional increases in cardiac output (20% with each contraction), heart rate, blood pressure and systemic vascular resistance. Because of contribution of pain and anxiety to the increase in heart rate and blood pressures, pain control may help mitigate the haemodynamic changes. Immediately following delivery, relief of caval compression and autotransfusion from the emptied and contracted uterus results in a further increase in preload with venous return of blood to the maternal circulation (approximately 500 mL). This effect can cause cardiac output to increase by 60–80%. Delivery of the placenta increases afterload by removing this low-resistance vascular bed. Most haemodynamic changes of pregnancy resolve by 2 weeks postpartum.
3 Heart Remodelling
During normal pregnancy, the progressive and marked increase in left ventricular stroke volume (as a high-output state) can result in an increased velocity across valves, which may falsely increase systolic or diastolic gradients. The normal flow murmur of pregnancy is typically soft (grade 1 or 2), located at the pulmonic region, associated with a normal first and second heart sound, and is not accompanied by a diastolic murmur or signs of heart failure. As the heart enlarges, the mitral, tricuspid and pulmonary annuli dilate and small functional atrioventricular regurgitations may appear through these valves. As left ventricular volume increases and the position of the mitral valve leaflets changes with respect to one another, pre-existing mitral regurgitation due to mitral valve prolapse may actually improve during pregnancy. During gestation, a small pericardial effusion haemodynamically non-significant is not necessarily indicative of pathology.
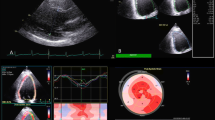
4 Echocardiography
Echocardiography is, by far, an important tool during pregnancy and the preferred diagnostic exam to evaluate pregnant women with cardiac disease due to its availability, accuracy and safety with no risk of radiation to the mother and the foetus. A transthoracic echocardiogram provides both qualitative and quantitative information; in addition it can help to stratify maternal risk during pregnancy and consequently to choose the correct management. Depending on the underlying cardiac abnormality, serial echo examinations rather than a single study may be indicated.
The following conditions are indications to perform an echocardiogram in a pregnant woman:
-
1.
Cardiac complaints including shortness of breath and palpitations out of proportion to what is expected in a normal pregnancy to exclude a diagnosis of a new cardiac disease
-
2.
Pre-existing hypertension to evaluate systolic and diastolic cardiac function
-
3.
Known heart disease (congenital heart disease, cardiomyopathy, ischemic heart disease, valvular heart disease, arrhythmia) to exclude residual defects that need intervention and to evaluate maternal risk
-
4.
Known aortic root dilatation to stratify risk of rupture and decide management
-
5.
Stroke of unknown aetiology
-
6.
A prior history of chemotherapy or radiation in a woman to evaluate cardiac function
MRI (without gadolinium) should be considered if echocardiography is insufficient for diagnosis, and it can be safely performed after the first trimester.
4.1 Echocardiographic Findings
The echocardiographic changes during pregnancy are based on the morphological and physiological adaptation of the human heart to transient preload and afterload changes. The main features are detailed in Table 47.1.
Healthy pregnancy is associated with prolonged cardiac volume overload secondary to increased blood volume that results in a reversible “physiologic” eccentric left ventricular (LV) hypertrophy with the aim of preserving adequate oxygen supply. Starting from as early as 12 weeks of gestation, LV wall thickness increases by about 15–25% to minimize wall stress and maintain myocardial oxygenation; LV wall mass increases by about 50% above pre-pregnancy values mainly during the third trimester (increase in both LV mass and left ventricle mass index). The LV mass increases result from the increased LV end-diastolic and end-systolic diameters (about 12% and 20%, respectively), increased LV posterior wall diastole and systole (about 22% and 13%, respectively) and intraventricular septal thickness during diastole and systole (about 15% and 19%, respectively). Similar to the LV, the right ventricle (RV) increases in size throughout pregnancy because of increased preload. Sphericity index decreases during pregnancy, indicating a more spherical shape of the left chamber towards the third trimester. This physiologic cardiac remodelling resolves in the first weeks postpartum.
4.1.1 Left Atrium
Left atrium acts as a reservoir, a conduit and a booster pump during the cardiac cycle. The left atrium dimensions and function are enhanced gradually in pregnancy, as an adaptive response to increased preload. These changes cause a gradually improved atrial contribution to ventricular filling, so as to maintain adequate LV stroke volume and cardiac output. These findings result in a slightly lower tissue Doppler E velocity and ascended tissue Doppler A wave. The speckle-tracking echocardiography as well shows an improved left atrium reservoir and booster pump function; concerning the conduit function the speckle-tracking echocardiography shows it is decreased. However, all these changes are reversible.
4.1.2 Left Ventricular Function
The data regarding systolic LV function during normal pregnancy are conflicting. The debate is still open whether the LV function deteriorates as a consequence of the physiological changes during pregnancy (comparable to exercise-induced cardiac remodelling) or has no changes or is enhanced in pregnancy. Regarding diastolic function, E wave and A wave are increased, as a result of the over preload and increased blood volume. The E/A ratio and E’/A’ ratio decrease, while the E/E’ remains into normal range.
4.1.3 Right Ventricular Function
There are too few echocardiographic studies that evaluate RV function during normal pregnancy.
5 Hypertensive Disorders
Paradigmatic examples of the utility of echocardiography in pregnancy are the hypertensive disorders. Echocardiography has the potential to categorize patients with gestational hypertension or preeclampsia into high- and low-risk groups. Women with increased LV mass are more likely to have complications. Reduced e’ and therefore elevated E/e’ may be an early predictor of preeclampsia. Echocardiography can also help to identify the small numbers of women with LV systolic dysfunction who are more likely to deteriorate during pregnancy or postpartum. In addiction the use of 3D speckle tracking confirms the known LV remodelling and changes in LV function and allows additional detection of earlier abnormal radial and longitudinal strain values in early preeclampsia compared to late preeclampsia.
6 Valvular Heart Diseases
The main features are detailed in Table 47.2.
7 Congenital Heart Diseases
The main features are detailed in Table 47.3.
Suggested Reading
Castleman JS. Echocardiographic structure and function in hypertensive disorders of pregnancy a systematic review. Circ Cardiovasc Imaging. 2016;9:1–13.
Greutmann M, Pieper PG. Pregnancy in women with congenital heart disease. Eur Heart J. 2015;36:2491–9.
Liu S, et al. Echocardiography in pregnancy: part 1. Curr Cardiol Rep. 2016;18:92.
Melchiorre K, et al. Cardiac structure and function in normal pregnancy. Curr Opin Obstet Gynecol. 2012;24:413–21.
Regitz-Zagrosek V, et al. ESC guidelines on the management of cardiovascular diseases during pregnancy. Eur Heart J. 2011;32:3147–97.
Waksmonski CA. Cardiac imaging and functional assessment in pregnancy. Semin Perinatol. 2014;38:240–4.
Warnes CA. Pregnancy and delivery in women with congenital heart disease. Circ J. 2015;79:1416–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lorini, F.L., Viviani, C. (2019). Obstetric Echocardiography. In: Sarti, A., Lorini, F. (eds) Textbook of Echocardiography for Intensivists and Emergency Physicians. Springer, Cham. https://doi.org/10.1007/978-3-319-99891-6_47
Download citation
DOI: https://doi.org/10.1007/978-3-319-99891-6_47
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99890-9
Online ISBN: 978-3-319-99891-6
eBook Packages: MedicineMedicine (R0)