Abstract
The neonate is uniquely susceptible to bacterial infections, which can range from a subtle to a flagrant presentation. Early identification and treatment of bacterial infection in the newborn can prevent major complications and often depend on consideration of risk factors—such as chorioamnionitis and prolonged rupture of the membranes—in combination with careful, repeated physical examinations.
This chapter presents cases that illustrate key principles of diagnosing and treating neonatal sepsis and meningitis. It reviews appropriate steps in evaluating a newborn with a history and clinical presentation suggestive of sepsis, including the value of screening laboratory tests, such as C-reactive protein and procalcitonin. The chapter also reviews a significant recent development in the field of neonatal sepsis: introduction of a publicly accessible calculator to quantify a newborn’s risk, based on maternal history and clinical presentation. This sepsis calculator is powered by large clinical datasets and represents an important step forward in the effort to rationally assess the risk of sepsis.
While bacterial infection should be considered early in the evaluation of any baby with an unstable presentation, not all symptomatic newborns require antibiotics. This chapter also aims to discuss the familiar dilemma of when and how to evaluate and empirically treat symptomatic newborns, emphasizing that in some cases—particularly during the first 6 h of life when the physiologic transition may still be occurring—watchful waiting is an appropriate course of action.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Sepsis
- Meningitis
- Sepsis calculator
- Chorioamnionitis
- C-reactive protein
- Procalcitonin
- Group B Streptococcus
Introduction
The perinatal period is a time of increased susceptibility to bacterial infections. While recent literature has shown that the amnioplacental unit has a distinct and likely adaptive microbiome [1], the fact remains that during birth the newborn transitions from a nearly sterile milieu into an extrauterine environment teeming with bacteria. Exposure to potentially pathogenic species can occur prenatally, during passage through the birth canal, or from environmental sources after birth.
Furthermore, the neonatal immune system has key limitations that render it vulnerable to invasion by bacteria that pose little threat later in childhood (e.g., group B Streptococcus). Adaptive immunity—which depends on a diverse repertoire of antibodies against foreign antigens—is rudimentary at birth, consisting mainly of maternal IgG transferred across the placenta during pregnancy.
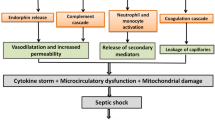
Neonatal innate immunity is also relatively weak compared with later in childhood. Neutrophils , the first responders to developing infection, are less abundant and less effective during the newborn period [2, 3]. Newborn skin and mucosal barriers are more permeable to bacteria [4]. Finally, the baby’s own colonizing microbiome, which primes the immune system and excludes potential pathogens, takes months to become established and stabilized [5, 6]. Underdevelopment of these protective systems leaves the newborn at high risk of infection.
Many newborn bacterial infections present with non-specific signs, which can be subtle in the early stages. For the practitioner in the nursery, the challenge is maintaining a high level of suspicion and readiness to act with appropriate urgency if there is persuasive evidence of infection while simultaneously recognizing that the majority of babies with mild symptoms early in life are not actually infected.
Case Presentation
You arrive at the nursery, where a 3-h-old, ex-39-week gestation, 4.1 kg boy awaits your assessment. His primiparous mother is a healthy 32-year-old. Delivery was by Cesarean section following arrest of descent, 22 h after spontaneous rupture of the membranes. The amniotic fluid was clear. A maternal temperature of 101.5 °C was recorded 60 min before delivery, which her obstetrician attributed to her epidural anesthesia. There was fetal tachycardia to 190 beats per minute coincident with the fever. Maternal GBS screening at 35 weeks was negative, and she received no intrapartum antibiotics. Her CBC and differential, drawn an hour before delivery, were unremarkable.
The baby is pink and comfortably sleeping. You note a respiratory rate of 70 breaths per minute, with no retractions. Other vital signs are normal for a newborn. During your examination, he wakes briefly and cries but otherwise remains asleep. There are no other significant examination findings. The nurse says that he has breastfed once since birth. His blood glucose level was 53 mmol/L before feeding and rose to 65 mmol/L after feeding.
What risk factor for early-onset sepsis is present in this case?
-
1.
Chorioamnionitis.
-
2.
Prolonged rupture of membranes.
-
3.
Male gender.
-
4.
Hypoglycemia.
