Abstract
Cervical spondylosis can lead to clinical symptoms of both cervical radiculopathy and myelopathy or a combination of the two. Clinical decision-making is based on a foundation of a detailed history and physical examination, combined with the appropriate imaging studies, such as plain static and dynamic radiographs, magnetic resonance imaging (MRI), computed tomography (CT), and, occasionally, myelography with post-myelography CT imaging. However, in certain situations, additional diagnostic testing may be required. The clinician may decide to use additional studies such as electromyography with nerve conduction studies, motor or sensory evoked potentials, diagnostic selective nerve root blocks, or other less frequently used diagnostic tools in order to guide clinical decision-making. This chapter will delineate the basics of these alternative diagnostic tools in the preoperative setting.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cervical spondylosis
- Electromyography
- Nerve conduction study
- Selective nerve root blocks
- Alternative diagnostic tools or studies
-
EMG/NCV should not be used as a replacement for a detailed history and physical examination, and should be used sparingly and only when necessary, as these tests increase cost and discomfort to the patient.
-
EMG/NCV should be performed by an appropriate and well-trained physician. In some states, these tests may legally be performed by physical therapists or chiropractors. The study should be performed with the interpreting neurologist or physiatrist on site and not performed by a technician and interpreted at a later time.
-
Electrophysiologic studies should be reviewed in the appropriate clinical context. For example, a study that determines that a radiculopathy is present based solely on paraspinal muscle denervation, in a patient that has already had one or more spine surgeries, should be viewed with suspicion.
-
EMG/NCV studies should be obtained when a patient has clinical signs and symptoms that cannot be correlated to one specific finding on imaging or when imaging shows compression at several different levels that may be similar in nature. In this setting, EMG may be useful in delineating which are of compression is the causative agent.
-
EMG/NCV may also be useful in helping determine if a patient has a specific cervical radiculopathy versus a distal entrapment neuropathy, such as median or ulnar neuropathy.
-
While cervical transforaminal selective nerve root blocks may be performed as a diagnostic tool in order to determine if a specific neural foramen is the location of neural compression, this injection is not without significant risk of vertebral artery injury, which should be taken into account prior to obtaining or ordering such a test.
Introduction
Cervical radiculopathy and myelopathy are among the more common causes of patients presenting to a spinal specialist. Radiculopathy typically presents with a combination of neck pain, paresthesias, numbness, and/or weakness in a specific cervical nerve root distribution in one or both arms. There may be absence of reflexes in the affected distribution as well. Cervical myelopathy may present with neck pain as well as upper motor neuron signs, which include hyperreflexia, including a positive Hoffman’s sign, and symptoms related to increased spasticity, such as difficulty with fine motor skills, balance, Lhermitte’s sign, paresthesias in the arms and legs, and increased muscle tone.
The annual age-adjusted incidence of cervical radiculopathy is 83.2 per 100,000 person-years [1]. There is age adjusted incidence , and then there is age specific incidence for the age group 50–54 years old, where it reaches a peak of 202.9 per 100,000 person-years. The incidence and prevalence of cervical myelopathy have been estimated to be 41 and 605 per million in North America, respectively, while the incidence of cervical spondylotic myelopathy-related hospitalizations has been estimated at 4.04 per 100,000 person-years [2].
The basis of surgical decision-making for patients with cervical radiculopathy or myelopathy is a detailed history and physical examination, with correlation of radiographic studies. For patients who have distinct and well-delineated symptoms, with appropriate findings on physical examination, and corresponding radiographic findings, the causative agent in most cases need not be confirmed with additional testing.
However, in cases in which the differential diagnosis continues to encompass more than one possible etiology for the patient’s presentation, other diagnostic tools may be required to determine the most effective treatment paradigm. In most cases, these adjuvant tests have a lower sensitivity and/or specificity than imaging studies. But in situations where the diagnosis is not definitive based on history, physical/neurological examination, and imaging, supplementing with these additional studies may be necessary in order to confirm the diagnosis and determine treatment.
This chapter will focus on diagnostic studies apart from imaging studies such as magnetic resonance imaging, which are used in the evaluation of patients with cervical radiculopathy or myelopathy. The most commonly used adjuvant diagnostic test is electromyography and nerve conduction testing. Some are used relatively often, while others are used rarely. These studies may be a useful adjuvant when used in combination with imaging and a detailed history and physical/neurological examination.
