Abstract
Cervical spondylotic myelopathy (CSM) is caused by damage to the spinal cord from progressive, age-related degenerative narrowing of the spinal canal. Regardless of the degree of narrowing, signs and symptoms can vary widely for each individual patient with CSM. Currently there are no universally accepted guidelines regarding the timing of surgery for CSM. Surgical decision-making for CSM requires complex integration of each patient’s symptoms, physical exam findings, radiographic findings, patient lifestyle, and overall health. These characteristics can then be used to stratify patients with CSM into asymptomatic, mild, moderate, and severe disease categories. This chapter aims to provide evidence-based recommendations to determine the need and timing of surgical decompression in patients with CSM based upon disease severity category.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Pitfalls/Pearls-
Asymptomatic and mild cervical spondylotic myelopathy patients can be treated with nonoperative therapy.
-
Surgical decompression should be offered in cases of progressive, moderate, or severe cervical spondylotic myelopathy or in those who have failed nonoperative treatment.
-
Surgical decision-making requires careful consideration in elderly, chronically ill, or mildly symptomatic patients.
Introduction
Cervical spondylotic myelopathy (CSM) is the result of progressive degenerative narrowing of the spinal canal causing spinal cord compression. The pathophysiology of CSM involves both primary mechanical and secondary biological injury to the spinal cord. Primary mechanical spinal cord injury is frequently caused by a combination of disc degeneration, facet hypertrophy, and ligamentum flavum thickening. This results in compressive, distracting, or shear forces on the spinal cord. Secondary biological injury is multifactorial and involves elements of glutamate-related toxicity, cell injury from free radicals, apoptosis, or spinal cord ischemia [5]. While surgery is able to relieve primary mechanical compression of the spinal cord, it does not directly treat secondary biological injury. As the inherent recuperative capacity of the spinal cord is unpredictable, neurological recovery should never be guaranteed to patients considering surgery – although this is commonly the case.
The prevalence of CSM is estimated at 604 per million in North America, with 16 per million requiring surgery [3, 17]. Although over half of all middle-age people have radiographic evidence of cervical spondylosis, only 10% have myelopathic or radicular symptoms [13]. Furthermore, for patients with cervical spondylotic myelopathy, approximately 20% to 60% will deteriorate neurologically overtime without surgery [12]. In order to prevent this deterioration and irreversible neurological injury, some surgeons offer decompression surgery to all patients with radiographic evidence of cervical spinal cord compression, regardless of symptom severity. However, a small but significant risk of neurological injury or other complications exists with any surgical intervention. Based on data [2] from the National Inpatient Sample of CSM patients undergoing surgery from 1993 to 2002, the postoperative complication rate was 13.4%. A single postoperative complication led to a 4-day increase in mean length of hospital stay, increased the mortality rate twofold, and added more than $10,000 to hospital charges. Patients aged 65–84 years had 8- and 14-fold increases in complications and mortality, respectively, compared to patients less than 64 years of age.
Despite a high prevalence of this disease and different surgical treatment options, there remains a lack of universally accepted guidelines regarding the timing of operative intervention for patients with CSM. This chapter aims to provide evidence-based recommendations to determine the need and timing for surgical decompression in patients with cervical spondylotic myelopathy (Table 12.1).
Assessment and Treatment
Evaluation
History and Physical Examination
Each patient with suspected cervical spondylotic myelopathy should have a detailed history and physical exam. Signs and symptoms of myelopathy may be subtle, including changes in axial balance, dysfunctional bladder control, decreased dexterity, distorted proprioception, or abnormal gait. The interviewer should explore risk factors that may accelerate the degenerative processes of cervical spondylosis, including occupational or lifestyle hazards (carrying objects on the head or contact sports), as well as associated comorbidities, such as Down syndrome, rheumatoid arthritis , or Klippel-Feil syndrome. Additionally, patient lifestyle may have an impact on whether patients considered “on the bubble” for surgery based on rather modest symptomatology would be more optimally treated with surgical intervention. This could include individuals who engage in recreational or occupational high-impact activities, (e.g., surfing) or those with a history of frequent falls.
