Abstract
Damage or loss of corneal and/or limbal cells from injury or infection can lead to irreversible loss of corneal transparency and blindness. A population of active limbal stem cells has been identified in the limbal epithelial crypts that provide a continuous supply of progenitors and mature epithelial cells, and participate in wound healing. With our growing knowledge of this stem cell population, our understanding of the homeostatic mechanisms regulating corneal epithelial homeostasis has expanded dramatically. Loss of these limbal stem cells leads to the range of conditions representing limbal stem cell deficiency. Here, we review the biology and cellular characterization of the limbal stem cell in health and disease. We also review clinical approaches to ocular surface stem cell transplantation that have been developed over the last 30 years, including autograft and allograft techniques currently in clinical practice, and the challenges associated with systemic immunosuppression when required. Emerging therapies in cultivated limbal epithelial transplantation are described, which may provide an unlimited source of cells for ocular surface restoration.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
The cornea is a transparent tissue which transmits and refracts light, to allow a focus image to be projected onto the retina. The average human cornea is about 500 μm thick centrally and near 1000 μm thick peripherally [1]. It consists of five cellular layers : an outer epithelial layer, Bowman’s layer, a middle stroma composed of hydrated collagenous extracellular matrix, Descemet’s layer of basement membrane, and an inner endothelial monolayer. The surface epithelium is composed of stratified non-keratinized cells, with a thickness of approximately 50 μm. A number of antimicrobial and anti-inflammatory factors are secreted by the epithelium within an insoluble mucous layer that aids in maintaining a stable ocular surface tear film [2]. The corneal stroma is composed of over 300 lamellae of type I collagen interspersed with glycosaminoglycans; it resembles a hydrogel, with 80% water by weight. The stoma is maintained by the resident population of fibroblast-like keratocytes. This network gives the cornea its strength, and the lamellation provides transparency. The endothelial monolayer is the functional layer essential for maintaining appropriate water balance in the corneal stroma, and hence transparency. It contains sodium/potassium ATPase membrane pumps that maintain an osmotic balance to drive aqueous humor between the stroma and anterior chamber. Regarding the surface epithelium , as cells are lost, the basal layer proliferates to replace these superficial cells [3]. These basal cells are replaced by a population of stem cells that reside within the limbus, found at the corneoscleral junction. These limbal stem cells (LSCs) are important for the proper maintenance and regeneration of the corneal epithelium [4, 5].
Any irreversible damage or loss of corneal and/or limbal cells, from injury or infection, can lead to loss of corneal transparency and blindness. A World Health Organization study shows that corneal disease is second only to cataracts as the leading cause of blindness worldwide [6]. Corneal ulcers and ocular surface trauma are estimated to account for an incidence of 1.5–2 million case of blindness annually, with a prevalence of 10 million.
The management of corneal disease has changed dramatically in the last 40 years. In the 1970s, all patients with corneal disease had a poor visual prognosis. The only available techniques included penetrating and lamellar keratoplasty to replace the corneal tissue, and tarsorrhaphy and artificial tears to maintain surface hydration.
A full-thickness corneal transplantation with a cadaveric allograft, known as a penetrating keratoplasty (PKP) , can be used to replace the entire cornea. While PKP is successful in the short term, varying rates of rejection have been reported up to 15% in some studies [7]. This can lead to graft failure, with loss of the endothelial cells and subsequent loss of corneal transparency from edema. Graft failure rates are greater in high-risk transplantation populations. These include those patients with autoimmune disease , chemical alkali burns , severe dry eye , Stevens-Johnson syndrome (SJS) , ocular cicatricial pemphigoid (OCP) , neurotrophic cornea from herpetic eye disease (zoster and/or simplex), and in those who have had recurrent grafts [8]. This often results in the eye not being able to support a corneal transplant. Deep anterior lamellar keratoplasty (DALK) is an alternative procedure, involving removal of only the epithelium and stroma, leaving the endothelium intact. This reduces the rates of rejection and postoperative complications such as leakage, and improves graft stability [9]. It also results in reduced loss of endothelial cells postoperatively compared to PKP.
Importantly, there is also a severe shortage of donor corneal tissue worldwide, as is the case in other solid organ transplantations. With an aging population, wait times for donor tissue are expected to increase. As well, suitable donor tissue may be more limited with the increased incidence of infectious diseases including HIV and hepatitis. The development of artificial corneal replacements , or keratoprostheses (KPro) , has helped to decrease our dependence on donor tissue [10]. In the developing and under-developed world, the skills and resources to perform these surgeries are extremely limited [11].
Modern-day treatment has evolved significantly. In this chapter, we will focus on the surgical methods that ophthalmologists have developed to restore the ocular surface, in the context of diseases of limbal stem cell deficiency. Special note will be made to the importance of immunomodulatory therapy in the context of limbal tissue allografts. We will also provide perspective on new and emerging methods of ocular surface stem cell therapy.
7.2 Limbal Stem Cells and the Niche
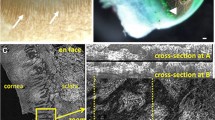
The corneal epithelium is constantly being sloughed and renewed by a regular homeostatic mechanism. The renewal process involves centripetal and circumferential migration from the limbus in addition to vertical migration from basal layers [12, 13]. Davanger and Evensen [4] were first to recognize that pigmented limbal cells seemed to move centrally in the cornea, suggesting centripetal migration. From this observation, they hypothesized that limbal cells were likely involved in normal corneal epithelial renewal. They postulated that these source-cells were resident in the limbal crypts of the palisades of Vogt, a series of radially oriented fibrovascular ridges that are observed in the human limbus [14, 15], and can be imaged by optical coherence tomography with sub-micrometer resolution [16].
It was Schermer and colleagues [5] who postulated that corneal epithelial stem cells were located in the limbus. They based their theory on the pattern of expression of cornea-specific 64K keratin present in all corneal epithelial cells except the limbal basal cells, suggesting that the limbal basal cells were less differentiated than those found in other areas of the corneal epithelium. This is true of basal cells in skin epidermis [17], as well as mucosal epithelium in the intestine [18].