Electromyography and Nerve Conduction Study
Electromyography and nerve conduction studies are some of the most commonly used adjuvant diagnostic tools used in patients with potential cervical radiculopathy. Laws regarding what type of practitioner is qualified to perform an EMG/NCV vary state to state and can include neurologists, physiatrists, chiropractors, or physical therapists. The American Association of Neuromuscular & Electrodiagnostic Medicine issued a position statement recommending that this testing only be performed by physicians who specialize in neurology or physical medicine and rehabilitation in order to ensure high-quality testing [3]. Because this testing is directed at electrophysiologic testing of a specific nerve root, it is of limited value in a patient with cervical myelopathy. In fact, a patient may have an obvious cervical myelopathy and have a normal electromyography and nerve conduction study. Electromyography (EMG) is a separate test from nerve conduction studies (NCS), but both are commonly performed together.
EMG utilizes an electromyograph to determine the electric potential or difference in voltage which is generated by muscle tissue when stimulated. EMG uses either surface electrodes or intramuscular leads to measure this difference; however, intramuscular needle EMG testing is typically more accurate [3]. Most commonly, a monopolar EMG needle is inserted in the muscle with a surface electrode used as reference.
The intramuscular needle inserted for EMG will measure insertional activity and resting activity in the muscle. Insertional activity is the short burst activation that occurs with insertion of the needle into the muscle. This short activation is typically less than 100 milliseconds. Insertion of the needle or subsequent movement of the needle will cause a short burst of depolarization from muscle fibers, which should cease once the movement is stopped. Prolonged insertional activity may be pathologic in patients who have myopathy, or in patients with early neuropathy, prior to more advanced neuropathy in which fibrillation potentials are present. Increased insertional activity may occur in partially denervated muscles, which become progressively more irritable as denervation progresses. Increased insertional activity is not a specific finding, but an indication of irritability and early denervation. Decreased insertional activity can be seen in patients with advanced muscle loss or necrosis. Once inserted into the muscle, resting activity is measured, and pathology may be seen if the resting muscle displays fasciculations or fibrillations.
Further EMG study measures the electrical potential during active muscle contraction. The resultant size, frequency, and shape of electrical activity during muscle contraction are used to determine the functional capability of the muscle being analyzed. See Fig. 10.1 for an example of a normal EMG waveform. Additional parameters measured by EMG include the maximal voluntary contraction, which measures the peak force generated by the muscles being measured. In addition, muscle fatigue can be measured during the test by monitoring the degradation of the signal amplitude and duration through the course of the test. EMG may also delineate pathology at the neuromuscular junction, by measuring decreased recruitment of muscle activity in a motor unit action potential.
EMG is typically performed with a concurrent nerve conduction study test. While EMG measures electrical potential, or difference in electrical voltage, neve conduction studies measure the time it takes for an electrical stimulus to travel from the site of stimulation to the site of recording. There are four parts to a complete nerve conduction study test. These include motor NCS, sensory NCS, F-wave study, and H-reflex study. See Fig. 10.2 for a normal NCS waveform. While the study is often called nerve conduction velocity , or NCV, this is a misnomer, as the velocity is just one component of the entire study.
Motor NCS measures the time interval for an electrical stimulus to reach the muscle supplied by the nerve stimulated, which is called latency, and is measured in milliseconds. Once the stimulus reaches the muscle, the amplitude of the response is measured in millivolts. Measurements done on two or more locations along the same nerve allow the nerve conduction velocity to be measured by determining the difference in latencies against the difference between the distances of the stimulating electrodes.
Sensory nerve conduction studies are recorded from a sensory area of the nerve stimulated. In most cases, this is a distal area, such as a finger. Again, latency and amplitude are measured, but sensory amplitudes are smaller than motor amplitudes and are measured in microvolts rather than millivolts. The sensory nerve conduction velocity is again calculated using the latency and the distance between electrodes.
One key component in interpretation of nerve conduction studies is that the neural cell bodies for the sensory nerves are located in the dorsal ganglion. Therefore, in cervical radiculopathy, the lesion will be proximal to the cell bodies, and the sensory NCS will be normal, while electromyography will be positive. In the setting of a positive NCS, lesions distal to the dorsal root ganglion must be considered, such as brachial plexitis or median or ulnar neuropathy [4].
