Abstract
Viral infections seen in the newborn nursery may be acquired in utero or during delivery. Presentations range from asymptomatic to severe multi-organ system involvement. Common viral infections encountered in the newborn nursery include cytomegalovirus (CMV), human immunodeficiency virus (HIV), herpes simplex virus (HSV), hepatitis B virus, Zika virus, and parvovirus B19. A series of case vignettes, including an approach for the clinician, is presented in this chapter.
The initial workup is focused on identifying maternal exposure and the newborn’s risk of infection. It includes obtaining a history of chronic maternal infections (HIV, hepatitis B), acute illnesses during pregnancy or delivery (CMV, HSV), travel during pregnancy (Zika), interpretation of maternal labs, and initiation of newborn workup.
CMV is the most common congenital infection and is diagnosed with polymerase chain reaction assay (PCR) on urine or saliva in the first 3 weeks of life. HIV-exposed newborns should be started on antiretroviral therapy within 6–12 h of life, and HIV DNA PCR should be sent for testing. All newborns should receive hepatitis B vaccine within 24 h of life, and if maternal hepatitis B surface antigen is positive, hepatitis B immunoglobulin should be given within 12 h of life. In an asymptomatic newborn born to a mother with active genital HSV lesions, HSV surface cultures and PCR should be sent at 24 h of life. The decision to do a further workup and start acyclovir is based on symptomatology and HSV test results. Travel to a Zika endemic region during pregnancy and maternal labs suggestive of definitive or probable Zika infection should prompt collaboration with the local Department of Health and neonatal testing for Zika infection.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Virus
- Viral infection
- Cytomegalovirus (CMV)
- Human immunodeficiency virus (HIV)
- Herpes simplex virus (HSV)
- Hepatitis B virus
- Zika virus
- Parvovirus B19
Introduction
Viral infections seen in the newborn nursery may be acquired in utero or during delivery. Human immunodeficiency virus (HIV), hepatitis B virus, cytomegalovirus (CMV), Zika virus, herpes simplex virus (HSV), and parvovirus B19 are examples of congenital infections that may be encountered in the nursery. The spectrum of these infections ranges from asymptomatic to severe multi-system organ involvement. Issues for the clinician include aspects of diagnosis and treatment.
Through a series of case vignettes, we will overview a number of these conditions and present an approach for the clinician faced with one of these scenarios.
Case Presentation
You are examining a 24-h-old female infant born at 38 weeks who failed her newborn hearing screen. Her mother works as a teacher’s aide in a child care program. The infant’s weight and head circumference are both within the 95th percentile. Physical examination is normal, without any evidence of hepatosplenomegaly, rashes, or jaundice. You order a urine CMV PCR, which returns positive. At this time, you:
-
1.
Confirm CMV testing with a urine viral culture and CMV IgM.
-
2.
Discharge the patient with pediatrician follow-up within 24 h.
-
3.
Schedule outpatient audiology follow-up for sequential hearing tests.
-
4.
Start the patient on antiviral therapy (valganciclovir).
Cytomegalovirus (CMV) infection is the most common congenital viral infection in the United States. Asymptomatic infection is the most common presentation at birth; only 10% exhibit clinical findings. Primary infection in pregnant women is often more severe and may present as a “mono-like” illness during pregnancy. Those with prior immunity to CMV may be asymptomatic. CMV infection acquired in the first half of gestation is associated with more severe sequelae in the neonate [1, 2].
The most common sequela of congenital CMV infection is sensorineural hearing loss, higher in symptomatic infections (50%), but occurring in up to 15% of asymptomatic infections. All children found to have congenital CMV infection must be evaluated with sequential hearing tests. A normal newborn hearing screen in a CMV+, asymptomatic infant does not rule out CMV-related hearing loss; 55% of symptomatic and 75% of asymptomatic children who develop CMV-associated hearing loss have a normal hearing test at birth. Hearing loss can be delayed for years, which is why sequential testing is so important [1].
Proof of congenital CMV infection must be obtained within 3 weeks of birth. Otherwise, it is impossible to differentiate perinatal/postnatally acquired infection from congenitally acquired asymptomatic infection. Diagnosis of congenital CMV includes real-time PCR of saliva, urine, or both (saliva is preferred). CMV culture has equal specificity but is less sensitive than PCR. A CMV-specific IgM, though suggestive of congenital infection, has lower specificity and a higher false-positive rate, making use of this test problematic [1].
