Abstract
In 2016 the World Health Organization released an update of the classification of brain tumors, based on the increased understanding, over the past two decades, of the genetic basis of tumorigenesis. The new classification, for the first time, integrated both genotypic and phenotypic parameters, leading to a molecular stratification of brain tumors, with significant implications not only for neuropathological diagnosis, but also for prognosis and therapy. The knowledge of this new classification and of the molecular markers that correlate with specific tumor subtypes is essential for radiologist. Understanding how these molecular phenotypes are reflected on imaging is thus becoming increasingly important to define novel magnetic resonance imaging biomarkers that can help clinical decision-making. To this end, advanced imaging techniques, such as spectroscopy, diffusion-weighted imaging, diffusion tensor imaging, perfusion imaging, and functional magnetic resonance imaging, have shown to be promising to increase the accuracy of molecular subtyping of brain tumors by conventional magnetic resonance imaging.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
5.1 Introduction
The 2016 central nervous system (CNS) World Health Organization (WHO) classification of brain neoplasms has completely changed the way brain tumors are now classified, integrating both genotypic and phenotypic parameters, incorporated into the newly updated classification schema. This classification is based on a combination of histology and molecular patterns by direct evaluation of the mutated DNA or by immunohistochemistry, which evaluates the effects of the mutated genes on proteins (and this technique is more widely used also because of lower costs). Since histologic grading is still used in clinical practice, potential relevant inconsistency between the two might appear. The knowledge of this new classification is essential for radiologist as well as for all neuroscientists. The modern approach of imaging in the assessment of brain tumors aims to identify some morphological or metabolic patterns that may have an impact on their classification. This is synthesized in the term radiogenomics.
5.2 Radiogenomics
The molecular stratification of brain tumors is quickly becoming an integral part of their diagnosis, prognosis, and clinical decision-making. Several studies over the past two decades provided insights into the genetic basis of tumorigenesis, explaining why tumors assigned to the same histopathological entity can have broadly different therapy responses and highly divergent clinical outcomes. The new 2016 WHO classification of CNS tumors uses, for the first time, molecular parameters in addition to histology to define many tumor entities [1, 2], thus clearly indicating the utmost significance of genome-wide biomarkers in the molecular era.
The molecular stratification is essential for estimating the individual prognosis [3,4,5]. The more relevant molecular biomarkers are isocitrate dehydrogenase (IDH) 1/2 mutation status and chromosome 1p/19q loss of heterozygosity (LOH). They are complemented by alpha-thalassemia/mental retardation syndrome X-linked (ATRX), which is predictive for associated IDH or H3F3A hotspot mutations [6]. The ATRX status itself confers a prognostic potential in diffuse gliomas [7]. The loss of ATRX expression is mostly induced by truncating ATRX mutations, resulting in an alternative lengthening of telomeres (ALT) phenotype [8, 9]. Moreover, O6-methylguanine DNA methyltransferase (MGMT) can be regarded as an independent prognostic factor in diffuse gliomas [10, 11], and the epidermal growth factor receptor (EGFR) amplification and EGFR variant III (EGFRvIII) mutation are related to neo-angiogenesis evaluation and representation.
Understanding how these molecular phenotypes are reflected on imaging is thus becoming increasingly important to define novel magnetic resonance imaging (MRI) biomarkers that can be used as surrogates for tissue-based molecular subtyping required to predict prognosis, to develop individualized patient therapies, and to follow up patients.
Radiogenomics is a new field of study aiming at determining the association between imaging features and molecular markers. Hence, more accurate approaches are recommended to identify the specific biological and microstructural characteristics of the underlying tumor tissue.
To this end, more sophisticated quantitative imaging approaches such as the analysis of texture features (i.e., pattern of local variations in image intensity) can be applied on anatomical MR images, seeking for correlations between tissue microstructure and thus tumor biology. Recent studies focused their attention on post-contrast T1-weighted and T2/FLAIR images searching for a link with molecular markers representing gene, protein, or metabolite expression, in order to create radiogenomics map to associate image features with biologic processes and molecular subgroups [12].
More recently, advanced imaging features derived from physiological imaging techniques, such as dMRI, PWI, and magnetic resonance spectroscopy (MRS), have shown to be promising to increase the accuracy of molecular subtyping by MRI.
5.3 Conventional Imaging
For many years computed tomography (CT) with contrast enhancement has been the gold standard for the diagnosis of brain tumors due to its ability to ascertain the presence of a brain lesion, to define its dimension and relation with surrounding brain structures, to assess perilesional edema, and to define the presence of multiple brain lesions. CT is superior to MRI for detecting calcifications, skull lesions, and hyper acute hemorrhage and helps direct differential diagnosis as well as immediate patient management [13, 14]. Continuous developments in MRI provide new insights into the diagnosis, classification, and understanding of the biology of brain tumors. MRI studies are characterized by higher contrast resolution associated with multiplanar views. MRI is characterized by high sensitivity for structural alterations caused by tumoral growth, which can be further enhanced by the use of paramagnetic contrast agents. Standard T1- and T2-weighted MRI acquisitions display high sensitivity for brain tumors and give information on the size and localization of the tumor [15]. A normal contrast-enhanced MRI scan essentially rules out the possibility of a brain tumor, but the role of neuroimaging is no longer simply to evaluate structural abnormality and to identify tumor-related complications. Functional, hemodynamic, metabolic, cellular, and cytoarchitectural alterations can be assessed by means of modern MRI. Thereby the current state of neuroimaging has evolved into a comprehensive diagnostic tool that allows the characterization of morphological as well as biological alterations, to diagnose and grade brain tumors, and to monitor and assess treatment response and patient prognosis [16]. Among advanced techniques, MR spectroscopy, diffusion-weighted imaging (DWI) and diffusion tensor imaging (DTI) with tractography, perfusion-weighted imaging, and functional MRI play a role in the transition of clinical MR imaging from a purely morphology-based discipline to one that combines structure with brain function.