F-wave is a measurement of action potentials from a muscle during supramaximal stimulation. Stimulation occurs in the limb, and travels to the ventral horn of the spinal cord, and then returns to the limb in the same nerve. The stimulation creates both antidromic (distal to proximal, i.e., toward the spinal cord) and orthodromic (proximal to distal) impulses. Once the antidromic response reaches the motor neuron cell bodies, a reflex compound muscle action potential (CMAP) response called the F-wave travels back distally down the nerve. The time difference measured between when the orthodromic response reaches the distal recording electrode, and when the F-wave reaches the recording electrode is the latency. The latency is then used to determine the conduction velocity between the spine and the distal nerve.
The H-reflex is a measurement of both the afferent and efferent reflex aspects of the peripheral nerves. In this case, the sensory nerve is stimulated (the afferent impulse), and the reflex motor response (the efferent impulse) is measured.
EMG/NCS Utilization in Practice
While cervical radiculopathy is often due to nerve root compression in the cervical spine from either a disc herniation or other spondylotic compression, there are several other entities that could present with a similar clinical constellation of symptoms. A detailed physical examination by a well-trained clinician should achieve a high level of certainty as to the clinical diagnosis when attempting to differentiate between cervical radiculopathy and median or ulnar entrapment neuropathy. However, the first-line diagnostic test of choice may be more of a function of the specialty of the physician to whom the patient presents. Those presenting to a neurologist may be sent first for electrophysiologic testing, while those presenting to a primary care physician or spinal specialist may obtain MRI or imaging studies as the first-line test.
Other pathologies that should be in the differential diagnosis include entrapment neuropathies of the upper limb, such as median neuropathy at the wrist or ulnar neuropathy at the elbow, idiopathic brachial neuritis or plexitis, radiation plexopathy, intramedullary spinal cord lesion or neoplasm, multifocal motor neuropathy, diabetes mellitus, thoracic outlet syndrome, leptomeningeal carcinomatosis, or other inflammatory polyneuropathies. While these are less common, the clinician must keep other potential causes of such symptoms in the differential diagnosis until it is reasonable to rule them out.
One of the most common indications for EMG/NCS in the clinical setting is the differentiation between cervical radiculopathy and entrapment neuropathies, such as carpal tunnel syndrome and ulnar neuropathy, or as a confirmation tool for evaluation of peripheral neuropathy.
In the case of median neuropathy at the wrist, or carpal tunnel syndrome, the presentation may be similar to that of a distinct C6 radiculopathy. While there is a similar sensory deficit in both cases, primarily involving the thumb, index, and middle fingers, there is a specific difference between the motor involvement of the two different entities. Median neuropathy will cause a motor deficit of the abductor pollicis brevis, innervated by the recurrent branch of the median nerve. The recurrent branch of the median nerve splits off distal to the carpal tunnel. However, a C6 nerve root compression will also affect the postaxial muscles of the forearm, specifically the brachioradialis. On clinical examination, a Tinel’s sign at the wrist, as well as Phalen’s sign, exacerbates the signs and symptoms of median neuropathy, but will not do so for a patient with cervical radiculopathy. In addition, a Spurling’s maneuver may be positive in the patient with cervical radiculopathy, but not in the patient with median neuropathy at the wrist.
Distinguishing between ulnar neuropathy at the elbow and C8 radiculopathy is another common indication for EMG/NCS testing. In general, the sensory difference between the two entities is that ulnar neuropathy will cause sensory loss in the fifth digit and the medial aspect of the fourth digit, while a C8 radiculopathy will affect the entire fourth digit. This is a relatively small difference in sensation, and in some cases, the variability in the overlapping dermatomes may account for such a difference. However, isolated ulnar neuropathy should not have a component of axial neck pain, which one would expect with a cervical radiculopathy.
Interpretation of Results
In general, the literature supports the utilization of needle EMG for evaluation of cervical radiculopathy and NCS in the evaluation of entrapment neuropathy. The American Association of Electrodiagnostic Medicine performed a literature review and made practice guidelines for electrophysiologic testing in 1999 [5]. These guidelines state that for a properly performed EMG, examination should be performed of at least one muscle innervated by the C5, C6, C7, C8, and T1 spinal roots in a symptomatic limb, and cervical paraspinal muscles in at least one or more levels as appropriate to the clinical presentation. If there is suspicion for a radiculopathy of a specific root, it is recommended that one of two additional muscles innervated by the suspected root be examined or demonstration of normal muscles above and below the involved root. These guidelines also recommend that at least one motor and one sensory NCS should be performed in order to determine if concomitant polyneuropathy or nerve entrapment exists.