A comprehensive physical examination is critically important and should focus on strength testing, evaluation of reflexes, and sensation. Objective clinical findings of myelopathy include increased deep tendon reflexes, positive pathological reflexes, and sensory disturbances. Finally, consideration should be given to other etiologies of myelopathy, such as syringomyelia, trauma, amyotrophic lateral sclerosis, multiple sclerosis, progressive polyarthritis, congenital pathologies, or vitamin B12 deficiency.
The presence and severity of cervical myelopathy can be assessed with multiple quantitative scales, including Nurick grade, Japanese Orthopaedic Association score, modified Japanese Orthopaedic Association (mJOA) score, the short form-36, walking test, and grip and release test. We typically use the mJOA score, one of the most frequently used measurements, which utilizes a functional assessment scale in patients with CSM [14]. It cannot be stressed enough, however, that although quantitative scores may be used to evaluate patients and improve documentation, they should be considered adjunctive, and not the primary tool used in surgical decision-making.
Radiographical Imaging
All patients with presumed cervical stenosis should have AP/lateral X-rays with dynamic flexion and extension views, as well as MRI of the cervical spine. X-ray imaging is important to visualize bony anatomy, evaluate cervical stability, assess cervical alignment, and accurately localize spinal levels. CT scans are helpful in diagnosing lesions that are poorly evaluated with MRI such as ossification of the posterior longitudinal ligament or calcified intervertebral discs. However, MRI is the most useful imaging modality overall, as it provides a detailed visualization of soft tissue anatomy and high-resolution imaging of the spinal cord macrostructure. It is believed that an anteroposterior compression ratio (anterior-posterior cord diameter divided by the transverse cord diameter) of less than 40%, a reduction in the size of the spinal cord by 30%, or a transverse area less than 60 sq mm are likely to result in myelopathic symptoms [8, 18]. Many surgeons also use an AP diameter cutoff of 7 mm to assess for potential cervical cord compression. In 2009, the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons published Guidelines for the Surgical Management of Cervical Degenerative Disease, which concluded that multilevel T2 hyperintensity, T1 focal hypointensity combined with T2 focal hyperintensity, and spinal cord atrophy were all associated with poor prognosis after surgery [16]. Some believe that areas of increased T2-weighted signal change represent edema, gliosis, ischemia, and potentially reversible change, whereas corresponding areas of T1 hypointensity have been correlated histopathologically with late stages of myelomalacia or cystic necrosis and, thus, represent irreversible spinal cord injury [19].
Electrophysiological Testing
Some surgeons report that electrophysiological testing before and after surgery can aid in preoperative diagnosis, assist with disease monitoring, and provide accurate prognostic information [9]. However, we do not advocate routine electrophysiological testing. Yet in cases when distinguishing myelopathy from radiculopathy is challenging (or when myelopathy and radiculopathy coexist), then electrophysiological testing should be considered. Of note, this type of testing is distinct from intraoperative electrophysiological monitoring that alerts the surgeon to intraoperative neurophysiological changes, although it’s overall intraoperative utility remains controversial.
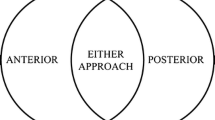
At present, no radiographic, serologic, or electrophysiological sign is regularly used clinically for predicting functional impairment due to CSM. Recent research has pointed to advanced imaging techniques, such as diffusion tensor imaging, as potentially showing promising results which may be useful in the future [6]. Until a reliable and reproducible biomarker is discovered, determination of when to offer surgery to patients with CSM requires integrating physical exam findings, imaging results, and careful analysis of the patient’s history. Patients should then be stratified into asymptomatic, mild, moderate, and severe categories, which will be reviewed here.