Most IDH-mutant and non-mutant diffuse astrocytomas infiltrate the white matter (far behind the abnormal MR signal) sparing of the cortex with mild mass effect. They are typically hypointense on T1WI and hyperintense on T2/FLAIR, without enhancement following contrast administration (Fig. 5.1). Blooming T2* signal can be appreciated if calcifications are present. IDH-mutant anaplastic astrocytomas are hypointense on T1WI and hyperintense on T2/FLAIR as well. Contrast enhancement ranges from none to moderate, but 50–70% of lesions may show some degree of enhancement.
A 52-year-old woman affected by recent epileptic episode. A hyperintense lesion on FLAIR images (a–c) is evident, with left fronto-temporal cortex involvement close to sylvian fissure. Low value of ADC (d) and relative CBV (e) with no enhancement after gadolinium injection (f) are visible. An area of BOLD signal changes close to the lesion after words recruitment task was interpreted as Broca’s area (g). The spectroscopic evaluation reported a reduction of N-acetyl-aspartate into the lesion without significant increase of choline (h). After biopsy (i), a glioma was diagnosed, with lack of mutation of IDH1 (wild-type glioma) and methylation of MGMT. The follow-up examination (j, k) showed a stability of lesion extension. In the last follow-up (l, m) a significant progression of glioma with involvement of contralateral frontal lobe through genu of corpus callosum is appreciable with great enhancement after gadolinium injection. The patient died 13 months after diagnosis
IDH-wild-type anaplastic astrocytoma shows a diffuse infiltrative pattern frequently involving more than three cerebral lobes. This feature was commonly described in the past as gliomatosis cerebri, a term that is no longer used in the pathologic report.
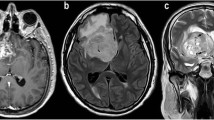
IDH-wild-type glioblastoma (GBM) shows T1WI hyposignal with poorly marginated margins; mixed signal indicating subacute hemorrhage can be seen. T2/FLAIR signal is heterogeneous as well with hyperintensity with indistinct tumor margins and vasogenic edema. Inside the neoplasm mixed signal can indicate necrosis, cysts, fluid and debris levels, and “flow voids” from neovascularization. Enhancement is strong and irregular and typically surrounds a central non-enhancing core. Enhancement can be observed far from the central core of the neoplasm representing tumor extension into adjacent structures. This extension is microscopically evident even far from visible T2 signal alterations and areas of enhancement (Fig. 5.3).
IDH-mutant GBMs may appear non-enhancing, being somehow different from the classic large central necrotic core of IDH-wild-type GBMs.
Oligodendrogliomas (ODs) are glial neoplasms originated from oligodendrocytes that primarily affect supratentorial parenchyma (Fig. 5.2). Historically, co-deletion of whole chromosome arms 1p and 19q, namely 1p/19q co-deletion, has proved to be a diagnostic and prognostic biomarker of ODs. According to the 2016 WHO classification system, the “integrated diagnosis” of ODs requires histological classification, WHO grade, and molecular information (both IDH mutation and 1p/19q co-deletion). High-grade ODs are more prone to prominent edema and enhancement than low-grade ODs [17].
Some studies have tried to construct probabilistic radiographic atlases on anatomical magnetic resonance images of preoperative glioma locations, which may reflect the genetic profile of tumor precursor cells. IDH1 mutant tumors tended to be localized to the frontal lobe, whereas tumors with the methylation of the MGMT promoter occurred most frequently in the left temporal lobe, having a better prognosis than unmethylated tumors due to the higher sensitivity to chemotherapy [18].
A recent study assessed that tumor location was significantly different between MGMT promoter methylated and unmethylated groups, implying that the subventricular zone was more likely to be spared in patients with MGMT promoter methylation (Fig. 5.3). Besides, MGMT promoter methylation is prone to be associated with tumor necrosis. Other qualitative image features were not significantly different between these two groups, including multifocal, tumor cross midline, cyst, edema, enhancement, and side [19].
Some studies indicated that MGMT promoter methylation is poorly predicted with standard MRI features, such as T1-weighted images (T1WI), T2-weighted images (T2WI), and gadolinium (Gd)-enhanced T1WI.
Extracting additional information from medical imaging and relating it to a clinical variable of interest is broadly defined as radiomics. Radiomics is an emerging field that converts imaging data into a high-dimensional, mineable feature space using a large number of automatically extracted data characterization algorithms. Radiomics features include metrics such as spatial relationships, textural heterogeneity, and many other characteristics.
Radiomics features of GBM, especially the combination of enhanced T1W and T2W images, could reflect tumor molecular pathology indicators of MGMT methylation status. An association between imaging features and MGMT promoter methylation status in GBM could exist. MRI data could be applied to infer the molecular pathology of tumor target and may further guide clinical diagnosis and treatment [20].
Tumors with EGFR amplification and EGFRvIII mutation, which showed an increased angiogenesis, commonly occurred in the left temporal lobe anterior to the region identified by MGMT promoter methylation [2].
