Abstract
Leukocyte (WBC) to endothelial cell (EC) adhesion is a receptor-mediated process governed by the avidity and affinity of selectins, which modulate adhesive forces during WBC rolling, and integrins, which determine the strength of firm adhesion. Adhesion receptors on the EC surface lie below an endothelial surface layer (ESL) comprised of the EC glycocalyx and adsorbed proteins which, in vivo, have a thickness on the order 500 nm. The glycocalyx consists of a matrix of the glycosaminoglycans heparan sulfate and chondroitin sulfate, bound to proteoglycans and encased in hyaluronan. Together, these carbohydrates form a layer that varies in glycan content along the length of post-capillary venules where WBC-EC adhesion occurs. Thickness and porosity of the glycocalyx can vary dramatically during the inflammatory response as observed by increased infiltration and diffusion of macromolecules within the layer following activation of the EC by cytokines and chemoattractants. In models of inflammation in the living animal, the shedding of glycans and diminished thickness of the glycocalyx rapidly occur to facilitate penetration by the WBCs and adhesion to the EC. The primary effectors of glycan shedding appear to be metalloproteases and heparanase released by the EC. Retardation of glycan shedding and WBC-EC adhesion has been demonstrated in vivo using MMP inhibitors and low-molecular-weight heparin (LMWH), where the latter competitively binds to heparanase liberated by the EC. Together, these agents may serve to stabilize the ESL and provide a useful strategy for treatment of inflammatory disorders.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
The inflammatory process revolves around a sequence of events that leads to emigration of leukocytes (WBCs) through the microvascular wall into the tissue space. Convective transport of WBCs to the microvasculature leads to their radial migration to the microvessel wall (margination), rolling along the endothelium and firm adhesion to the endothelium (EC) prior to diapedesis (Atherton and Born 1972, 1973; Grant 1973), as depicted in Fig. 1. As blood traverses the arteriolar network, hemodynamic and topographical features promote WBC-EC interaction (Bagge and Karlsson 1980; Braide et al. 1984; Goldsmith and Spain 1984; Schmid-Schonbein et al. 1980). As blood exits from capillaries to post-capillary venules, WBC radial migration to the EC occurs due to hemodynamic forces and red blood cell (RBC) interactions (Schmid-Schonbein et al. 1980). Rolling of WBCs on the EC is then promoted by adhesive interactions with the molecular surface layer on the EC and receptor-mediated adhesion with the selectin family of carbohydrates (Springer and Lasky 1991). Subsequent firm adhesion of WBCs ensues due to receptor-mediated adhesion of integrins on the WBC surface to counter receptors on the EC (Zarbock and Ley 2009; Springer 1990). Successful completion of the adhesion process hinges on the availability of ligands in the EC surface layer (ESL) formed by the EC glycocalyx and adsorbed proteins (Pries et al. 2000; Reitsma et al. 2007; Weinbaum et al. 2007).
Leukocyte-endothelium adhesion in post-capillary venules is an essential step in the inflammatory process. As WBCs exit the capillaries, hemodynamic forces and interactions with red cells cause the radial migration of WBCs to the EC surface (margination) with subsequent rolling along and firm adhesion to the EC. WBC rolling is facilitated by the selectin family of adhesion molecules that maintains WBC contact with the EC surface. Arrest and firm adhesion follow due to the strong adhesion mediated by integrins on the WBC and their receptors on the EC. The selectins and integrin receptors are buried within the endothelial surface layer (ESL) that consists of the EC glycocalyx and adsorbed proteins. The ESL is typically about 500 nm thick and shields selectins and integrin receptors that protrude from 20 to 40 nm above the EC membrane
The interface between blood and endothelium has been of interest for decades in light of its role in inflammation, permeability to macromolecules, and thrombosis. Early studies on the structural makeup of the capillary wall drew attention to the surface of the endothelium as an essential part of the “hematoparenchymal barrier” (Zweifach 1955). The observations of microvascular function recognized that endothelial cells continuously secrete substances that form an “intercellular cement” and the basement membrane. With advances in intravital microscopy, direct visualization of the dynamics of blood-endothelial cell (EC) interactions in the microcirculation led to hypotheses to explain the basis for blood cell to EC adhesion, the clotting of blood, and the transvascular exchange of fluid and macromolecules. It is now recognized that the surface of the endothelium is coated with a layer of polysaccharides and transmembrane proteins, as described in Chap. 1, that was subsequently visualized by electron microscopy by Bennett and others (Bennett et al. 1959; Luft 1966). In view of its predominant polysaccharide constituents, Bennett (Bennett et al. 1959) termed it the “glycocalyx,” as derived from the Latin for “sweet husk.” Initially viewed as an extension of the endothelial cell basement membrane onto the luminal surface of the EC, the fine structure of the glycocalyx has been described as a network of glycoproteins on the order of 50–100 nm thick, with a characteristic spacing of 20 nm that accounts for the resistance to filtration of small molecules (Squire et al. 2001). Recognition that the EC surface contains an abundance of negatively charged carbohydrates (Simionescu et al. 1982) led to the use of lectins to visualize the endothelial surface layer (Schnitzer et al. 1990a). Visualization of the glycocalyx with lectin staining is illustrated in Fig. 2, where the surface of post-capillary venules is stained with the fluorescently labeled lectin BS-1 (Bandeiraea simplicifolia) (Mulivor and Lipowsky 2004). Lectins are carbohydrate-binding proteins that may be used to loosely identify specific glycoproteins in the EC surface layer (Schnitzer et al. 1990b). As shown in Fig. 2a, staining of the glycocalyx reaches a maximum at the vessel walls. The average radial profile of fluorescence along the length of a microvessel reveals a peak intensity that is proportional to concentration of lectin-binding sites on the EC surface. Peak staining along the length of one wall (Fig. 2d) illustrates the variability of glycans on the surface, which may vary ±50% about the mean. As shown in the following, peak intensity of glycan staining may be used to quantify the shedding of glycans during the inflammatory process and changes in glycan concentration with hemodynamic (shear) conditions.
Visualization of the endothelial glycocalyx. (a) Bright-field view of post-capillary venules in mesentery of the rat. (b) Fluorescence microscopy of the glycocalyx labeled with the fluorescently labeled lectin BS-1. (c) The average radial profile of fluorescence along the measurement line R shows a peak value at each wall with intensity proportional to the concentration of lectins bound to the EC surface. Reductions in peak fluorescence were taken as a measure of the shedding of glycans from the EC surface. (d) Variation of fluorescence intensity with length L along a wall varies ±50% as shown for the wall next to the dashed line
2 Microvascular Hemodynamics
Historically, the role of the glycocalyx in affecting microvascular hemodynamics arose from the seminal studies of Klitzman and Duling (1979) and Desjardin and Duling (1990) in their studies of the basis for the anomalous levels of capillary hematocrit observed in most tissues by intravital microscopy. At that time, studies subsequent to the pioneering observations of reduced small vessel hematocrit by Poiseuille (1835) and Fahraeus (1929) noted reductions in capillary hematocrit that were well below 50% of systemic values (Pries et al. 1990; House and Lipowsky 1987a). Average values of capillary hematocrit on the order of 10–20% of systemic hematocrit far exceeded the hypothetical maximum reduction of 50%, based upon red cell velocity profiles in small tubes (Sutera et al. 1970) where, for a parabolic velocity profile, peak velocity along the vessel center line may reach a maximum of twice the mean velocity. Klitzman and Duling (1979) hypothesized that the low capillary hematocrits arose from retardation of fluid on the endothelial cell surface. To validate this hypothesis and explore the role of the glycocalyx in contributing to the anomalous low capillary hematocrits, Desjardin and Duling (1990) inserted finely drawn micropipettes into feeding vessels and perfused individual capillaries with heparinase to strip off the glycocalyx. Their results showed a twofold rise in capillary hematocrit, presumably due to the resultant increase in the effective capillary diameter with degradation of the glycocalyx. Subsequent studies have shown increases in capillary hematocrit in response to its removal by perfusion with hyaluronidase (Cabrales et al. 2007) or degradation due to the presence of reactive oxygen species derived from oxidized LDL (Constantinescu et al. 2001).