Valganciclovir is an oral antiviral with activity against CMV. Valganciclovir is not recommended for asymptomatic neonates with isolated hearing loss or mild congenital infection (defined as mild hepatomegaly, single low platelet count, single raised ALT, and/or 1–2 isolated manifestations) [3]. Antiviral therapy is only recommended for neonates with moderate-severe symptomatic disease. Neonates with moderate-severe symptomatic congenital CMV with or without CNS involvement have improved neurodevelopmental and audiologic outcomes at age 2 when treated with valganciclovir for 6 months [4]. Moderate-severe disease is defined as multiple manifestations attributable to CMV, including hepatosplenomegaly, intrauterine growth restriction, hepatitis, thrombocytopenia, and petechiae/purpura, and CNS involvement may be present (ventriculomegaly, periventricular echogenicity, calcifications, cortical/cerebellar malformations, chorioretinitis, hearing loss).
Significant neutropenia occurs in 20% of infants treated with valganciclovir . Absolute neutrophil counts should be checked weekly for the first 6 weeks, at 8 weeks, and then monthly for the remainder of the treatment [4].
Answer:
3
Case Presentation
A healthy 38-week-old male was born abruptly via NSVD to a mother with a history of HIV infection . Maternal viral load was >1000 copies/ml throughout pregnancy, and she reports noncompliance with her antiretroviral therapy. For the infant, the next best step is to:
-
1.
Start zidovudine (AZT).
-
2.
Obtain an HIV genotype.
-
3.
Start nevirapine and zidovudine.
-
4.
Obtain an HIV DNA PCR to assess viral load.
Mother-to-child HIV transmission can occur in utero, during labor and delivery, or postnatally through breastfeeding [5]. Since the 1990s, a sharp decrease in rates of mother-to-child HIV transmission has been observed in the United States due to antenatal HIV testing, antiretroviral (ARV) prophylaxis, combination ARV during pregnancy, cesarean delivery before labor (when indicated), and avoidance of breastfeeding and pre-mastication of food [6].
Most transmission occurs during the intrapartum period. Risk factors include elevated maternal viral load and duration of exposure (e.g., prolonged ruptured membranes, breastfeeding).Without any intervention, the risk of transmission from an HIV-infected mother to her infant is 22.6–25.5% [7].
In infants, a DNA PCR is the preferred diagnostic test for HIV. RNA assays have similar specificity and sensitivity, but there is greater clinical experience with DNA assays. False-negative RNA assays may occur in infants receiving ARV prophylaxis. Serology is not helpful in diagnosing children under 18–24 months of age, as infants born to HIV-infected mothers acquire maternal antibodies passively.
To reduce the risk of perinatal transmission, all HIV-exposed infants should receive ARV prophylaxis as close to birth as possible (within 6–12 h of delivery). If infected, 95% of infants will have positive results by 1 month. Infants should be tested sequentially in follow-up with an infectious diseases specialist [5].
A combination prophylaxis regimen (zidovudine and nevirapine ) should be considered in HIV-exposed infants whose mothers are “high risk”: those who have not received antepartum or intrapartum ARV, have only received intrapartum ARV, or have not achieved viral suppression near delivery [6].
Infants of mothers who report compliance with their medications throughout pregnancy, or whose viral loads are undetectable, are considered “low risk” and should be started solely on zidovudine (AZT) [6, 7]. Both the infant and mother should have prescriptions for ARV before leaving the hospital. A 4-week regimen can be used for full-term infants when the mother has been adherent to a standard ARV regimen during pregnancy with sustained viral suppression. The most common side effect of AZT is bone marrow suppression. A CBC and differential should be performed on newborns as a baseline evaluation [5].
For infants born to mothers with unknown HIV status, expedited HIV testing of mothers and infants is recommended, with immediate initiation of infant ARV prophylaxis if the initial test is positive [6].
Answer:
3
Case Presentation
You are seeing a full-term 24-h-old male whose mother traveled to Ecuador 2 months prior to delivery. She recalls fever, rash, and fatigue 2 weeks post-travel. She has been tested for Zika virus and reports “Zika RNA detected.” After a thorough physical exam of the infant, you find no abnormalities.
At this time, you:
-
1.
Order a neurology consult for evaluation of sequelae of Zika.
