Abstract
The arrival of a patient with imbalance can often lead to a silent groan from the treating otolaryngologist. Often it is easy to conclude the clinic visit with “your imbalance is multifactorial” without precisely identifying the contributing factors. Computerized dynamic posturography (CPD) attempts to replicate real-life balance disturbances in an effort to objectively identify potential causes of imbalance. Testing specifically identifies weakness in somatosensory input, visual input, vestibular input, and overall compensation to give a complete picture of a patient’s control of posture. This chapter aims to provide an overview of the techniques and findings of CPD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Postural response and subsequent balance have always been difficult to analyze and isolate. Initial attempts involved testing somatosensory input under eyes-closed and eyes-open conditions to look for postural sway [1]. This involved the patient standing on a force plate to quantitatively measure the center of vertical forces exhibited by the patient and, thereby, the patient’s center of gravity (COG). Using the COG and the center of vertical force, characteristics of the patient’s sway and functional compensation can be examined to look for postural disturbance [2]. However, testing via this method can be consciously manipulated and is highly dependent on patient cooperation.
Further attempts have aimed to provide diagnostic information independent of the patient’s willingness by measuring discrete evoked postural responses. This is usually achieved by causing periods of stability alteration by rotating the standing surface. Measurements from these toes-up or toes-down positions give valuable information about the latency, strength, and pattern of the neurological response.
Computerized dynamic posturography (CDP) is a method that aims to combine the results from the static conditions of performance testing with those from the dynamic postural responses. Typically CDP has four main functional protocols: the posture-evoked response (PER), the motor control test (MCT), the adaptive protocol (ADP), and the sensory organization test (SOT).
Posture-Evoked Response (PER)
Description of Test
The PER utilizes support surface rotations to cause gastrocnemius and anterior tibialis muscle stretch bilaterally [3]. Muscle response to these actions is then measured via surface electromyography (EMG). With rapid dorsiflexion of the ankle (toes up), the gastrocnemius muscle is stretched, stimulating an EMG response. When rapid plantar flexion occurs (toes down), the anterior tibialis muscle provides a response [1]. Testing with toes-up and toes-down movements occurs randomly at high velocity and is usually repeated up to 20 times.
Under normal circumstances, after a support surface rotation, short-latency and medium-latency responses in the above muscles initially exaggerate the sway disturbance. In a non-dizzy patient, loss of balance is then prevented by the stabilizing long-latency component. EMG readings can identify the presence of these responses and be analyzed. PER testing gives qualitative leg- and muscle-dependent information about the presence, duration, and onset of each of these responses.
Depiction of Results
Averaged responses from multiple attempts will usually be shown as a graph with SL, ML, and LL marked, corresponding to the short-latency, medium-latency, and long-latency responses, respectively. In addition, the responses will often be annotated with the numbers 1 (onset of the response) and 2 (the end of the response). Abnormal responses will be illustrated by delayed onset or absence.
-
1.
SL: Corresponds to the monosynaptic stretch reflex system [4] and are not seen after stretching the anterior tibialis muscles [1]. Normal latencies of the SL response are 32 ms [1].
-
2.
ML: Can be absent in non-dizzy patients but, when present, will represent the polysynaptic segmental reflex mechanisms [5]. These are present in both muscles and typically activate around 80 ms [1].
-
3.
LL: Origin remains controversial, but the response usually occurs at 110 ms in both muscles [1, 6, 7].
Motor Control Test (MCT)
Description of Test
The MCT involves a patient standing on a force plate that is displaced anteriorly or posteriorly at different velocities to elicit autonomic postural responses. Under normal conditions, when the standing surface is moved horizontally, the patient’s COG will initially be stationary, and the patient will rotate at the ankles, (i.e., the patient will lean forward or backward) [7]. Stretch of the gastrocnemius muscle (when the baseplate is moved backward and the patient leans forward) or anterior tibialis muscle (when the force plate moves forward and the patient leans backward) [1] elicits compensation to remain upright [7].