5.4 Advanced Techniques
5.4.1 Spectroscopy
The major clinical application of magnetic resonance spectroscopy for brain tumor patients has been its potential for non-invasive tumor grading [21,22,23]. These studies have predominantly used MR spectroscopy techniques that detect a signal spectrum from a small region of interest (single-voxel MR spectroscopy). Higher mean choline and lower mean NAA levels in higher-grade tumors have been reported. However, most of the studies found large standard deviations in metabolite ratios and substantial overlap in individual values, which may restrict the accuracy of the technique. Studies using sophisticated data analysis techniques have shown a higher degree of accuracy for in vitro and in vivo spectroscopy studies [24]. A significant improvement in accuracy was obtained using a two-dimensional MRS imaging technique [23]. The combination of improved spatial resolution and increased number of voxels provides much more data about tumor heterogeneity and contributes in exploring the tumor margin. As a result, it is possible to measure the metabolite content of different areas of neoplasms and surrounding normal tissue. This is very useful for better characterizing glial tumors, in which very often coexist areas with different grading, and for a more accurate monitoring of possible malignant degeneration of benign tumors. In a serial proton MRS imaging study it was clearly demonstrated that an increased choline signal is associated with malignant progression of cerebral gliomas and that serial MRS imaging effectively and accurately differentiates between stable and progressive disease [25]. Moreover, sampling of several voxels inside tumors is very important in guiding biopsies, surgery, and radiotherapy. Color choline maps are indeed helpful in guiding stereotactic biopsy, thus improving diagnostic accuracy with decreased sampling error. Multi-voxel MRS techniques provide important information about tumor heterogeneity and allow targeting the region for biopsy to that of maximum spectral abnormality, resulting in an improvement of the diagnosis [26]. It was recently described that 3T MRS may show an elevated 2-hydroxyglutarate peak (2-HG) resonating at 2.25 ppm in IDH-mutant diffuse astrocytomas. Mutations in IDH1/2 confer a gain-of-function neomorphic enzymatic activity, resulting in the aberrant production and subsequent accumulation of 2-HG, which has been suggested to be an oncometabolite for this genetic mutation [27]. Magnetic resonance spectroscopy (MRS) has been identified as a tool in the diagnosis of IDH-mutant gliomas via the non-invasive detection of 2-HG. Although 2-HG represents an attractive marker for diagnosis and monitoring of disease progression, unambiguous detection via MRS has proven difficult to establish. Complex spectral overlap by a number of metabolites, such as glutamate, glutamine, and gamma-aminobutyric acid (GABA), found in abundance within healthy brain tissue, often confound the identification and detection of 2-HG as well as compromise accurate quantification of metabolite concentration. Several methods for detection of 2-HG in vivo have been proposed to optimize MRS for this application [27,28,29,30,31]. These encompass a range of acquisition and post-processing protocols designed to eliminate the confounding spectral overlap, and reliably quantify the 2-HG concentration in patients with IDH-mutant gliomas. The feasibility of detection of 2-HG in vivo at clinical strengths (3 T), using a standard single-voxel double echo point-resolved spectroscopy (PRESS) sequence with a TE of 30 ms, has been reported [31, 32].
Spectroscopy studies are also very useful in the assessment of response to therapy. The sensitivity of this technique in fact exceeds that of conventional MRI, with useful information being provided in lesions treated with chemotherapy or radiation therapy. There is general agreement that within high-dose regions that correspond to the radiation target, treatment response is reflected in reduction in the levels of choline, creatine, and NAA 2–3 months after treatment. In regions that are not responsive to the radiation treatment, levels of choline may increase, corresponding to residual or recurrent tumor. This different behavior is of paramount importance in helping to differentiate between radio necrosis and recurrence, one of the most difficult topics in oncological neuroradiology. The possibility of monitoring the efficacy of new anti-tumoral compounds explains why MRS is included as a useful tool in many experimental protocols.
The high sensitivity of MRS is not matched by its specificity. Although several studies have reported that MRS makes possible the differentiation of diverse histological tumor types or abscesses or cystic lesions from neoplasms, the experience of routine daily practice has drawn attention to the risks related to the technique and warrants caution when considering differential diagnosis.
5.4.2 Diffusion Weighted Imaging and Diffusion Tensor Imaging
Diffusion-weighted MR has been widely used in the evaluation of brain tumors. With regard to extra-axial neoplasms, DWI can differentiate epidermoids from arachnoid cysts, both presenting similar signal intensity on T1- and T2-weighted images, while only epidermoids display very low ADC values [33, 34]. DWI has also been utilized in the differential diagnosis of malignant forms of meningiomas (grade WHO II–III) [35]. Primary cerebral lymphomas typically show signal hyperintensity in DWI with a low signal in the relative ADC maps, which is probably linked to the high cellularity of the tumor.
For intra-axial neoplasms it has been shown that pathological tissue has higher ADC values than healthy cerebral tissue and that the central necrotic component and the cystic component present greater diffusivity than the other components of neoplastic tissue [36]. Moreover, Brunberg et al. [37] demonstrated that edema and neoplastic tissue significantly differ in ADC values. Edema has a higher ADC value, which is probably linked to the preserved integrity of the myelin. Some studies have shown that water diffusibility is lower in high than in low-grade gliomas [38, 39], but a considerable overlap between ADCs has also been described [40]. DWI is commonly not restricted in IDH-mutant and non-mutant diffuse, anaplastic astrocytomas, and glioblastoma. ADC values obtained from standard clinical DWI are a highly significant predictor of non-enhancing glioma IDH status and may permit non-invasive molecular subtyping in accordance with the 2016 WHO classification. Low ADC values are associated with increased glioma cellularity and worse prognosis, supported by comparisons of diffusivity, histological specimens, and clinical data in multiple studies. Low diffusivity predicts poor astrocytoma survival independent from WHO grade and low ADC values are related to wild-type gliomas [41], as well as to high-grade ODs [17]. Older age, multifocality, brainstem involvement, lack of cystic change, and low ADC are independent predictors of IDH-wild-type grade II diffuse gliomas (DGs). Among these, ADCmin was most predictive with a threshold of ≤0.9 × 10−3 mm2/s conferring to it the greatest sensitivity (91%). Furthermore, while shorter progression free survival (PFS) and overall survival (OS) were seen in IDH-wild-type grade II DGs, combining IDH status and ADCmin better predicted PFS and OS than IDH status alone [42].