-
2.
Refer the baby for outpatient infectious disease follow-up in 1–2 months.
-
3.
Provide reassurance, and discharge the infant with close follow-up with his pediatrician.
-
4.
Perform hearing testing, ophthalmology exam, Zika laboratory testing, and head ultrasound.
Zika virus infection during pregnancy can cause severe fetal brain defects. Congenital Zika syndrome is characterized by microcephaly, intracranial calcifications and other brain anomalies, eye anomalies, tremors, seizures, and/or irritability. Clubfoot and joint contractures (arthrogryposis) have also been observed [8].
Practitioners should ask about potential congenital Zika exposure for every newborn, including travel/residence in an area with risk of Zika during pregnancy or 8-week preconception and/or unprotected sex during pregnancy/preconception with a partner with this exposure (who did not receive testing) [8]. See the CDC website (as referenced) for a full list of countries with Zika risk.
For infants without evidence of birth defects consistent with congenital Zika syndrome born to mothers without laboratory evidence of Zika virus infection during pregnancy, further evaluation and testing for Zika virus are not recommended unless abnormalities are noted on physical exam [8]. A full, detailed algorithm of testing and follow-up can be found on the CDC website.
For infants without evidence of birth defects consistent with congenital Zika syndrome born to mothers with laboratory evidence of Zika virus infection during pregnancy, Zika virus testing and a comprehensive physical exam (including growth parameters and repeated, consistent head circumference measurements) should be performed. A head ultrasound, ABR (automated auditory brain stem response), and ophthalmology exam should be performed within 1 month of birth [8].
For infants with evidence of birth defects consistent with congenital Zika syndrome born to mothers with possible exposure to Zika virus during pregnancy (regardless of mother’s Zika test results), the above testing should be performed with additional referrals to early intervention services and a developmental specialist. Consultation with infectious diseases, genetics, and neurology should also be considered. Family support should be made available, and infants should be continually monitored for additional clinical findings of congenital Zika syndrome, including increased intracranial pressure, dysphagia, or respiratory distress [8].
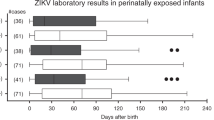
Recommended laboratory testing for congenital Zika syndrome includes Zika virus RNA in blood and urine and Zika virus IgM antibodies in blood. If CSF is obtained for other purposes, RNA and IgM antibody testing should be performed. Testing of cord blood is not recommended, as false-positive and false-negative results have been reported. If infant’s Zika virus RNA testing is positive, this represents a confirmed congenital Zika virus infection, regardless of IgM results. If infant’s Zika virus RNA testing is negative, but IgM is positive/equivocal, this indicates probable congenital Zika virus infection. If confirmatory testing with plaque neutralization testing (PRNT) is negative, this suggests that the infant’s IgM test is a false positive. If both Zika RNA and IgM are negative, congenital Zika virus infection is unlikely [8].
Answer:
4
Case Presentation
A call comes from the labor and delivery room. The OB/GYN resident informs you of a 20-year-old female in active labor with painful genital ulcers. They have high suspicion for genital herpes simplex infection and have sent an HSV PCR from a genital lesion as well as maternal serology for HSV-1, HSV-2 IgG, and IgM. Later in the day, you examine the baby. His weight is 6 lbs (2700 grams), and physical exam is normal with no rashes. At this time, the next best step is:
-
1.
Reassure the mother as the baby is completely asymptomatic.
-
2.
Obtain HSV surface cultures now.
-
3.
Obtain HSV surface cultures at 24 hours of life.
-
4.
Obtain HSV surface cultures if lesions develop.
Neonatal herpes simplex virus (HSV) infection has an estimated incidence of 1 in 3000 to 1 in 20,000 live births in the United States. HSV is a DNA virus capable of establishing latency after primary infection. There are two types, HSV -1 and HSV-2, both of which can cause neonatal disease. The management of an asymptomatic neonate born to a mother with active genital herpes simplex virus infection poses a challenge. HSV is an uncommon infection in neonates, despite a 20% rate of genital herpes among adults in the United States, and signs of neonatal infection are often not apparent until the second to third week of life.
As delineated in the report of the Committee on Infectious Diseases and Committee on Fetus and Newborn of American Academy of Pediatrics [9], the risk of neonatal HSV infection depends upon five factors:
-
(a)
Type of maternal infection (primary versus recurrent): The risk of neonatal HSV is 57% in primary infection and 2% in recurrent infection.