Non-myelopathic Spondylosis
Non-myelopathic spondylosis refers to patients without symptoms of myelopathy but with imaging evidence of cord compression (Fig. 12.1). The diagnosis of cervical spondylosis in this patient population is often made incidentally after imaging has been obtained for other reasons such as neck pain or trauma.
Asymptomatic spondylosis. A 38-year-old male with neck pain, found to have hyperreflexia but no weakness, sensory change, or gait abnormality (mJOA 18). He was treated with physical therapy and has not required surgical intervention (mJOA 18). (a) CT cervical spine showing areas of osteophyte formation. (b) MRI cervical spine with mild spondylosis and ventral cord effacement without spinal cord signal change
Cervical spondylosis is an expected consequence of aging, with an incidence of 10% at age 25 and 95% by the age of 65 [22]. Senior citizens are the fastest-growing age group in the United States, and by the middle of this century, it is predicted that they will represent 23% of the population [23]. Thus, asymptomatic cervical spondylosis is likely to be encountered with increasing frequency in the coming years.
Non-myelopathic spondylosis patients can be subdivided into those with and without radiculopathy. The rationale for this distinction is that the presence of symptomatic radiculopathy, either clinical or electrophysiological, has been reported as a significant predictor of myelopathy development. Utilizing multivariate analysis, in a recent systematic review, Wilson et al. determined that clinically symptomatic radiculopathy (p = 0.007; moderate level evidence) and prolonged somatosensory (SEP) (p = 0.007; moderate level evidence) and motor evoked potentials (MEP) (p = 0.033; moderate level evidence) were significantly associated with early (≤1 year) myelopathic development [25]. Additionally, a diagnosis of radiculopathy was encountered in 63% of patients that developed myelopathy within 1 year compared to only 23% that did not develop myelopathy. Expectedly, abnormal SEP and MEP were present in a much larger percentage of patients that developed myelopathy than those that did not. One of the most cited clinical studies in this patient population was performed by Bednarik et al., who longitudinally evaluated the clinical examination, EMG, and SEP in a group of 66 non-myelopathic patients with spinal cord compression [1]. Development of myelopathy was defined by neurological examination and a decrease in mJOA score of 1 point or greater. Approximately 20% of the cohort developed CSM, and radiculopathy was encountered in 92% of those that developed CSM and 24% of those that did not (p < 0.0001). EMG abnormalities were observed in 61% of those that developed CSM and 11% of those that did not (p < 0.01).
However, there is no evidenced-based consensus to support prophylactic surgical decompression in asymptomatic patients with spinal cord compression. These patients should be informed about the signs and symptoms of myelopathy, the risks of progression, and observed clinically. In contrast, the treatment of non-myelopathic patients with spinal cord compression and radiculopathy is more controversial. While there have been no published studies comparing operative to nonoperative treatment in this patient population, there is mounting evidence that the presence of radiculopathy is associated with the development of myelopathy [1]. Moreover, some of these patients will require surgery for significant radiculopathy that is refractory to nonoperative therapy. As such, surgery can be considered in this patient population, and consideration should be made to treat both the radiculopathy and the spinal cord compression. These entities may be located at different spinal levels, and a multilevel procedure may be required, even if the radiculopathy originates from a single level. Nonoperative intervention consisting of close longitudinal follow-up or a supervised trial of structured rehabilitation can also be offered and, in fact, may be the most appropriate initial option for the majority of these patients. However, if myelopathy develops during the course of nonoperative treatment, surgical management should be entertained.