Autonomic postural responses are examined by testing a range of conditions by varying the velocity, displacement of the footplate, and timing. This random testing decreases the chances of biasing the results. Each specific condition is repeated three times for an average result. Typically, responses of both legs to movement forward and backward are analyzed separately to localize which part of the individual pathways may be affected. Compensatory forces and the proportion of total body weight distributed by each foot can also be recorded.
Depiction of Results
Graphical results such as those in Fig. 7.1 will be seen for backward and forward movement in addition to each leg, typically COG sway, horizontal shear force, and left and right center of vertical force responses. Three plots for each of the above conditions are provided, with normal results falling in the unshaded areas. Typical results include:
-
1.
Weight symmetry: Indicates the percentage of total body weight on each leg during the postural response. A score of 100 means the weight is distributed equally between both legs, while a score of 0 or 200 means none or all of the weight is borne by that leg, respectively [1].
-
2.
Active force latency: Measures the time it takes for the postural responses to be enacted after medium or large displacements of the support surface. Typically, a latency score (2–4) will also be displayed, with 4 representing the most consistent results. Latency increases with age and during the medium displacement [1].
-
3.
Active force strength: Measures the force exerted to restore the patient to an upright position. Typically, each leg will be measured separately, and results between the two legs and anterior and posterior direction will be similar.
Adaptive Protocol (ADP)
Description of Test
The ADP is similar to PER testing except the toes-up and toes-down movement of the support surface is at a much slower rate. The slower velocities enable the autonomic nervous system to enact adaptive responses that are not witnessed during the MCT. Response testing is repeated five times to look for adaption. Initially, the patient is not expecting the first toes-up/toes-down rotation and is unable to stabilize the COG by swaying at the ankle. Patients with normal postural control may show large variances in COG sway during this first displacing movement but will usually not fall over. By the fifth toes-up/toes-down movement, non-dizzy patients will be able to anticipate the rotation [8]. During these last rotations, autonomic responses are enacted to increase the resistance of the ankles and overall stability.
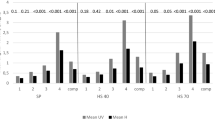
Depiction of Results
COG is expressed as sway energy scores during the adaptive periods following a rotation. Scores typically decrease from the first to the fifth rotation as can be seen in the example in Fig. 7.2. Graphs of sway energy will also illustrate shaded areas, which represent responses outside the normal distribution. Impairment of central processing, reduced muscle strength, or limited mobility at the ankles may be responsible for abnormal adaptive responses.
Sensory Organization Testing (SOT)
Description of Test
SOT aims to evaluate the patient’s ability to utilize information provided by the visual, vestibular, and somatosensory systems to maintain posture. Testing is performed by a method called sway referencing, where somatosensory and/or visual inputs are disrupted. Sway referencing is accomplished by tilting the support surface and/or visual surround to follow the anteroposterior (AP) sway of the patient [9]. Although information is still received from these senses, the body perceives no change in position relative to gravity due to the altered conditions and inputs. The non-dizzy patient ignores this “inaccurate” information provided by the sway-reference sense and maintains balance via other senses [1].
During the testing protocol, patients are exposed to six sensory conditions with increasing difficulty for adaptation [9]:
-
1.
Eyes open and support surface fixed.
-
2.
Eyes closed and support surface fixed.
(Both of the above conditions provide baseline measurements.)
-
3.
Visual input is sway referenced, and support surface is fixed.
-
4.
Eyes open and support surface is sway referenced.
-
5.
Eyes closed and support surface is sway referenced
-
6.
Both visual input and support structure are sway referenced.
This protocol is repeated three times for each condition to improve reliability and identify if the patient can compensate for altered conditions. In addition to the COG sway, another measure of stability, the equilibrium score, is measured for each trial. The equilibrium score is found by comparing the peak amplitude of AP sway to that experienced by the matched non-dizzy population. This is expressed as a percentage, with 100 representing perfect balance and 0 indicating loss of balance.