Stem cells are characterized by two cardinal properties: self-renewal and multipotentiality . In self-renewal by asymmetric division, one daughter cell remains a stem cell while the other becomes a more differentiated progenitor. Multipotentiality refers to the potential for tissue-specific stem cell progeny to differentiate into any of the mature cell types that make up that adult tissue. Cell kinetic studies in intestine and epidermis have shown that stem cells and their early progeny, the transit amplifying cells (TACs) , make up the proliferating cells of epithelium [19, 20]. Schermer and colleagues [5] proposed the cell proliferation scheme for the cornea as proceeding to limbal basal stem cells, to basal corneal epithelial TACs, to differentiating suprabasal corneal epithelium (Fig. 7.1). In 2005, based on histological examination of the human limbus, Dua et al. reported the presence of limbal epithelial crypts (LECs) and proposed that they also harbor LSCs [21]. LECs are more frequently detected in the superior or inferior limbus compared to temporal or nasal limbus [22, 23]. In nonhuman species, only porcine limbus has been reported to share the structure of the human limbus regarding the topography of the palisades of Vogt and LEC, while no evidence of palisades of Vogt has been found in other animals [22].
(a) Location of the limbus, at the junction of the conjunctival and corneal epithelium. (b) LSCs resident in the epithelial crypts of the palisades of Vogt give rise to transit amplifying cells (TACs) , which migrate towards the center of the cornea, before differentiating and migrating towards the superficial layers of the epithelium as terminally differentiated suprabasal epithelial cells (Reproduced with permission, Notara and colleagues, 2008)
In mice, LSCs were first identified as slow-cycling label-retaining cells in the basal layer of the limbal epithelium [24]. Despite lacking palisade of Vogt structures, lineage-tracing studies clearly show that murine corneal stem cells exist in the limbus and are capable of producing daughter cells with centripetal migration patterns during corneal epithelial regeneration [25,26,27,28].
As a result of their high proliferative potential and their absence of markers, a decades-long search has been underway for a bona fide LSC marker that would enable prospective isolation for therapeutic applications. Numerous potential LSC markers have been proposed [29], but for most, evidence for successful prospective enrichment of cells capable of long-term corneal restoration is currently lacking. Pellegrini and colleagues proposed that transcription factor p63 identifies human LSCs [30], and Rama and colleagues [31] evaluated the effectiveness of autologous limbal cell transplants grafted onto patients with unilateral limbal stem cell deficiency. The success of the transplants seemed to depend on the number of p63+ cells in the graft. Several additional potential human LSC markers have been identified, including Lgr5 [32], Tcf4 [33], CD157 [34], CD71low/Integrin-alpha6high [35], TrkA [36], N-cadherin [35], ABCG2 [37, 38], Cytokeratin15 [39], and ABCB5 [40]. In the case of ABCB5, prospectively isolated human ABCB5+ LSC possessed the capacity to fully restore corneal epithelium after grafting onto LSC-deficient mice. ABCB5 was found to be preferentially expressed on label-retaining cells at the limbus in mice. Furthermore, ABCB5+ cells were significantly depleted in patients with LSC deficiency. ABCB5 loss-of-function mutant mice showed defective corneal differentiation and wound healing, demonstrating that ABCB5 is both a marker and also of functional significance in maintaining LSCs.
Of note, due to the complexity of the LSC niche and the elusiveness of definitive LSC identification, the developmental origin of the LSC has remained elusive. Our current understanding of the developmental origins and formation of the corneo-limbal-scleral junction is reviewed in detail elsewhere [29].
7.3 Limbal Stem Cell Deficiency
Limbal stem cell deficiency (LSCD), caused by inherited, or acquired disruption of this stem cell niche , results in poor corneal epithelialization and epithelial defects, secondary vascularization of the cornea, stromal scarring, and/or corneal conjunctivalization [41]. Etiologies include chemical or thermal burns; ocular cicatricial pemphigoid (OCP) and pseudo-OCP; aniridia; various forms of ectodermal dysplasia ; Stevens-Johnson syndrome ; contact lens wear-related; or iatrogenic injury during ocular surface surgery. These conditions may result in partial or total limbal stem cell deficiency in the affected eye because of the degree of destruction of the limbus, conjunctival scarring, decreased tear film production, and the high risk of corneal keratinization. The patient will experience a number of distressing symptoms including ocular pain, photophobia, and decreased vision (Fig. 7.2).
Eyes with severe LSC resulting from (a) acid burn; (b) Stevens–Johnson syndrome ; (c) alkali burn; (d) Contact lens wear-related severe LSCD. Total conjunctivalized corneal surface with stromal haze, and large infiltrating vessels from the conjunctiva are seen. (e) Fluorescein staining of the cornea, viewed under cobalt-blue illumination, reveals the classic late-staining pattern with a whorl-like epitheliopathy pattern, demonstrating severe LSCD (a–c, Reproduced with permission, Lavker and colleagues, 2004; d, e, Reproduced with permission, Chan and Holland, 2013)
When a significant number of limbal stem cells are lost, conjunctival epithelial cells invade and populate the corneal surface. This process of conjunctivalization results in a thickened, irregular, unstable epithelium, often with secondary neovascularization, inflammatory cell infiltration and disruption of the basement membrane [42]. Impression cytology typically demonstrates the presence of goblet cells and conjunctival epithelial cells on the corneal surface [41]. Punctate corneal epithelial defects and larger confluent defects are common and can lead to corneal scarring . Debridement of the conjunctivalized pannus results in a reinvasion of the abnormal epithelium. A PKP or lamellar keratoplasty with normal epithelium results in a stable ocular surface as long as the donor epithelium is present. However, with eventual epithelial sloughing, the surface often fails, resulting in re-conjunctivalization owing to continued LSCD [43]. Donor epithelium in routine PKP may survive for several months without the need for re-epithelialization from the limbus. This survival time is known, from studies that observed epithelial rejection as late as 13 months postoperatively [44]. The observation that stable corneal re-epithelialization was not possible without a healthy limbal zone led ophthalmologist to begin investigating approaches to epithelial transplantation.
7.4 Clinical Approaches to Ocular Surface Stem Cell Transplantation
Over the last three decades, the field has seen a remarkable proliferation and variation in the techniques of ocular surface stem cell transplantation (OSST) [45], often combined with PK or deep lamellar keratoplasty (DLK) . In unilateral LSCD, tissue harvested from the contralateral eye may be used in an autograft [46,47,48]. In bilateral disease, which is more common, allogeneic donor material must be used [49,50,51,52,53]. Holland and Schwartz proposed a nomenclature and classification system [54] for ocular surface stem cell transplantation; we will use this system here (Table 7.1).