To delineate the hemodynamic significance of the glycocalyx insofar as it affects the resistance to blood flow, studies have explored the effects of its enzymatic removal by direct intravital microscopy. Measurements by Pries et al. of regional pressure drops and flows in the mesenteric microvasculature following enzymatic removal of the glycocalyx, by perfusion with heparinase, suggested a 14–20% decrease in the resistance to flow (Pries et al. 1997). Their analysis of this diminished resistance suggested that removal of the glycocalyx theoretically increased microvessel diameter throughout the network by about 1 μm. Consistent with these findings, a hydrodynamically significant glycocalyx has been explicitly shown by analysis of the velocity profiles of small fluorescent microspheres in the in vivo microcirculation using techniques of particle image velocimetry (PIV) (Potter and Damiano 2008; Smith et al. 2003). Within small venules in the exteriorized cremaster muscle, these studies revealed a glycocalyx thickness on the order of about 0.3–0.4 μm which displaces blood flow from the surface of the endothelium. In contrast, similar applications of PIV to analysis of particle flow over cultured human umbilical vein and bovine aortic endothelial cells revealed hydrodynamically significant thicknesses of only 0.03 and 0.02 μm, respectively (Smith et al. 2003). Thus, in vitro models clearly fail to replicate the in vivo structure of the glycocalyx.
3 Structure of the Glycocalyx
As discussed in Chap. 1, several studies to date have reviewed the structure of the endothelial glycocalyx (Pries et al. 2000; Reitsma et al. 2007; Weinbaum et al. 2007; Chappell et al. 2009a; Gotte 2003). Salient features relevant to WBC adhesion may be summarized as follows. The most prominent components of the glycocalyx are the glycosaminoglycans (GAGs) heparan sulfate (HS), chondroitin sulfate (CS), and hyaluronan (HA). The GAGs HS and CS are covalently linked to membrane-bound proteoglycans (PGs). Sulfate groups on HS and CS confer a negative charge to these GAGs. The density of GAGs on PGs and glycoproteins varies considerably (Reitsma et al. 2007), and each PG may carry multiple chains of HS and CS, with a ratio of HS/CS of about 4:1 (Rapraeger 1989), and their sulfation level may change depending on the physiological microenvironment (Rapraeger 1989; Vogl-Willis and Edwards 2004). HA does not possess sulfate groups and is not covalently linked to a proteoglycan core protein but is held in place by specific hyaluronan-binding proteins (Laurent and Fraser 1992). In addition to GAG-carrying proteoglycans, adsorbed blood-borne soluble proteins comprise substantial components of the glycocalyx and may be decreased by removing plasma proteins (Adamson and Clough 1992; Huxley and Curry 1991). Under normal physiological conditions, the structure of the glycocalyx layer is stable, and its molecular composition represents a dynamic balance between continued biosynthesis of new glycans and shear-dependent alterations.
Studies of the dimensions and structure of the endothelial glycocalyx have been confounded by the methods of fixation and source of the cells studied (Pries et al. 2000; Reitsma et al. 2007). In vivo observations by direct microscopy have revealed an apparent thickness of the glycocalyx, estimated by the exclusion of erythrocytes and macromolecules (Vink and Duling 1996), on the order of 400–500 nm, which significantly exceeds the dimensions obtained in either fixed specimens or cultured cells. In vitro models with cultured ECs fail to express a glycocalyx of thickness comparable to that found ex vivo (Chappell et al. 2009a). As shown therein, electron microscopy studies of fixed umbilical vein EC revealed a glycocalyx with an average thickness of 878 nm, whereas cultured HUVECs revealed a glycocalyx thickness ranging from only 29 to 118 nm.
Direct measurement of glycocalyx thickness in post-capillary venules by intravital microscopy is technically challenging. In the case of capillaries with single-file motion of RBCs, the width of the red cell column can be easily distinguished from the anatomical capillary diameter (Vink and Duling 1996) to reveal a distance to the EC surface of about 500 μm. As shown therein, infusion of fluorescently labeled 70 kDa dextran (Dx70) revealed a lesser gap between the edge of the fluorescent column and the EC on the order of 400 nm. With cessation of flow, RBCs could be observed to infiltrate the dextran exclusion space completely with zero gap. Mathematical modeling of fluid flow in the glycocalyx suggests that fluid dynamical pressures generated within the glycocalyx can lead to variations of red cell shape and gap width with flow velocity (Feng and Weinbaum 2000; Secomb et al. 2001) that are consistent with in vivo observations (Vink and Duling 1996). Studies of the width of the molecular exclusion zone in capillaries (Vink and Duling 2000) revealed that the edge of the dye column is both charge and molecule size dependent. However, anionic and neutral Dx70 maintained a discrete distance from the EC surface. Application of such techniques has been applied to measure the thickness of the glycocalyx in venules, where WBC-EC adhesion occurs (Gao and Lipowsky 2010). As shown in Fig. 3a for a 35 μm venule, the RBC column is surrounded by a plasma layer that extends to the outer edge of a dark refractive band on the EC surface. Following the infusion of fluorescently labeled Dx70 (Fig. 3b), the edge of the dye column becomes diffuse due to the relatively large diameter and path length along the optical axis. To objectively demarcate the dye exclusion zone, a sigmoidal fit of the radial intensity distribution was made (Fig. 3c) and the edge of the glycocalyx taken as the location of its inflection point. The thickness of the glycocalyx was calculated as the distance between the inflection point and the outer edge of the dark refractive band.
Measurement of the thickness of the glycocalyx in a 35 μm diameter venule. (a) Bright-field view reveals the plasma layer that surrounds the red cell (RBC) core. A dark refractive band can be seen near the EC surface. The outer edge of this band is at the EC surface. (b) Circulating fluorescently labeled 70 kDa dextran is shown under fluorescence microscopy and infiltrates the gap between the RBC core and EC surface. (c) Radial distribution of dextran fluorescence intensity exhibits a sigmoidal distribution between the RBC column and EC surface (outer edge of the dark refractive band) due to the varying path length along the optical axis. An objective measure of the thickness of the glycocalyx was taken as the distance between the intensity inflection point (IP) and outer edge of the refractive band. (d) Thickness was observed to be significantly (*p < 0.05) reduced following infusion (by micropipette) with either heparanase, chondroitinase, or hyaluronidase and reduced by 90% with a mixture of all three enzymes. Activation of the endothelium with fMLP significantly reduced thickness due to shedding of glycans. Reproduced from Gao and Lipowsky (2010), with permission
Shown in Fig. 3d are measurements of the thickness of this barrier to infiltration of Dx70 under controlled conditions and following infusion of enzymes to remove specific GAGs from the EC surface. Individually, all three major enzymes significantly reduced the layer thickness below its normal 500 μm level, with heparinase having the greatest effect. A mixture of all three enzymes reduced the layer thickness by almost 90%. Accounting for cross-reactivity of the enzymes resulted in (by solving the simultaneous algebraic equations for each GAG) contributions to the thicknesses of the barrier of 43.3, 34.1, and 12.3%, for HS, CS, and HA, respectively. Thus, heparan sulfate appears to represent the major component of the glycocalyx. To simulate changes in the structure of the glycocalyx anticipated in the inflammatory response, the chemoattractant fMLP was topically applied (Fig. 3d) and revealed a significant 28% reduction in glycocalyx thickness that was not significantly different from the losses due to enzymatic cleavage.
Reductions in intensity of lectin staining of the glycocalyx due to fMLP have been correlated with the shedding of glycans (Mulivor and Lipowsky 2004). Loss of glycans has been correlated with increased infiltration of macromolecules in the surface layer in response to the cytokine TNF-α (Henry and Duling 1999, 2000). Quantitative estimates of changes in the porosity of the ESL have been made by calculation of the diffusion coefficients (D) of the small fluorescent molecule fluorescein isothiocyanate (FITC, 350 Da) by applying a 1-D diffusion model to measurements of radial concentration gradients in the ESL (Gao and Lipowsky 2010). By comparison of measured transients in radial intensity of a bolus of FITC with that of a computational model, a diffusion coefficient D was obtained. Values of D were obtained corresponding to the thickness of the layer demarcated by Dx70 (DDx70), and a smaller sublayer 173 nm above the EC surface (D173), prior to and following enzyme infusion and superfusion with fMLP. The magnitude of DDx70 was twice that of D173 suggesting that the glycocalyx is more compact near the EC surface. Chondroitinase and hyaluronidase significantly increased both DDx70 and D173. However, heparinase decreased DDx70 and did not induce any significant change for the D173. These observations suggest that the three GAGs are not evenly distributed throughout the glycocalyx and that they each contribute to permeability of the glycocalyx to a differing extent.