The effectiveness of EMG/NCS is highly dependent upon having a specially trained physician perform the test, as well as a clinician who is able to apply the results of the test to the patient’s clinical scenario. It is imperative that the entire report be read by the clinician, to ensure that the results are based on conduction differences in distal muscles affected by a specific nerve root, rather than just on denervation of paraspinal muscles. If an EMG report states that a specific cervical radiculopathy is present, and that result is based purely on paraspinal muscle denervation, that result should be viewed with suspicion. Paraspinal musculature has overlapping innervation throughout the spine. To be able to delineate an isolated cervical radiculopathy based purely on paraspinal denervation is highly suspect, as EMG testing is not performed with any concurrent radiographic imaging which would corroborate which nerve would innervate a specific portion of the paraspinal musculature. One study [6] showed that positive sharp waves were present in 92% of patients older than 40 years, and fibrillations were present in 8% of those patients. These findings were not found in patients under 40 years old. Date et al. [7] showed positive sharp waves in 12% of the paraspinal muscles of asymptomatic patients. These findings exemplify how EMG changes in the paraspinal musculature may be erroneous and should not be the sole criteria for a positive EMG test. However, positive findings in the paraspinal muscles when combined with findings in the extremities increase the sensitivity for cervical radiculopathy [8]. In addition, in the setting of a patient who has undergone a prior surgical procedure through a posterior cervical approach, the cervical paraspinal musculature will be partially denervated from the prior surgical procedure. Therefore, in patients who have undergone a prior posterior cervical surgical procedure, the utilization of EMG changes in the paraspinal musculature of limited value in determining a specific cervical radiculopathy.
Specific EMG and NCV changes will be seen in various pathologies. As mentioned above, entrapment neuropathy at the wrist or elbow will cause decreased motor latency as well as decreased conduction velocity distal to the area of entrapment. Radiation plexopathy will display myokymia, or spontaneous discharges accompanied by wavelike muscle quivering. Multifocal motor neuropathy will cause reduction in CMAP at proximal sites compared to distal sites, with multifocal conduction block, decreased velocities, prolonged terminal latencies, and delayed or absent F-waves. Sensory NCS will be normal across the same segments. Diabetes mellitus causes abnormal spontaneous potentials, positive sharp waves, decreased CMPA amplitude, and fibrillation potentials on EMG while also causing slowing of the nerve conduction velocities due to demyelination.
Sensitivity and Specificity
In the abovementioned literature review, 22 articles provided data which addressed the diagnostic value of needle EMG confirmation [5]. These studies showed that needle EMG examination provided confirmation of cervical root pathology in patients with signs and symptoms of cervical radiculopathy in 30–72% of cases. In studies based on patients with clear neurological or radiological signs, sensitivity was estimated between 50% and 71%. It was shown that needle EMG abnormalities highly correlated with motor weakness. In patients with motor weakness, EMG findings correlated with imaging studies in 65–85% of cases. This shows that needled EMG testing confirms the diagnosis of cervical radiculopathy with a moderate degree of sensitivity and a high degree of specificity. For the well-trained clinician, the more severe of a radiculopathy that is present, the less likely a confirmatory electrophysiologic test will be required.
However, in a study by Askhan et al. [9] comparing the sensitivity for MRI and neurophysiological studies in diagnosing cervical radiculopathy, it found that MRI was predictive 93% of the time, compared to 42% for EMG. The positive predictive values were similar between MRI and EMG (91% vs. 85%); however, the negative predictive value was higher in MRI (25% vs. 7%). Alwari et al. [10] performed a small prospective study to attempt to determine whether EMG could accurately predict outcome in patients undergoing anterior cervical fusion. In 20 patients who were described as having borderline surgical findings on preoperative CT myelogram, those who underwent a preoperative EMG that confirmed radiculopathy had a better postoperative Prolo score than those that did not (p = 0.001). However, this study should be viewed with trepidation, as the Prolo scale is a non-validated outcome measure, and in this study, reviewers were unblinded for outcome measure and patient selection. Therefore, based on this information, EMG/NCS should be used as a supplemental diagnostic test and not as a replacement for a detailed physical examination or imaging.