-
(b)
Maternal HSV antibody status: The risk is lower with preexisting maternal antibodies.
-
(c)
Duration of rupture of membranes (increased risk if ≥4 h).
-
(d)
Integrity of mucocutaneous barrier (e.g., use of a fetal scalp monitoring device increases risk).
-
(e)
Mode of delivery (increased risk with vaginal delivery).
After obtaining maternal information as listed above, a through physical examination should be performed. If a skin lesion is seen, the base of the vesicle or ulcer should be scraped and sent for HSV culture in viral transport medium. The sensitivity of HSV PCR on surface specimens has not been studied; therefore if used, it should be sent in addition to HSV cultures.
If the baby is asymptomatic with a normal exam, surface cultures and HSV DNA blood PCR should be obtained at 24 h of life. Surface cultures are obtained from the conjunctivae, mouth, nasopharynx, and rectum. The rationale for waiting for 24 h is detection of a virus at that time represents viral replication at infant’s mucosal membrane, rather than contamination from maternal lesions.
After 3 days, the parents are anxious to go home. The baby is still asymptomatic, but the HSV culture comes back positive. At this time, the next best step is to:
-
1.
Reassure the parents as the baby is still asymptomatic and discharge home.
-
2.
Obtain CSF for HSV PCR and start PO acyclovir.
-
3.
Obtain CSF for HSV PCR and start IV acyclovir.
-
4.
Repeat surface cultures and observe.
If the baby remains asymptomatic and 48-h HSV surface cultures and serum PCR are negative, then the baby can safely go home, provided other parameters of discharge are met.
If the baby remains asymptomatic but HSV surface cultures and/or serum PCR return positive, the neonate should undergo a complete evaluation, including CSF for HSV PCR as well as serum alanine aminotransferase to determine the extent of infection. The neonate should be started on intravenous acyclovir at a dose of 60 mg/kg/day divided every 8 h [10].
If this evaluation is normal, it will imply that the baby acquired HSV infection but did not develop HSV disease. In this situation the duration of acyclovir is 10 days. In terms of symptomatic neonatal HSV infection, about 45% of cases present with skin eye mouth (SEM) disease, 30% present with CNS disease (with or without skin involvement), and 25% develop disseminated disease.
Answer:
3
Case Presentation
You are seeing a newborn girl at 37 weeks of gestation born to a 35-year-old Chinese mother. While reviewing the prenatal laboratory testing, you notice the hepatitis screen is not available. The baby received hepatitis B vaccination in the delivery room. The baby is 5 lb and 5 ounces (2500 grams) and appropriate for gestational age. Physical examination is normal with no hepatomegaly. The next best step in this baby’s management would be to:
-
1.
Administer hepatitis B immunoglobulin at a dose of 0.5 ml within 12 h.
-
2.
Administer hepatitis B immunoglobulin at a dose of 0.5 ml within 7 days.
-
3.
Obtain maternal hepatitis B surface antibody and antigen.
-
4.
Reassure the mother as the baby is asymptomatic.
Hepatitis B virus (HBV ) is a DNA virus transmitted through blood or other bodily fluids. Perinatal transmission of HBV is highly efficient and usually occurs via blood exposure during labor and delivery. All pregnant women should be screened for hepatitis B surface antigen (HBsAg) at the first prenatal visit.
In the United States, a comprehensive immunization strategy to eliminate perinatal HBV transmission has been implemented [11]. The core elements of this program include (a) universal immunization of all infants beginning at birth and (b) postexposure prophylaxis with hepatitis B immunoglobulin in neonates born to mothers with a positive HBsAg or unknown hepatitis B status.
Hepatitis B vaccine is >90% effective in preventing infection. Without postexposure hepatitis B immunoglobulin (HBIG) prophylaxis, the risk of an infant acquiring HBV from a HBsAg+, HBeAg+ mother is 70–90%. The risk is 5–20% for infants born to HBsAg+, HBeAg− mothers.
Recommendations are provided by the Centers of Disease Control and Prevention based on risk of infection [12] (Table 8.1).
