Abstract
Local anesthetics block nerve conduction via blockade of voltage-gated sodium channels. The physiochemical properties of the individual drugs lead to variability in individual drug potency, onset, and duration. Systemic toxicity can occur via drug overdose, intravenous dosing, or impaired drug elimination. Clinical signs of toxicity can be manifested via the central nervous system and may progress to the cardiovascular system. Treatment of local anesthetic systemic toxicity (LAST) is directed at supportive treatment and administration of lipid emulsion.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Local anesthetics have been utilized for medicinal purposes for thousands of years. More recently, local anesthetics have been utilized in local infiltration, transdermal, intravenous, neuraxial and adjacent to peripheral nerves in an effort to provide analgesia and significantly minimize opioid analgesic administration. While generally well tolerated, a thorough understanding of local anesthetic mechanism of action, pharmacokinetics and pharmacodynamics and potential adverse reactions is required to safely utilize these agents.
Mechanism of Action
Local anesthetics exert an action on a wide range of molecular targets, explaining the effects, both adverse and desirable, observed in various other organ systems. The primary target for local anesthetic effects is the voltage-gated Na+ channel [1,2,3,4]. In neuronal cells, an action potential is produced by the inward flow of Na+ ions through voltage-gated Na+ channels. Na+ channels are present in three states: activated-open, resting-closed, and inactivated-closed. Local anesthetics bind to open and resting Na+ channels and convert them to an inactive-closed state. This prevents the inward passage of Na+ ions, slowing the rate of depolarization and preventing propagation of the action potential that would lead to neuronal excitation and conduction. Frequency-dependent blockade describes the phenomena in which a stimulated nerve is more sensitive to blockade than a resting nerve. This is because more binding sites for local anesthetic become available and drug dissociation is slower when the channel is in an open state.
Properties
The clinical effects of various local anesthetic agents are due, in part, to their physiochemical properties that affect their potency, onset, and duration of effect. These are illustrated in Table 216.1. Other factors such as volume, dosage, drug concentration, site of injection, and vasoconstriction or vasodilation can also impact onset and duration. Lipid solubility, as described by partition coefficient, is positively correlated with potency and facilitates nerve membrane penetration. Bupivacaine, etidocaine, and tetracaine are the most lipid soluble while procaine, prilocaine, and mepivacaine are the least [2,3,4].
Drug onset time is roughly correlated with pKa, or the pH at which ionized and unionized forms of the drug molecule exist in equal amounts. Unionized molecules are more lipid soluble and are able to cross cell membranes. Local anesthetics are weak bases, with pKa values ranging from 7.6 to 8.9 [2, 4]. In general, local anesthetics with a pKa closer to physiologic pH have a greater proportion of molecules in the unionized state and are able to exert a faster onset of action. A higher drug pKa or a more acidic environment leads to a larger proportion of ionized drug molecules that are unable to cross cell membranes to exert a clinical effect. Ion trapping can occur when unionized drug molecules cross a cell membrane, enter a more acidic environment, become ionized, and cannot cross back. Many local anesthetics are preserved in an acidic environment and the addition of sodium bicarbonate to alkalinize local anesthetic solutions may, theoretically, hasten block onset by increasing the unionized drug fraction.
Protein binding is associated with duration of action. Only the unbound fraction of drug molecules are able to exert a clinical effect. In general, agents that are more lipid soluble are more highly protein bound.
Drug Classes
The general chemical structure of a local anesthetic is a lipophilic unit linked to a hydrophilic unit via a hydrocarbon chain. Local anesthetics are classified based on chemical structure of this link into aminoesters and aminoamides [1,2,3,4]. The aminoesters include procaine, chloroprocaine, tetracaine, and cocaine. They are rapidly metabolized via ester hydrolysis by plasma pseudocholinesterase in plasma and the liver. Cocaine is the exception, in which significant hepatic metabolism occurs. P-aminobenzoic acid (PABA) is a metabolite of ester hydrolysis and can cause hypersensitivity reactions. Chloroprocaine has a half life of 45 seconds due to a very fast metabolism and therefore maternal systemic toxicity is rare as almost no drug crosses the placenta.
Aminoamides largely undergo hepatic metabolism by microsomal enzymes. Metabolites are excreted in the urine or bile. The agents of the aminoamide class can be remembered as always having two “I’s” in their names (aminoamides are lidocaine, bupivacaine, etc.).
Toxicity
Systemic toxicity may occur due to overdose, inadvertent intravascular injection, or impaired elimination or biotransformation. Decreased biotransformation can occur in patients with decreased cardiac output and hepatic failure. Pregnant patients are more sensitive to local anesthetics and may exhibit higher plasma concentrations [3]. However, it is common clinical practice to administer epidural boluses of chloroprocaine to pregnant women. This practice is generally not associated with systemic reactions likely due to rapid hydrolysis of aminoester local anesthetics via plasma esterases.