Some degree of DWI restriction is linked to other molecular characteristics of brain neoplasms such as MGMT methylation. MGMT promoter methylation is a strong predictor for response to alkylating agents and correlates with better survival. ADC was used as a potential surrogate biomarker for MGMT promoter methylation, however, with controversies [43,44,45,46,47,48]. In a study of Han et al. [19], the ADC value in GBMs with MGMT promoter methylation was higher than in those without MGMT promoter methylation. In accordance with several previous studies, ADC ratios or ADC minimum values are lower in tumors with unmethylated MGMT promoters than with methylated promoters [45, 46], and mean ADC had a positive relationship with the MGMT promoter methylation ratio [49] (Fig. 5.3). However, lower ADC value in MGMT promoter methylated GBMs was reported in a recent histogram analysis study [50]. Besides, no significant correlation between ADC values and MGMT promoter methylation status was also reported [48].
Diffusion tensor imaging is presently used to document the presence of white matter (WM) tracts and define their location with respect to the tumor (Fig. 5.4). Brain tumors may alter WM fibers in several ways: in particular, WM tracts may be displaced, infiltrated by tumor or edema, or destroyed [51]. Many studies have demonstrated that fractional anisotropy (FA), an index of fiber organization, decreases in the WM close to brain tumors [52, 53]. An increased ADC seems to play a major role in reducing the number of fibers, at least in symptomatic patients [54]. Diffusion tensor tractography (DTT), the main application of DTI, is the only imaging technique with the potential to generate realistic fiber-tract trajectories in the white matter (WM) of the brain in vivo [55]. DTI studies have demonstrated that edema, tissue compression, and degeneration may cause significant problems in the identification of trajectories compatible with WM tracts. Despite this, the combination of functional MRI (fMRI) and DTI is a useful tool for defining the seed region of interest for DTI-based tractography (DTT) and thus providing more comprehensive, functionally related, white matter mapping in preoperative assessment [56, 57]. Despite the high incidence of cases in which the lesion is responsible for changes that hinder the reconstruction of white matter tracts, the technique can change the surgical approach for corticotomy and define the extent of resection leading to change in the surgical procedure in 80% of cases [57, 58]. Combination of DTI-FT and intraoperative subcortical mapping makes possible the accurate identification of eloquent fiber tracts and enhances surgical performance and safety, while maintaining a high rate of functional preservation [58].
Pre-surgical planning with tractographic reconstructions and motor area representation: axial (a–f) and volume rendering (g, h). Left fronto-parietal lesion (rolandic area) is evident (a–f). The lesion dislocated anteriorly the left cortico-spinal tract (green) (a–f), inferiorly the optic radiation (violet) (g, h). Motor areas of right hand (orange) (d–f) and right face (pink) (b–d) are dislocated anteriorly
5.4.3 Perfusion Imaging
In the clinical setting, perfusion MRI has been proposed for tumor grading, identifying the best site for biopsy, for the differential diagnosis with non-neoplastic pathologies and to assess treatment response [59,60,61]. A cerebral blood volume ratio (rCBV) between the maximum value inside the tumor and the normal white matter higher than 1.75 was suggested as a threshold to distinguish between high- and low-grade gliomas [61].
In case of oligodendrogliomas (Fig. 5.2) these results are more debated since some studies demonstrated high rCBV even in low-grade tumors [62], whereas more recent studies demonstrated that perfusion MR is helpful in differentiating low-grade from anaplastic oligodendrogliomas [63]. In transforming low-grade gliomas, MR perfusion imaging demonstrated significant increases in rCBV up to 12 months before contrast enhancement was apparent on T1-weighted MR images, thus indicating the potential role of the technique in predicting malignant transformation [64]. As in high-grade gliomas, metastatic lesions show elevated rCBV. Lower rCBV values outside the enhancing component of the lesion might differentiate secondary from primary neoplasms, with a lower value in metastatic disease [65].
Moreover, rCBVmax values are significantly associated with the IDH mutational status. Recent research showed that IDH mutation leads to 2HG accumulation, resulting in decreased hypoxia-inducible-factor 1-activation and downstream inhibition of angiogenesis-related signaling [66]. As demonstrated by Kickingereder et al. [67], IDH-mutant and wild-type tumors were both associated with distinct imaging phenotypes and were predictable with rCBV imaging in a clinical setting (i.e., IDH-mutant tumors represented considerably lower rCBV). In a recent study, the rCBVmax values in IDH-mutant tumors were significantly lower than in wild types [66]. Similar results are reported in a study of Lin et al. [17] on ODs, showing that rCBV values can differentiate low- and high-grade types.
The MGMT can be regarded as an independent prognostic factor in patients with primary GBM as MGMT promoter methylation increases responsiveness to temozolomide chemotherapy. The association between MGMT methylation and CBV results is debated. Ryoo et al. [68] found significantly higher rCBV values in GBMs with an unmethylated MGMT promoter than in those with a methylated MGMT; however, they did not take the IDH1/2 mutation status into account and analyzed only a small cohort of 25 patients. Conversely, in a study of Hempel et al. [3], rCBV values were significantly higher in IDH-wild-type GBMs with a methylated MGMT than in those with an unmethylated MGMT. These findings support the hypotheses of Chahal et al. [69], who found that MGMT-positive cells displayed higher levels of vascular endothelial growth factor receptor 1 (VEGFR-1) compared with MGMT unmethylated U87/EV cells leading to higher vascularization of GBM.