Prolonged rupture of membranes (≥18 h) is a risk factor for early-onset sepsis (sepsis that develops within the first 72 h of life). Shorter durations of rupture are also associated with sepsis risk that increases over time [7]. The chorioamniotic membranes and the amniotic fluid together provide an important physical and immunologic barrier against bacterial infection of the fetus. Ex vivo studies of intact membrane samples have shown that they are impermeable to GBS, even at high inoculum densities [8]. Amniotic fluid is rich in antimicrobial peptides (AMPs), and bacterial exposure increases AMP expression by the membranes [9].
When these integrated protective barriers are compromised for a prolonged period, bacteria that have ascended from the lower reproductive tract are able to multiply in the uterine cavity, colonize the fetus, and potentially invade the bloodstream before or shortly after birth, leading to early-onset sepsis.
Chorioamnionitis , meaning invasion of the membranes and amniotic fluid by a pathogenic microorganism, is an independent risk factor for early-onset sepsis [10], but was not diagnosed in this case. The diagnosis of chorioamnionitis is typically made based on clinical criteria of maternal fever plus two of the five additional signs: maternal leukocytosis, maternal tachycardia, fetal tachycardia, uterine tenderness, and purulent amniotic fluid. The diagnosis can also be made based on histological identification of placental infection.
In reality, however, studies have shown that formal criteria for diagnosing maternal chorioamnionitis are frequently bypassed by practitioners, who make the diagnosis of chorioamnionitis on the basis of maternal fever alone [11]. This can put the provider in a difficult position: caring for a newborn whose mother was diagnosed with chorioamnionitis on the basis of a single criterion that may have other potential causes (such as epidural anesthesia).
While the most recent versions of official guidelines for managing newborns with risk factors for sepsis recommend a conservative approach—with automatic empiric antibiotic administration —to babies whose mothers were diagnosed with chorioamnionitis [12,13,14], a consensus among neonatologists has been shifting toward a more nuanced approach. Many believe that, when the only risk factor is maternal chorioamnionitis (regardless of how it was diagnosed), term or late-preterm newborns without symptoms can be safely managed with regularly scheduled serial examinations rather than a laboratory workup and empiric antibiotics [15]. Strong evidence is accruing for this approach [16,17,18], and updated guidelines with a greater degree of flexibility are likely forthcoming.
Hypoglycemia is a non-specific sign of early-onset sepsis, but is not an independent risk factor, and the blood glucose measurements reported in this case are normal for a newborn. Male gender is not an independent risk factor for early-onset sepsis.
Answer:
2
Case Presentation (Continued)
Over the next 2 h, the baby’s condition deteriorates. By 5 h of age, he is tachypneic to 100 breaths per minute, and his tone is decreased.
Your next step should be to obtain:
-
1.
Blood culture.
-
2.
Surface cultures of the axilla and ear canal.
-
3.
Head ultrasound.
-
4.
Urine culture.
Signs of early-onset sepsis are variable and often non-specific. A previously well-appearing newborn who develops abnormal vital signs and a concerning physical examination should always prompt consideration of infection. In these circumstances, multiple steps should be taken: blood should be drawn for culture, a complete blood count, and C-reactive protein or procalcitonin measurement. A repeat blood glucose evaluation would also be prudent. At least one chest X-ray should be obtained as part of an evaluation for early-onset sepsis, which often develops from an underlying pneumonia.
Urinary tract infection, though a common infection in older infants, is extremely unusual in the immediate newborn period (unless there is an underlying genitourinary malformation). Urine culture should therefore not be part of routine evaluations for early-onset sepsis. If surface cultures are positive, they represent colonization and not infection. They add expense to the sepsis workup and provide very little information.
Answer:
1
Although central nervous system injury could present with tachypnea and hypotonia, there was no suggestion of hypoxic/ischemic injury during birth, and a sudden deterioration at 3–5 h of life should prompt assessment for infection before brain imaging.
Although not among the answer choices, a lumbar puncture might also be reasonably performed along with the blood culture at this time. Lumbar puncture is appropriate for babies with signs highly suggestive of sepsis, regardless of the blood culture status. Obtaining a cerebrospinal fluid sample prior to initiating antibiotics increases the odds of growing the causative organism. However, in cases where the diagnosis of sepsis is less clear but still necessary to exclude with a blood culture, it is acceptable to proceed without a lumbar puncture . If the blood culture does grow a pathogen, a lumbar puncture can be performed after antibiotics are initiated, often permitting meningitis to be diagnosed or excluded based on spinal fluid glucose, protein concentrations, and cell counts.