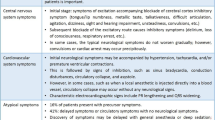
The central nervous system is generally more sensitive to systemic local anesthetics and, therefore, initial clinical signs are associated with the central nervous system. Typically, convulsions, if present, occur at lower doses of bupivacaine relative to levobupivacaine and ropivacaine. Cardiovascular toxicity is due to both direct and indirect effects on the heart and vasculature. Bupivacaine is a unique agent among the local anesthetics and will produce cardiac arrest at lower systemic concentrations than both levobupivacaine and ropivacaine with central nervous system effects often not preceding cardiovascular effects [1,2,3]. In addition, bupivacaine binds strongly to inactive and resting Na + channels for an increased duration relative to other local anesthetics, which may hinder resuscitation efforts.
Risk for central nervous system toxicity is increased with respiratory and metabolic acidosis, and increased cerebral blood flow from hypercapnia and therefore hypoventilation should be avoided. In the event of cardiac arrest following local anesthetic administration, current American Society of Regional Anesthesia (ASRA) advisories recommend decreased doses of epinephrine secondary to evidence that suggests that conventional resuscitation doses impede the efficacy of lipid rescue and recovery from local anesthetic systemic toxicity (LAST) [5].
Clinical Signs of Local Anesthetic Toxicity [1,2,3,4,5]
-
Dizziness.
-
Tinnitus.
-
Muscle fasciculations/tremors.
-
Seizures.
-
Respiratory depression or arrest.
-
Coma.
-
Increased PR interval and duration of QRS complex.
-
Sinus bradycardia or sinus arrest.
Treatment of Local Anesthetic Systemic Toxicity (LAST) [5]
-
Initial focus: Ventilate with 100% oxygen.
-
Hyperventilation-induced respiratory alkalosis reduces local anesthetic ion trapping, decreases cerebral blood flow and increases local anesthetic protein binding.
-
Treatment of seizures: benzodiazepines are preferred; AVOID propofol in patients with cardiovascular instability.
-
-
Management of cardiac arrhythmias.
-
Basic and advanced cardiac life support (ACLS).
-
AVOID vasopressin, calcium channel blockers, beta blockers, and local anesthetic.
-
Vasopressin administration for local anesthetic systemic toxicity is associated with adverse effects in animal models [6].
-
Calcium channel blockers may enhance the negative inotropic effects of local anesthetics and may increase local anesthetic-induced mortality [7].
-
Beta blockers can reduce hepatic metabolism of local anesthetics; lidocaine has been shown to enhance negative inotropic effects of propranolol [7].
-
Reduce individual epinephrine doses to <1 mcg/kg.
-
Evidence demonstrates that epinephrine can reduce the efficacy of lipid emulsion rescue and impair LAST resuscitation efforts [5].
-
-
Lipid emulsion therapy (20%).
-
In patients >70 kg, bolus 100 ml. In patients <70 kg, bolus 1.5 ml/kg (lean body mass) intravenously over 2–3 minutes.
-
In patients >70 kg, initiate a continuous infusion of 200–250 ml over 15–20 minutes. In patients <70 kg, initiate an infusion of 0.25 ml/kg/min.
-
Repeat bolus once or twice and double the infusion rate for persistent cardiovascular collapse.
-
Continue monitoring patient for 4–6 hours following a cardiovascular event or 2 hours following a limited CNS event.
-
Recommended upper limit of 20% lipid emulsion: 12 ml/kg.
-
Allergies and Other Adverse Reactions
Other toxic effects can be associated with the administration of local anesthetics. Parenteral and topical administration of several different local anesthetic agents, particularly prilocaine, benzocaine, and lidocaine, have been implicated in the development of methemoglobinemia. Metabolites of these agents can cause methemoglobinemia via the transformation of hemoglobin iron molecules in such a way that diminishes the ability of oxygen to be bound and released by red blood cells [1, 2].
True allergic reactions to local anesthetic agents are quite rare and are generally more appropriately ascribed to vagal reactions, inadvertent intravascular injections, or reactions to additives (epinephrine) or metabolites. Methylparaben is an additive that is utilized in multi-dose vials to decrease microbial growth. Sulfites are rarely added in dental preparations of local anesthetics to prevent the oxidization of vasopressors. Allergic reactions to both methylparaben and sulfites have been described [1, 2]. Ester local anesthetics are derivatives of ρ-aminobenzoic acid and this may contribute to an increased risk of hypersensitivity reactions [1, 2]. Similarly, hypersensitivity reactions to EDTA present in many local anesthetic solutions have been reported. It is important to carefully examine vial additives in patients presenting with a history of allergic reactions to EDTA. Due to similarities in drug structures, it is also possible for patients with known sulfa allergies to have an increased risk of allergic reaction to methylparaben, sulfites or ester local anesthetics and therefore this should be considered prior to administration. Should a patient report a history of allergic reaction to a local anesthetic of one class, consultation with an allergist may be appropriate to confirm safety of utilization of agents from another class.