Mild Spondylotic Myelopathy
Mild spondylotic myelopathy refers to patients with subtle or relatively minor myelopathic symptoms that may not be disabling in any one category but with objective radiographic or physical exam findings of spinal cord narrowing. These patients typically have a mJOA score of 15–17. As with non-myelopathic patients with spinal cord compression and radiculopathy, controversy remains regarding optimal treatment of patients with mild CSM due to a relative lack of high-level published data directly comparing operative to nonoperative treatment for this patient population. Kadanka et al. [10] performed a prospective study that included both mild and moderate CSM patients (n = 68) that were randomized to either surgical (n = 33) or nonoperative treatment (n = 35). The patients were evaluated using the mJOA scale, a timed 10-meter walk, video assessment of daily activity performance, and self-reported evaluation at standardized time points over a 3-year period. There was no significant deterioration in the mJOA score in the two groups over the 3-year follow-up period. However, there was a significant difference in the time walk that favored the nonoperative group. Nonetheless, the mJOA score demonstrated no difference between groups. The authors concluded that there was no significant difference between surgery and nonoperative therapy in the treatment of patients with mild to moderate CSM. This initial cohort was subsequently followed for a total of 10 years, and the results were reported in a separate publication [11]. Once again the authors did not find a significant difference between nonoperative and surgical intervention at the latter time point. However, it must be noted that the lack of improvement following surgical intervention in these two studies is contrary to the results from a number of other investigations [20].
Although nonoperative management has been demonstrated to stabilize disease progression in some mildly affected CSM patients, the ability of this modality to effect neurological improvement is another matter. Based on the available literature, it appears as though neurological improvement that reaches the minimal clinically important difference (MCID) may be possible in a cohort of nonoperatively treated patients with soft disc herniation and/or dynamic myelopathy [15]. Intuitively this makes sense as a soft disc herniation may resorb with immobilization, and cessation of movement is a well-known treatment of dynamic myelopathy. However, nonoperative treatment is less likely to induce neurological recovery that reaches the MCID in patients with severe static compression from spondylotic bars or ossified spinal elements. In contrast, surgery may result in neurological improvement in patients with a wide variety of pathophysiology and radiographic findings compared to immobilization alone. Results from the AOSpine North America prospective multicenter study have suggested that mildly affected CSM patients can achieve statistically significant improvements in both the mJOA and Nurick scores despite the ceiling effect associated with these functional assessment tools [7].
Based on the aforementioned data, it is therefore reasonable to offer surgical intervention or a supervised trial of structured rehabilitation for patients with mild CSM. In patients treated nonoperatively, surgery should be recommended if there is neurological deterioration during the observation period. Although there are no published guidelines regarding the duration of observation, many surgeons offer surgery if symptoms persist after 3 or more months of nonoperative therapy. There is no convincing available data that mild or asymptomatic patients should undergo prophylactic decompression surgery to prevent the occurrence of paralysis following a traumatic event, such as a fall or motor vehicle accident. A recent study by Chang et al. [4] prospectively followed 55 asymptomatic or mildly affected patients with cervical stenosis that were treated nonoperatively. Thirty-one patients (56%) were previously recommended surgery by a previous physician. Twenty-six patients (47%) were told that they would be paralyzed after a motor vehicle accident or fall unless surgery was performed. The patients were followed for a mean of 2.3 years. Ten patients (18%) experienced a traumatic event during the follow-up, with none sustaining an SCI. The authors concluded that occurrence of SCI in this patient population after minor trauma is likely smaller than many physicians surmise, yet a prospective study with a large cohort of patients is necessary to fully elucidate their true risk stratification.