7.4.1 Autografts
Epithelial transplantation can be divided into autografts and allografts. In traditional autografts, the donor tissue is obtained from the fellow eye, thereby avoiding the major problem of immunologic rejection that faces allograft procedures. Some newer techniques involve harvesting autograft tissue from an area of healthy limbus in the same eye. Epithelial transplantation for severe ocular surface disease was first described by Thoft in 1977 [56], when he described conjunctival transplantation for monocular chemical burns. This was an autograft procedure using several pieces of bulbar donor conjunctiva harvested from a normal fellow eye. In 3/5 eyes, the cornea was successfully re-epithelialized, and this procedure was based on the concept of conjunctival transdifferentiation [20, 57, 58]. Studies have subsequently shown that the conjunctiva cannot transdifferentiate into epithelium that is truly phenotypical corneal epithelium [59].
Kenyon and Tseng [47] were the first to specifically transplant limbal stem cells in a conjunctival-limbal autograft (CLAU) from the contralateral eye. In this procedure, conjunctiva and limbus from a normal fellow eye were used to manage diffuse LSCD in unilateral disease, or focal limbal deficiency in unilateral or bilateral disease. The harvest of bulbar conjunctiva extended 0.5 mm onto the clear corneal surface, thus containing limbal cells. The preoperative diagnoses included chemical and thermal injuries, contact lens-induced keratopathy , and surface disease secondary to multiple ocular surface surgeries. This resulted in rapid surface healing, improved ocular surface, and improved visual acuity.
Jenkins and colleagues [60] reported on CLAU in five patients with epitheliopathy secondary to chronic contact lens overuse. Two of five procedures failed, and one of the fellow donor eyes developed LSCD post-harvest. These results stress the importance of careful selection of donor tissue for autografting only from a fellow eye that is otherwise normal. It is likely that these fellow donor eyes were not normal given their exposure to chronic contact lens wear, even though they did not show overt LSCD. CLAU should only be obtained from eyes with normal, functional epithelial surfaces.
7.4.2 Allografts
While autografting is a very successful procedure used today for unilateral LSCD, it does not provide a therapeutic approach to severe bilateral LSCD. Thoft described the first allograft procedure in 1984 [61] which he named keratoepithelioplasty. His procedure involved the use of “lenticules” of peripheral cornea from a cadaveric donor eye. These lenticules were harvested from the midperipheral cornea and consisted of cornea and a thin layer of stroma. They were placed evenly around the corneoscleral limbus of the host eye and sutured to the sclera. The limbus was not harvested from donor eyes in this procedure. The donor epithelium spread from the lenticules and covered the host cornea. Three of four patients transplanted in his study maintained a stable ocular surface and improved vision. Turgeon and colleagues [62] expanded on this procedure to include limbal tissue with the peripheral cornea in order to capture LSCs in the allografts.
It was not until the mid-1990s that groups described the first keratolimbal allograft (KLAL) transplantations [63, 64]. They utilized a whole globe to make a 360° scleral incision approximately 1 mm from the limbus at the same depth as a midperipheral corneal incision. Lamellar dissection of the keratolimbal tissue was performed, the keratolimbal ring was divided into three pieces, and transferred to the recipient eye. All patients were placed on systemic cyclosporine A (CsA) in addition to topical corticosteroid drops. Systemic CsA was tapered as possible. Of six patients with LSCD , five of six had improved vision resulting from the procedure. Tsubota and colleagues [64] showed that the corneolimbal tissue could be kept in storage media for 5 days prior to transplantation.
Given the concern regarding immunologic rejection in the context of limbal allografts, and the growing understanding from other fields of solid organ transplantation (e.g., kidney) of the importance of donor-host immunomatching, various groups began to explore the use of living-related donors as a source of allograft tissue. The first report of a living-related epithelial transplantation was by Kwitko and colleagues in 1995 [65], which they called “allograft conjunctival transplantation .” Limbal tissue was not transplanted in this study. Donor conjunctiva was obtained from siblings or parents. Human leukocyte antigen (HLA) typing and crossmatching was performed retrospectively in recipients/donors. Three of 12 eyes experienced epithelial rejection episodes, with no disturbance of the corneal surface in two patients. Two of these three cases had 100% incompatible HLA matching. Patients with identical or haplo-identical matching were less likely to undergo epithelial rejection. It is interesting to note that while 5/11 eyes had improved visual acuity and 10/11 eyes had improved ocular surface (transparency, decreased neovascularization, stable epithelium), these results were obtained with only transplantation of conjunctival tissue, without limbal tissue.
Kenyon and Rapoza [66] were the first to describe living-related limbal allografting with a conjunctival carrier from a living-donor (living-related conjunctival limbal allograft, lr-CLAL ). This was similar to the technique of limbal autografting (CLAU) , except that the donor tissue was derived from a living relative. Most patients also went simultaneous lateral tarsorrhaphy. Topical steroid drops were included in all cases, with topical and/or systemic CsA for HLA haplo-identical or incompatible cases. No episodes of rejection were observed in eight cases. The ocular surface remained stable in six of eight cases. Visual acuity also improved in six of eight cases.
Since this time, there have been numerous modifications and combinations of the techniques described above. For example, a “Cincinnati procedure ” has been described, which uses a combined lr-CLAL and KLAL in patients with bilateral severe LSCD and conjunctival deficiency [67]. A modified Cincinnati procedure involves a combined CLAU and KLAL for patients with severe unilateral LSCD [68] (Fig. 7.3).