4 Shedding of the Glycocalyx
Functional changes in the barrier formed by the ESL have been observed in response to a broad spectrum of agents. Topical stimulation of the endothelium for prolonged periods (20–120 min) with the cytokine TNF-α results in an increased porosity of the glycocalyx in the absence of WBC-EC adhesion (Henry and Duling 2000). Significant shedding of components of the glycocalyx in coronary vessels has been observed following perfusion of isolated hearts for 20 min with TNF-α, which was lessened by the serine protease inhibitor antithrombin III (Chappell et al. 2009b). Acute activation of the endothelium in post-capillary venules with the chemoattractant fMLP induced a rapid (<5 min) shedding of glycans from the EC surface as evidenced by a loss of lectin-laden microspheres bound to the EC surface (Mulivor and Lipowsky 2004). Shedding of proteoglycans and GAGs from cultured endothelial cells, or their analogs, occurs in response to a broad spectrum of agonists (Park et al. 2000; Colburn et al. 1994; Fux et al. 2009; Ihrcke et al. 1993; Platt et al. 1990, 1991; Fitzgerald et al. 2000). Shedding of heparan sulfate proteoglycans (namely, the ectodomain of syndecans 1–4) occurs in response to endotoxin (Colburn et al. 1994), serine and/or cysteine proteinases (Ihrcke and Platt 1996), complement activation (Platt et al. 1991), thrombin and growth factors (Subramanian et al. 1997), and activation of protein tyrosine kinase by phorbol ester (Fitzgerald et al. 2000). Using hydroxamic acid inhibitors of matrix metalloproteinases, it has been shown that proteolytic cleavage of the syndecan ectodomain results from the convergence of multiple intracellular pathways that activate a cell surface metalloproteinase (Fitzgerald et al. 2000).
In vivo, shedding of the endothelial glycocalyx has been found in response to inflammation (Mulivor and Lipowsky 2004; Henry and Duling 2000), hyperglycemia (Zuurbier et al. 2005), endotoxemia and septic shock (Hofmann-Kiefer et al. 2009), presence of oxidized LDL (Constantinescu et al. 2001), TNFα (Chappell et al. 2009b), atrial natriuretic peptide (Bruegger et al. 2005), abnormal blood shear stress (Gouverneur et al. 2006; Haldenby et al. 1994), ischemia-reperfusion injury (Mulivor and Lipowsky 2004), light-induced production of free radicals (Vink and Duling 1996), and bypass surgery (Rehm et al. 2007; Svennevig et al. 2008). These observations have led to an underlying connection between integrity of the glycocalyx and vascular homeostasis (Mulivor and Lipowsky 2004; Zuurbier et al. 2005).
Shedding of the glycocalyx in response to cytokines and chemoattractants occurs in all three principal divisions of the microvasculature: arterioles (Henry and Duling 2000), capillaries (Constantinescu et al. 2001; Henry and Duling 2000), and venules (Mulivor and Lipowsky 2004; Henry and Duling 2000). To illustrate, shown in Fig. 4 is the intensity of glycans in the ESL stained with a fluorescently labeled lectin (BS-1) in the three principal divisions of the mesenteric microvasculature (rat) (Lipowsky et al. 2011). The normalized intensity is shown under resting conditions and following topical application of the chemoattractant fMLP (10−7 M). About 30% of all lectin-stained glycans were shed from the EC during a 30 min exposure to fMLP. This shedding appears to be accompanied by a significant reduction in thickness in each division (Fig. 4d). Although it has been postulated that such reductions in thickness are insufficient to expose WBC adhesion receptors (Marki et al. 2015), concomitant increases in porosity (Henry and Duling 1999, 2000) and deformability (Padberg et al. 2014; Wiesinger et al. 2013) of the ESL may promote WBC infiltration and adhesion during inflammation.
Shedding of glycans on the EC surface of post-capillary venules in mesentery (rat) in response to topical application of the chemoattractant fMLP (10−7 M) compared to control values obtained with superfusion of the tissue with Ringer’s solution. Glycan concentration was assumed proportional to the intensity of fluorescently labeled lectin (BS-1) on the EC surface and normalized to initial values. Shown are mean values ± SE for arterioles, capillaries, and venules. Intensity of the lectin stain falls rapidly within the first 5 min of onset of the fMLP and steadily decreases during the entire observation period. After 30 min exposure to fMLP, thickness of the glycocalyx decreased significantly (*p < 0.05). Data are mean ± SE. From Lipowsky et al. (2011), with permission
5 Enzymatic Cleavage of the Glycocalyx
With the majority of WBC adhesion receptors situated in post-capillary venules, as, for example, in the case of ICAM-1 (Iigo et al. 1997), shedding of the venular glycocalyx may play an important role in the inflammatory process. The cellular signaling cascades resulting from pathological conditions and initiating shedding of the glycocalyx are not fully understood. However, direct in situ observations of shedding in post-capillary venules suggest that several key enzymes may be responsible for shedding of the glycocalyx components (Mulivor and Lipowsky 2009). Matrix metalloproteases (MMPs) on the surface of the venular endothelium are rapidly activated by superfusion of the mesenteric tissue with fMLP and may be inhibited by superfusion with subantimicrobial doses (0.5 μM) of the antibiotic doxycycline (Mulivor and Lipowsky 2009). The inhibitory activity of doxycycline on shedding results from its direct effect on MMP activation and not by its ability to chelate divalent cations (Lipowsky et al. 2011), as evidenced by inhibition of MMP activation by the zinc-chelating hydroxamic acid inhibitor GM6001, and lack of inhibition by chelation of cations with EDTA. The possible role of doxycycline as a scavenger of reactive oxygen species (ROS) has been raised (Golub et al. 1998). However, direct evidence that ROS cause shedding in response to chemoattractants or cytokines remains to be obtained. In addition, MMP inhibition has been shown to have no effect on ROS-induced shedding (Lipowsky and Lescanic 2013).
Fluid shear stresses acting on the EC surface may affect the structure of the glycocalyx by either disrupting molecular constituents, affecting biosynthesis of new components, or activating proteases and lyases synthesized by the endothelium (Mulivor and Lipowsky 2004; Arisaka et al. 1995). Increased synthesis of GAGs by cultured monolayers of ECs occurs with prolonged exposure to high shear stresses of 15 or 40 dyn/cm2 (Arisaka et al. 1995). These results were in contrast to prior studies that revealed a decrease in proteoglycan synthesis when ECs were cultured under low levels of shear stress (Grimm et al. 1988). In vivo studies of the accumulation of glycans on the surface of post-capillary venules during a 1 h period of ischemia demonstrated a 15–40% increase in glycan content on the surface of the EC (Mulivor and Lipowsky 2004). Upon reperfusion of these venules, this excess of surface glycans was washed out, and glycan levels (indicated by accumulation of lectins on the EC surface) momentarily fell below pre-ischemic (control) conditions before returning to normal levels. This postischemic fall below pre-ischemic levels was inhibited by superfusion of the tissue with pertussis toxin, thus suggesting a G-protein-mediated activation of enzymatic cleavage of GAGs and/or proteoglycans on the EC surface.