Perfusion MRI might help in the differential diagnosis with non-neoplastic disease. In demyelinating lesions and abscess rCBV is lower than in high-grade neoplasm and in cases of demyelinating disease even lower than in normal brain tissue [70].
The size of an enhancing lesion is commonly used as a feature of tumor behavior after therapy. Despite this, it has been demonstrated that rCBV and permeability (Ktrans) assessed with perfusion MR may decrease after therapy indicating success even without changes in tumor size. Consensus panels have published recommendations concerning the use of perfusion MR in monitoring the efficacy of therapy in intra-axial tumors [71].
Lastly, recurrent high-grade neoplasms are typically characterized by high rCBV, whereas tumor necrosis is generally associated with lack of rCBV elevation [72].
5.4.4 Functional MRI
In brain tumor patients, the aim of neurosurgery is to remove as much pathologic tissue as possible, thereby increasing survival time, while simultaneously minimizing the risk of postoperative neurological deficits [73]. Functional MR imaging is increasingly being used as part of the routine preoperative work-up of patients to establish the relationship of the lesion to eloquent areas, such as language or motor areas, and to evaluate hemispheric dominance. Identifying these areas purely on an anatomical basis is inexact, owing to considerable interindividual anatomical and functional variability, especially for language representation. Moreover, in the presence of a lesion, functional areas may be displaced due to mass effect, or function may have shifted to other areas in the brain due to plasticity [74] (Fig. 5.4). A preoperative functional MR imaging study of the main brain functions provides information on the feasibility of surgery and allows adequate assessment of the risk of postoperative neurologic deficits.
For optimal results, the relationship between the tumor margins and the functionally important brain areas needs to be established as accurately as possible [75].
The correlation between functional areas, as established with functional MR imaging versus intraoperative electrocortical stimulation, has been studied for both motor and, to a lesser extent, language representation brain areas. A high correlation has been shown for motor representation areas, but results from language representation studies are conflicting and disappointing.
Bizzi et al. [76] showed that the diagnostic performance of functional MR imaging may change according to the grade of the glioma: sensitivity is higher and specificity is lower in grade II and III gliomas than in glioblastoma multiforme, particularly for functional MR imaging of language. In patients with Rolando area tumors, the sensitivity and specificity of functional MR imaging are higher (88% and 87%, respectively) than in patients with a mass near language cortical areas (80% and 78%, respectively).
In conclusion, although functional MR imaging cannot yet replace intraoperative electrocortical stimulation in patients undergoing neurosurgery, it may be useful for guiding surgical planning and mapping, thereby reducing the extent and duration of craniotomy [77]. Moreover the combination of functional MRI and DTI-based tractography provides more complete preoperative cortical and subcortical mapping.
References
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131:803–20.
Castellano A, Falini A. Progress in neuro-imaging of brain tumors. Curr Opin Oncol. 2016;28:484–93.
Hempel JM, Schittenhelm J, Klose U, Bender B, Bier G, Skardelly M, et al. In vivo molecular profiling of human glioma: cross-sectional observational study using dynamic susceptibility contrast magnetic resonance perfusion imaging. Clin Neuroradiol. 2018:21.
Reuss DE, Kratz A, Sahm F, Capper D, Schrimpf D, Koelsche C, et al. Adult IDH wild type astrocytomas biologically and clinically resolve into other tumor entities. Acta Neuropathol. 2015;130:407–17.
Reuss DE, Mamatjan Y, Schrimpf D, Capper D, Hovestadt V, Kratz A, et al. IDH mutant diffuse and anaplastic astrocytomas have similar age at presentation and little difference in survival: a grading problem for WHO. Acta Neuropathol. 2015;129:867–73.
Ebrahimi A, Skardelly M, Bonzheim I, Ott I, Mühleisen H, Eckert F, et al. ATRX immunostaining predicts IDH and H3F3A status in gliomas. Acta Neuropathol Commun. 2016;4:60.
Pekmezci M, Rice T, Molinaro AM, Walsh KM, Decker PA, Hansen H, et al. Adult infiltrating gliomas with WHO 2016 integrated diagnosis: additional prognostic roles of ATRX and TERT. Acta Neuropathol. 2017;133:1001–16.
Abedalthagafi M, Phillips JJ, Kim GE, Mueller S, Haas-Kogen DA, Marshall RE, et al. The alternative lengthening of telomere phenotype is significantly associated with loss of ATRX expression in high-grade pediatric and adult astrocytomas: a multi-institutional study of 214 astrocytomas. Mod Pathol. 2013;26:1425–32.
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352:997–1003.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96.
van den Bent MJ, Baumert B, Erridge SC, Vogelbaum MA, Nowak AK, Sanson M, et al. Interim results from the CATNON trial (EORTC study 26053-22054) of treatment with concurrent and adjuvant temozolomide for 1p/19q non-co-deleted anaplastic glioma: a phase 3, randomised, open-label intergroup study. Lancet. 2017;390:1645–53.
Gevaert O, Mitchell LA, Achrol AS, Xu J, Echegaray S, Steinberg GK, et al. Glioblastoma multiforme: exploratory radiogenomic analysis by using quantitative image features. Radiology. 2015;276:313.