Case Presentation (Continued)
The baby is started on ampicillin and gentamicin and transferred to the neonatal ICU. Twenty-two hours after the blood culture is drawn, the laboratory confirms that it grew group B Streptococcus . A subsequent lumbar puncture yields CSF with glucose 15 mmol/L, protein 730 mg/dL, 10,000 RBC/μL, and 95 nucleated cells/μL with 90% PMNs and 10% lymphocytes.
Antibiotics should be started at anti-meningitis dosages when ruling out early-onset sepsis.
-
1.
True
-
2.
False
Multiple factors, including the dose, affect an antibiotic’s ability to cross the blood-brain barrier [19]. Inflammation disrupts intercellular tight junctions, improving the penetrance of hydrophilic antibiotics (e.g., β-lactams and vancomycin) but not lipophilic antibiotics (e.g., fluoroquinolones and rifampin). Low molecular weight drugs penetrate more easily than those with higher molecular weight. Other factors include the degree of protein binding (antibiotics which are more tightly bound to serum proteins are less penetrant), presence of active transport systems, and specific etiology of the infection (L. monocytogenes causes more permeability than E. coli, for instance).
Ampicillin and gentamicin provide reasonably broad coverage against Gram-positive and Gram-negative bacteria in the cerebrospinal fluid and have synergistic effects for group B Streptococcus, Listeria, and Enterococcus that promote rapid sterilization of the central nervous system.
Adequate meningitis treatment consists of intravenous ampicillin 150 mg/kg per dose every 12 h and gentamicin 4 mg/kg per dose every 24 h. These doses are recommended regardless of whether a lumbar puncture has been performed. As mentioned above, in the case that the blood culture turns positive, a lumbar puncture can still provide significant diagnostic value even if the cerebrospinal fluid is already sterile.
Proven group B Streptococcus meningitis can be treated with ampicillin monotherapy for 14 days following the first negative blood culture. Combination of ampicillin and cefotaxime (75 mg/kg every 12 h) therapy is a good choice for early-onset meningitis without a definite organism (e.g., based on cerebrospinal fluid leukocytosis and elevated protein) in the setting of negative blood cultures.
Answer:
1
Approximately what percent of infants with early-onset sepsis due to group B Streptococcus are born to mothers with negative colonization screens?
-
1.
5%.
-
2.
20%.
-
3.
40%.
-
4.
70%.
Antenatal screening for maternal colonization with GBS and administration of intrapartum antibiotics have reduced the incidence of early-onset GBS sepsis from 1.7/1000 to 0.28/1000 live births [20, 21]. Screening has had no effect on the incidence of late-onset GBS sepsis. The majority of early-onset group B Streptococcus sepsis (between 60% and 75%) occurs in babies whose mother’s antenatal colonization screen was negative [21]. Negative colonization screens in mothers whose babies develop group B Streptococcus early-onset sepsis may reflect improper testing procedures, maternal factors that decrease test sensitivity (such as undisclosed antibiotic use), or late colonization in the intervening weeks between the negative screen and delivery.
Answer:
4
What is the upper limit of acceptable CSF leukocytosis in a term neonate on day of life 1?
-
1.
Any leukocytes in the CSF are indicative of meningitis
-
2.
8 cells/μL.
-
3.
14 cells/μL.
-
4.
40 cells/μL.
The normal CSF leukocyte count decreases during the first 7–10 days of life, eventually stabilizing at a mean count of 5 cells/μL [22]. A 2012 prospective study examined CSF indices in hospitalized babies undergoing lumbar puncture as part of sepsis evaluations that were ultimately negative (i.e., no definitive evidence of meningitis or bacteremia, Table 7.1) [23].
Among 130 term babies whose lumbar puncture was performed during the first week of life, the upper limit of normal CSF leukocytosis was 14 cells/μL (the upper limit was defined as the 75th percentile plus 1.5 × the interquartile range).
Answer:
3
The resident on service asks about correcting the number of WBCs in the CSF for the number of RBCs because the lumbar puncture was traumatic.
