Abstract
Ten million cases of tuberculosis occur annually in the world, and the second most frequent extrapulmonary manifestation is meningitis. Tuberculous meningitis is notoriously difficult to diagnose as the disease initially resembles many common and nonsevere illnesses, and detection of the organism is difficult, especially in young children who are particularly prone to developing the disease. The clinical manifestations closely follow the pathophysiology, much of which is determined by the host response to the organisms. Treatment requires the use of several drugs for many months and is often complicated by immune reconstitution inflammatory syndrome. All of these problems are enhanced in patients with HIV coinfection, who also may be affected by other unusual pathogens that cause similar clinical manifestations. Neuroradiology is critically important for the early and accurate diagnosis of tuberculous meningitis. While treatment has concentrated on killing the organism, there is renewed emphasis on determining how to best control the deleterious effects of the inflammation that accompanies the infection.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Tuberculosis
- Meningitis
- Tuberculoma
- Immune reconstitution inflammatory syndrome (IRIS)
- Hydrocephalus
- Vasculitis
Tuberculosis continues to be one of the most important infectious diseases in the world. Although 85% of tuberculosis cases occur in the lungs, 15% of cases occur outside of the respiratory system, with the central nervous system (CNS) being the second most common site of extrathoracic involvement. Children are more prone to extrapulmonary tuberculosis in general and to CNS tuberculosis because of their relative inability to contain the infection. Although tuberculous meningitis is uniformly fatal if untreated, early detection, combined with appropriate medical and surgical intervention, can lead to greatly improved outcomes for many patients. Tuberculous meningitis is the most common form of CNS tuberculosis, but tuberculoma, an inflammatory mass in the brain, is common in certain areas of the world [1]. In some developing countries, tuberculomas are the most common cause of mass-occupying CNS lesions, and Mycobacterium tuberculosis is the most common cause of bacterial meningitis [2].
Epidemiology
It is estimated that in 2016 10.4 million people developed tuberculosis disease in the world, with approximately 1.8 million associated deaths [3]. Tuberculosis cases in children are grossly underestimated because of the difficulty in obtaining microbiologic confirmation from young children. Many children with CNS tuberculosis are misdiagnosed as having a “bacterial meningitis.” It is not known how many cases of CNS tuberculosis actually occur, but 10–15% of children <2 years of age with untreated tuberculosis infection develop tuberculous meningitis.
There are two separate risk factors for developing tuberculosis disease. The first is the risk of becoming infected with M. tuberculosis, which depends on the person’s chance of coming into contact with a person with contagious tuberculosis. In many developing countries, infection rates of 3–5% per year are common so that the majority of young adults carry infection with M. tuberculosis. It is estimated that one third of the world’s population is infected, serving as reservoirs for future disease cases. For children, the likelihood of becoming infected with M. tuberculosis depends on the risk factors of the adults in their environment, because children rarely are contagious. Most children are infected in the home, but outbreaks of childhood tuberculosis centered in elementary and high schools, nursery schools, day care homes, churches, school buses, and stores still occur [4].
The second risk factor is the likelihood of developing disease after infection has occurred. A variety of medical conditions increase an infected person’s chance of developing disease, especially conditions that suppress the immune system. Corticosteroids and tumor necrosis factor-α antibodies are the major classes of drugs that increase the risk of infection progressing to disease. For adults with tuberculosis infection, the most important risk factor for the development of tuberculosis, including CNS tuberculosis, is coinfection with HIV. Adults who are infected with both HIV and M. tuberculosis have a 5–10% annual chance of developing tuberculosis disease, and adults with immune systems that have been damaged by HIV are more likely to develop CNS tuberculosis. The HIV epidemic has had a profound effect on the epidemiology of tuberculosis among children by two major mechanisms. First, HIV- infected adults with pulmonary tuberculosis may transmit M. tuberculosis to children, some of whom will develop tuberculosis disease, including meningitis. Second, children with HIV infection are at increased risk of experiencing progression from tuberculosis infection to disease and developing CNS tuberculomas as a complication of immune reconstitution inflammatory syndrome (IRIS). Unfortunately, both pulmonary and CNS tuberculosis in HIV-infected adults and children can be similar in clinical presentation to many other opportunistic infections that are common in this population. In general, adults and children living with HIV infection in an area endemic for tuberculosis who develop severe acute CNS disease should be given empiric antituberculosis chemotherapy until a definite diagnosis can be established.
Pathophysiology
The portal of entry for M. tuberculosis is the lung in more than 95% of cases. During the development of the lesion in the lung, bacilli escape via the bloodstream and lymphatic systems to infect many other parts of the body, most commonly the apices of the lungs, liver, spleen, lymph nodes, and meninges. This dissemination can involve either large numbers of bacilli, which leads to disseminated tuberculosis disease, or small numbers of bacilli that cause asymptomatic microscopic tuberculous foci scattered in tissues, including the meninges, which can be the origin of CNS tuberculosis that occurs years to decades later.