The Cincinnati procedure for combined lr-CLAL/KLAL: (a) The conjunctival graft is harvested from the living-related donor eye in the 12- and 6-o’clock meridians. (b) The recipient eye is prepared by performing a 360° limbal peritomy and undermining/retracting conjunctival tissue, followed by (c) removal of abnormal corneal epithelium and fibrovascular pannus. (d) The harvested living-related tissue is sutured in the same anatomical orientation, with the (e) cadaveric donor segments placed at the 3- and 9-o’clock meridians also in the same anatomical orientation with the limbal edge at the recipient limbus. The modified Cincinnati procedure for combined Fig. 7.3 (continued) CLAU/KLAL: (f) CLAUs are harvested from the fellow eye while (g) KLAL segments are prepared from a cadaveric donor corneoscleral rim. (h) 360° conjunctival peritomy and removal of abnormal epithelium and fibrovascular pannus is performed. (i) CLAU and (j) KLAL segments are secured at the limbus of the recipient eye (a–e, Reproduced with permission, Biber and colleagues, 2011 [67]; f–j, Reproduced with permission, Chan and colleagues [68])
7.4.3 Rejection and Systemic Immunosuppression in Limbal Allografts
Systemic immunosuppression is critical for graft integration and survival following allograft transplantation [69]. Limbal allografts are at significantly higher risk of rejection than other more “central” corneal procedures involving the avascular stroma. In corneal transplantation, an avascular tissue is being transplanted into an avascular host site. In contrast, the limbus has a high concentration of tissue antigen presenting cells (Langerhans’ cells ), which can trigger immunologic rejection [70] by T-cells [71]. This may present as either acute allograft rejection with injection at the graft-host junction and conjunctivalization of the ocular surface, or a chronic rejection characterized by slowly progressive conjunctivalization without evidence of acute inflammation [72]. It should be noted that the role of humoral immunity is not well defined in the context of the limbal allografts. The graft-host state in limbal transplantation must therefore be treated similarly to most cases of vascular solid organ transplants.
Thoft and Sugar [73] gave us the description of the typical features of patients with acute rejection following KLAL. However, with chronic features (irregular epithelium, recurrent LSCD, epithelial failure) it can be difficult to differentiate between chronic low-grade disease or failure of the transplanted graft. In the case of limbal allografts, there is perpetuation of donor epithelial cells and antigen presenting cells beyond the first year [71], and thus the threat of graft rejection persists. Therefore, long-term systemic immunosuppression is extremely important.
The options to treat bilateral LSCD include KLAL, lr-CLAL, and ex-vivo cultured stem cell transplantation. The early allograft protocols used systemic CsA almost exclusively for long-term immunosuppression [52, 53, 74,75,76,77,78,79], occasionally with the addition of azathioprine [80]. Long-term CsA therapy can have a number of systemic side effects, including nephrotoxicity [81], hypertension [82, 83], and hyperlipidemia [84]. Patient monitoring on CsA includes regular blood trough levels, as well as trends in blood pressure and creatinine. After 2000, these studies often used short-term courses of high-dose steroids in the postoperative phase, and also in induction protocols preoperatively [16, 25, 27,28,29,30,31, 33,34,35]. Early corticosteroid withdrawal has been shown to decrease corticosteroid-related morbidity in patients receiving solid organ transplants [85]. Steroid-sparing immunosuppression protocols in kidney transplantation, with discontinuation of steroids as early as 1 week postoperatively, have been studied in prospective trials [86].
The modern immunosuppressive protocols target stages of the immune response to tailor postoperative medical therapy [45]. Both MMF and azathioprine can affect bone marrow functioning, and require regular monitoring. However, in other organs, MMF has been shown to decrease the incidence of acute transplant rejection over azathioprine, in patients also on steroids and CsA [87]. Due to these reasons, the use of MMF has generally replaced azathioprine in OSST post-transplantation immunosuppression. It should be noted that MMF can be teratogenic, and thus all women of childbearing age should be discouraged from pregnancy during therapy.
One example of the progression from CsA-based long-term immunosuppression to next-generation immunosuppressive protocols is the OSST program at The Cincinnati Eye Institute. Their program began with the use of CsA, azathioprine, and prednisone [80], but in the last 10 years, has moved to a regime including long-term tacrolimus and MMF, in addition to a short-term oral prednisone taper [69]. This protocol is based on the success achieved by the ELITE-Symphony randomized control study in renal transplantation [88] showing an ability to reduce exposure to calcineurin inhibitors using low-dose tacrolimus. Tacrolimus and MMF together has been shown to be more effective and safer than CsA in renal transplantation by reducing acute rejection [89], and decreased risk in high-risk PK [90]. While tacrolimus , like CsA, is a calcineurin inhibitor, the adverse effects of hirsuitism and gingival hyperplasia are eliminated [91], increasing patient tolerance and adherence to therapy. Some groups taper tacrolimus beginning 1–2 years postoperatively if the ocular surface has been stable [69]. Morbidity in OSST patients is much lower than that seen in renal transplantation patients [92], likely because of the increased preponderance of comorbidities in patients with end-stage renal disease.
For allografts, important preoperative assessment of risk includes blood group type (ABO), donor type (KLAL vs. lr-CLAL), tissue HLA type, panel reactive antibody (PRA) , and donor-specific HLA antibody (DSA) identification . ABO blood group antigens have been detected on human corneal epithelial cells, and may contribute to allograft rejection once the rejection response has begun [93]. HLA-A/B/C antigens can be found on corneal epithelium and stromal keratinocytes, while HLA-DR/DQ/DP are present on Langerhans and other antigen presenting cells [94]. The protocols for preoperative risk assessment are generally based on experience with solid organ transplantation and our understanding of transplant rejection immunobiology. Drugs have been developed which target the cell-mediated immune responses specifically that can contribute to graft rejection, including IL-2 receptor blockers such as basiliximab. Holland and colleagues [69] have used preoperative induction with basiliximab in patients receiving lr-CLAL without a perfect HLA match and a nonzero PRA. In addition, they use basiliximab in patients receiving KLAL with a nonzero PRA. In high-risk patients, undergoing KLAL, lr-CLAL with non-HLA identical, HLA-identical/PRA >50%, or any patient undergoing repeat OSST, initiation of maintenance therapy (MMF/tacrolimus) occurs 2 weeks prior to surgery. Overall, the absence of comprehensive histocompatibility data in limbal transplants represents a significant gap in the understanding of rejection processes.
Given the concerns around donor-host matching and long-term systemic immunosuppression, the opportunity to avoid these issues by performing an autograft in the case of unilateral disease is tempting [95]. As mentioned previously, a very careful evaluation must be undertaken as, in many cases, the “normal” fellow eye may have subclinical LSCD. In this case, the host eye may fail to re-epithelialize because of deficiency inherent in the graft, and the donor eye would be left without sufficient limbal stem cell capacity to maintain surface integrity [60].