Moderate Spondylotic Myelopathy
Moderate spondylotic myelopathy refers to patients with clear signs and symptoms of myelopathy and that typically have a mJOA score of 12–14 (Fig. 12.2). They may present with mild to moderate hand coordination and gait difficulty or relatively profound isolated impairment in one of these functions. Although nonoperative treatment may be attempted in patients at the cusp of mild to moderate myelopathy, current literature suggests that patients with moderate CSM should undergo surgical intervention. In fact, patients are 1.22 times more likely to achieve a postoperative mJOA score of >16 for every 1-point increase in preoperative mJOA [24]. Conversely, in a study of patients with a mJOA score of 11–14 who were treated nonoperatively, the change in mJOA score was minimal (0–2.3), and up to 54% of patients eventually required surgery [25]. As such, nonoperative treatments are typically considered stopgap measures prior to surgery. Part of the rationale with this recommendation is that spinal cord compression severe enough to result in moderate spinal cord dysfunction can be associated with progressive permanent microstructural changes that cannot be reversed through decompression surgery. Therefore, pursing nonoperative treatment in this patient population confers the risk of neurological functional decline. As part of a large multicenter study, Fehlings et al. prospectively followed 110 moderately affected CSM patients that underwent surgical decompression [7]. The mean improvement in the mJOA score was 2.58, the Nurick grade 1.51, and the NDI 9.79. All of these were statically significant improvements compared to the preoperative baseline and surpassed the MCID measurements for moderate CSM.
Moderate CSM. A 40-year-old male with bilateral hand weakness, paresthesias, and positive Hoffman’s sign (mJOA 14). Per patient wishes, conservative therapy was trialed for 3 months with persistent symptoms, and thus, the patient underwent C3–6 laminoplasty. Postoperatively the patient’s hand strength and sensation improved significantly (mJOA 16). (a) X-ray cervical spine showing cervical straightening and moderate osteophyte formation. (b) MRI cervical spine with diffuse spondylosis and focal stenosis at C5–6, with corresponding spinal cord T2-weighted signal hyperintensity
This sentiment was also found in a study by Sampath et al. who prospectively compared the results of operative versus nonoperative treatment for moderate to severe CSM [21]. Surgical patients had improved functional status and overall pain but with nonsignificant improvement in preoperative neurological symptoms. In contrast, nonoperative patients had significant worsening of their functional status and nonsignificant worsening of their baseline neurological symptoms. The fact that the operative cohort noted functional improvement while the nonoperative group declined infers a benefit to operative management in this patient population.
Nonoperative treatment may be appropriate in this patient population under certain circumstances, including severe medical comorbidities that significantly increase surgical risk, personal aversion to surgery, or improving symptomatology. However, if a nonoperative strategy is pursued, patients in this moderate category must be closely monitored for progressive symptoms or red flags, such as bowel/bladder symptoms, sexual dysfunction, or new-onset paresis.
Severe Spondylotic Myelopathy
Severe spondylotic myelopathy refers to patients with significant signs and symptoms of myelopathy or those with rapidly progressive disease (Fig. 12.3). These patients typically have a mJOA score of 0–11 and may be wheelchair bound or completely dependent on a walking assist device. MRI characteristics frequently include an AP diameter of 7 mm or less, suggesting severe spinal canal narrowing with cord compression, and may demonstrate evidence of spinal cord injury. This includes high T2-weighted intramedullary signal intensity, corresponding low T1-weighted intramedullary signal intensity or spinal cord atrophy.
Severe spondylosis. An 82-year-old male with hand weakness, progressive gait abnormality, and hyperreflexia (mJOA 7). The patient underwent C3–7 laminectomy and fusion 1 week after consultation. Postoperatively, the patient’s dexterity and ability to ambulate improved, although some gait dysfunction persisted (mJOA 11). (a) X-ray cervical spine demonstrating severe degenerative changes, kyphosis, osteophyte formation, and auto-fusion. (b) MRI cervical spine with multilevel stenosis and T2 signal change at C6–7
A recent study of patients with severe spondylotic myelopathy found that with surgery, the average mJOA score improved by 4.91 and Nurick score improved by 1.74 [7]. Although the nearly 5-point increase in mJOA appears impressive, these patients with severe CSM still have a relatively low postoperative mJOA score, suggesting only a minimal change in true functional capacity. Therefore, surgery should ideally be performed before the symptoms become severe. Nonetheless, Yoshimatsu et al. [26] performed a retrospective study in which CSM patients chose to either undergo operative intervention or nonoperative treatment. Patients that underwent surgery had more severe CSM, with a mean JOA of 9.1, compared to those in the nonoperative group. In the immediate surgery group, 78% improved their JOA score at last follow-up, whereas only 23% of patients in the nonoperative group improved from their baseline scores. Accordingly, results of this study advocate for urgent surgical decompression in this patient population, typically within a few weeks. Nonoperative treatments are of limited utility and could delay surgical intervention, resulting in further neurological injury.