What is the best way to correct the CSF leukocyte count for blood contamination in a traumatic lumbar puncture ?
-
1.
Set the acceptable leukocyte threshold at 0.002 × CSF RBC.
-
2.
Set the acceptable leukocyte threshold at (blood WBC × CSF RBC)/(blood RBC × 1000,000).
-
3.
For every 1000 RBC/μL CSF, add 2 to the upper limit of normal CSF leukocytes.
-
4.
Do not make any correction for the blood contamination.
Variants of the first three corrections have been used over the years, but have not held up under systematic scrutiny. Specifically, several groups have examined records from traumatic lumbar punctures in children ultimately found not to have meningitis (based on clinical course and culture results). Comparisons between measured CSF leukocyte counts from these traumatic lumbar punctures and predicted counts based on proposed correction factors have shown a poor correlation [24].
While it can be tempting to allow a higher CSF leukocyte count in babies whose CSF is contaminated with blood, the prudent approach is to retain standard test limits. Babies with true bacterial meningitis usually exhibit other abnormal CSF values (such as low CSF glucose concentrations) and clinical signs. This fact can be helpful when deciding how to proceed in a case where the CSF leukocyte count is slightly elevated and blood contamination is present.
Answer:
4
Case Presentation
You are caring for a 3-day-old, ex-38-week gestation boy whose mother had postpartum hemorrhage, complicating her discharge home. The pregnancy was uncomplicated. Maternal antenatal laboratory studies were normal except for a positive screen for group B Streptococcus, for which she received appropriate intrapartum antibiotic prophylaxis.
Until today, the baby has had an uneventful course, rooming in with the mother. This is her second child, and breastfeeding was established smoothly. Serial physical examinations have been unremarkable except for a mild pectus excavatum and a Mongolian spot.
Today the mother reports that the baby has been much more irritable and difficult to console. He has been feeding poorly since early morning, pulling off the breast and crying for up to 15 min at a time. He had a stool at midnight and a wet diaper at 8 AM, but no urine for the past 5 h. No fever has been recorded.
On examination, he is awake and crying loudly. When briefly calmed with a pacifier, his respiratory rate is 85 breaths per minute with mild retractions that are accentuated by his pectus. You note mild clear rhinorrhea . Lung auscultation is clear bilaterally. The cardiac exam is normal. The abdomen is soft and non-tender, with normal bowel sounds. His extremities are warm and well-perfused. Tone is normal.
You tell the mother that you will closely observe the baby. You also plan to send several laboratory studies.
Which sepsis screening laboratory result provides the most reassurance that the baby is uninfected?
-
1.
White blood cell count under 10,000 cells/μL.
-
2.
A normal absolute neutrophil count (ANC).
-
3.
C-reactive protein (CRP) <10 mg/L.
-
4.
Serum procalcitonin concentration > 0.2ng/mL.
The white blood cell count is a poor predictor of sepsis unless very low (<5000/μL) or very high (>40,000/μL), in which case it has a better predictive value. A normal white blood cell count in a newborn should not be reassuring (i.e., the baby may still have sepsis). The same is true for a normal ANC.
CRP and procalcitonin are two well-studied infectious biomarkers [25, 26]. Procalcitonin levels start to rise 2–3 h after onset of a bacterial infection, peak at around 12 h, and then gradually normalize over the following 48–72 h. A normal procalcitonin (less than 0.2 ng/mL) is reassuring the baby is not infected. An elevated procalcitonin level is not predictive of infection, because inflammation from any etiology can elevate procalcitonin levels.
CRP follows a similar response curve, but the initial rise is slightly delayed (6–8 h after infection), and the peak is also reached later (between 24 and 48 h) than procalcitonin. Like procalcitonin, a persistently normal CRP value (<10 mg/L) is a good evidence the baby is uninfected, while CRP elevation can result from other forms of inflammation and therefore is not a strong predictor of sepsis.
Answer:
3
Case Presentation (Continued)
The CBC returns with a normal white blood cell count and ANC. The CRP is modestly elevated at 15.5 mg/L. The baby remains fussy and has had two dry diapers in a row. You decide to initiate an evaluation for sepsis by drawing a blood culture.