The balance of evidence suggests that long-term immunosuppression may be important to graft success, but more prospective and/or randomized trials are required to determine the optimal therapeutic approach and to compare immunosuppressive practices. There is currently no consensus on which regimen is most efficacious for various pathologies or grafts. It would also be advantageous to assess the results of larger numbers of patients with a common approach across multiple centers.
7.5 Cultivated Limbal Epithelial Transplantation
In the mid-1990s, Pellegrini and colleagues [96] described a procedure using autologous cultivated corneal epithelium to restore the ocular surface . Sheets of corneal epithelial cells were cultured in vitro, and these sheets were transplanted to the injured eye. This procedure was particularly effective for patients who are resistant to the idea of using six clock hours of limbal tissue from their healthy eye as a donor source for CLAU grafting into their blind eye [45]. The patients retained a stable ocular surface without systemic immunosuppression for >2 years after the procedure. In the interim, multiple studies have investigated the molecular genetic mechanisms regulating limbal stem cell self-renewal and differentiation potential in vivo [30, 40, 97], and their ability to be grown as holoclones in vitro [98]. For success in this approach, adequate numbers of autologous stem cells will need to be generated prior to transplantation [31]. However, this approach is still limited: it cannot be applied to patients suffering from total bilateral LSCD, because these patients lack the autologous limbal stem cells necessary for culture. As well, the cost of establishing and maintaining a stem cell laboratory for cGMP cell therapy production is very high [99], and may result in CLET only being available in a handful of advanced centers worldwide. Some regional CLET facilities are being established in Europe, which may serve multiple transplant sites across the region. The reader is directed to an excellent review of cultivated epithelial sources for transplant provided in Chap. 6.
With the advent of induced pluripotent stem (iPS) cells [100,101,102] with the same properties as bona fide embryonic stem (ES) cells, it may be possible to use a patient’s autologous somatic cells (e.g., fibroblasts from a skin biopsy) to generate epithelial stem cells. Early studies have already shown the potential of iPS cells to generate corneal epithelium [103]. These findings could result in autologous limbal grafts event for patients with bilateral total LSCD, once safety and proper regulation of iPS cell generation has been established.
7.6 Simple Limbal Epithelial Transplantation
It had been recognized that CLAU proposed some perceived risk to the donor eye of limbal decompensation. Tseng and colleagues, who pioneered the original CLAU technique [47], even developed a smaller single two-clock-hour donor tissue harvest, aimed at minimizing the amount of donor tissue used to treat total LSCD in the fellow eye: they termed this technique mini-CLAU [104].
Another technique aimed at reducing the amount of tissue harvested from donors is the simple limbal epithelial transplantation (SLET) technique . This involves a resection of one clock hour of limbal tissue from the donor eye, division into small pieces, and transplantation of these autografts on an amniotic membrane placed over the recipient cornea [105] (Fig. 7.4). This technique does not require the cell culture facilities required for ex vivo donor cell expansion that is necessary for cultivated limbal epithelial transplantation (CLET). SLET incorporates the advantages of CLAU by being a single-stage autograft procedure. Like CLET, it also minimizes the risk of precipitating LSCD in the donor eye as only one clock hour is harvested., but minimizes donor tissue.
Simple limbal epithelial transplantation (SLET) : (a) 2 × 2 mm area of limbus is marked in the donor eye; (b) a subconjunctival dissection 1 mm into clear cornea allows (c) excision of the donor tissue; (d, e) a peritomy is performed and fibrovascular pannus and irregular epithelium is removed from the recipient corneal surface; (f) a human amniotic membrane graft is placed on the bare ocular surface and secured with fibrin glue; (g, h) the donor limbal tissue is cut into 8–10 small pieces and secured to the surface of the amniotic membrane with fibrin glue (Reproduced with permission, Sangwan and colleagues [105])
7.7 Conclusions and Outlook
Important clinical advances have been made in the techniques used to treat patients suffering from partial and total limbal stem cell deficiency. Our growing understanding of the role of the limbal stem cell in normal corneal epithelial homeostasis and disease has led to the refinement of procedures for limbal allografting and autografting, as well as important discoveries that may lead to the widespread use of cultivated limbal epithelial transplants. The use of in vitro cultivated cells may eventually supplant our need for donor corneal tissue in the treatment of LSCD. The possibility of targeted stimulation of endogenous stem cell stimulation to effect repair of diseased ocular tissue, without the need for cell transplantation, constitutes the ultimate goal of regenerative medicine in the eye. The ability to unlock this potential with LSCs in the context of ocular surface disease will depend on a deeper understanding of the stem cell biology underlying the regulation of LSC proliferation and differentiation under physiologic and pathophysiologic conditions. Advances in drug delivery and bioengineering may contribute to spatial and temporal control of LSC kinetics and dynamics in situ. Notwithstanding these challenges, the promise of regenerative medicine for ocular surface therapy can build on the success recognized in other tissues, to further advance future clinical application.
References
Jonas, J. B., & Holbach, L. (2005). Central corneal thickness and thickness of the lamina cribrosa in human eyes. Investigative Ophthalmology & Visual Science, 46, 1275–1279.
Sack, R. A., Nunes, I., Beaton, A., & Morris, C. (2001). Host-defense mechanism of the ocular surfaces. Bioscience Reports, 21, 463–480.
Ren, H., & Wilson, G. (1996). The cell shedding rate of the corneal epithelium—A comparison of collection methods. Current Eye Research, 15, 1054–1059.
Davanger, M., & Evensen, A. (1971). Role of the pericorneal papillary structure in renewal of corneal epithelium. Nature, 229, 560–561.
Schermer, A., Galvin, S., & Sun, T. T. (1986). Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. The Journal of Cell Biology, 103, 49–62.
Whitcher, J. P., Srinivasan, M., & Upadhyay, M. P. (2001). Corneal blindness: A global perspective. Bulletin of the World Health Organization, 79, 214–221.