It was initially thought that tuberculous meningitis was a direct result of infection of the meninges from organisms spread through the blood [5]. Patients with HIV infection and tuberculosis have a higher incidence of tuberculous meningitis, including occult meningeal disease. This observation may be a result, at least in part, of the finding that up to 40% of patients with HIV infection and severe immune suppression have detectable mycobacteremia associated with their tuberculosis disease, increasing the likelihood of meningeal seeding. On the other hand, pathologic studies performed in the 1930s showed that tuberculous meningitis can occur without disease in other parts of the body; meningitis may be absent in the most extreme cases of disseminated bloodstream tuberculosis; and introduction of large numbers of bacilli into the bloodstream of susceptible laboratory animals invariably produces bloodstream tuberculosis but fails to cause tuberculous meningitis [6]. From these observations, investigators postulated that tuberculous meningitis usually arises in two stages. First, tuberculous lesions form in the brain or in the meninges from the blood-borne dissemination of bacilli early in the infection. Meningitis develops by discharge of bacilli from a subjacent focus directly into the subarachnoid space. This may explain why tuberculous meningitis is extremely rare in infants younger than 6 months of age: it takes at least 6 months for the lesion to develop. Rarely, a tuberculous lesion develops in the spinal cord or arises from a site of tuberculous spondylitis or a skull lesion. Second, proteins and other chemicals from the organisms leak into the cerebrospinal fluid (CSF), producing an intense immune reaction not unlike the reaction to a tuberculin skin test. As a result, inflammation occurs around the brain and meninges. This inflammatory reaction may damage nerves, block the circulation of CSF, and thrombose small blood vessels producing multiple cerebral infarcts. The type and extent of CNS lesions that follow this discharge of organisms and proteins into the CSF depend on the number of bacilli, their virulence, and the inflammation caused by the immune response of the host.
Several basic pathological mechanisms are responsible for the damage and symptoms caused by tuberculous meningitis. Initially, a thick exudate fills the cisterns. This exudate surrounds the base of the brain, affecting the cranial nerves and the major blood vessels at the base. The brain tissue underlying this exudate develops a variable degree of edema. As the exudate enlarges, circulation of CSF is blocked, and some degree of hydrocephalus is usually present in patients with tuberculous meningitis who have survived more than several weeks. The blockage occurs most frequently in the basal cisterns or around the outflow foramina of the fourth ventricle; it rarely occurs between the third and fourth ventricle causing aqueductal stenosis. At the same time, the inflammation causes vasculitis involving large, medium, and small arteries as well as veins emanating from the circle of Willis. Partial or complete occlusion of the arteries—most often the middle and anterior cerebral arteries—may be seen, and the venous sinuses may become thrombosed. These vascular changes result in ischemic damage or infarction that occasionally is hemorrhagic. These infarctions may be superficial but often include the basal ganglia or hypothalamus and watershed areas. In children, infarction of the brainstem also has been observed.
The pathogenesis of tuberculomas is incompletely described. They may originate from a small area of necrosis surrounded by some very large cells that form in or just below the cortex of the brain. These lesions continue to enlarge and aggregate, producing a nodule. The bacilli stimulate a local immune reaction, with resulting edema and continued inflammation in the surrounding brain. Occasionally, these lesions may stimulate extensive necrosis, causing a tuberculous brain abscess. Patients with tuberculous brain abscess become ill very rapidly and usually require immediate surgical intervention for survival.
Clinical Manifestations
Prior to the development of treatment for tuberculosis, tuberculous meningitis had a progressive course that inevitably resulted in death. However, during the past four decades, the clinical presentation has become increasingly varied, and atypical cases are now more common, particularly in developed countries [7, 8]. The clinical manifestations in an individual depend on the degree of severity of the basic pathological processes: the thick basilar exudates (resulting in cranial nerve palsies and hydrocephalus), vasculitis (resulting in infarct and focal neurological deficits), allergic reaction to antigens of the organism, cerebral edema (causing impaired consciousness and seizures), and the presence of tuberculomas. It is interesting to note that the organism genotype, drug resistance pattern, coinfection with HIV, and BCG immunization status do not consistently change the clinical manifestations.
Early diagnosis of tuberculous meningitis is notoriously difficult and delayed because the clinical onset is often gradual, occurring over 1–3 weeks [9, 10]. As a result, the presentation is subacute, and neck stiffness, the classic sign of acute meningitis, is usually lacking during the early stages. Unfortunately, early diagnosis and rapid initiation of treatment are the most important factors for determining the clinical outcome. Rarely, the onset is abrupt and marked by convulsions or rapid progression of neurological deficits.
The natural history of TB meningitis was described in the prechemotherapy era and was divided into three stages. The first stage is characterized by personality change, irritability, anorexia, weight loss, listlessness, fever, and general ill health, but no focal neurological findings on examination. Infants and toddlers in this stage often lose developmental milestones. These nonspecific signs and symptoms are differentiated from more common and less serious illnesses by their persistence and usually can be recognized as caused by tuberculous meningitis only in retrospect. After 1–2 weeks, the second stage begins with drowsiness, stiff neck, cranial nerve palsies (especially of cranial nerves III, VI, and VII), papillary abnormalities, vomiting, and convulsions. In some patients, headache and vomiting are the major complaints until a devastating neurological event occurs. In many cases, children present to medical attention repeatedly and may be misdiagnosed as having more common acute conditions [4, 7]. The second stage of tuberculous meningitis may be heralded by a sudden onset of focal neurological deficits and stroke. Hemiplegia may occur at the onset of disease or at a later stage but usually correlates with ischemic infarction in the territory of the middle cerebral artery. Quadriplegia occurs only in advanced cases after bilateral infarctions or severe generalized edema has occurred. Monoplegia is uncommon and is caused by a small vascular lesion that occurs at an early stage of disease. Rare cases of tuberculous meningitis are dominated early by abnormal movements such as choreiform or hemiballistic movements, athetosis, tremors, myoclonic jerks, or ataxia due to infarcts in the basal ganglia or thalamus. In addition, a variety of neurological and psychiatric syndromes have been described in association with tuberculous meningitis in older children and adults: acute-onset somnolence, transient amnesia, psychosis, and agoraphobia. Tuberculous encephalopathy is restricted to children and characterized by convulsions, stupor, or coma without signs of meningitis. The third stage of tuberculous meningitis is characterized by coma or stupor, irregular pulse and respirations, rising fever, and, eventually, death. Papilledema may be seen but is not a universal finding. Once the classic signs and symptoms of tuberculous meningitis have appeared, the diagnosis is easier to establish but the outcomes are far worse [11].