Specific Time Frame of Surgery
There are no published studies that support a specific time frame for surgery, and the majority of previous investigations and guidelines have assessed this important question by stratifying timing based on severity of disease, as presented in this chapter. However, we have provided some time frames based on our experience and interpretation of the available medical literature in Table 12.1. The overall concept of erring toward earlier instead of later surgical intervention appears to be supported in a large prospective multicenter study of CSM patients undergoing surgical intervention [24]. They found that the odds of a successful outcome decreased by 22% when the duration of symptoms increased from ≤ to 3 months to at least 3 but less than 6 months.
Conclusions
Surgical decision-making for cervical spondylotic myelopathy requires careful integration of patients’ subjective symptoms, objective physical exam findings, radiographic evidence, patient lifestyle, and overall health. Based upon this analysis, patients may be stratified into asymptomatic, mild, moderate, and severe disease categories. Patients with non-myelopathic disease do not require treatment, per se, but should be followed closely, particularly if there is evidence of concurrent radiculopathy. Patients with mild disease may improve or stabilize with nonoperative treatment, but surgical management has been also demonstrated to provide benefit. Patients with moderate disease usually require surgery, which should be considered first-line treatment. Conservative measures may be offered to patients who refuse surgery or who have elevated operative risk. However, these patients require vigilant monitoring for signs of disease progression, including gait dysfunction or loss of dexterity. Finally, patients with severe spondylotic myelopathy should be managed with surgical decompression, as delays in utilizing nonoperative management may result in further irreversible neurologic decline.
References
Bednarik J, Kadanka Z, Dusek L, Novotny O, Surelova D, Urbanek I, et al. Presymptomatic spondylotic cervical cord compression. Spine. 2004;29:2260–9.
Boakye M, et al. Cervical spondylotic myelopathy: complications and outcomes after spinal fusion. Neurosurgery. 2008;62:455–61; discussion 461–452.
Boogaarts HD, Ronald HM. Prevalence of cervical Spondylotic myelopathy. Eur Spine J. 2013;24(S2):139–41.
Chang V, Ellingson BM, Salamon N, Holly LT. The risk of acute spinal cord injury after minor trauma in patients with preexisting cervical stenosis. Neurosurgery. 2015;77(4):561–5; discussion 565.
Dolan RT, Butler JS, O’Byrne JM, Poynton AR. Mechanical and cellular processes driving cervical myelopathy. World J Orthop. 2016;7(1):20–9.
Ellingson BM, Salamon N, Grinstead JW, Holly LT. Diffusion tensor imaging predicts functional impairment in mild-to-moderate cervical spondylotic myelopathy. Spine J. 2014;14(11):2589–97.
Fehlings MG, Wilson JR, Kopjar B, Yoon ST, Arnold PM, Massicotte EM, Vaccaro AR, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America Prospective Multi-Center Study. J Bone Joint Surg Am. 2013;95(18):1651–8.
Fujiwara K, Yonenobu K, Ebara S, Yamashita K, Ono K. The prognosis of surgery for cervical compression myelopathy. An analysis of the factors involved. J Bone Joint Surg. 1989;71(3):393–8.
Hu Y, Ding Y, Ruan D, Wong YW, Cheung KMC, Luk KDK. Prognostic value of somatosensory-evoked potentials in the surgical management of cervical spondylotic myelopathy. Spine. 2008;33(10):E305–10.