What is an appropriate volume of blood to draw to optimize culture sensitivity?
-
1.
>0.5 mL.
-
2.
>1 mL.
-
3.
2–3 mL.
-
4.
Because symptomatic sepsis requires a bacterial concentration of at least 1 × 106 bacteria/mL blood, the volume doesn’t matter; if the baby has sepsis, the culture will grow.
Several clinical and laboratory studies have shown that symptomatic sepsis can occur in the setting of bacterial burdens low enough that blood culture volumes <1 mL might not grow [27, 28]. Sensitivity is improved significantly if an adequate volume is obtained. Since a volume > 1 mL will grow—even in the setting of very low bacterial burden—there is no advantage to drawing 2–3 mL of blood. The size of the blood culture bottle itself (adult vs. pediatric) does not impact the sensitivity.
Answer:
2
Case Presentation (Continued)
You are preparing to draw the culture when the baby’s 3-year-old brother enters the room with his father. Both appear tired. The 3-year-old has rhinorrhea , and the father speaks with a hoarse voice before pausing for a coughing fit.
The best test to identify the likely cause of the infant’s symptoms is:
-
1.
A tracheal aspirate to check for growth of Streptococcus pneumoniae.
-
2.
Urine culture for cytomegalovirus.
-
3.
A viral PCR panel from a nasotracheal aspirate sample.
-
4.
A rapid screen for group A Streptococcus pharyngitis.
Common respiratory viruses are a frequent (and often overlooked) cause of fussiness and poor feeding in neonates. A recent prospective study found that, out of 137 infants with suspected late-onset sepsis, 7% had a viral infection [29]. A variety of high-sensitivity, high-specificity PCR- and ELISA-based assays are now widely available and should be strongly considered when evaluating a symptomatic infant with any potential respiratory viral exposures.
Answer:
3
Importantly, just because a newborn has a viral infection rather than bacterial sepsis does not mean that he or she does not need medical attention. Viruses that rarely cause severe illness in older children and adults, such as rhinovirus, can lead to significant dehydration, hyperbilirubinemia, and poor weight gain in a newborn who cannot feed adequately. Adenovirus , which is rarely serious in older patients, can cause life-threatening multiorgan system failure in newborns. The baby in the scenario should be closely observed. Laboratory testing to track electrolytes and serum bilirubin would be appropriate, and he may need transfer to the NICU for respiratory support, fluid replacement, or both. The time required to receive viral testing results varies between hospitals. Empiric antibiotics should not be withheld while awaiting viral testing results, since there is substantial overlap between the presentations of viral and bacterial infections in the newborn.
Tracheal aspirate Gram stain and culture studies are sometimes used when diagnosing ventilator-associated pneumonia , but are not useful in babies with mild, non-specific symptoms. The trachea is not a sterile site, and colonization by a variety of microorganisms occurs quickly during and after birth [6]. Bacteria that grow from a suctioned tracheal sputum sample are likely harmless commensals.
Perinatal transmission of cytomegalovirus (not to be confused with congenital cytomegalovirus, which implies vertical transmission earlier in pregnancy) is usually asymptomatic but in a subset of babies can cause pneumonitis that presents with tachypnea, retractions, wheezing, and poor feeding. The family history in this case is more suggestive of a respiratory virus.
“Strep throat” from group A Streptococcus infection does not occur during the neonatal period (group A Streptococcus can cause neonatal sepsis, however).
Case Presentation
You attend the Cesarean section delivery of a 38-week gestation baby girl. The mother is a 32-year-old primigravida whose pregnancy has been complicated by gestational diabetes, group B Streptococcus urinary tract infection at 20 weeks’ gestation, and persistent breech positioning of the fetus. The Cesarean delivery, performed because of the fetal position, occurs 3 h after the onset of spontaneous labor. One dose of penicillin was administered an hour before delivery. The membranes are ruptured in the operating room just prior to delivery. The amniotic fluid is clear. The highest maternal temperature recorded was 99.1°F. The baby emerges pink, cries vigorously, and is dried under radiant warmth. The Apgar scores are 9 and 9 at 1 and 5 min, respectively.
At 30 min of life, she has a respiratory rate of 70 breaths per minute with expiratory grunting and symmetric intercostal and subcostal retractions. Her oxygen saturation is 98%. Her lungs are mildly coarse to auscultation bilaterally, with decent aeration. You provide nasotracheal suctioning and gentle chest percussion.