Other hepatitis B serological and nucleic acid testing classifies maternal infection as either acute or chronic infection, as well as predicts infectivity to the baby. The presence of hepatitis B DNA and hepatitis B e-antigen infers high infectivity. A positive HB core antibody (anti-HBc) may represent chronic HBV infection. Pediatricians should be aware that passively transferred maternal anti-HBc is detectable for as long as 24 months among infants born to HBsAg-positive women.
Answer:
3
Clinical Pearls
-
Testing for CMV in newborns must be performed within the first 3 weeks if congenital infection is suspected, using a real-time PCR on a specimen of urine or saliva.
-
Valganciclovir antiviral therapy is not recommended for asymptomatic neonates with isolated hearing loss or mild congenital infection, only those with moderate-severe symptomatic infections.
-
Only 30–40% of HIV-infected infants will have positive DNA PCR assay results before 48 h of life. All HIV-exposed infants should receive ARV therapy as close to birth as possible (within 6–12 h).
-
Laboratory testing for Zika virus is recommended for infants with birth defects consistent with congenital Zika syndrome (regardless of mother’s Zika test results) and infants without birth defects consistent with congenital Zika syndrome whose mothers have laboratory evidence of Zika virus infection during pregnancy. See CDC algorithm for full details.
-
Most cases of neonatal HSV occur in infants born to mothers whom are unaware they are infected. The risk of neonatal infection is 57% in primary infection, as opposed 2% in recurrent infection.
-
All infants should receive hepatitis B vaccination within 24 h of birth, and infants born to mothers with positive hepatitis B surface antigen should receive hepatitis B immunoglobulin as well within 12 h.
References
American Academy of Pediatrics. Cytomegalovirus. In: Kimberlin DW, editor. Red book: 2015 report of the committee on infectious diseases. 30th ed. Elk Grove: American Academy of Pediatrics; 2015.
CDC: Congenital CMV Infection. https://www.cdc.gov/cmv/congenital-infection.html. Accessed August, 2017.
Rawlinson WD, Boppana SB, Fowler KB, et al. Congenital CMV infection in pregnancy and the neonate: consensus recommendations for prevention, diagnosis, and therapy. Lancet Infect Dis. 2017;17(6):e177–88.
Kimberlin DW, Jester PM, Sanchez PJ, et al. Valganciclovir for symptomatic congenital CMV disease. N Engl J Med. 2015;372(10):933–43.
Postpartum Care Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States: Initial Postnatal Management of the HIV-Exposed Neonate. https://aidsinfo.nih.gov/guidelines/html/3/perinatal-guidelines/188/initial-postnatal-management-of-the-hiv-exposed-neonate. Accessed August, 2017.
CDC: HIV Infection. https://www.cdc.gov/globalaids/Resources/pmtct-care/docs/%20Complete_Presentation_Bklt.pdf. Accessed August, 2017.
American Academy of Pediatrics. HIV infection. In: Kimberlin DW, editor. Red Book: 2015 report of the committee on infectious diseases. 30th ed. Elk Grove: American Academy of Pediatrics; 2015.
CDC: Zika virus: Healthcare Providers Caring for Infants and Children. https://www.cdc.gov/zika/hc-providers/infants-children.html. Accessed August, 2017.
Kimberlin DW, Baley J. Committee on infectious diseases; committee on fetus and newborn. Guidance on management of asymptomatic neonates born to women with active genital herpes lesions. Pediatrics. 2013;131(2):e635–46.
American Academy of Pediatrics. Herpes simplex. In: Kimberlin DW, editor. Red Book: 2015 report of the committee on infectious diseases. 30th ed. Elk Grove: American Academy of Pediatrics; 2015.
American Academy of Pediatrics. Hepatitis B. In: Kimberlin DW, editor. Red Book: 2015 report of the committee on infectious diseases. 30th ed. Elk Grove: American Academy of Pediatrics; 2015.
Centers for Disease Control and Prevention. A comprehensive immunization strategy to eliminate transmission of hepatititis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP); Part 1 : immunizatoion of infants, children and adolescents. MMWR. 2005;54(RR–16).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Noor, A., Fiorito, T.M., Krilov, L.R. (2019). Viral Infections in the Nursery. In: Martin, G., Rosenfeld, W. (eds) Common Problems in the Newborn Nursery. Springer, Cham. https://doi.org/10.1007/978-3-319-95672-5_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-95672-5_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95671-8
Online ISBN: 978-3-319-95672-5
eBook Packages: MedicineMedicine (R0)