Kadanka Z, Mares M, Bednanik J, Smrcka V, Krbec M, Stejskal L, et al. Approaches to spondylotic cervical myelopathy: conservative versus surgical results in a 3-year follow-up study. Spine. 2002;27:2205–10; discussion 2210–2201.
Kadanka Z, Bednarik J, Novotny O, et al. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J. 2011;20:1533–8.
Karadimas SK, Mark Erwin W, Ely CG, Dettori JR, Fehlings MG. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine. 2013;38(22 Suppl 1):S21–36.
Klineberg E. Cervical spondylotic myelopathy: a review of the evidence. Orthop Clin North Am. 2010;41(2):193–202.
Kopjar B, Tetreault L, Kalsi-Ryan S, Fehlings M. Psychometric properties of the modified Japanese Orthopaedic Association scale in patients with cervical spondylotic myelopathy. Spine. 2015;40(1):E23–8.
Matsumoto M, Chiba K, Ishikawa M, Maruiwa H, Fujimura Y, Toyama Y. Relationships between outcomes of conservative treatment and magnetic resonance imaging findings in patients with mild cervical myelopathy caused by soft disc herniations. Spine. 2001;26(14):1592–8.
Matz PG, Anderson PA, Kaiser MG, Holly LT, Groff MW, Heary RF, Mummaneni PV, et al. Introduction and methodology: guidelines for the surgical management of cervical degenerative disease. J Neurosurg Spine. 2009;11(2):101–3.
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine. 2015;40(12):E675–93.
Ono K, Ota H, Tada K, Yamamoto T. Cervical myelopathy secondary to multiple Spondylotic protrusions. Spine. 1977;2(2):109–25.
Ramanauskas WL, Wilner HI, Metes JJ, Lazo A, Kelly JK. MR imaging of compressive myelomalacia. J Comput Assist Tomogr. 1989;13(3):399–404.
Rhee JM, Shamji MF, Erwin WM, et al. Nonoperative management of cervical myelopathy: a systematic review. Spine (Phila Pa 1976). 2013;38:S55–67.
Sampath P, Bendebba M, Davis JD, et al. Outcome of patients treated for cervical myelopathy. A prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976). 2000;25:670–6.
Steinmetz MP, Benzel EC. Benzel’s spine surgery: techniques, complication avoidance, and management. 2017.
Stevens JA, Olson S. Reducing falls and resulting hip fractures among older women. MMWR Recomm Rep. 2000;49:3–12.
Tetreault LA, Kopjar B, Vaccaro A, Yoon ST, Arnold PM, Massicotte EM, Fehlings MG. A clinical prediction model to determine outcomes in patients with cervical spondylotic myelopathy undergoing surgical treatment: data from the prospective, Multi-Center AOSpine North America Study. J Bone Joint Surg Am. 2013;95(18):1659–66.
Wilson JR, Barry S, Fischer DJ, Skelly AC, Arnold PM, Daniel Riew K, Shaffrey CI, Traynelis VC, Fehlings MG. Frequency, timing, and predictors of neurological dysfunction in the nonmyelopathic patient with cervical spinal cord compression, canal stenosis, and/or ossification of the posterior longitudinal ligament. Spine. 2013;38:S37–54.
Yoshimatsu H, Nagata K, Goto H, et al. Conservative treatment for cervical spondylotic myelopathy. Prediction of treatment effects by multivariate analysis. Spine J. 2001;1:269–73.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tucker, A.M., Niu, T., Nagasawa, D.T., Holly, L.T. (2019). Timing of Operative Intervention. In: Kaiser, M., Haid, R., Shaffrey, C., Fehlings, M. (eds) Degenerative Cervical Myelopathy and Radiculopathy . Springer, Cham. https://doi.org/10.1007/978-3-319-97952-6_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-97952-6_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97951-9
Online ISBN: 978-3-319-97952-6
eBook Packages: MedicineMedicine (R0)