Falini A, Romano A, Bozzao A. Tumours. Neurol Sci. 2008;29:S327–32.
Del Sole A, Falini A, Ravasi L, Ottobrini L, De Marchis D, Bombardieri E, et al. Anatomical and biochemical investigation of primary brain tumours. Eur J Nucl Med. 2001;28:1851–72.
Jacobs AH, Kracht LW, Gossmann A, Rüger MA, Thomas AV, Thiel A, et al. Imaging in neurooncology. NeuroRx. 2005;2:333–47.
Cha S. Update on brain tumor imaging: from anatomy to physiology. AJNR Am J Neuroradiol. 2006;27:475–87.
Lin Y, Xing Z, She D, Yang X, Zheng Y, Xiao Z, et al. IDH mutant and 1p/19q co-deleted oligodendrogliomas: tumor grade stratification using diffusion-, susceptibility-, and perfusion-weighted MRI. Neuroradiology. 2017;59:555–62.
Ellingson BM, Lai A, Harris RJ, Selfridge JM, Yong WH, Das K, et al. Probabilistic radiographic atlas of glioblastoma phenotypes. AJNR Am J Neuroradiol. 2013;34:533–40.
Han Y, Yan LF, Wang XB, Sun YZ, Zhang X, Liu ZC, et al. Structural and advanced imaging in predicting MGMT promoter methylation of primary glioblastoma: a region of interest based analysis. BMC Cancer. 2018;18:215.
Xi YB, Guo F, Xu ZL, Li C, Wei W, Tian P, et al. Radiomics signature: a potential biomarker for the prediction of MGMT promoter methylation in glioblastoma. J Magn Reson Imaging. 2018;47:1380–7.
Demaerel P, Johannik K, Van Hecke P, Van Ongeval C, Verellen S, Marchal G, et al. Localized 1H NMR spectroscopy in fifty cases of newly diagnosed intracranial tumors. J Comput Assist Tomogr. 1991;15:67–76.
Negendank WG, Sauter R, Brown TR, Evelhoch JL, Falini A, Gotsis ED, et al. Proton magnetic resonance spectroscopy in patients with glial tumors: a multicenter study. J Neurosurg. 1996;84:449–58.
Preul MC, Caramanos Z, Collins DL, Villemure JG, Leblanc R, Olivier A, et al. Accurate, noninvasive diagnosis of human brain tumors by using proton magnetic resonance spectroscopy. Nat Med. 1996;2:323–5.
Somorjai RL, Dolenko B, Nikulin AK, Pizzi N, Scarth G, Zhilkin P, et al. Classification of 1H MR spectra of human brain neoplasms: the influence of preprocessing and computerized consensus diagnosis on classification accuracy. J Magn Reson Imaging. 1996;6:437–44.
Tedeschi G, Lundbom N, Raman R, Bonavita S, Duyn JH, Alger JR, et al. Increased choline signal coinciding with malignant degeneration of cerebral gliomas: a serial proton magnetic resonance spectroscopy imaging study. J Neurosurg. 1997;87:516–24.
Dowling C, Bollen AW, Noworolski SM, McDermott MW, Barbaro NM, Day MR, et al. Preoperative proton MR spectroscopic imaging of brain tumors: correlation with histopathologic analysis of resection specimens. AJNR Am J Neuroradiol. 2001;22:604–12.
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462:739–44.
Choi C, Ganji SK, DeBerardinis RJ, Hatanpaa KJ, Rakheja D, Kovacs Z, et al. 2-Hydroxyglutarate detection by magnetic resonance spectroscopy in IDH-mutated patients with gliomas. Nat Med. 2012;18:624–9.
Andronesi OC, Kim G, Gerstner E, Batchelor T, Tzika AA, Fantin VR, et al. Detection of 2-hydoxyglutarate in IDH-mutated glioma patients by spectral-editing and 2D correlation magnetic resonance spectroscopy. Sci Transl Med. 2012;4:116ra4.
Emir UE, Larkin SJ, De Pennington N, Voets N, Plaha P, Stacey R, et al. Noninvasive quantification of 2-hydroxyglutarate in human gliomas with IDH1 and IDH2 mutations. Cancer Res. 2016;76:43–9.
Pope WB, Prins RM, Thomas MA, Nagarajan R, Yen KE, Bittinger MA, et al. Non-invasive detection of 2-hydroxyglutarate and other metabolites in IDH1 mutant glioma patients using magnetic resonance spectroscopy. J Neurooncol. 2012;107:197–205.
Leather T, Jenkinson MD, Das K, Poptani H. Magnetic resonance spectroscopy for detection of 2-hydroxyglutarate as a biomarker for IDH mutation in gliomas. Metabolites. 2017;7:29.
Tsuruda J, Chew W, Moseley M, Norman D. Diffusion-weighted MR imaging of the brain: value of differentiating between extra-axial cysts and epidermoid tumors. AJNR Am J Neuroradiol. 1990;11:925–31.
Maeda M, Kawamura Y, Tamagawa Y, Matsuda T, Itoh S, Kimura H, et al. Intravoxel incoherent motion (IVIM) MRI in intracranial, extra-axial tumors and cysts. J Comput Assist Tomogr. 1992;16:514–8.
Filippi CG, Edgar MA, Ulug A, Prowda JC, Heier LA, Zimmerman RD. Appearance of meningiomas on diffusion- weighted images: correlating diffusion constants with histopathologic findings. AJNR Am J Neuroradiol. 2001;22:65–72.
Tien R, Felsberg G, Friedman H, Brown M, MacFall J. MR imaging of high grade cerebral gliomas: value of diffusion-weighted echoplanar pulse sequences. AJR Am J Roentgenol. 1994;162:671–7.