A tuberculoma usually presents with the symptoms and signs that occur with any intracranial space-occupying lesion. The clinical picture depends on the size and location of the tuberculoma(s), the amount of associated inflammation and edema, and the pressure they produce on adjacent structures. Headache, seizures, paralysis, personality changes, and focal neurological problems occur frequently. Children are more prone to developing infratentorial lesions, so ataxia and sudden onset of severe neurological dysfunction are more common. Children also are more likely to develop a single tuberculoma, whereas multiple and supratentorial tuberculomas are more common in adults. Small tuberculomas can be clinically silent, discovered only by neuroimaging, especially if the inflammatory reaction is minimal or suppressed.
Tuberculosis-related IRIS of the CNS is often a life-threatening complication caused by the interactions of HIV and M. tuberculosis and their respective therapies [12,13,14,15]. “Unmasking” IRIS occurs when previously unrecognized tuberculosis infection suddenly arises after starting antiretroviral therapy (ART), while “paradoxical” IRIS occurs when new or worsening signs and symptoms of CNS tuberculosis develop in a patient already under treatment for tuberculosis in whom ART was recently started. The most common manifestations are neck stiffness, symptoms caused by new intracranial and/or spinal mass lesions, radiculomyelitis, new onset or worsening of hydrocephalus, visual impairment, and seizures, which can be focal or generalized. Tuberculosis-related IRIS appears to be more common in adults than children, and associated mortality is up to 30% in adults [16]. The optimal time to initiate ART in a patient with HIV-associated CNS tuberculosis is unknown; however, it appears that the timing of the start of ART makes little difference in mortality.
Diagnosis : Some General Principles (Box 6.1)
Box 6.1 Major Challenges and Research Needs in Diagnosis
-
The initial signs and symptoms are nonspecific and mimic common less severe conditions, making early diagnosis difficult. Their persistence is characteristic of tuberculous meningitis.
-
In children, tuberculous meningitis often arises within weeks to a few months after infection. The source case often has not yet been diagnosed so the exposure history is “negative.”
-
The tests of tuberculosis infection, acid-fast stain, and PCR of the CSF are often negative, and the correct diagnosis is not considered.
-
CSF cultures for M. tuberculosis are positive in fewer than 50% of cases in most series, meaning diagnosis cannot be confirmed microbiologically and drug susceptibility results are not available.
-
All of these difficulties are greater when patients also have immune compromise, especially poorly controlled HIV infection.
-
There currently are no biomarkers or patterns of biomarkers that improve the diagnosis of CNS tuberculosis.
-
Neuroradiology is essential to support the diagnosis of tuberculous meningitis in most cases but is often unavailable in high-burden settings. The key to early diagnosis is often clinical presentation and suggestive neuroradiology findings (basilar enhancement, hydrocephalus, evidence of ischemia, or stroke).
-
Standardized methods of diagnosis should be utilized across studies to enhance the quality and comparability of tuberculous meningitis studies [17,18,19].
Diagnosis is often delayed in industrialized nations, as the lower incidence of tuberculosis results in clinicians having a low index of suspicion for the disease. As a general rule, any child or adult who presents with basilar meningitis without an obvious cause and one or a combination of stroke, cranial nerve abnormalities, or hydrocephalus should be considered to have tuberculous meningitis until proven otherwise; antituberculosis chemotherapy should be started immediately while the workup is in progress.
Establishing the diagnosis of CNS tuberculosis is often difficult because detecting the organism is not easy. One key to establishing the diagnosis is often finding another focus of tuberculosis disease, such as pulmonary tuberculosis. Many adults with CNS tuberculosis have a normal chest radiograph, but over 90% of children with meningeal tuberculosis have an abnormal chest radiograph showing adenopathy, pulmonary infiltrates, or atelectasis caused by the bronchial obstruction that is a classic sign of childhood tuberculosis. Differences in the utility of chest radiographs between children and adults may be explained at least partly by the incubation period. In children, there is a very short time between infection and the development of tuberculosis meningitis, and insufficient time has passed to heal the lung parenchyma or for adenopathy to have resolved. In adults, tuberculous meningitis may be caused by reactivation of a remote infection, and the chest radiograph is more likely to be normal. At any age, the combination of meningitis and an abnormal chest X-ray should suggest the diagnosis of tuberculous meningitis. Because tuberculous meningitis tends to be an early complication of tuberculosis infection in children, the infected patient may have had recent contact with an adult with contagious tuberculosis. However, because of the short incubation time of tuberculous meningitis in children, the contagious person may not yet have been diagnosed. Whenever tuberculous meningitis is suspected, it is critical to evaluate the adolescent and adult contacts of the patient immediately to determine if any of them have evidence of contagious pulmonary tuberculosis. Some hospitals routinely screen adults accompanying children with suspected tuberculosis by chest radiograph. This strategy prevents potentially contagious adults from nosocomial transmission of the bacteria and allows for rapid referral for medical evaluation; it also may help assist in the diagnosis of the ill child.
General Laboratory Evaluation
Most patients with tuberculous meningitis have a normal complete blood count and differential. Basic blood chemistries are often normal, although hyponatremia can be seen secondary to either the syndrome of inappropriate antidiuretic hormone secretion or salt wasting. Serum chloride and bicarbonate may be altered due to dehydration from decreased intake and emesis. The erythrocyte sedimentation rate is elevated in up to 80% of cases of tuberculous meningitis, but this is a nonspecific abnormality.