At 2 h of life, the baby is still grunting. Her blood glucose is normal, and she has made one attempt at breastfeeding. Her vital signs are essentially unchanged, and her oxygen saturation remains >95%.
At this point, you should:
-
1.
Allow the infant to room in with the mother.
-
2.
Draw a blood culture and start ampicillin and gentamicin.
-
3.
Transfer the baby to the NICU for CPAP.
-
4.
Continue close observation.
The physiologic transition to extrauterine life can be marked by a period of mild respiratory distress, sometimes lasting up to 6 h. It is important that the newborn not be simply left to her mother’s care. In this case, incomplete administration of intrapartum antibiotic prophylaxis for maternal GBS colonization represents a risk factor for sepsis. However, decisions about whether to perform a workup should ultimately be driven by the newborn’s clinical status and should take into consideration that the transition to extrauterine life is not instantaneous. While the risk of sepsis in this case is low, close monitoring for resolution or worsening of symptoms remains essential. Observations should be at least hourly until symptoms resolve.
Answer:
4
While talking with the mother, she asks you, “What are the odds that my baby has a bacterial infection”?
What tool or measure can you use to establish an estimate of the sepsis risk in this case?
-
1.
Gastric aspirate analysis.
-
2.
A sepsis screen using neutrophil indices and CRP.
-
3.
An online sepsis risk calculator .
-
4.
Histopathological examination of the placenta.
A 2011 study by Puopolo et al. used records from over 600,000 mother-infant pairs to establish an online, publically accessible, data-driven algorithm for determining the risk of early-onset sepsis in babies ≥34 weeks’ gestation based on maternal risk factors [30].
An updated version of the online sepsis calculator , released in 2014, stratifies neonatal risk based on postnatal physical exam findings [31]. The calculator is available online at https://neonatalsepsiscalculator.kaiserpermanente.org. Entering this baby’s data reveals a risk of early-onset sepsis of 0.08 per 1000 live births, but taking into consideration the mild respiratory symptoms (which place the baby in the “equivocal” exam category) increases the risk to 0.38 per 1000 live births. The calculator makes management recommendations, suggesting empiric treatment for well-appearing patients whose risk factors alone place the chances of early-onset sepsis at >1.54/1000 live births and for those with equivocal clinical presentations whose risk at birth is >0.65/1000 live births. As with all recommendations, these must be viewed in the context of the complete history and clinical scenario.
Gastric aspirates contain bacteria and white blood cells found in the amniotic fluid. They are poor predictors of infection. Histopathological examination of the placenta may reveal inflammation; however, it has a poor correlation with early-onset neonatal sepsis.
Answer:
3
Case Presentation (Continued)
At 5 h of life, the baby is still mildly retracting and intermittently tachypneic, but the symptoms are improving. She is no longer grunting. Her oxygen saturation remains 98–100%. A nurse is concerned that the presentation is consistent with early-onset sepsis partially masked by the single perinatal maternal dose of penicillin.
Among babies with culture-positive early-onset sepsis, the main effect of perinatal maternal antibiotics is:
-
1.
Increased time to positivity for the infant’s blood culture.
-
2.
Need for two blood cultures in the infant.
-
3.
Increased risk of infection by resistant Gram-negative bacteria.
-
4.
No proven effect.
Although clinicians often worry about maternal antibiotics causing a false-negative infant blood culture by transiently decreasing the bacterial burden, there is no evidence that maternal antibiotics systematically alter the clinical course for septic infants [32].
Babies with signs consistent with sepsis should be managed the same way regardless of maternal antibiotic history. There is no need to draw multiple blood cultures and no data showing that maternal antibiotics increase the time required for an initial blood culture to turn positive.
While it is true that widespread use of broad-spectrum antibiotics promotes infection by resistant bacteria, there is no evidence that a single course of maternal antibiotics increases the risk of early-onset sepsis with an organism resistant to that specific antibiotic.
Answer:
4
In the case of the baby in the example, her improving symptoms within 6 h of birth are consistent with the physiologic transition to extrauterine life. Over the next 2 h, her breathing pattern normalized, and she had an uneventful course in the newborn nursery.