Claesson, M., Armitage, W. J., Fagerholm, P., & Stenevi, U. (2002). Visual outcome in corneal grafts: A preliminary analysis of the Swedish Corneal Transplant Register. The British Journal of Ophthalmology, 86, 174–180.
Williams, K. A., et al. (2006). How effective is penetrating corneal transplantation? Factors influencing long-term outcome in multivariate analysis. Transplantation, 81, 896–901.
Ardjomand, N., et al. (2007). Lamellar corneal dissection for visualization of the anterior chamber before triple procedure. Eye (London, England), 21, 1151–1154.
Myung, D., et al. (2008). Development of hydrogel-based keratoprostheses: A materials perspective. Biotechnology Progress, 24, 735–741.
Chirila, T. V. (2001). An overview of the development of artificial corneas with porous skirts and the use of PHEMA for such an application. Biomaterials, 22, 3311–3317.
Thoft, R. A., & Friend, J. (1983). The X, Y, Z hypothesis of corneal epithelial maintenance. Investigative Ophthalmology & Visual Science, 24, 1442–1443.
Yoon, J. J., Ismail, S., & Sherwin, T. (2014). Limbal stem cells: Central concepts of corneal epithelial homeostasis. World Journal of Stem Cells, 6, 391–403.
Goldberg, M. F., & Bron, A. J. (1982). Limbal palisades of Vogt. Transactions of the American Ophthalmological Society, 80, 155–171.
Townsend, W. M. (1991). The limbal palisades of Vogt. Transactions of the American Ophthalmological Society, 89, 721–756.
Bizheva, K., et al. (2017). In-vivo imaging of the palisades of Vogt and the limbal crypts with sub-micrometer axial resolution optical coherence tomography. Biomedical Optics Express, 8, 4141–4151.
Potten, C. S., & Loeffler, M. (1987). Epidermal cell proliferation. I. Changes with time in the proportion of isolated, paired and clustered labelled cells in sheets of murine epidermis. Virchows Archives B, Cell Pathology, 53, 279–285.
Potten, C. S., & Loeffler, M. (1987). A comprehensive model of the crypts of the small intestine of the mouse provides insight into the mechanisms of cell migration and the proliferation hierarchy. Journal of Theoretical Biology, 127, 381–391.
Lajtha, L. G. (1979). Stem cell concepts. Differentiation, 14, 23–34.
Kinoshita, S., Friend, J., & Thoft, R. A. (1983). Biphasic cell proliferation in transdifferentiation of conjunctival to corneal epithelium in rabbits. Investigative Ophthalmology & Visual Science, 24, 1008–1014.
Dua, H. S., Shanmuganathan, V. A., Powell-Richards, A. O., Tighe, P. J., & Joseph, A. (2005). Limbal epithelial crypts: A novel anatomical structure and a putative limbal stem cell niche. The British Journal of Ophthalmology, 89, 529–532.
Grieve, K., et al. (2015). Three-dimensional structure of the mammalian limbal stem cell niche. Experimental Eye Research, 140, 75–84.
Pajoohesh-Ganji, A., Pal-Ghosh, S., Simmens, S. J., & Stepp, M. A. (2006). Integrins in slow-cycling corneal epithelial cells at the limbus in the mouse. Stem Cells, 24, 1075–1086.
Cotsarelis, G., Cheng, S. Z., Dong, G., Sun, T. T., & Lavker, R. M. (1989). Existence of slow-cycling limbal epithelial basal cells that can be preferentially stimulated to proliferate: Implications on epithelial stem cells. Cell, 57, 201–209.
Amitai-Lange, A., et al. (2015). Lineage tracing of stem and progenitor cells of the murine corneal epithelium. Stem Cells, 33, 230–239.
Di Girolamo, N., et al. (2015). Tracing the fate of limbal epithelial progenitor cells in the murine cornea. Stem Cells, 33, 157–169.
Dorà, N. J., Hill, R. E., Collinson, J. M., & West, J. D. (2015). Lineage tracing in the adult mouse corneal epithelium supports the limbal epithelial stem cell hypothesis with intermittent periods of stem cell quiescence. Stem Cell Research, 15, 665–677.
Lobo, E. P., et al. (2016). Self-organized centripetal movement of corneal epithelium in the absence of external cues. Nature Communications, 7, 12388.
Gonzalez, G., Sasamoto, Y., Ksander, B. R., Frank, M. H., & Frank, N. Y. (2017). Limbal stem cells: Identity, developmental origin, and therapeutic potential. Wiley Interdisciplinary Reviews: Developmental Biology, 2, PMID:29105366.
Pellegrini, G., et al. (2001). p63 identifies keratinocyte stem cells. Proceedings of the National Academy of Sciences of the United States of America, 98, 3156–3161.
Rama, P., et al. (2010). Limbal stem-cell therapy and long-term corneal regeneration. The New England Journal of Medicine, 363, 147–155.
Brzeszczynska, J., Ramaesh, K., Dhillon, B., & Ross, J. A. (2012). Molecular profile of organ culture-stored corneal epithelium: LGR5 is a potential new phenotypic marker of residual human corneal limbal epithelial stem cells. International Journal of Molecular Medicine, 29, 871–876.
Lu, R., et al. (2012). Transcription factor TCF4 maintains the properties of human corneal epithelial stem cells. Stem Cells, 30, 753–761.
Horenstein, A. L., et al. (2009). CD38 and CD157 ectoenzymes mark cell subsets in the human corneal limbus. Molecular Medicine, 15, 76–84.
Hayashi, R., et al. (2008). Enrichment of corneal epithelial stem/progenitor cells using cell surface markers, integrin alpha6 and CD71. Biochemical and Biophysical Research Communications, 367, 256–263.
Qi, H., et al. (2008). Nerve growth factor and its receptor TrkA serve as potential markers for human corneal epithelial progenitor cells. Experimental Eye Research, 86, 34–40.
Budak, M. T., et al. (2005). Ocular surface epithelia contain ABCG2-dependent side population cells exhibiting features associated with stem cells. Journal of Cell Science, 118, 1715–1724.
de Paiva, C. S., Chen, Z., Corrales, R. M., Pflugfelder, S. C., & Li, D. Q. (2005). ABCG2 transporter identifies a population of clonogenic human limbal epithelial cells. Stem Cells, 23, 63–73.