In the clinical setting, the surgeon must determine if EMG/NCS testing will change his or her clinical decision-making. If the clinician has an imaging study that shows a specific neural compressive lesion which would correlate with the patient’s presenting signs and symptoms, he or she must determine if there is enough uncertainty in the cause of the symptoms to warrant the additional electrophysiologic testing. Considerations that should be made prior to ordering the test include the delay in care due to the time taken to order, schedule, and obtain the results of the test, the additional cost of obtaining the EMG, as well as the discomfort caused to the patient during the test.
Evoked Potential Studies
Somatosensory evoked potentials and motor evoked potential recordings may further delineate the extent of pathology in patients with cervical spondylotic disease. SEPs are recorded after the electrical stimulation of a nerve in either the upper or lower extremity. In the lower extremities, the posterior tibial nerve, sural nerve, or common peroneal nerve are used, while in the upper limb, the median, radial, and ulnar nerves are used. In patients with cervical myelopathy, diminished SEPs from the posterior tibialis are used for diagnosis. In patients with radiculopathy, several nerves supplied by different spinal segments must be used to ascertain the appropriate level [11].
Motor evoked potentials, first described by Baker in 1985 [12], involve transcranial stimulation of the cerebral cortex with short magnetic pulses that stimulate the peripheral nerves and then record muscle action potentials from muscles in the upper and lower extremities. Muscles typically tested during MEPs are abductor pollicis, adductor minimi, quadriceps, tibialis anterior, gastrocnemius, extensor halluces, and abductor hallucis. Again, segmental innervation of the muscles determines the level affected. In general terms, MEPs measure efferent signals, while SEPs measure afferent signals.
SEPs and MEPs are most often used intraoperatively to monitor electrophysiologic changes during surgical intervention. While these studies may be obtained in the preoperative setting, the availability of MEPs and SEPs in the preoperative setting may be limited when compared to the availability of EMGs. As mentioned previously, the surgeon must take into account whether the diagnosis and appropriate surgical treatment will be altered by ordering such studies.
Some studies have utilized transcranial MEPs as a screening tool or confirmatory test in the evaluation of patients with cervical myelopathy. Lo et al. [13] evaluated the sensitivity and the specificity of MEPs in relation to the severity of pathology present on MRI. The purpose was to show that MEPs could be used as a rapid, inexpensive, and noninvasive screening tool prior to obtaining imaging with MRI. This study grouped 231 patients into 4 cohorts based on the severity of cord compression on MRI. Group 1 had spondylosis with or without contact with the cord, but no cord deformity. Group 2 showed mild indentation or flattening of the cord, with AP cord diameter not less than two-thirds of the original size. Group 3 showed significant cord indentation with AP cord diameter less than two-thirds of the original size, with absence of hyperintense T2 cord signal. Group 4 had indentation of the cord, with AP cord diameter less than two-thirds of original, with hyperintense T2 cord signal present. Transcranial MEPs were obtained in these patients and compared to the results of 45 control patients. As expected, patients who had more severe pathology (groups 3 and 4) had significant findings on physical examination and correlated over 90% of the time. However, for less severe pathology (group 2), correlation was 70%. EMG correlation was approximately the same as physical examination, which is not unexpected, as EMG is utilized for radiculopathy rather than myelopathy. When MEPs were positive in all four parameters used, there was high sensitivity in patients in group 2, as well as groups 3 and 4.
The basis for these findings may be that myelopathy, especially from anterior compression syndromes, will produce abnormalities in the corticospinal tract which are seen on MEPs, rather than from compression of the dorsal columns.
SSEPs and MEPs have also been studied as a predictor of progression of cervical spondylotic myelopathy or as a predictor of conservative vs. surgical outcomes. Bedarnik et al. [14] showed that cord dysfunction detected by SSEPs or MEPs was associated with early development of myelopathy (less than 12 months), while the presence of T2 hyperintense cord signal abnormality predicted later progression (more than 12 months) to symptomatic myelopathy. This indicates that MEP and SSEP changes, i.e., electrophysiologic changes, occur early in the pathogenesis of myelopathy, while T2 cord signal abnormality may be a sign of prolonged cord compression. In terms of prediction of outcome, Kadanka et al. [15] performed a 3-year prospective randomized study that evaluated outcome in conservatively and surgically treated patients with myelopathy in relation to clinical, electrophysiological, and imaging parameters. Those that had a good outcome when treated conservatively were those of older age and normal MEPs and those with a larger transverse area of the spinal cord (over 70 mm2). Those that had a good outcome when treated surgically had a worse modified JOA score and slower walk and thus more severe myelopathy. This would indicate that the more severe that cord compression is at presentation, the more likely it is that surgery will be necessary as treatment.