Tests of Tuberculosis Infection
The tuberculin skin test is used to determine if a patient has been infected with M. tuberculosis. A small amount of purified protein derivative is injected into the upper layer of the skin. A positive result is induration (firmness) or blistering that occurs 48–72 h after placement of the test; erythema alone should not be considered positive. Reactions of various sizes may occur, but the larger the reaction, the more likely it is caused by infection with M. tuberculosis. However, when evaluating a child for possible tuberculous meningitis, any induration in response to a tuberculin skin test should be considered significant. Unfortunately, up to 50% of adults and children with tuberculous meningitis have a negative tuberculin skin test at the time of diagnosis. Therefore, a positive tuberculin skin test can be very helpful in diagnosing tuberculous meningitis, but a negative tuberculin skin test never eliminates tuberculosis as a cause of disease.
Interferon-γ release assays (IGRAs) are also tests of infection that measure the immunological response to M. tuberculosis antigens [20]. In contrast to the tuberculin skin test, IGRAs contain only two or three proteins found primarily in M. tuberculosis and only a few nontuberculous species, increasing the specificity of the test; there is no cross-reaction with the BCG vaccine. The sensitivity of IGRAs is similar to that of the tuberculin skin test for most forms of tuberculosis disease. However, when evaluating a patient for tuberculous meningitis, optimizing sensitivity is critical, and any test (tuberculin skin test or IGRA) being positive should be considered. Often, a positive IGRA or tuberculin skin test may be the first specific evidence that a patient has tuberculosis. To maximize sensitivity, we routinely obtain a tuberculin skin test and send both commercially available IGRAs licensed in the United States (QuantiFERON [Qiagen, Inc., Hilden, Germany] and T- SPOT.TB [Oxford Immunotec, Abingdon, United Kingdom]) in patients in whom we suspect tuberculosis disease, particularly CNS disease.
Cerebrospinal Fluid Examination
Lumbar puncture reveals an elevated opening pressure in most cases of tuberculous meningitis. The CSF is usually clear and colorless but may show a pellicle or clot on standing. There is usually a moderate degree of pleocytosis not exceeding 500–1000 cells/mm3. Although polymorphonuclear cells may predominate early in the course, a change to a predominance of lymphocytes develops fairly quickly. However, an abundance of neutrophils may predict a poorer outcome and increased tendency for IRIS to occur. The lumbar CSF protein concentration is usually in the range of 100–500 mg/dl, but can be much higher. Simultaneously obtained ventricular CSF may have a normal cell count and protein because the fluid is obtained proximal to the inflammation. The protein concentration may increase as the disease progresses and may increase suddenly—to several gm/dl—if spinal block occurs because of obstruction of the outflow of CSF. Initial protein concentrations higher than 300 mg/dl correlate with a poor prognosis in adults. The CSF glucose concentration initially is in the low-normal range but declines steadily as illness progresses. One study of adults with tuberculous meningitis demonstrated that low levels of CSF glucose and high levels of lactate were associated with mortality. The measurement of adenosine deaminase levels in the CNS might be a useful adjunctive test to suggest the diagnosis of tuberculous meningitis; the reported sensitivities have ranged from 50% to 70% and the specificities from 60% to 90%, but inconsistencies in study methodology have made the results difficult to interpret [21].
Microbiology, Biomarkers, and Genetics
Microscopic examination of the spinal fluid for M. tuberculosis organisms, using an acid-fast stain, is the most important procedure for the early diagnosis of tuberculous meningitis. The frequency with which organisms are seen varies widely but depends on the amount of CSF that is sampled and the time devoted to searching for the organisms. The auramine-rhodamine (Truant) fluorescent stain is the most sensitive. Some studies have demonstrated organisms in more than 90% of consecutive cases of tuberculous meningitis in adults, but most studies have shown a far lower percentage, particularly in children. The gold standard for the diagnosis of tuberculous meningitis is to isolate M. tuberculosis in culture from the CSF. In most series of tuberculous meningitis, the organism has been isolated from the CSF in 10–50% of patients depending on the quantity of fluid cultured and the laboratory facilities. A negative CSF culture never rules out tuberculous meningitis. Gastric aspirate cultures are positive in up to 20% of children with CNS tuberculosis. Polymerase chain reaction (PCR) and other nucleic acid amplification tests performed on CSF, including GeneXpert MTB-RIF (Cepheid, Sunnyvale, California), have sensitivities of 50–85% and specificities of 88–100%, respectively, when compared with CSF stain and cultures [22, 23]. As with most tests, a positive result is valuable, but a negative result never excludes tuberculous meningitis [24].
Because of the difficulties in directly detecting M. tuberculosis, there is increasing interest in developing biomarkers both for diagnosis and to detect or monitor the degree of inflammation. While there are many specific proteins and transcriptional patterns in the CSF, no specific diagnostic biosignature of tuberculous meningitis has yet emerged. However, some patterns of biomarkers have been associated with intensity and type of inflammation and neuron cell damage; these markers may ultimately help predict and monitor anti-inflammatory therapy and establish prognosis for neurologic function [25]. There is also growing interest in host genotypes [26]. As one example, a single nucleotide polymorphism in the leukotriene A4 hydrolase (LTA4H) promoter influences the balance between proinflammatory leukotriene B4 and immunosuppressive A4; in tuberculous meningitis, this polymorphism is associated with bacterial load, inflammatory cell recruitment, patient survival, and response to anti-inflammatory therapy.