Chloroprocaine was historically prepared with sodium bisulfite that was thought to result in neurotoxic reactions. Chloroprocaine was also historically prepared with ethylene glycol-bis-(β-aminoethyl ether)-N, N-tetraacetic acid (EGTA) which was reported to result in muscle spasms [2]. Back pain, paraesthesias, radicular pain and hypoesthesia have been reported following all local anesthetics but are more frequent following intrathecal delivery of lidocaine and mepivacaine. These transient neurologic symptoms (TNS) may also be increased with intraoperative lithotomy positioning and are not associated with neurological deficits [2].
Site of Delivery
The action of local anesthetics can be heavily influenced by their location of injection. Site of injection can greatly impact serum local anesthetic levels with greatest levels being detected after intercostal nerve blocks followed by caudal epidural space, lumbar epidural space, brachial plexus and subcutaneous tissue [2]. With neuraxial administration, baricity can greatly influence the spread of local anesthetics injected into the intrathecal space. Commonly used preparations are isobaric as compared to cerebrospinal fluid and, theoretically, patient positioning does not affect the spread of local anesthetic blockade. Patient positioning does affect neuraxial anesthetic blockade when hyperbaric solutions are used. Hyperbaric solutions are prepared in dextrose and generally travel towards the most dependent position. Hypobaric solutions are prepared in sterile water and have a lower baricity than cerebrospinal fluid and travel against gravity.
High Yield Points
-
Local anesthetics has 2 types, esters and amides.
-
They differ in their metabolism and allergic potential.
-
Local anesthetics in general act by blocking sodium channels.
-
There are several types of local anesthetics which differ in their onset and duration of action.
Questions
-
1.
Appropriate treatment of Local Anesthetic Systemic Toxicity (LAST) includes all of the following except:
-
A.
Lipid emulsion therapy (20%)
-
B.
Basic and advanced life support (ACLC)
-
C.
Decreased dose of epinephrine (<1 mcg/kg)
-
D.
Propofol
-
Answer: D
-
A.
-
2.
Potency of local anesthetics is generally related to:
-
A.
pKa
-
B.
Protein Binding
-
C.
Lipid Solubility
-
D.
Dosage
-
Answer: C
-
A.
-
3.
Local Anesthetics work via blockade of voltage gated Na+ channels. All of the following are true regarding this blockade except:
-
A.
Local anesthetics bind to voltage gated Na+ channels on the external surface of axons
-
B.
Frequency dependent blockade results in faster block onset times with active nerve firing
-
C.
Local anesthetics bind to voltage gated Na+ channels in their open and resting configurations
-
D.
Blockage of voltage gated Na+ channels slowing the rate of axonal depolarization and prevents propagation of action potentials
-
Answer: A
-
A.
References
Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog. 2012;59(2):90–102.
Berde CB, Strichartz GR. Local anesthetics. In: Miller RD, Cohen NH, Eriksson LI, et al., editors. Miller’s anesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2015. p. 1028–55.
French J, Sharp LM. Peri-operative care series: local anaesthetics. Ann R Coll Surg Engl. 2012;94:76–80.
Lirk P, Picardi S, Hollna MW. Local anaesthetics: 10 essentials. Eur J Anaesthesiol. 2014;31:575–85.
Neal JM, Woodward CM, Harrison TK. American society of regional anesthesia and pain management checklist for managing local anesthetic systemic toxicity: 2017 version. Reg Anesth Pain Med. 2018;43:150–53. Also available at asra.com
Dr Gregorio G, Schwartz D, Ripper R, et al. Lipid emulsion is superior to vasopressin in a rodent model of resuscitation from toxin-induced cardiac arrest. Crit Care Med. 2009;37(3):993–9.
Neguib M, Magboul MM, Samarkandi AH, Attia M. Adverse effects and drug interactions associated with local and regional anaesthesia. Drug Saf. 1998;18(4):221–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Schroeder, C., Schroeder, K. (2019). Local Anesthetics. In: Abd-Elsayed, A. (eds) Pain. Springer, Cham. https://doi.org/10.1007/978-3-319-99124-5_216
Download citation
DOI: https://doi.org/10.1007/978-3-319-99124-5_216
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99123-8
Online ISBN: 978-3-319-99124-5
eBook Packages: MedicineMedicine (R0)