The hypothesis that matrix metalloproteinases (MMPs) may alter the endothelial glycocalyx and thus facilitate shedding under pathological conditions is well supported. Matrix metalloproteinases represent a family of over two dozen zinc-dependent proteases that play a role in normal tissue remodeling during bone growth, wound healing, reproduction, cancer, inflammation, and cardiovascular disease (Spinale 2007). MMPs (−1 and − 9) serve to cleave the endothelial insulin receptor and CD18 on leukocytes in the spontaneously hypertensive rat (DeLano and Schmid-Schonbein 2008). Oxidative stress in the diabetic heart may activate MMP-2 and lead to the development of diabetic cardiomyopathy (Yaras et al. 2008). Modification of the extracellular matrix by MMPs has been shown to be a critical step in angiogenesis (Haas et al. 2000) and atherosclerosis (Li et al. 1996). MMP-2, MMP-7, and MMP-9 were shown to be capable of directly cleaving chondroitin sulfate (Gronski et al. 1997). In addition, MMP-1 was shown to cleave the heparan sulfate proteoglycan syndecan-1 (Endo et al. 2003). MMPs can be stored within and released by the endothelium. It has been shown (Taraboletti et al. 2002) that both the active and proactive forms of MMP-2 and MMP-9 are stored in vesicles within the EC and both forms of MMP-7 have a high affinity for and bind to heparan sulfate (Yu and Woessner Jr 2000). Therefore, mechanisms exist by which MMP’s may be rapidly released by endothelial cells. Innate inhibition of MMPs is derived from tissue inhibitors of metalloproteinases (TIMPs), a family of four different molecules made unique by their expression, localization, and inhibitory activity. Much like the MMPs, TIMPs are capable of binding heparan sulfate and chondroitin sulfate in the glycocalyx (Yu and Woessner Jr 2000).
The putative role of MMPs in cleaving glycans from the EC surface is supported by studies of in situ microzymography to quantify MMP activation on the surface of post-capillary venules (Mulivor and Lipowsky 2009). Hence, it is likely that cleavage of GAG-bearing proteoglycans by either membrane-bound or cytosolic MMPs in the endothelial cell may be responsible for shedding of the glycocalyx. This hypothesis is also supported by studies of syndecan-1 shedding from human embryonic kidney cells caused by membrane type matrix metalloproteinase-1 (MT1-MMP) (Endo et al. 2003), shedding of syndecan-1 and syndecan-4 from HeLa tumor cells by MMP-9 (Brule et al. 2006), shedding of syndecan-1 from pancreatic carcinoma cells by MMP-7 (Ding et al. 2005), and shedding of syndecan-1 by MMP-7 during transmigration of neutrophils from the interstitium to alveoli in the lung (Li et al. 2002).
The effects of MMP inhibition on glycan shedding and WBC-EC adhesion in response to topical application of fMLP is illustrated in Fig. 5. Without MMP inhibition, fMLP induces a rapid (<10 min) shedding of glycans and an eightfold increase in the number of WBCs adhered to the walls of post-capillary venules (Mulivor and Lipowsky 2009). Superfusing the tissue with 0.5 μM. doxycycline results in a significant attenuation of glycan shedding and WBC-EC adhesion.
Enzymatic shedding of the glycocalyx and WBC-EC adhesion in mesenteric venules. Glycan concentration was taken in proportion to the intensity of fluorescently labeled lectin (BS-1), normalized to initial values as a function of time following topical application of fMLP. (a) Glycan concentration in the glycocalyx fell dramatically following onset of fMLP stimulation. This fall was completely abolished by superfusion of the tissue with the MMP inhibitor doxycycline at a concentration of 0.5 μM. (b) Glycan concentration due to fMLP following IV administration of low-molecular-weight heparin (LMWH) of the indicated doses. Low doses (0.22 mg/kg) inhibited the initial fall during the first 10 min. High doses (>0.60 mg/kg) resulted in a rise in glycan concentration presumably due to ligation of HS chains and subsequent collapse of the glycocalyx. (c). The WBC-EC adhesion response to fMLP, with and without superfusion with doxycycline. (d) WBC-EC adhesion with infusion of LMWH. The high dose of LMWH initially delayed the rise in WBC-EC adhesion. Data are means ± SE. (a) and (c) redrawn from Mulivor et al. (Atherton and Born 1972); (b) and (d) redrawn from Lipowsky et al. (Atherton and Born 1973)
Whereas MMP activity presumably cleaves the protein core of GAG-bearing proteoglycans, cleavage of GAG chains by EC secretion of heparanase may also contribute to shedding (Chappell et al. 2008; Becker et al. 2015). Heparin has long been recognized as an inhibitor of heparanase activity (Bar-Ner et al. 1987), and considerable experimental and clinical evidence supports its anti-inflammatory activity (Page 2013). The anti-inflammatory properties of unfractionated and low-molecular-weight heparins (LMWH) have been studied extensively, although precise mechanisms have not been established (Oduah et al. 2016). Several studies have aimed to delineate the role of heparin in WBC-EC rolling and adhesion, and transmigration trough the microvessel wall. Treatment with LMWH dramatically diminished sepsis-induced neutrophil sequestration in the lung (Ning et al. 2015) and attenuated shedding of the glycocalyx in septic shock (Yini et al. 2015). Heparin has been reported to diminish or protect against reperfusion injury in various animal models (Young 2008). Intradermal administration of heparin attenuated eosinophil accumulation in response to inflammatory stimuli in a dose-dependent manner (Teixeira and Hellewell 1993). Binding of heparins to selectins (Koenig et al. 1998), WBCs (Page 2013; Diamond et al. 1995; Lever et al. 2000), and HSPGs and other constituents of the EC glycocalyx (Nordling et al. 2015; VanTeeffelen et al. 2007) has been shown to inhibit the inflammatory process. Use of low-molecular-weight heparin fractions has shown potential for protecting the endothelial glycocalyx from degradation in nephrosis (Gaddi et al. 2010), diabetes (Eskens et al. 2013), thrombosis (Daniels et al. 2006), retinal neovascularization (Jo et al. 2014), and inflammation (Becker et al. 2015; Kolarova et al. 2014). These studies found that the agent sulodexide, a mixture of low-molecular-weight heparin and dermatan sulfates, afforded significant protection of the glycocalyx from degradation.
The effects of graded concentrations of LMWH (Lovenox®, relative molecular mass, Mr. = 4500) on shedding of glycans and WBC-EC adhesion (Lipowsky and Lescanic 2017) are illustrated in Fig. 5b, d. With increasing doses of LMWH up to 0.22 mg/kg, competitive binding of LMWH to heparanase may attenuate the initial shedding of glycans due to fMLP. With greater doses (>0.6 mg/kg), glycan concentration appears to rise due to a compaction of the glycocalyx as HS chains are cleaved and the layer collapses. Eventually, the inhibition of shedding by LMWH is overwhelmed by activity of either MMPs, heparanase, or other sheddases. The WBC-EC adhesion response to fMLP (Fig. 5d) was significantly attenuated during the initial 10 min at the highest dose of LMWH but eventually rose with prolonged exposure to the chemoattractant. In these studies, WBC adhesion correlated with intensity of the lectin stain for all measurements and revealed a significant 40% reduction in adhesion as intensity increased 50%. This relationship was attributed to LMWH inhibition of heparanase and/or binding to components of the glycocalyx with a resultant mitigation of glycan shedding, compaction of the lectin stain, and stabilization of the glycocalyx.
6 Leukocyte Rolling and Adhesion
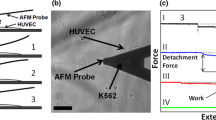
Based upon the rolling and adhesion of WBCs on either artificial surfaces coated with receptors for specific ligands (Alon et al. 1995; Lawrence and Springer 1991, 1993) or monolayers of cultured endothelial cells (Arisaka et al. 1995; Hoover et al. 1980; Lawrence et al. 1987), it has long been held that adhesiveness is governed by regulation of the affinity and avidity of the integrin molecules on the WBC and EC (Zarbock and Ley 2009; Kinashi and Katagiri 2004; Laudanna et al. 2002; Luo et al. 2007). In vivo studies of post-capillary venules (Arfors et al. 1987; House and Lipowsky 1987b; Ley et al. 1995) have supported this concept. In addition, the mechanical properties of the glycocalyx may play a role in the adhesion process in light of the ability of microvilli on the surface of rolling WBCs to penetrate the surface layer to reach adhesion receptors (Zhao et al. 2001). WBC microvilli may range in length from 0.3 to 0.7 μm (Weinbaum et al. 2007). The ability to penetrate the glycocalyx may depend on changes in porosity and stiffness attendant to physiological stimuli (Weinbaum et al. 2007; Platts et al. 2003; Platts and Duling 2004). Under normal conditions, the apparent thickness of the glycocalyx significantly exceeds the lengths of endothelial cell (EC) receptors involved in leukocyte (WBC) rolling on the EC (selectins) and firm adhesion to the EC (integrins). The lengths of these receptors range from 20 nm for the β2 integrin ligands to 30–40 nm for E- and P-selectins (Springer 1990). Thus, reduction in thickness of the glycocalyx by either chemoattractants (e.g., fMLP) (Gao and Lipowsky 2010) or cytokines (e.g., TNF-α) (Henry and Duling 2000) accompanied by increased porosity may enhance access to adhesion receptors on the EC surface. It has been shown that perfusion of post-capillary venules with heparinase or superfusion of the tissue with fMLP served to increase binding of circulating antibodies to ICAM-1 on the EC surface (Mulivor and Lipowsky 2002). Although in this study, firm adhesion of WBCs was not stimulated by perfusion of venules with heparinase, most likely because substrates for leukocyte rolling were also removed, subsequent studies using heparitinase (which may cleave less sulfated heparan sulfate chains) produced an increase in firm WBC adhesion (Constantinescu et al. 2003). Alternatively, it has been demonstrated that heparinase reduces stimulated rolling and adhesion of WBCs in post-capillary venules by inhibiting externalization of P-selectin and/or compromising the structural interactions between heparan sulfate proteoglycans and selectins (Hayward et al. 1998).