Mazur et al. [16] looked at MEPs as an objective measure of improvement of cervical myelopathy after surgery, which may be more appropriate than as a diagnostic or predictive tool. While only 17 patients were evaluated in this study, patients underwent MEP evaluation before surgery and at 1, 3, 6, and 12 months after surgery. Other objective tests were performed as well, including the 10-m walk test, the 9-hole peg task, and grip and release test. It was found that the MEPs correlated with these objective tests both before and after surgery and suggested that MEPs could be used to monitor disease severity and recovery of neurological function before and after surgical intervention. It was also shown that prolonged baseline MEPs were associated with worse surgical outcome, most likely due to worse myelopathy prior to surgery.
However, MEPs do not provide an anatomic picture that can be used for surgical planning. Therefore, the surgeon will need to take the entire clinical picture into account to determine if MEPs would change the course of clinical action if a patient is suspected of having cervical compression.
Cervical Transforaminal Selective Nerve Root Blocks
Cervical epidural steroid injections are a frequent treatment modality in patients with cervical radiculopathy. It is most commonly used in patients who have mild to moderate nerve root compression with signs and symptoms consistent with radiculopathy, rather than in those with large disc herniations or severe nerve root compression, in whom surgery would be a more appropriate and definitive treatment option.
The two approaches for epidural steroid injections are translaminar and transforaminal. In the cervical spine, the translaminar approach can be performed safely and in most cases in the office setting. This approach is effective, and in addition, the injected medication can cover more than one level of the cervical spine, as it spreads through the epidural space.
The transforaminal approach allows the physician to place the tip of the needle in the foraminal space, thus applying steroid medication to just one exiting nerve root, rather than multiple. In this way, this injection can be both therapeutic and diagnostic. If there is question as to which specific nerve root is causing the patient’s radicular symptoms, a transforaminal selective nerve root block may be performed. If the patient experiences relief with a transforaminal selective nerve root block, even temporary, then that block may confirm the presence of the causative radiculopathic agent at the site of the transforaminal injection. However, if the patient received no benefit from such an injection, then consideration should be given to other potential causes of the symptoms.
However, the transforaminal approach for selective nerve root blocks has increased the risk of complication than the translaminar approach. Due to the location of the vertebral artery in such close proximity to the foramen, there is a higher risk of inadvertent injection or damage to the vertebral artery. Therefore, some practitioners will utilize CT guidance during these injections in order to reduce the risk of vertebral artery injection. Fitzgerald et al. [17] reviewed the position of the vertebral artery relative to the typical injection point for a transforaminal injection at 70 cervical levels in 68 patients. It was found that the more advanced the foraminal degenerative narrowing present in a patient, the higher the risk of the vertebral artery compromising the course of the injection. The needle trajectory intersected with the vertebral artery in 46% of injections. Using oblique fluoroscopic technique, the trajectory intersected with the vertebral artery in 39%. In patients with severely narrowed foramen, 65% of patients had complete or near-complete covering of the foramen.
Diagnostic transforaminal selective nerve root blocks are done with far more frequency in the lumbar spine due to the lower risk of complications, and some pain management physicians will therefore not perform transforaminal injections in the cervical spine. When considering obtaining a cervical transforaminal selective nerve root block, the surgeon must take into account how useful this injection will be in determining the treatment in relation to the risk of such an injection, as well as the availability of a practitioner willing and capable of performing such an injection.
Other Diagnostic Tests
While there are other tests that may be of use in the diagnosis of cervical radiculopathy or entrapment neuropathy, they are of limited value at this point in time. Recently, advanced imaging studies of the peripheral nervous system have been utilized, including high field strength MRI and ultrasound. Recent advances in MRI and ultrasound now have been shown to have the ability to demarcate nerve compression and inflammatory conditions within the extremity. In the case of MRI, signal changes on T2-weighted sequences of the peripheral nerve can show demyelinating segments or inflammatory changes that were not previously seen with lower strength magnets [18]. Newer, high strength ultrasound can also see localized edema in larger peripheral nerves in patients with localized nerve inflammation. However, the clinician must make the determination of whether this testing will alter the clinical course prior to obtaining such a study.