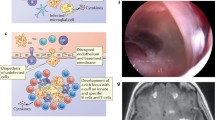
Neuroradiology
The findings on neuroimaging mirror the pathology described previously [27, 28]. Although a computed tomography (CT) scan cannot definitely establish the diagnosis of tuberculous meningitis, it is useful to rule out other diseases in patients who have an obscure illness, or evidence of increased intracranial pressure or generalized or focal neurological deficits, and to identify patients in need of prompt neurosurgical or enhanced medical intervention [29]. The most common imaging feature seen in CNS tuberculosis is hydrocephalus, noted in 80–100% of patients. The most sensitive radiologic feature (89%) is basal enhancement on a contrast-enhanced CT, with thickened meninges in the basilar areas of the brain. The most specific feature (almost 100%) is the presence of high density within the basal cisterns on a noncontrast CT. Additional findings suggestive of tuberculosis include vasculitis and thromboses causing ischemia, often visible as areas of radiolucency, particularly when located in the basal ganglia or near the Sylvian fissure. The hydrocephalus that occurs with tuberculous meningitis may increase as the patient improves; this is not a poor prognostic sign but may need to be treated with a CSF shunt or acetazolamide [30]. Magnetic resonance imaging has some advantages over CT in the evaluation of tuberculous meningitis because it allows better visualization of the exudate in the basilar cisterns and smaller infarcts in strategic locations such as the brainstem [31]. It also is better for identifying miliary leptomeningeal tubercles present in most patients with tuberculous meningitis [32].
Neuroimaging is important in monitoring the appearance and evolution of tuberculomas which usually present as one or several mass lesions surrounded by edema. The lesions are relatively avascular. The neuroradiological images of tuberculoma are nonspecific; diagnosis is usually established by biopsy or strong epidemiological or other clinic evidence of tuberculosis. These lesions can develop in patients with tuberculous meningitis who are being adequately treated [33]. With increased use of MRI, more patients have been recognized as having tuberculomas; in some case series, almost two thirds of adults with tuberculous meningitis have tuberculomas on presentation, and up to three quarters have them when imaged 2–3 months after starting therapy [34]. These so-called paradoxical tuberculomas develop after chemotherapy is started. It is thought that the development of these lesions represents an immunological phenomenon caused by inflammation as organisms are killed and proteins are released into the surrounding tissues, and is one form of IRIS .
Additional imaging should include chest radiographs, which are abnormal in >80% of children with CNS tuberculosis. The most common findings include hilar adenopathy (33%), infiltrates (33%), and miliary disease (20%).
Differential Diagnosis
While the diagnosis of tuberculous meningitis is often difficult in previously normal hosts, the difficulties are increased in patients with immune compromise, especially HIV infection, as other opportunistic infections can mimic tuberculosis [35,36,37]. The differential diagnosis of tuberculous meningitis includes fungal (e.g., cryptococcal) meningitis, viral meningoencephalitis (e.g., cytomegalovirus), and noninfectious processes such as CNS lymphoma, meningeal metastases, and sarcoidosis. Rare infectious diseases that may present a clinical picture similar to that of tuberculous meningitis include leptospirosis, brucellosis, cat-scratch encephalitis (bartonellosis), toxoplasmosis, and infection due to Naegleria. Additional considerations are focal parameningeal infections such as brain abscess, cancer, sarcoidosis, and meningitis or encephalitis that result from embolic complications of infective endocarditis. CNS vasculitis can mimic tuberculous meningitis. The differential diagnosis of tuberculomas includes infectious (abscesses, septic emboli, fungal balls) and noninfectious (primary and metastatic malignancies) causes of mass-occupying lesions.
Management and Treatment (Box 6.2)
Box 6.2 Major Challenges and Research Needs in Management and Treatment
-
As cultures are positive in only about 50% of cases, drug susceptibility results also are unknown for half the cases, meaning significant drug resistance is often missed in locales with a high prevalence of drug-resistant tuberculosis.
-
Although ethambutol is part of the WHO-recommended regimen for initial treatment of tuberculous meningitis, it penetrates into the CSF poorly. Most experts prefer a different fourth drug, classically ethionamide or amikacin, and more recently a fluoroquinolone.
-
Rifampin also penetrates poorly into the CSF. Emerging evidence has demonstrated improved outcomes using larger doses of rifampin, 20–30 mg/kg/day, with no increase in adverse drug effects.
-
Outcomes are generally poor with traditional management. Clinical trials in adults have suggested that when a fluoroquinolone, usually moxifloxacin, is included in the initial regimen, the outcomes are improved.
-
Management of acute hydrocephalus is critical. While ventriculostomy and ventriculoperitoneal shunts provide immediate relief, medical management using acetazolamide and furosemide also can be effective.
-
There is increasing emphasis on the management of the inflammation of CNS tuberculosis. Corticosteroids sometimes have limited effectiveness and a large number of potential adverse effects. More specific therapies aimed at specific cytokines or other mediators of inflammation are needed. Thalidomide has shown great potential to decrease inflammation and even restore vision in some children.
-
The prognosis of tuberculous meningitis is extremely variable and difficult to predict. Recent work on neurologic biomarkers and specific genetic alleles has demonstrated some predictive associations, but much more work is needed.
-
Management of multidrug-resistant tuberculous (MDR-TB) meningitis is extremely challenging as many second-line drugs do not penetrate well into the CSF. In addition to fluoroquinolones, linezolid has been identified as a very useful drug for MDR-TB meningitis.
Despite the use of effective antituberculosis drugs, morbidity and mortality rates from tuberculous meningitis remain high throughout the world [38]. Early death and poor clinical response are usually due to failure to recognize the disease and begin appropriate antituberculosis chemotherapy and manage the inflammation in the early stages. Because it is difficult to isolate the organism in a patient with tuberculous meningitis, initial therapy is usually empirical based on the clinical, laboratory, and radiographic data. It is important to start therapy before the diagnosis is proven because any delay may worsen the outcome substantially.