Changes in the glycocalyx attendant to EC activation also affect WBC rolling adhesive interactions with the EC. Taking the rolling velocity of WBCs (normalized with respect to estimated wall shear rates, S.R.) as a measure of the adhesiveness of the EC surface (the lower the ratio of VWBC/SR, the greater the adhesiveness), it was found that superfusion of the tissue with inhibitors of MMP activity, such as doxycycline or the zinc chelator GM6001, decreased the rolling velocity, thus promoting adhesiveness of the EC surface during WBC rolling. These results suggest that there is a basal level of sheddase activity on the EC surface that may be suppressed by MMP inhibition, which leads to an excessive accumulation of adhesion receptors on the EC surface that retard the rolling motion of WBCs. The presence of a basal level of MMP activity on the EC surface of post-capillary venules has been demonstrated by measuring the fluorescence activity of fluorescence substrates circulating in the plasma, which is reduced with MMP inhibition (Mulivor and Lipowsky 2009). Interestingly, superfusion of the tissue with fMLP alone causes a similar reduction in rolling velocity, presumably due to a combination of conformational changes in adhesion receptors on the EC surface and enhanced externalization of adhesion receptors (e.g., P-selectin) and shedding of the glycocalyx. While inhibition of MMP activation and activation with fMLP both resulted in diminished rolling velocity, the strength of the adhesive bond during firm adhesion was found to be less with MMP suppression compared to that with fMLP, presumably due to conformational changes of WBC integrin receptors induced by fMLP (Lipowsky et al. 2015).
Similar adhesive interactions have also been observed, in part, by experiments in other tissues and cells. Inhibition of L-selectin shedding from WBCs by the metalloprotease inhibitor KD-IX-73-4 was found to reduce WBC rolling velocity in post-capillary venules of hamster cremaster muscle (Hafezi-Moghadam et al. 2001), which was attributed to inhibition of L-selectin shedding on the leukocyte alone. Although KD-IX-73-4 had no apparent effect on the endothelial glycocalyx, these studies bring to light the potential for metalloprotease inhibition to affect leukocyte rolling and adhesion. Further, comparison of the inhibitory activity of KD-IX-73-4 on the shedding of the endothelial protein C receptor (EPCR) from EA.hy926 endothelial cells, with inhibition of the MMP inhibitor GM6001, revealed that the latter was ineffective in inhibiting the release of EPCR (Xu et al. 2000). Thus, if this endothelial selectivity of the MMP inhibitors GM6001 and doxycycline applies to the reductions of WBC rolling velocity in venules, then the role of MMP inhibition on affecting the adhesive properties of the endothelial glycocalyx is further supported. It has also been shown that reduced rolling velocity of WBCs occurs following exposure of cremaster venules to TNF-α (Jung et al. 1998). Although these results were attributed to conformational changes of adhesion receptors in response to TNF-α, this trend may reflect the shedding of glycans from the EC surface, as noted previously (Henry and Duling 2000), and the enhanced access to adhesion ligands (e.g., ICAM-1).
7 Conclusions
In summary, the endothelial surface layer, which consists of the EC glycocalyx and a layer of adsorbed proteins, has been implicated as a barrier to WBC-EC adhesion. The primary glycoproteins are decorated with the principal glycosaminoglycans (GAGS) heparan sulfate (HS) and chondroitin sulfate (CS) that are encased in a meshwork of hyaluronic acid (HA). Together, these glycans form a layer that can be observed in vivo on the surface of the EC that is on the order of 500 μm thick. Measurement of the precise thickness of the ESL is fraught with many difficulties and is most easily implemented by exclusion of macromolecules from the EC surface. In vitro, the ESL is much smaller, on the order of 1/10th the in vivo thickness. Staining of glycans with carbohydrate-binding proteins (lectins) permits visualization of the ESL and reveals that the composition of the glycocalyx readily changes during the inflammatory process, as evidenced by the shedding of glycans with activation of the endothelium by chemoattractants and cytokines. Reductions in thickness and increases in porosity of the ESL due to an inflammatory stimulus facilitate greater access to WBC adhesion receptors on the EC surface and thus promote WBC-EC adhesion.
The effectors of ESL shedding are most likely members of the family of metalloproteinases, which cleave the core proteoglycans, and endoglycosidases (namely, heparanase), which cleave GAGs attached to the core proteins. Direct intravital microscopic studies of shedding of the glycocalyx have suggested that glycan shedding may be inhibited by MMP inhibitors and competitive binding to EC-derived heparanase. The relative proportions of MMP and heparanase-induced shedding remain to be fully delineated, as well as the extent to which MMPs and heparanase affect their mutual release and activation. Identification of the specific proteases responsible for shedding is further complicated by the ability of specific MMPs to activate other members of the MMP family and for other proteases to activate MMPs. There is also an indirect association between heparanase and MMP expression (Purushothaman et al. 2008, 2011, 2010; Zcharia et al. 2009). For example, blocking activation of MMP-9 inhibited heparanase-induced syndecan-1 shedding in myeloma cells (Purushothaman et al. 2010), and overexpression of heparanase in cultured human mammary carcinoma cells resulted in diminished expression of MMP-2, MMP-9, and MMP-14 (Zcharia et al. 2009). It is clear, however, that stabilization of the glycocalyx during inflammation may indeed mitigate WBC-EC adhesion. Thus, the development of new strategies to directly target shedding of the glycocalyx may have significant therapeutic value.