Clinical Pearls
-
1.
In deciding whether to perform a laboratory evaluation and treat for neonatal sepsis, one must consider historical risk factors, the infant’s clinical appearance, and the time since delivery. Remember that the postnatal transition may take up to 6 h.
-
2.
In the absence of significant risk factors for sepsis, a term or late-preterm newborn with mild or moderate respiratory signs—which are improving over the first 6 h of life—can usually be observed for resolution of the physiologic transition.
-
3.
The majority of group B Streptococcus early-onset sepsis affects infants whose mothers had negative screens for GBS colonization.
-
4.
Serial normal C-reactive protein or procalcitonin values provide a high degree of reassurance the baby is uninfected. Elevations in either measure can result from noninfectious causes.
-
5.
An adequate blood culture is >1 mL.
-
6.
There is no evidence to support algorithmic “correction” of blood contamination in CSF following a traumatic lumbar puncture.
-
7.
When assessing a newborn with signs consistent with sepsis, consider potential viral exposures.
-
8.
Urinary tract infection is uncommon in the immediate newborn period.
-
9.
Maternal antibiotic exposure will not obscure symptoms or systematically alter laboratory results in a baby with early-onset sepsis.
References
Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J. The placenta harbors a unique microbiome. Sci Transl Med. 2014;6(237):237ra65.
Schmutz N, Henry E, Jopling J, Christensen RD. Expected ranges for blood neutrophil concentrations of neonates: the Manroe and Mouzinho charts revisited. J Perinatol. 2008;28(4):275–81.
Birle A, Nebe CT, Hill S, Hartmann K, Poeschl J, Koch L. Neutrophil chemotaxis in cord blood of term and preterm neonates is reduced in preterm neonates and influenced by the mode of delivery and anaesthesia. PLoS One. 2015;10(4):e0120341.
Levy O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat Rev Immunol. 2007;7(5):379–90.
Murgas Torrazza R, Neu J. The developing intestinal microbiome and its relationship to health and disease in the neonate. J Perinatol. 2011;31(Suppl 1):S29–34.
Lal CV, Travers C, Aghai ZH, Eipers P, Jilling T, Halloran B, et al. The airway microbiome at birth. Sci Rep Nat Pub Group. 2016;6(1):31023.
Jackson GL, Rawiki P, Sendelbach D, Manning MD, Engle WD. Hospital course and short-term outcomes of term and late preterm neonates following exposure to prolonged rupture of membranes and/or chorioamnionitis. Pediatr Infect Dis J. 2012;31(1):89–90.
Kjaergaard N, Helmig RB, Schønheyder HC, Uldbjerg N, Hansen ES, Madsen H. Chorioamniotic membranes constitute a competent barrier to group b streptococcus in vitro. Eur J Obstet Gynecol Reprod Biol. 1999;83(2):165–9.
Boldenow E, Jones S, Lieberman RW, Chames MC, Aronoff DM, Xi C, et al. Antimicrobial peptide response to group B Streptococcus in human extraplacental membranes in culture. Placenta. 2013;34(6):480–5.
Wortham JM, Hansen NI, Schrag SJ, Hale E, Van Meurs K, Sánchez PJ, et al. Chorioamnionitis and culture-confirmed, early-onset neonatal infections. Pediatr Am Acad Pediatr. 2016;137(1):e20152323.
Greenberg MB, Anderson BL, Schulkin J, Norton ME, Aziz N. A first look at chorioamnionitis management practice variation among US obstetricians. Infect Dis Obstet Gynecol. 2012;2012(2):628362–9.
Verani JR, McGee L, Schrag SJ. Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). Prevention of perinatal group B streptococcal disease--revised guidelines from CDC. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports. 2010;59:1–36.
National Collaborating Centre for Women's and Children's Health (UK). Antibiotics for Early-Onset Neonatal Infection. Antibiotics for the prevention and treatment of early-onset neonatal infection. London: RCOG Press; 2012.
Polin RA. Committee on fetus and newborn. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics. 2012;129(5):1006–15.
Benitz WE, Wynn JL, Polin RA. Reappraisal of guidelines for management of neonates with suspected early-onset sepsis. J Pediatr. 2015;166(4):1070–4.