Yoshida, S., et al. (2006). Cytokeratin 15 can be used to identify the limbal phenotype in normal and diseased ocular surfaces. Investigative Ophthalmology & Visual Science, 47, 4780–4786.
Ksander, B. R., et al. (2014). ABCB5 is a limbal stem cell gene required for corneal development and repair. Nature, 511, 353–357.
Puangsricharern, V., & Tseng, S. C. (1995). Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology, 102, 1476–1485.
Tseng, S. C. (1985). Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology, 92, 728–733.
Tugal-Tutkun, I., Akova, Y. A., & Foster, C. S. (1995). Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology, 102, 576–585.
Alldredge, O. C., & Krachmer, J. H. (1981). Clinical types of corneal transplant rejection. Their manifestations, frequency, preoperative correlates, and treatment. Archives of Ophthalmology, 99, 599–604.
Holland, E. J., & Schwartz, G. S. (2000). Changing concepts in the management of severe ocular surface disease over twenty-five years. Cornea, 19, 688–698.
Tsai, R. J., Li, L. M., & Chen, J. K. (2000). Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. The New England Journal of Medicine, 343, 86–93.
Kenyon, K. R., & Tseng, S. C. (1989). Limbal autograft transplantation for ocular surface disorders. Ophthalmology, 96, 709–722.; discussion 722.
Tsai, R. J., Sun, T. T., & Tseng, S. C. (1990). Comparison of limbal and conjunctival autograft transplantation in corneal surface reconstruction in rabbits. Ophthalmology, 97, 446–455.
Dua, H. S., & Azuara-Blanco, A. (1999). Allo-limbal transplantation in patients with limbal stem cell deficiency. The British Journal of Ophthalmology, 83, 414–419.
Tsubota, K., et al. (1999). Treatment of severe ocular-surface disorders with corneal epithelial stem-cell transplantation. The New England Journal of Medicine, 340, 1697–1703.
Shimazaki, J., et al. (1999). Evidence of long-term survival of donor-derived cells after limbal allograft transplantation. Investigative Ophthalmology & Visual Science, 40, 1664–1668.
Reinhard, T., Sundmacher, R., Spelsberg, H., & Althaus, C. (1999). Homologous penetrating central limbo-keratoplasty (HPCLK) in bilateral limbal stem cell insufficiency. Acta Ophthalmologica Scandinavica, 77, 663–667.
Sundmacher, R., & Reinhard, T. (1996). Central corneolimbal transplantation under systemic ciclosporin A cover for severe limbal stem cell insufficiency. Graefe’s Archive for Clinical and Experimental Ophthalmology, 234(Suppl 1), S122–S125.
Holland, E. J., & Schwartz, G. S. (1996). The evolution of epithelial transplantation for severe ocular surface disease and a proposed classification system. Cornea, 15, 549–556.
Daya, S. M., Chan, C. C., Holland, E. J., & Members, OTCSOSPNC. (2011). Cornea Society nomenclature for ocular surface rehabilitative procedures. Cornea, 30, 1115–1119.
Thoft, R. A. (1977). Conjunctival transplantation. Archives of Ophthalmology, 95, 1425–1427.
Shapiro, M. S., Friend, J., & Thoft, R. A. (1981). Corneal re-epithelialization from the conjunctiva. Investigative Ophthalmology & Visual Science, 21, 135–142.
Tseng, S. C., Hirst, L. W., Farazdaghi, M., & Green, W. R. (1984). Goblet cell density and vascularization during conjunctival transdifferentiation. Investigative Ophthalmology & Visual Science, 25, 1168–1176.
Dua, H. S., & Forrester, J. V. (1990). The corneoscleral limbus in human corneal epithelial wound healing. American Journal of Ophthalmology, 110, 646–656.
Jenkins, C., Tuft, S., Liu, C., & Buckley, R. (1993). Limbal transplantation in the management of chronic contact-lens-associated epitheliopathy. Eye (London, England), 7, 629–633.
Thoft, R. A. (1984). Keratoepithelioplasty. American Journal of Ophthalmology, 97, 1–6.
Turgeon, P. W., Nauheim, R. C., Roat, M. I., Stopak, S. S., & Thoft, R. A. (1990). Indications for keratoepithelioplasty. Archives of Ophthalmology, 108, 233–236.
Tsai, R. J., & Tseng, S. C. (1994). Human allograft limbal transplantation for corneal surface reconstruction. Cornea, 13, 389–400.
Tsubota, K., Toda, I., Saito, H., Shinozaki, N., & Shimazaki, J. (1995). Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology, 102, 1486–1496.
Kwitko, S., et al. (1995). Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology, 102, 1020–1025.
Kenyon, K. R., & Rapoza, P. A. (1995). Limbal allograft transplantation for ocular surface disorders. Ophthalmology, 102, 101–102.
Biber, J. M., Skeens, H. M., Neff, K. D., & Holland, E. J. (2011). The cincinnati procedure: Technique and outcomes of combined living-related conjunctival limbal allografts and keratolimbal allografts in severe ocular surface failure. Cornea, 30, 765–771.
Chan, C. C., Biber, J. M., & Holland, E. J. (2012). The modified Cincinnati procedure: Combined conjunctival limbal autografts and keratolimbal allografts for severe unilateral ocular surface failure. Cornea, 31, 1264–1272.
Holland, E. J., et al. (2012). Systemic immunosuppression in ocular surface stem cell transplantation: Results of a 10-year experience. Cornea, 31, 655–661.
Niederkorn, J. Y. (1995). Effect of cytokine-induced migration of Langerhans cells on corneal allograft survival. Eye (London, England), 9, 215–218.
Daya, S. M., Bell, R. W., Habib, N. E., Powell-Richards, A., & Dua, H. S. (2000). Clinical and pathologic findings in human keratolimbal allograft rejection. Cornea, 19, 443–450.
Holland, E. J. (1996). Epithelial transplantation for the management of severe ocular surface disease. Transactions of the American Ophthalmological Society, 94, 677–743.
Thoft, R. A., & Sugar, J. (1993). Graft failure in keratoepithelioplasty. Cornea, 12, 362–365.
Maruyama-Hosoi, F., Shimazaki, J., Shimmura, S., & Tsubota, K. (2006). Changes observed in keratolimbal allograft. Cornea, 25, 377–382.