References
Adamson RH, Clough G (1992) Plasma proteins modify the endothelial cell glycocalyx of frog mesenteric microvessels. J Physiol 445:473–486
Alon R, Hammer DA, Springer TA (1995) Lifetime of the p-selectin-carbohydrate bond and its response to tensile force in hydrodynamic flow. Nature 374:539–542
Arfors KE, Lundberg C, Lindbom L, Lundberg K, Beatty PG, Harlan JM (1987) A monoclonal antibody to the membrane glycoprotein complex cd18 inhibits polymorphonuclear leukocyte accumulation and plasma leakage in vivo. Blood 69:338–340
Arisaka T, Mitsumata M, Kawasumi M, Tohjima T, Hirose S, Yoshida Y (1995) Effects of shear stress on glycosaminoglycan synthesis in vascular endothelial cells. Ann N Y Acad Sci 748:543–554
Atherton A, Born GV (1972) Quantitative investigations of the adhesiveness of circulating polymorphonuclear leucocytes to blood vessel walls. J Physiol 222:447–474
Atherton A, Born GV (1973) Relationship between the velocity of rolling granulocytes and that of the blood flow in venules. J Physiol 233:157–165
Bagge U, Karlsson R (1980) Maintenance of white blood cell margination at the passage through small venular junctions. Microvasc Res 20:92–95
Bar-Ner M, Eldor A, Wasserman L, Matzner Y, Cohen IR, Fuks Z et al (1987) Inhibition of heparanase-mediated degradation of extracellular matrix heparan sulfate by non-anticoagulant heparin species. Blood 70:551–557
Becker BF, Jacob M, Leipert S, Salmon AH, Chappell D (2015) Degradation of the endothelial glycocalyx in clinical settings: searching for the sheddases. Br J Clin Pharmacol 80:389–402
Bennett HS, Luft JH, Hampton JC (1959) Morphological classifications of vertebrate blood capillaries. Am J Phys 196:381–390
Braide M, Amundson B, Chien S, Bagge U (1984) Quantitative studies on the influence of leukocytes on the vascular resistance in a skeletal muscle preparation. Microvasc Res 27:331–352
Bruegger D, Jacob M, Rehm M, Loetsch M, Welsch U, Conzen P et al (2005) Atrial natriuretic peptide induces shedding of endothelial glycocalyx in coronary vascular bed of Guinea pig hearts. Am J Physiol Heart Circ Physiol 289:H1993–H1999
Brule S, Charnaux N, Sutton A, Ledoux D, Chaigneau T, Saffar L et al (2006) The shedding of syndecan-4 and syndecan-1 from hela cells and human primary macrophages is accelerated by sdf-1/cxcl12 and mediated by the matrix metalloproteinase-9. Glycobiology 16:488–501
Cabrales P, Vazquez BY, Tsai AG, Intaglietta M (2007) Microvascular and capillary perfusion following glycocalyx degradation. J Appl Physiol 102:2251–2259
Chappell D, Jacob M, Rehm M, Stoeckelhuber M, Welsch U, Conzen P et al (2008) Heparinase selectively sheds heparan sulphate from the endothelial glycocalyx. Biol Chem 389:79–82
Chappell D, Jacob M, Paul O, Rehm M, Welsch U, Stoeckelhuber M et al (2009a) The glycocalyx of the human umbilical vein endothelial cell: an impressive structure ex vivo but not in culture. Circ Res 104:1313–1317
Chappell D, Hofmann-Kiefer K, Jacob M, Rehm M, Briegel J, Welsch U et al (2009b) TNF-alpha induced shedding of the endothelial glycocalyx is prevented by hydrocortisone and antithrombin. Basic Res Cardiol 104:78–89
Colburn P, Kobayashi E, Buonassisi V (1994) Depleted level of heparan sulfate proteoglycan in the extracellular matrix of endothelial cell cultures exposed to endotoxin. J Cell Physiol 159:121–130
Constantinescu AA, Vink H, Spaan JA (2001) Elevated capillary tube hematocrit reflects degradation of endothelial cell glycocalyx by oxidized ldl. Am J Physiol Heart Circ Physiol 280:H1051–H1057
Constantinescu AA, Vink H, Spaan JA (2003) Endothelial cell glycocalyx modulates immobilization of leukocytes at the endothelial surface. Arterioscler Thromb Vasc Biol 23:1541–1547
Daniels B, Linhardt RJ, Zhang F, Mao W, Wice SM, Hiebert LM (2006) In vivo antithrombotic synergy of oral heparin and arginine: endothelial thromboresistance without changes in coagulation parameters. Thromb Haemost 95:865–872
DeLano FA, Schmid-Schonbein GW (2008) Proteinase activity and receptor cleavage: mechanism for insulin resistance in the spontaneously hypertensive rat. Hypertension 52:415–423
Desjardins C, Duling BR (1990) Heparinase treatment suggests a role for the endothelial cell glycocalyx in regulation of capillary hematocrit. Am J Phys 258:H647–H654
Diamond MS, Alon R, Parkos CA, Quinn MT, Springer TA (1995) Heparin is an adhesive ligand for the leukocyte integrin mac-1 (cd11b/cd1). J Cell Biol 130:1473–1482
Ding K, Lopez-Burks M, Sanchez-Duran JA, Korc M, Lander AD (2005) Growth factor-induced shedding of syndecan-1 confers glypican-1 dependence on mitogenic responses of cancer cells. J Cell Biol 171:729–738
Endo K, Takino T, Miyamori H, Kinsen H, Yoshizaki T, Furukawa M et al (2003) Cleavage of syndecan-1 by membrane type matrix metalloproteinase-1 stimulates cell migration. J Biol Chem 278:40764–40770
Eskens BJM, Zuurbier CJ, van Haare J, Vink H, van Teeffelen J (2013) Effects of two weeks of metformin treatment on whole-body glycocalyx barrier properties in db/db mice. Cardiovasc Diabetol 12:175
Fahraeus R (1929) The suspension stability of blood. Physiol Rev 9:241–274
Feng J, Weinbaum S (2000) Lubrication theory in highly compressible porous media: the mechanics of skiing, from red cells to humans. J Fluid Mech 422:281–317
Fitzgerald ML, Wang Z, Park PW, Murphy G, Bernfield M (2000) Shedding of syndecan-1 and -4 ectodomains is regulated by multiple signaling pathways and mediated by a timp-3-sensitive metalloproteinase. J Cell Biol 148:811–824
Fux L, Ilan N, Sanderson RD, Vlodavsky I (2009) Heparanase: busy at the cell surface. Trends Biochem Sci 34:511–519
Gaddi AV, Cicero AF, Gambaro G (2010) Nephroprotective action of glycosaminoglycans: why the pharmacological properties of sulodexide might be reconsidered. Int J Nephrol Renovasc Dis 3:99–105
Gao L, Lipowsky HH (2010) Composition of the endothelial glycocalyx and its relation to its thickness and diffusion of small solutes. Microvasc Res 80:394–401
Goldsmith HL, Spain S (1984) Margination of leukocytes in blood flow through small tubes. Microvasc Res 27:204–222
Golub LM, Lee HM, Ryan ME, Giannobile WV, Payne J, Sorsa T (1998) Tetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanisms. Adv Dent Res 12:12–26
Gotte M (2003) Syndecans in inflammation. FASEB J 17:575–591
Gouverneur M, Spaan JA, Pannekoek H, Fontijn RD, Vink H (2006) Fluid shear stress stimulates incorporation of hyaluronan into endothelial cell glycocalyx. Am J Physiol Heart Circ Physiol 290:H458–H452
Grant L (1973) The sticking and emigration of white blood cells in inflammation. In: Zweifach BW, Grant L, McClusky R (eds) The inflammatory process, vol 2. Academic Press, Orlando, pp 205–249
Grimm J, Keller R, de Groot PG (1988) Laminar flow induces cell polarity and leads to rearrangement of proteoglycan metabolism in endothelial cells. Thromb Haemost 60:437–441
Gronski TJ, Martin RL, Kobayashi DK, Walsh BC, Holman MC, Huber M et al (1997) Hydrolysis of a broad spectrum of extracellular matrix proteins by human macrophage elastase. J Biol Chem 272:12189–12194
Haas TL, Milkiewicz M, Davis SJ, Zhou AL, Egginton S, Brown MD et al (2000) Matrix metalloproteinase activity is required for activity-induced angiogenesis in rat skeletal muscle. Am J Physiol Heart Circ Physiol 279:1540–1547
Hafezi-Moghadam A, Thomas KL, Prorock AJ, Huo Y, Ley K (2001) L-selectin shedding regulates leukocyte recruitment. J Exp Med 193:863–872
Haldenby KA, Chappell DC, Winlove CP, Parker KH, Firth JA (1994) Focal and regional variations in the composition of the glycocalyx of large vessel endothelium. J Vasc Res 31:2–9