The four drugs used most often to treat drug-susceptible tuberculosis are isoniazid, rifampin, pyrazinamide, and ethambutol. While isoniazid and pyrazinamide penetrate well into the CSF, rifampin and ethambutol do not [39]. The penetration of many antituberculosis drugs is enhanced by meningeal inflammation. Pyrazinamide and isoniazid penetrate into the CSF in the presence and absence of meningeal inflammation, and their use has significantly improved the prognosis of tuberculous meningitis. There is emerging evidence that the traditional rifampin dose of 10–15 mg/kg/day, maximum of 450–600 mg, is inadequate, and many experts now recommend using rifampin doses of at least 20–30 mg/kg/day, maximum of 1200 mg or higher. There is no evidence that the major adverse reactions to rifampin are dose-dependent. The selection of a fourth drug is problematic as no comparative controlled trials have been conducted. A fourth drug likely has little influence on outcomes of drug-susceptible tuberculous meningitis but may be beneficial when the organism is resistant to isoniazid. Ethambutol has poor CSF penetration, and even though its use is recommended in several guidelines, including those of the World Health Organization, consideration should be given to replacing this drug in the initial regimen with either oral ethionamide or a fluoroquinolone or an injectable agent such as amikacin in patients with suspected tuberculous meningitis.
There are few clinical trials of the treatment of tuberculous meningitis because the condition is rare in places where clinical trials can be performed. Early studies showed that treatment with isoniazid and rifampin for 12 months was generally effective in patients with drug-susceptible tuberculous meningitis. Recent studies have shown that when pyrazinamide has been added to the regimen for the first 2 months, a 6–9-month course of therapy with isoniazid and rifampin is curative [40, 41]. Unfortunately, the incidence of drug-resistant tuberculosis is increasing in many areas of the world. In the United States, as many as 10% of M. tuberculosis isolates are resistant to at least one antituberculosis drug , and rates of drug resistance may be as high as 30–40% in other areas of the world. Treatment of drug-resistant tuberculous meningitis is challenging and outcomes are far worse even in the most experienced and technically advanced centers [42]. Experts recommend that four antituberculosis drugs be given in the initial regimen for tuberculous meningitis in adults and children; the fourth drug provides additional coverage in the event the patient has an isoniazid-resistant organism. The three drugs that are virtually always used are isoniazid, rifampin, and pyrazinamide. A fourth drug traditionally was chosen from among ethionamide or injectable agents (amikacin, capreomycin, kanamycin, or streptomycin). Recent clinical trials among adults with tuberculous meningitis have demonstrated mixed outcomes when the initial treatment regimen included high-dose rifampin and a fluoroquinolone, either moxifloxacin or levofloxacin, along with isoniazid and pyrazinamide [43,44,45]. The four-drug regimen may be narrowed after drug susceptibility testing is available if the patient is responding well to therapy. Assuming a drug-susceptible M. tuberculosis isolate is found, pyrazinamide may be stopped after 2 months, and the fourth drug (e.g., injectable agent or ethionamide) may be stopped when a pansusceptible isolate is found. Isoniazid and rifampin are continued to complete a 6–9-month course.
The optimal medical treatment of tuberculoma has never been established. Superficial tuberculomas may be treated by surgery or the combination of surgical excision and chemotherapy. However, many tuberculomas have been cured with medical therapy alone. Most experts recommend an initial three- or four-drug regimen with a total length of treatment of 9–12 months.
Tuberculous meningitis may present with signs of increased intracranial pressure due to hydrocephalus. When acute hydrocephalus develops, insertion of a ventriculostomy may be lifesaving [46]. In industrialized countries, hydrocephalus is most often managed by placement of a permanent ventriculoperitoneal shunt (VPS) or a temporary endoscopic third ventriculostomy (ETV) [47]. Studies have implied that the risk of recurrent hydrocephalus is lower with VPS, but the ETV is associated with fewer long-term complications, especially in patients with HIV coinfection [48]. In many high-incidence countries, the hydrocephalus is managed medically using acetazolamide with or without furosemide for 4–6 weeks. There have been no controlled clinical trials comparing outcomes of medical versus surgical management.
While antimicrobial therapy of tuberculous meningitis has received almost all of the previous attention, it is becoming clear that management of the inflammation is also critically important and often inadequate [49]. Corticosteroid therapy has been routinely recommended for patients with tuberculous meningitis, although large controlled studies of the effectiveness of corticosteroid therapy are not available [50,51,52]. Available evidence examined in a recent Cochran study suggests that corticosteroids reduce cerebral edema and inflammation, reduce mortality, lead to more rapid radiographic resolution, and improve outcomes and mortality in non-HIV-infected persons; unfortunately, there seems to be little benefit for people who also have HIV infection [53]. Most experts have agreed that it is best to use corticosteroids early in treatment, especially if the diagnosis has been reasonably established and the patient’s condition is critical [34]. Corticosteroids should never be administered to a patient with suspected tuberculous meningitis without also starting antituberculosis therapy. Corticosteroids are usually given for 3–6 weeks and then tapered over a period of several weeks as the patient improves. All forms of corticosteroids (dexamethasone, prednisone, prednisolone, and hydrocortisone) seem to be effective. Corticosteroids also are used in the management of CNS manifestations of IRIS .