Brunberg J, Chenevert T, Mckeever P, Ross DA, Junck LR, Muraszko KM, et al. In vivo MR determination of water diffusion coefficients and diffusion anisotropy: correlation with structural alteration in gliomas of the cerebral hemisphere. AJNR Am J Neuroradiol. 1995;16:361–7.
Yang D, Korogi Y, Sugahara T, Kitajima M, Shigematsu Y, Liang L, et al. Cerebral gliomas: prospective comparison of multivoxel 2D chemical-shift imaging proton MR spectroscopy, echoplanar perfusion and diffusion weighted MRI. Neuroradiology. 2002;44:656–66.
Bulakbasi N, Kocaoglu M, Ors F, Tayfun C, Uçöz T. Combination of single-voxel proton MR spectroscopy and apparent diffusion coefficient calculation in the evaluation of common brain tumors. AJNR Am J Neuroradiol. 2003;24:225–33.
Kono K, Inoue Y, Nakayama K, Shakudo M, Morino M, Ohata K, et al. The role of diffusion weighted imaging in patients with brain tumors. AJNR Am J Neuroradiol. 2001;22:1081–8.
Thust SC, Hassanein S, Bisdas S, Rees JH, Hyare H, Maynard JA, et al. Apparent diffusion coefficient for molecular subtyping of non-gadolinium-enhancing WHO grade II/III glioma: volumetric segmentation versus two-dimensional region of interest analysis. Eur Radiol. 2018;28:3779–88.
Villanueva-Meyer JE, Wood MD, Choi BS, Mabray MC, Butowski NA, Tihan T, et al. MRI features and IDH mutational status of grade II diffuse gliomas: impact on diagnosis and prognosis. AJR Am J Roentgenol. 2018;210:621–8.
Ahn SS, Shin NY, Chang JH, Kim SH, Kim EH, Kim DW, et al. Prediction of methylguanine methyltransferase promoter methylation in glioblastoma using dynamic contrast-enhanced magnetic resonance and diffusion tensor imaging. J Neurosurg. 2014;121:367–73.
Gupta A, Omuro AM, Shah AD, Graber JJ, Shi W, Zhang Z, et al. Continuing the search for MR imaging biomarkers for MGMT promoter methylation status: conventional and perfusion MRI revisited. Neuroradiology. 2012;54:641–3.
Moon WJ, Choi JW, Roh HG, Lim SD, Koh YC. Imaging parameters of high grade gliomas in relation to the MGMT promoter methylation status: the CT, diffusion tensor imaging, and perfusion MR imaging. Neuroradiology. 2012;54:555–63.
Romano A, Calabria LF, Tavanti F, Minniti G, Rossi-Espagnet MC, Coppola V, et al. Apparent diffusion coefficient obtained by magnetic resonance imaging as a prognostic marker in glioblastomas: correlation with MGMT promoter methylation status. Eur Radiol. 2013;23:513–20.
Rundle-Thiele D, Day B, Stringer B, Fay M, Martin J, Jeffree RL, et al. Using the apparent diffusion coefficient to identifying MGMT promoter methylation status early in glioblastoma: importance of analytical method. J Med Radiat Sci. 2015;62:92–8.
Choi YS, Ahn SS, Kim DW, Chang JH, Kang SG, Kim EH, et al. Incremental prognostic value of ADC histogram analysis over MGMT promoter methylation status in patients with glioblastoma. Radiology. 2016;281:175–84.
Sunwoo L, Choi SH, Park CK, Kim JW, Yi KS, Lee WJ, et al. Correlation of apparent diffusion coefficient values measured by diffusion MRI and MGMT promoter methylation semiquantitatively analyzed with MS-MLPA in patients with glioblastoma multiforme. J Magn Reson Imaging. 2013;37:351–8.
Pope WB, Lai A, Mehta R, Kim HJ, Qiao J, Young JR, et al. Apparent diffusion coefficient histogram analysis stratifies progression-free survival in newly diagnosed bevacizumab-treated glioblastoma. AJNR Am J Neuroradiol. 2011;32:882–9.
Laundre BJ, Jellison BJ, Badie B, Alexander AL, Field AS. Diffusion tensor imaging of corticospinal tract before and after mass resection as correlated with clinical motor findings: preliminary data. AJNR Am J Neuroradiol. 2005;26:791–6.
Field AS, Alexander AL, Wu YC, Hasan KM, Witwer B, Badie B. Diffusion tensor eigenvector directional color imaging patterns in the evaluation of cerebral white matter tracts altered by tumor. J Magn Reson Imaging. 2004;20:555–62.
Price SJ, Burnet NG, Donovan T, Green HA, Peña A, Antoun NM, et al. Diffusion tensor imaging of brain tumors at 3T: a potential tool for assessing white matter tract invasion? Clin Radiol. 2003;58:455–62.
Romano A, Fasoli F, Ferrante M. Fiber density index, fractional anisotropy, ADC and clinical motor findings in the white matter of patients with glioblastoma. Eur Radiol. 2008;18:331–6.
Dong Q, Welsh RC, Chenevert TL, Carlos RC, Maly-Sundgren P, Gomez-Hassan DM, et al. Clinical application of diffusion tensor imaging. J Magn Reson Imaging. 2004;19:6–18.
Arfanakis K, Gui M, Lazar M. Optimization of white matter tractography for pre-surgical planning and image-guided surgery. Oncol Rep. 2006;15:1061–4.