Hayward R, Scalia R, Hopper B, Appel JZ III, Lefer AM (1998) Cellular mechanisms of heparinase iii protection in rat traumatic shock. Am J Phys 275:H23–H30
Henry CB, Duling BR (1999) Permeation of the luminal capillary glycocalyx is determined by hyaluronan. Am J Phys 277:H508–H514
Henry CB, Duling BR (2000) TNF-alpha increases entry of macromolecules into luminal endothelial cell glycocalyx. Am J Physiol Heart Circ Physiol 279:H2815–H2823
Hofmann-Kiefer KF, Kemming GI, Chappell D, Flondor M, Kisch-Wedel H, Hauser A et al (2009) Serum heparan sulfate levels are elevated in endotoxemia. Eur J Med Res 14:526–531
Hoover RL, Folger R, Haering WA, Ware BR, Karnovsky MJ (1980) Adhesion of leukocytes to endothelium: roles of divalent cations, surface charge, chemotactic agents and substrate. J Cell Sci 45:73–86
House SD, Lipowsky HH (1987a) Microvascular hematocrit and red cell flux in rat cremaster muscle. Am J Phys 252:H211–H222
House SD, Lipowsky HH (1987b) Leukocyte-endothelium adhesion: microhemodynamics in mesentery of the cat. Microvasc Res 34:363–379
Huxley VH, Curry FE (1991) Differential actions of albumin and plasma on capillary solute permeability. Am J Phys 260:H1645–H1654
Ihrcke NS, Platt JL (1996) Shedding of heparan sulfate proteoglycan by stimulated endothelial cells: evidence for proteolysis of cell-surface molecules. J Cell Physiol 168:625–637
Ihrcke NS, Wrenshall LE, Lindman BJ, Platt JL (1993) Role of heparan sulfate in immune system-blood vessel interactions. Immunol Today 14:500–505
Iigo Y, Suematsu M, Higashida T, Oheda J, Matsumoto K, Wakabayashi Y et al (1997) Constitutive expression of icam-1 in rat microvascular systems analyzed by laser confocal microscopy. Am J Phys 273:H138–H147
Jo H, Jung SH, Kang J, Yim HB, Kang KD (2014) Sulodexide inhibits retinal neovascularization in a mouse model of oxygen-induced retinopathy. BMB Rep 47:637–642
Jung U, Norman KE, Scharffetter-Kochanek K, Beaudet AL, Ley K (1998) Transit time of leukocytes rolling through venules controls cytokine-induced inflammatory cell recruitment in vivo. J Clin Invest 102:1526–1533
Kinashi T, Katagiri K (2004) Regulation of lymphocyte adhesion and migration by the small GTPase Rap1 and its effector molecule RAPL. Immunol Lett 93:1–5
Klitzman B, Duling BR (1979) Microvascular hematocrit and red cell flow in resting and contracting striated muscle. Am J Phys 237:H481–H490
Koenig A, Norgard-Sumnicht K, Linhardt R, Varki A (1998) Differential interactions of heparin and heparan sulfate glycosaminoglycans with the selectins. Implications for the use of unfractionated and low molecular weight heparins as therapeutic agents. J Clin Invest 101:877–889
Kolarova H, Ambruzova B, Sindlerova LS, Klinke A, Kubala L (2014) Modulation of endothelial glycocalyx structure under inflammatory conditions. Mediat Inflamm 2014:694312
Laudanna C, Kim JY, Constantin G, Butcher EC (2002) Rapid leukocyte integrin activation by chemokines. Immunol Rev 186:37–46
Laurent TC, Fraser JR (1992) Hyaluronan. FASEB J 6:2397–2404
Lawrence MB, Springer TA (1991) Leukocytes roll on a selectin at physiologic flow rates: distinction from and prerequisite for adhesion through integrins. Cell 65:859–873
Lawrence MB, Springer TA (1993) Neutrophils roll on E-selectin. J Immunol 151:6338–6346
Lawrence MB, McIntire LV, Eskin SG (1987) Effect of flow on polymorphonuclear leukocyte endothelial-cell adhesion. Blood 70:1284–1290
Lever R, Hoult JRS, Page CP (2000) The effects of heparin and related molecules upon the adhesion of human polymorphonuclear leucocytes to vascular endothelium in vitro. Br J Pharmacol 129:533–540
Ley K, Bullard DC, Arbones ML, Bosse R, Vestweber D, Tedder TF et al (1995) Sequential contribution of l- and p-selectin to leukocyte rolling in vivo. J Exp Med 181:669–675
Li Z, Li L, Zielke HR, Cheng L, Xiao R, Crow MT et al (1996) Increased expression of 72-kd type iv collagenase (mmp-2) in human aortic atherosclerotic lesions. Am J Pathol 148:121–128
Li Q, Park PW, Wilson CL, Parks WC (2002) Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell 111:635–646
Lipowsky HH, Lescanic A (2013) The effect of doxycycline on shedding of the glycocalyx due to reactive oxygen species. Microvasc Res 90:80–85
Lipowsky HH, Lescanic A (2017) Inhibition of inflammation induced shedding of the endothelial glycocalyx with low molecular weight heparin. Microvasc Res 112:72–78
Lipowsky HH, Sah R, Lescanic A (2011) Relative roles of doxycycline and cation chelation in endothelial glycan shedding and adhesion of leukocytes. Am J Physiol Heart Circ Physiol 300:H415–H422
Lipowsky HH, Lescanic A, Sah R (2015) Role of matrix metalloproteases in the kinetics of leukocyte-endothelial adhesion in post-capillary venules. Biorheology 52:433–445
Luft JH (1966) Fine structures of capillary and endocapillary layer as revealed by ruthenium red. Fed Proc 25:1773–1783
Luo B-H, Carman CV, Springer TA (2007) Structural basis of integrin regulation and signaling. Annu Rev Immunol 25:619–647
Marki A, Esko JD, Pries AR, Ley K (2015) Role of the endothelial surface layer in neutrophil recruitment. J Leukoc Biol 98:503–515
Mulivor AW, Lipowsky HH (2002) Role of glycocalyx in leukocyte-endothelial cell adhesion. Am J Physiol Heart Circ Physiol 283:H1282–H1291
Mulivor AW, Lipowsky HH (2004) Inflammation- and ischemia-induced shedding of venular glycocalyx. Am J Physiol Heart Circ Physiol 286:H1672–H1680
Mulivor AW, Lipowsky HH (2009) Inhibition of glycan shedding and leukocyte-endothelial adhesion in postcapillary venules by suppression of matrixmetalloprotease activity with doxycycline. Microcirculation 16:657–666
Ning F, Wang X, Shang L, Wang T, Lv C, Qi Z et al (2015) Low molecular weight heparin may prevent acute lung injury induced by sepsis in rats. Gene 557:88–91
Nordling S, Hong J, Fromell K, Edin F, Brannstrom J, Larsson R et al (2015) Vascular repair utilising immobilised heparin conjugate for protection against early activation of inflammation and coagulation. Thromb Haemost 113:1312–1322
Oduah EI, Linhardt RJ, Sharfstein ST (2016) Heparin: past, present, and future. Pharmaceuticals (Basel) 9 pii: E38
Padberg JS, Wiesinger A, di Marco GS, Reuter S, Grabner A, Kentrup D et al (2014) Damage of the endothelial glycocalyx in chronic kidney disease. Atherosclerosis 234:335–343
Page C (2013) Heparin and related drugs: beyond anticoagulant activity. ISRN Pharmacol 2013:910743
Park PW, Reizes O, Bernfield M (2000) Cell surface heparan sulfate proteoglycans: selective regulators of ligand-receptor encounters. J Biol Chem 275:29923–29926
Platt JL, Vercellotti GM, Lindman BJ, Oegema TR Jr, Bach FH, Dalmasso AP (1990) Release of heparan sulfate from endothelial cells. Implications for pathogenesis of hyperacute rejection. J Exp Med 171:1363–1368
Platt JL, Dalmasso AP, Lindman BJ, Ihrcke NS, Bach FH (1991) The role of c5a and antibody in the release of heparan sulfate from endothelial cells. Eur J Immunol 21:2887–2890
Platts SH, Duling BR (2004) Adenosine a3 receptor activation modulates the capillary endothelial glycocalyx. Circ Res 94:77–82
Platts SH, Linden J, Duling BR (2003) Rapid modification of the glycocalyx caused by ischemia-reperfusion is inhibited by adenosine a2a receptor activation. Am J Physiol Heart Circ Physiol 284:H2360–H2367
Poiseuille JLM (1835) Recherches sur les causes du mouvement du sang dans les vaisseaux capillaries. C R Acad Sci 6:554–560