Other anti-inflammatory agents have been studied. Aspirin has antithrombotic and anti-inflammatory properties. While a trial in adults with tuberculous meningitis showed a significant reduction in mortality at 3 months with the use of aspirin [54], a study in children demonstrated no benefit in mortality but did seem to limit development of hemiparesis [55]. Thalidomide has been used in trials involving South African children who had evidence of extreme inflammation, often in response to the large number of organisms found in tuberculous abscesses of the CNS [56, 57]. In these patients, there is a strong CNS cytokine response often including tumor necrosis factor-α [58, 59]. Thalidomide has improved outcomes in children with life-threatening tuberculous mass lesions, including those arising during IRIS, when corticosteroids have been inadequate to control the inflammation; it seems to be particularly helpful when there is visual compromise caused by optochiasmic arachnoiditis [56, 57, 60, 61]. The anti-TNF-α biologic agent infliximab has been used to reduce IRIS in two patients with neurotuberculosis [62].
The current mortality rate of tuberculous meningitis with adequate therapy is 10–20% in developed countries, but it may be as high as 30–40% in developing countries. In general, the prognosis is worse for infants and the very old, immunocompromised patients, malnourished patients, patients with associated disseminated disease, and patients who present with increased intracranial pressure.
The prognosis of meningitis correlates somewhat with the clinical stage of disease when antituberculosis chemotherapy is started [63,64,65]. The majority of patients diagnosed and treated in stage 1 have a normal outcome. Unfortunately, few patients are diagnosed at this stage. The majority of patients diagnosed in stage 3 will either die or have severe neurological sequelae. Some patients diagnosed in stage 2 have a good outcome, whereas others have persistent neurological deficits, sometimes severe. Some residual physical or cognitive deficit has been reported in 10–50% of young children with tuberculous meningitis. Visual and auditory impairments are the most common sequelae. The frequency of motor deficits after tuberculous meningitis has been reported to be 10–25%. Seizures are common in the early stages of the illness but are less common later, occurring in fewer than 10% of patients. Global developmental delay and impairment of intellect and judgment, dementia, or some degree of behavior or learning disorder are common problems in patients presenting with stage 2 or 3 disease. Endocrinopathies may become evident months or years after tuberculous meningitis. The most common forms cause obesity, hypogonadism, sexual precocity, diabetes insipidus, and growth retardation.
Predicting which patients will have sequelae can be challenging [30]. Young age, advanced state of tuberculous meningitis, presence of infarcts on CT at 1 month, and Glasgow Coma Scale scores may correlate with neurodevelopmental and behavioral outcomes [66]. The plasticity of the pediatric brain leads to many children having better neurodevelopmental outcomes than one would anticipate. However, clinicians should be cautious about estimating future developmental capacity. Often, the true developmental potential of a young child is not evident until they begin school. As with any form of bacterial meningitis, children should receive audiologic screening prior to hospital discharge. In adult patients, the presence of seizures and coma are predictors of mortality. Predictors of neurologic sequelae in this population included cranial nerve palsies and hemiparesis and hemiplegia.
Prevention (Box 6.3)
Box 6.3 Challenges and Research Needs in Prevention
-
BCG vaccines can prevent 50–80% of cases of tuberculous meningitis. However, there may be large variation in effectiveness among the various available strains of BCG, but this is largely unstudied. BCG vaccine rates are suboptimal in many high incidence locales. New, more effective tuberculosis vaccines are needed.
-
Most children who develop tuberculous meningitis do so rapidly—within weeks to a few months—after acquiring the infection. While treatment of recent tuberculosis infection is extremely effective in preventing tuberculous meningitis, it is not carried out in most high-burden settings. Contact tracing and treatment of children less than 5 years of age who are asymptomatic household contacts is recommended and should be carried out.
CNS tuberculosis will continue to occur as long as untreated tuberculosis infection occurs in adults and children. In the United States, the major methods of preventing tuberculosis infection and disease center on the public health activities of contact tracing with tests of tuberculosis infection. Identifying recently infected persons, particularly infants and toddlers and immunocompromised persons of all ages, and rapidly treating them are the best ways to prevent additional cases of tuberculosis in all its forms.
In many areas of the world, treatment of tuberculosis infection is not available. All countries of the world except the Netherlands and the United States have used BCG vaccines to prevent complications of tuberculosis infection, particularly in children. While universal BCG vaccination is still undertaken in most high-burden countries, the vaccination is more selective for specific high-risk groups in most middle- to low-burden countries. This vaccine is not very effective for preventing tuberculosis infection but is 50–80% effective in preventing serious forms of tuberculosis, such as meningitis, for at least 5 years after vaccination. Although BCG vaccines have had little impact on the control of tuberculosis globally, they have prevented countless cases of tuberculous meningitis, particularly in children, and this vaccination remains a cornerstone of the World Health Organization tuberculosis prevention programs. However, the disease will persist until a more effective vaccine is discovered [67].
References
van Well GT, Paes BF, Terwee CB, et al. Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics. 2009;123:e1–8.
van Toorn R, Solomons R. Update on the diagnosis and management of tuberculous meningitis in children. Semin Pediatr Neurol. 2014;21:12–8.
World Health Organization. Global tuberculosis report – 2017. Geneva: World Health Organization; 2017.
Doerr CA, Starke JR, Ong LT. Clinical and public health aspects of tuberculous meningitis in children. J Pediatr. 1995;127:27–33.
Donald PR, Schaaf HS, Schoeman JF. Tuberculous meningitis and miliary tuberculosis: the rich focus revisited. J Infect. 2005;50:193–5.
Rich AR, McCordock HA. The pathogenesis of tuberculous meningitis. Bull Johns Hopkins Hosp. 1933;52:5–35.
Wolzak NK, Cooke ML, Orth H, et al. The changing profile of pediatric meningitis at a referral centre in Cape Town, South Africa. J Trop Pediatr. 2012;58:491–5.
Yaramis A, Gurkan F, Elevli M, et al. Central nervous system tuberculosis in children: a review of 254 cases. Pediatrics. 1998;102:e49.