Finally, provocative cervical discography is a controversial diagnostic test utilized to determine if the degeneration of the disc itself is a causative agent for axial neck pain. Typically, when this test is being performed, it is for a patient with axial neck pain without radicular or myelopathic signs or symptoms, in order to justify a surgical procedure. While there are some studies that have shown that a positive discogram can lead to good results for patients undergoing a cervical fusion [19], there are many confounding factors that can lead to a high false-positive rate, both in the cervical and lumbar spine [20]. While the degeneration of cervical discs may cause spondylotic changes such as disc osteophyte complexes which result in nerve root or spinal cord compression, these anatomical entities which cause radiculopathy or myelopathy should be the indication for surgical intervention, rather than studies such as a discogram.
Conclusion
The indication for surgical intervention for the patient should be based upon the patient’s presenting symptoms and physical signs, as determined by a detailed history and physical examination and by their correlation with appropriate imaging studies such as MRI and CT myelogram. In cases where there is a diagnostic quandary in terms of either which cervical nerve root is responsible for the clinical syndrome or whether there is another causative agent that cannot be definitively eliminated from the differential diagnosis by physical examination or imaging (i.e., entrapment neuropathy or peripheral neuropathy), then electrophysiologic testing such as electromyography and nerve conduction studies may be a useful adjuvant to ensure that the appropriate surgical intervention is being performed. When considering a diagnostic cervical selective nerve root block, the surgeon must take into consideration the additional risk of vertebral artery injury using a transforaminal approach, as well as the availability of a pain management physician willing and able to perform such an injection. These tests should be used as a supplement to the physician’s history, examination, and clinical judgment and not as a replacement or substitution for a detailed physical examination.
References
Radhakrishnan K, Litchy W, O’Fallon W, et al. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain J Neurol. 1994;117(Pt 2):325–35.
Nouri A, Teteault L, Sing A, Karadimas S, Fehlings M. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine. 2015;40(12):E675–93.
American Association of Neuromuscular & Electrodiagnostic Medicine. Position statement: who is qualified to practice electrodiagnostic medicine? Muscle Nerve.1999;(Suppl. 8):S263–265.
Hakimi K, Spanier D. Electrodiagnosis of cervical radiculopathy. Phys Med Rehabil Clin N Am. 2013;24:1–12.
American Association of Electrodiagnostic Medicine, American Academy of Physical Medicine and Rehabilitation. The electrodiagnostic evaluation of patients with suspected cervical radiculopathy: literature review on the usefulness of needle electromyography. Muscle Nerve. 1999;22(Supplement 8):S213–221.
Gilad R, Dabby M, Boaz M, et al. Cervical paraspinal electromyography: normal values in 100 control subjects. J Clin Neurophysiol. 2006;23:573–6.
Date ES, Kim B, Yoon JS, et al. Cervical paraspinal spontaneous activity in asymptomatic subjects. Muscle Nerve. 2006;34:361–4.
Dillingham TR, Lauder TD, Andary M, et al. Identification of cervical radiculopathies: optimizing the electromyographer screen. Am J Phys Med Rehabil. 2001;80:84–91.
Ashkan K, Johnston P, Moore AJ. A comparison of magnetic resonance imaging and neurophysiological studies in the assessment of cervical radiculopathy. Br J Neurosurg. 2002;16(2):146–8.
Alrawi MF, Khalil NM, Mitchell P, Hughes SP. The value of neurophysiological and imaging studies in predicting outcome in the surgical treatment of cervical radiculopathy. Eur Spine J. 2007;16(49):5–500.
Dvorak J, Sutter M, Herdmann J. Cervical myelopathy: clinic and neurophysiological evaluation. Eur Spine J. 2003;12(Suppl 2):S181–7.
Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;1(8437):1106–7.
Lo YL, Chan LL, Lim W, Tan SB, Tan CT, Chen JLT, Fook-Chong S, Patnagopal P. Transcranial magnetic stimulation screening for cord compression in cervical spondylosis. J Neurol Sci. 2006;224:17–21.