Reinhard, T., et al. (2004). Long-term results of allogeneic penetrating limbo-keratoplasty in total limbal stem cell deficiency. Ophthalmology, 111, 775–782.
Ilari, L., & Daya, S. M. (2002). Long-term outcomes of keratolimbal allograft for the treatment of severe ocular surface disorders. Ophthalmology, 109, 1278–1284.
Shimazaki, J., Maruyama, F., Shimmura, S., Fujishima, H., & Tsubota, K. (2001). Immunologic rejection of the central graft after limbal allograft transplantation combined with penetrating keratoplasty. Cornea, 20, 149–152.
Meller, D., & Tseng, S. C. (2000). Amniotic membrane transplantation with or without limbal allografts in corneal surface reconstruction in limbal deficiency. Der Ophthalmologe: Zeitschrift der Deutschen Ophthalmologischen Gesellschaft Ophthalmologe, 97, 100–107 Transplantation von Amnionmembran mit oder ohne allogener Limbustransplantation zur Rekonstruktion der kornealen Oberflache bei Limbusinsuffizienz.
Tan, D. T., Ficker, L. A., & Buckley, R. J. (1996). Limbal transplantation. Ophthalmology, 103, 29–36.
Holland, E. J., Djalilian, A. R., & Schwartz, G. S. (2003). Management of aniridic keratopathy with keratolimbal allograft: A limbal stem cell transplantation technique. Ophthalmology, 110, 125–130.
Burdmann, E. A., Andoh, T. F., Yu, L., & Bennett, W. M. (2003). Cyclosporine nephrotoxicity. Seminars in Nephrology, 23, 465–476.
Curtis, J. J. (2002). Hypertensinogenic mechanism of the calcineurin inhibitors. Current Hypertension Reports, 4, 377–380.
Luke, R. G. (1991). Mechanism of cyclosporine-induced hypertension. American Journal of Hypertension, 4, 468–471.
Kobashigawa, J. A., & Kasiske, B. L. (1997). Hyperlipidemia in solid organ transplantation. Transplantation, 63, 331–338.
Woodle, E. S. (2002). Corticosteroid elimination in renal transplantation: Pro. Transplantation Proceedings, 34, 1693.
Alloway, R. R., et al. (2005). A prospective, pilot study of early corticosteroid cessation in high-immunologic-risk patients: The Cincinnati experience. Transplantation Proceedings, 37, 802–803.
European Mycophenolate Mofetil Cooperative Study Group. (1999). Mycophenolate mofetil in renal transplantation: 3-Year results from the placebo-controlled trial. Transplantation, 68, 391–396.
Ekberg, H., et al. (2007). Reduced exposure to calcineurin inhibitors in renal transplantation. The New England Journal of Medicine, 357, 2562–2575.
Boratynska, M., Banasik, M., Patrzalek, D., & Klinger, M. (2006). Conversion from cyclosporine-based immunosuppression to tacrolimus/mycophenolate mofetil in patients with refractory and ongoing acute renal allograft rejection. Annals of Transplantation, 11, 51–56.
Tabbara, K. F. (2008). Pharmacologic strategies in the prevention and treatment of corneal transplant rejection. International Ophthalmology, 28, 223–232.
Vanrenterghem, Y. F. (1999). Which calcineurin inhibitor is preferred in renal transplantation: Tacrolimus or cyclosporine? Current Opinion in Nephrology and Hypertension, 8, 669–674.
Mogilishetty, G., Haird, D., Alloway, R. R., et al. (2008). Comparison of immunosuppression related toxicities and complications in ocular surface transplant and renal transplant recipients: Implications for composite tissue transplantation [abstract]. Transplantation, 86, 11.
Salisbury, J. D., & Gebhardt, B. M. (1981). Blood group antigens on human corneal cells demonstrated by immunoperoxidase staining. American Journal of Ophthalmology, 91, 46–50.
Treseler, P. A., Foulks, G. N., & Sanfilippo, F. (1984). The expression of HLA antigens by cells in the human cornea. American Journal of Ophthalmology, 98, 763–772.
Clinch, T. E., Goins, K. M., & Cobo, L. M. (1992). Treatment of contact lens-related ocular surface disorders with autologous conjunctival transplantation. Ophthalmology, 99, 634–638.
Pellegrini, G., et al. (1997). Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet, 349, 990–993.
Ouyang, H., et al. (2014). WNT7A and PAX6 define corneal epithelium homeostasis and pathogenesis. Nature, 511, 358–361.
Pellegrini, G., et al. (1999). Location and clonal analysis of stem cells and their differentiated progeny in the human ocular surface. The Journal of Cell Biology, 145, 769–782.
Miri, A., Al-Deiri, B., & Dua, H. S. (2010). Long-term outcomes of autolimbal and allolimbal transplants. Ophthalmology, 117, 1207–1213.
Okita, K., Ichisaka, T., & Yamanaka, S. (2007). Generation of germline-competent induced pluripotent stem cells. Nature, 448, 313–317.
Takahashi, K., et al. (2007). Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell, 131, 861–872.
Takahashi, K., & Yamanaka, S. (2006). Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell, 126, 663–676.
Hayashi, R., et al. (2012). Generation of corneal epithelial cells from induced pluripotent stem cells derived from human dermal fibroblast and corneal limbal epithelium. PLoS One, 7, e45435.
Kheirkhah, A., Raju, V. K., & Tseng, S. C. (2008). Minimal conjunctival limbal autograft for total limbal stem cell deficiency. Cornea, 27, 730–733.
Sangwan, V. S., Basu, S., MacNeil, S., & Balasubramanian, D. (2012). Simple limbal epithelial transplantation (SLET): A novel surgical technique for the treatment of unilateral limbal stem cell deficiency. The British Journal of Ophthalmology, 96, 931–934.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ballios, B.G., Slomovic, A.R. (2018). Clinical Applications of Limbal Stem Cells for Regenerative Medicine. In: Ballios, B., Young, M. (eds) Regenerative Medicine and Stem Cell Therapy for the Eye. Fundamental Biomedical Technologies. Springer, Cham. https://doi.org/10.1007/978-3-319-98080-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-98080-5_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98079-9
Online ISBN: 978-3-319-98080-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)