Berardi A, Buffagni AM, Rossi C, Vaccina E, Cattelani C, Gambini L, et al. Serial physical examinations, a simple and reliable tool for managing neonates at risk for early-onset sepsis. World J Clin Pediatr. 2016;5(4):358–64.
Berardi A, Fornaciari S, Rossi C, Patianna V, Bacchi Reggiani ML, Ferrari F, et al. Safety of physical examination alone for managing well-appearing neonates ≥ 35 weeks' gestation at risk for early-onset sepsis. J Matern Fetal Neonatal Med Informa Healthcare. 2015;28(10):1123–7.
Jan AI, Ramanathan R, Chorioamnionitis CRG. Management of Asymptomatic Infants ≥35 weeks without empiric antibiotics. Pediatrics. 2017;140(1):e20162744.
Sullins AK, Abdel-Rahman SM. Pharmacokinetics of antibacterial agents in the CSF of children and adolescents. Paediatr Drugs. 2013;15(2):93–117.
Hamada S, Vearncombe M, McGeer A, Shah PS. Neonatal group B streptococcal disease: incidence, presentation, and mortality. J Matern Fetal Neonatal Med. 2008;21(1):53–7.
Stoll BJ, Hansen NI, Sánchez PJ, Faix RG, Poindexter BB, Van Meurs KP, et al. Early onset neonatal sepsis: the burden of group B streptococcal and E. coli disease continues. Pediatr Am Acad Pediatr. 2011;127(5):817–26.
Martin-Ancel A, García-Alix A, Salas S, Del Castillo F, Cabañas F, Quero J. Cerebrospinal fluid leucocyte counts in healthy neonates. Arch Dis Child Fetal Neonatal Ed. 2006;91(5):F357–8.
Srinivasan L, Shah SS, Padula MA, Abbasi S, McGowan KL, Harris MC. Cerebrospinal fluid reference ranges in term and preterm infants in the neonatal intensive care unit. J Pediatr. 2012;161(4):729–34.
Bonsu BK, Harper MB. Corrections for leukocytes and percent of neutrophils do not match observations in blood-contaminated cerebrospinal fluid and have no value over uncorrected cells for diagnosis. Pediatr Infect Dis J. 2006;25(1):8–11.
Benitz WE, Han MY, Madan A, Ramachandra P. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics. 1998;102(4):E41.
Lam HS, Ng PC. Biochemical markers of neonatal sepsis. Pathology. 2008;40(2):141–8.
Schelonka RL, Chai MK, Yoder BA, Hensley D, Brockett RM, Ascher DP. Volume of blood required to detect common neonatal pathogens. J Pediatr. 1996;129(2):275–8.
Connell TG, Rele M, Cowley D, Buttery JP, Curtis N. How reliable is a negative blood culture result? Volume of blood submitted for culture in routine practice in a children's hospital. Pediatrics. 2007;119(5):891–6.
Kidszun A, Klein L, Winter J, Schmeh I, Gröndahl B, Gehring S, et al. Viral infections in neonates with suspected late-onset bacterial sepsis-a prospective cohort study. Am J Perinatol. 2017;34(1):1–7.
Puopolo KM, Draper D, Wi S, Newman TB, Zupancic J, Lieberman E, et al. Estimating the probability of neonatal early-onset infection on the basis of maternal risk factors. Pediatrics. 2011;128(5):e1155–63.
Escobar GJ, Puopolo KM, Wi S, Turk BJ, Kuzniewicz MW, Walsh EM, et al. Stratification of risk of early-onset sepsis in newborns >= 34 Weeks' gestation. Pediatrics. Am Acad Pediatr. 2014;133(1):30–6.
Sarkar SS, Bhagat I, Bhatt-Mehta V, Sarkar S. Does maternal intrapartum antibiotic treatment prolong the incubation time required for blood cultures to become positive for infants with early-onset sepsis? Am J Perinatol. 2015;32(4):357–62.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hooven, T.A., Polin, R.A. (2019). Neonatal Bacterial Infections. In: Martin, G., Rosenfeld, W. (eds) Common Problems in the Newborn Nursery. Springer, Cham. https://doi.org/10.1007/978-3-319-95672-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-95672-5_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95671-8
Online ISBN: 978-3-319-95672-5
eBook Packages: MedicineMedicine (R0)