Bedarnik J, Kadanka Z, Dusek L, Kerkovsky M, Vohanka S, Novotny O, Urbanek I, Kratochvilova D. Presymtomatic spondylotic cervical myelopathy: an updated predictive model. Eur Spine J. 2008;17:421–31.
Kadanka Z, Mares M, Bedarnik J, Smrcka V, Krbec M, Chaloupka R, Dusek L. Predictive factors for mild forms of spondylotic cervical myelopathy treated conservatively or surgically. Eur J Neurol. 2005;12:16–24.
Mazur MD, White A, McEvoy S, Bisson EF. Transcranial magnetic stimulation of the motor cortex correlated with objective clinical measures in patients with cervical spondylotic myelopathy. Spine. 2014;39(14):1113–20.
Fitzgerald RT, Bartynski WS, Collins HR. Vertebral artery position in the setting of cervical degenerative disease: implications for selective cervical transforaminal epidural injections. Interv Neuroradiol. 2013;19(4):425–31.
Stoll G, Wilder-Smith E, Bendszus M. Imaging of the peripheral nervous system. Handb Clin Neurol. 2013;115:137–53.
Motimaya A, Arici M, George D, Ramsby G. Diagnostic value of cervical discography in the management of cervical discogenic pain. Conn Med. 2000;64(7):395–8.
Carragee EJ, Tammer CM, Khurana S, Hayward C, Welsh J, Date E, Truong T, Rossi M, Hagle C. The rates of false-positive lumbar discography in select patients without low back symptoms. Spine (Phila Pa 1976). 2000;25(11):1373–80; discussion 1381.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Case Review: GM 3-28-68
Case Review: GM 3-28-68
Patient GM is a 49-year-old male construction worker who presented primarily with neck pain and radicular pain down both arms. He has had a chronic history of numbness in both of his hands, but that has been getting worse. He now wakes up in the middle of the night and shakes out his hands. The pain in his neck started approximately 2 months prior to presentation. There was no traumatic inciting event. He has been taking tramadol and Celebrex for the past 6 weeks and has not done any therapy, injections, or chiropractic manipulation. He is otherwise healthy but does smoke 1 pack per day for 35 years. The patient had already obtained both an EMG and an MRI prior to presenting to his surgeon.
On examination, the patient has no focal motor deficits. He has non-dermatomal sensory loss that involves all of his fingers except for his fifth digit. His reflexes are 1+ and symmetric, and he has no Hoffman’s sign. He has a positive Tinel’s sign bilaterally and a positive Phalen’s test.
The patient presented with an EMG which showed bilateral median neuropathy at the wrist, but no acute cervical radiculopathy. There was no spontaneous insertional activity in any of the tested muscles. On the right side, the nerve conduction velocity across the wrist was 35.1 M/s, compared to 62.1 M/s proximal to the wrist. On the left side, the nerve conduction velocity was 34.7 M/s across the wrist, compared to 64.2 M/s proximal to the wrist.
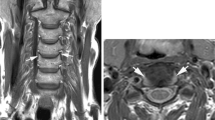
His MRI is shown below in Fig. 10.3. He has a C5–C6 disc osteophyte complex which causes significant central canal stenosis and bilateral neural foraminal stenosis.
As the patient was clearly symptomatic from both his C5–C6 disc osteophyte complex and his longstanding bilateral median neuropathy at the wrist, he ultimately underwent both an anterior cervical discectomy and fusion at C5–C6 and also bilateral carpal tunnel release. Due to the patient’s smoking history and the increased risk of pseudoarthrosis, the patient first underwent a right carpal tunnel release while he underwent smoking cessation. Three weeks later, he underwent a C5–C6 anterior cervical fusion and then, 2 weeks after that, a left carpal tunnel release. Now 3 months out from his first surgery, the patient has minimal neck pain, has had complete resolution of his radicular arm pain as well as the longstanding numbness in his hands, and has returned to work.
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Eichholz, K.M. (2019). Alternative Diagnostic Tools. In: Kaiser, M., Haid, R., Shaffrey, C., Fehlings, M. (eds) Degenerative Cervical Myelopathy and Radiculopathy . Springer, Cham. https://doi.org/10.1007/978-3-319-97952-6_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-97952-6_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97951-9
Online ISBN: 978-3-319-97952-6
eBook Packages: MedicineMedicine (R0)