Potter DR, Damiano ER (2008) The hydrodynamically relevant endothelial cell glycocalyx observed in vivo is absent in vitro. Circ Res 102:770–776
Pries AR, Secomb TW, Gaehtgens P, Gross JF (1990) Blood flow in microvascular networks. Experiments and simulation. Circ Res 67:826–834
Pries AR, Secomb TW, Jacobs H, Sperandio M, Osterloh K, Gaehtgens P (1997) Microvascular blood flow resistance: role of endothelial surface layer. Am J Phys 273:H2272–H2279
Pries AR, Secomb TW, Gaehtgens P (2000) The endothelial surface layer. Pflugers Arch 440:653–666
Purushothaman A, Chen L, Yang Y, Sanderson RD (2008) Heparanase stimulation of protease expression implicates it as a master regulator of the aggressive tumor phenotype in myeloma. J Biol Chem 283:32628–32636
Purushothaman A, Uyama T, Kobayashi F, Yamada S, Sugahara K, Rapraeger AC et al (2010) Heparanase-enhanced shedding of syndecan-1 by myeloma cells promotes endothelial invasion and angiogenesis. Blood 115:2449–2457
Purushothaman A, Hurst DR, Pisano C, Mizumoto S, Sugahara K, Sanderson RD (2011) Heparanase-mediated loss of nuclear syndecan-1 enhances histone acetyltransferase (hat) activity to promote expression of genes that drive an aggressive tumor phenotype. J Biol Chem 286:30377–30383
Rapraeger A (1989) Transforming growth factor (type beta) promotes the addition of chondroitin sulfate chains to the cell surface proteoglycan (syndecan) of mouse mammary epithelia. J Cell Biol 109:2509–2518
Rehm M, Bruegger D, Christ F, Conzen P, Thiel M, Jacob M et al (2007) Shedding of the endothelial glycocalyx in patients undergoing major vascular surgery with global and regional ischemia. Circulation 116:1896–1906
Reitsma S, Slaaf DW, Vink H, van Zandvoort MA, oude Egbrink MG (2007) The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch 454:345–359
Schmid-Schonbein GW, Usami S, Skalak R, Chien S (1980) The interaction of leukocytes and erythrocytes in capillary and postcapillary vessels. Microvasc Res 19:45–70
Schnitzer JE, Ulmer JB, Palade GE (1990a) A major endothelial plasmalemmal sialoglycoprotein, gp60, is immunologically related to glycophorin. Proc Natl Acad Sci U S A 87:6843–6847
Schnitzer JE, Shen CP, Palade GE (1990b) Lectin analysis of common glycoproteins detected on the surface of continuous microvascular endothelium in situ and in culture: identification of sialoglycoproteins. Eur J Cell Biol 52:241–251
Secomb TW, Hsu R, Pries AR (2001) Motion of red blood cells in a capillary with an endothelial surface layer: effect of flow velocity. Am J Physiol Heart Circ Physiol 281:H629–H636
Simionescu M, Simionescu N, Palade GE (1982) Differentiated microdomains on the luminal surface of capillary endothelium: distribution of lectin receptors. J Cell Biol 94:406–413
Smith ML, Long DS, Damiano ER, Ley K (2003) Near-wall micro-piv reveals a hydrodynamically relevant endothelial surface layer in venules in vivo. Biophys J 85:637–645
Spinale FG (2007) Myocardial matrix remodeling and the matrix metalloproteinases: influence on cardiac form and function. Physiol Rev 87:1285–1342
Springer TA (1990) Adhesion receptors of the immune system. Nature 346:425–434
Springer TA, Lasky LA (1991) Cell adhesion. Sticky sugars for selectins. Nature 349:196–197
Squire JM, Chew M, Nneji G, Neal C, Barry J, Michel C (2001) Quasi-periodic substructure in the microvessel endothelial glycocalyx: a possible explanation for molecular filtering? J Struct Biol 136:239–255
Subramanian SV, Fitzgerald ML, Bernfield M (1997) Regulated shedding of syndecan-1 and -4 ectodomains by thrombin and growth factor receptor activation. J Biol Chem 272:14713–14720
Sutera SP, Seshadri V, Croce PA, Hochmuth RM (1970) Capillary blood flow II. Deformable model cells in tube flow. Microvasc Res 2:420–433
Svennevig K, Hoel T, Thiara A, Kolset S, Castelheim A, Mollnes T et al (2008) Syndecan-1 plasma levels during coronary artery bypass surgery with and without cardiopulmonary bypass. Perfusion 23:165–171
Taraboletti G, D'Ascenzo S, Borsotti P, Giavazzi R, Pavan A, Dolo V (2002) Shedding of the matrix metalloproteinases mmp-2, mmp-9, and mt1-mmp as membrane vesicle-associated components by endothelial cells. Am J Pathol 160:673–680
Teixeira MM, Hellewell PG (1993) Suppression by intradermal administration of heparin of eosinophil accumulation but not oedema formation in inflammatory reactions in Guinea-pig skin. Br J Pharmacol 110:1496–1500
VanTeeffelen JW, Brands J, Jansen C, Spaan JA, Vink H (2007) Heparin impairs glycocalyx barrier properties and attenuates shear dependent vasodilation in mice. Hypertension 50:261–267
Vink H, Duling BR (1996) Identification of distinct luminal domains for macromolecules, erythrocytes, and leukocytes within mammalian capillaries. Circ Res 79:581–589
Vink H, Duling BR (2000) Capillary endothelial surface layer selectively reduces plasma solute distribution volume. Am J Physiol Heart Circ Physiol 278:H285–H289
Vogl-Willis CA, Edwards IJ (2004) High-glucose-induced structural changes in the heparan sulfate proteoglycan, perlecan, of cultured human aortic endothelial cells. Biochim Biophys Acta 1672:36–45
Weinbaum S, Tarbell JM, Damiano ER (2007) The structure and function of the endothelial glycocalyx layer. Annu Rev Biomed Eng 9:121–167
Wiesinger A, Peters W, Chappell D, Kentrup D, Reuter S, Pavenstadt H et al (2013) Nanomechanics of the endothelial glycocalyx in experimental sepsis. PLoS One 8:e80905
Xu J, Qu D, Esmon NL, Esmon CT (2000) Metalloproteolytic release of endothelial cell protein c receptor. J Biol Chem 275:6038–6044
Yaras N, Sariahmetoglu M, Bilginoglu A, Aydemir-Koksoy A, Onay-Besikci A, Turan B et al (2008) Protective action of doxycycline against diabetic cardiomyopathy in rats. Br J Pharmacol 155:1174–1184
Yini S, Heng Z, Xin A, Xiaochun M (2015) Effect of unfractionated heparin on endothelial glycocalyx in a septic shock model. Acta Anaesthesiol Scand 59:160–169
Young E (2008) The anti-inflammatory effects of heparin and related compounds. Thromb Res 122:743–752
Yu WH, Woessner JF Jr (2000) Heparan sulfate proteoglycans as extracellular docking molecules for matrilysin (matrix metalloproteinase 7). J Biol Chem 275:4183–4191
Zarbock A, Ley K (2009) Neutrophil adhesion and activation under flow. Microcirculation 16:31–42
Zcharia E, Jia J, Zhang X, Baraz L, Lindahl U, Peretz T et al (2009) Newly generated heparanase knock-out mice unravel co-regulation of heparanase and matrix metalloproteinases. PLoS One 4:e5181
Zhao Y, Chien S, Weinbaum S (2001) Dynamic contact forces on leukocyte microvilli and their penetration of the endothelial glycocalyx. Biophys J 80:1124–1140
Zuurbier CJ, Demirci C, Koeman A, Vink H, Ince C (2005) Short-term hyperglycemia increases endothelial glycocalyx permeability and acutely decreases lineal density of capillaries with flowing red blood cells. J Appl Physiol 99:1471–1476
Zweifach BW (1955) Structural makeup of capillary wall. Ann N Y Acad Sci 61:670–677
Acknowledgments
This work was supported in part by NIH R01 HL-39286.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Lipowsky, H.H. (2018). Role of the Glycocalyx as a Barrier to Leukocyte-Endothelium Adhesion. In: Fu, B., Wright, N. (eds) Molecular, Cellular, and Tissue Engineering of the Vascular System. Advances in Experimental Medicine and Biology, vol 1097. Springer, Cham. https://doi.org/10.1007/978-3-319-96445-4_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-96445-4_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-96444-7
Online ISBN: 978-3-319-96445-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)