Romano A, Ferrante M, Cipriani V. Role of magnetic resonance tractography in the preoperative planning and intraoperative assessment of patients with intra-axial brain tumours. Radiol Med. 2007;112:906–20.
Bello L, Gambini A, Castellano A, Carrabba G, Acerbi F, Fava E, et al. Motor and language DTI Fiber tracking combined with intraoperative subcortical mapping for surgical removal of gliomas. NeuroImage. 2008;39:369–82.
Law M, Yang S, Wang H, Babb JS, Johnson G, Cha S, et al. Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol. 2003;24:1989–98.
Aronen HJ, Pardo FS, Kennedy DN, Belliveau JW, Packard SD, Hsu DW, et al. High microvascular blood volume is associated with high glucose uptake and tumor angiogenesis in human gliomas. Clin Cancer Res. 2000;6:2189–200.
Knopp EA, Cha S, Johnson G, Mazumdar A, Golfinos JG, Zagzag D, et al. Glial neoplasms: dynamic contrast-enhanced T2*-weighted MR imaging. Radiology. 1999;211:791–8.
Lev MH, Ozsunar Y, Henson JW, Rasheed AA, Barest GD, Harsh GR 4th, et al. Glial tumor grading and outcome prediction using dynamic spin-echo MR susceptibility mapping compared with conventional contrast-enhanced MR: confounding effect of elevated rCBV of oligodendrogliomas. AJNR Am J Neuroradiol. 2004;25:214–21.
Spampinato MV, Smith JK, Kwock L, Ewend M, Grimme JD, Camacho DL, et al. Cerebral blood volume measurements and proton MR spectroscopy in grading of oligodendroglial tumors. AJR Am J Roentgenol. 2007;188:204–12.
Danchaivijitr N, Waldman AD, Tozer DJ, Benton CE, Brasil Caseiras G, et al. Low-grade gliomas: do changes in rCBV measurements at longitudinal perfusion- weighted MR imaging predict malignant transformation. Radiology. 2008;247:170–8.
Cha S, Lupo JM, Chen MH, Lamborn KR, McDermott MW, Berger MS, et al. Differentiation of glioblastoma multiforme and single brain metastasis by peak height and percentage of signal intensity recovery derived from dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol. 2007;28:1078–84.
Xing Z, Yang X, She D, Lin Y, Zhang Y, Cao D. Noninvasive assessment of IDH mutational status in World Health Organization grade II and III astrocytomas using DWI and DSC-PWI combined with conventional MR imaging. AJNR Am J Neuroradiol. 2017;38:1138–44.
Kickingereder P, Sahm F, Radbruch A, Wick W, Heiland S, Deimling AV, et al. IDH mutation status is associated with a distinct hypoxia/angiogenesis transcriptome signature which is non-invasively predictable with rCBV imaging in human glioma. Sci Rep. 2015;5:16238.
Ryoo I, Choi SH, Kim JH, Sohn CH, Kim SC, Shin HS, et al. Cerebral blood volume calculated by dynamic susceptibility contrast-enhanced perfusion MR imaging: preliminary correlation study with glioblastoma genetic profiles. PLoS One. 2013;19:8.
Chahal M, Xu Y, Lesniak D, Graham K, Famulski K, Christensen JG, et al. MGMT modulates glioblastoma angiogenesis and response to the tyrosine kinase inhibitor sunitinib. Neuro-Oncology. 2010;12:822–33.
Bernarding J, Braun J, Koennecke HC. Diffusion and perfusion-weighted MR imaging in a patient with acute demyelinating encephalomyelitis (ADEM). J Magn Reson Imaging. 2002;15:96–100.
Leach MO, Brindle KM, Evelhoch JL, et al. Assessment of anti-angiogenic and anti-vascular therapeutics using magnetic resonance imaging: recommendations for appropriate methodology for clinical trials. In: Proceedings of the Eleventh Meeting of the International Society for Magnetic Resonance in Medicine. Berkeley: International Society for Magnetic Resonance in Medicine; 2003. p. 1268.
Wenz F, Rempp K, Hess T, Debus J, Brix G, Engenhart R, et al. Effect of radiation on blood volume in low-grade astrocytomas and normal brain tissue: quantification with dynamic susceptibility contrast MR imaging. AJR Am J Roentgenol. 1996;166:187–93.
Duffau H. Lessons from brain mapping in surgery for low-grade glioma: insights into associations between tumour and brain plasticity. Lancet Neurol. 2005;4:476–86.
Sunaert S, Yousry TA. Clinical applications of functional magnetic resonance imaging. Neuroimaging Clin N Am. 2001;11:221–36.
Oritz C, Haughton V. Functional MR imaging: paradigms for clinical preoperative mapping. Magn Reson Imaging Clin N Am. 2003;11:529–42.
Bizzi A, Blasi V, Falini A, Ferroli P, Cadioli M, Danesi U, et al. Presurgical functional MR imaging of language and motor functions: validation with intraoperative electrocortical mapping. Radiology. 2008;248:579–89.
Smits M, Visch-Brink E, Schraa-Tam CK, Koudstaal PJ, van der Lugt A. Functional MR imaging of language processing: an overview of easy-to implement paradigms for patient care and clinical research. Radiographics. 2006;26(Suppl 1):S145–58.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Minniti, G., Romano, A., Scaringi, C., Bozzao, A. (2019). Imaging in Neuro-Oncology. In: Bartolo, M., Soffietti, R., Klein, M. (eds) Neurorehabilitation in Neuro-Oncology. Springer, Cham. https://doi.org/10.1007/978-3-319-95684-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-95684-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95683-1
Online ISBN: 978-3-319-95684-8
eBook Packages: MedicineMedicine (R0)