Depiction of Results (Fig. 7.3)
The first graph typically shows the equilibrium scores for each trial under the six sensory conditions. Results that are below the fifth centile of an age-matched sample are seen as the notched aspect of the graph. The final column in the graph shows the composite equilibrium score, which is the best representation of a patient’s performance. This composite score places more emphasis on the results of conditions 3 through 6 than 1 and 2.
Sensory organization analysis characterizes the specific cause of the patient’s balance disturbance, with results indicating the contribution of particular senses. This is identified by analyzing the averaged equilibrium scores of one condition compared to that of another condition.
-
1.
The somatosensory ratio quantifies the effect of balance when eyes are closed on a stationary platform by comparing conditions 1–2.
-
2.
The visual ratio compares conditions 4 and 1 by removing the somatosensory input.
(For both of the above ratios, if the vestibular input is used, instead of the somatosensory or visual input, the sway ratio would remain large. Therefore, an abnormal [lower than normal] ratio would indicate an abnormality of the mentioned senses [1].)
-
3.
The vestibular ratio compares conditions 5 and 1 and occurs when both the visual and somatosensory inputs are disrupted.
-
4.
The vision preference compares conditions 3 and 6 with the sum of conditions 2 and 5. This compares the balance with eyes open and closed when the visual input and platform is sway referenced.
Strategy analysis examines the contribution of the hip and ankle to the sway and movement of the patient. Normal results are found within a diagonal area of the graph. Typically, when the sway is small, ankle movement will be used to compensate, with hip movement used prior to loss of balance.
COG is also illustrated by plotting the AP and lateral COG positions of all trials. Points located superior to the center of the plot indicate a COG forward on the support structure, while those inferior reflect a more posterior position on the platform. Points left or right correspond to lateral displacement of the COG.
Conclusion
CDP can give the physician objective information about a patient’s postural control by examining their motor control, sensory input, and adaption. Results can be used to examine a patient’s functional impairment or localize the areas contributing to loss of balance. Together with clinical acumen, they may help diagnose postural instability and tailor treatments for individual patients.
References
Nasher L. Computerized dynamic posturography. In: Jacobson GP, Shepard NT, editors. Balance function assessment and management. 2nd ed. San Diego: Plural Publishing; 2014. p. 451–76.
Blaszczyk JW. The use of force-plate posturography in the assessment of postural instability. Gait Posture. 2016;44:1–6.
Diener HC, Horak FB, Nasher LM. Influence of stimulus parameters on human postural responses. J Neurophysiol. 1988;59(6):1888–905.
Jacobs JV, Horak FB. Cortical control of postural responses. J Neural Transm. 2007;114(10):1339–48.
Dietz V, Quintern J, Berger W. Cerebral evoked potential associated with the compensatory reactions following stance and gait disturbance. Neurosci Lett. 1984;50(1–3):181–6.
Berger W, Dietz V, Quintern J. Corrective reactions to stumbling in man: neuronal co-ordination of bilateral leg muscle activity during gait. J Physiol. 1984;357:109–25.
Nasher LM. Fixed patterns of rapid postural responses among leg muscles during stance. Exp Brain Res. 1977;150:403–7.
Nasher LM. Adapting reflexes controlling the human posture. Exp Brain Res. 1976;26(1):59–72.
Nasher LM, Black FO, Wall C. Adaption to altered support and visual conditions during stance: patients with vestibular deficits. J Neurosci. 1992;2(5):536–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Allsopp, T.J., Dornhoffer, J.L. (2019). Dynamic Posturography. In: Babu, S., Schutt, C., Bojrab, D. (eds) Diagnosis and Treatment of Vestibular Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-97858-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-97858-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-97857-4
Online ISBN: 978-3-319-97858-1
eBook Packages: MedicineMedicine (R0)