Checkley AM, Njalale Y, Scarborough M, et al. Sensitivity and specificity of an index for the diagnosis of TB meningitis in patients in an urban teaching hospital in Malawi. Trop Med Int Health. 2008;13:1042–6.
Lammie GA, Hewlett RH, Schoeman JF, et al. Tuberculous cerebrovascular disease: a review. J Infect. 2009;59:156–66.
Wiseman CA, Gie RP, Starke JR, et al. A proposed comprehensive classification of tuberculosis disease severity in children. Pediatr Infect Dis J. 2012;31:347–52.
Marais S, Meintjes G, Pepper DJ, et al. Frequency, severity, and prediction of tuberculous meningitis immune reconstitution inflammatory syndrome. Clin Infect Dis. 2013;56:450–60.
Meintjes G, Lawn S, Scano F, et al. Tuberculosis- associated immune reconstitution inflammatory syndrome: case definitions for use in resource- limited settings. Lancet Infect Dis. 2008;8:516–23.
Meintjes G, Lawn SD, Scano F, et al. International network for the study of HIV-associated IRIS. Tuberculosis-associated immune reconstitution inflammatory syndrome: case definitions for use in resource-limited settings. Lancet Infect Dis. 2008;8:516–23.
Post MJ, Thurnher MM, Clifford DB, et al. CNS- immune reconstitution inflammatory syndrome in the setting of HIV infection, Part 2: discussion of neuro-immune reconstitution inflammatory syndrome with and without other pathogens. AJNR Am J Neuroradiol. 2013;34:1308–18.
Pepper DJ, Marais S, Maartens G, et al. Neurologic manifestations of paradoxical tuberculosis-associated immune reconstitution inflammatory syndrome: a case series. Clin Infect Dis. 2009;48:e96–107.
Marais BJ, Heemskerk AD, Marais SS, et al. Standardized methods for enhance quality and comparability of tuberculous meningitis studies. Clin Infect Dis. 2017;64:501–9.
Marais S, Thwaites G, Schoeman J, et al. Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect Dis. 2010;10:803–12.
Solomons RS, Visser DH, Marais BJ, Schoeman JF, van Furth AM. Diagnostic accuracy of a uniform research case definition for TBM in children: a prospective study. Int J Tuberc Lung Dis. 2016;20:903–8.
Metcalfe JZ, Everett CK, Steingart KR, et al. Interferon-gamma release assays for active pulmonary tuberculosis diagnosis in adults in low- and middle income countries: systematic review and meta-analysis. J Infect Dis. 2011;204:S1120–9.
Xu HB, Jiang RH, Li L, Sha W, Xiao HP. Diagnostic value of adenosine deaminase in cerebrospinal fluid for tuberculous meningitis: a meta-analysis. Int J Tuberc Lung Dis. 2010;14:1382–7.
Pai M, Flores LL, Pai N, et al. Diagnostic accuracy of nucleic acid amplification tests for tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2003;3:633–43.
Tortoli E, Russo C, Piersimoni C, et al. Clinical validation of Xpert MTB/RIF for the diagnosis of extrapulmonary tuberculosis. Eur Respir J. 2012;40:442–7.
Patel VB, Theron G, Lenders L, et al. Diagnostic accuracy of quantitative PCR (Xpert MTB/RIF) for tuberculous meningitis in a high burden setting: A prospective study. PLoS Med. 2013;10:e1001536.
Rohlwink UK, Mauff K, Wilkinson KA, et al. Biomarkers of cerebral injury and inflammation in pediatric tuberculous meningitis. Clin Infect Dis. 2017;65:1298–307.
Tobin DM, Roca FJ, Oh SF, et al. Host genotype-specific therapies can optimize the inflammatory response to mycobacterial infections. Cell. 2012;148:434–46.
Andronikou S, Smith B, Hatherhill M, Douis H, Wilmshurst J. Definitive neuroradiological diagnostic features of tuberculous meningitis in children. Pediatr Radiol. 2004;34:876–85.
Gupta RK, Kumar S. Central nervous system tuberculosis. Neuroimaging Clin N Am. 2011;21:795–814.
Bruwer GE, van der Westhuizen S, Lombard CJ, et al. Can CT predict the level of CSF block in tuberculous hydrocephalus? Childs Nerv Syst. 2004;20:183–7.
Schoeman JF, Van Zyl LE, Laubscher JA, et al. Serial CT scanning in childhood tuberculous meningitis: prognostic features in 198 cases. J Child Neurol. 1995;10:320–9.
Janse van Rensburg P, Andronikou S, van Toorn R, et al. Magnetic resonance imaging of the central nervous system in children with tuberculous meningitis. Pediatr Radiol. 2008;38:1306–13.
Pienaar M, Andronikou S, van Toorn R. MRI to demonstrate features and complications of TBM not seen with CT. Childs Nerv Syst. 2009;25:941–7.
van Toorn R, Rabie H, Dramowski A, et al. Neurological manifestations of TB-IRIS: a report of 4 children. Eur J Paediatr Neurol. 2012;16:676–82.
Thwaites GE, Mac-Mullin-Price J, Tran TH, et al. Serial MRI to determine the effect of dexamethasone on the cerebral pathology of tuberculous meningitis: an observational study. Lancet Neurol. 2007;6:230–6.
Thwaites G, Chau T, Stepniewska K, et al. Diagnosis of adult tuberculous meningitis by use of clinical and laboratory features. Lancet. 2002;360:1287–92.
Thwaites GE, Nguyen DB, Nguyen HD, et al. The influence of HIV infection on clinical presentation, response to treatment, and outcome in adults with tuberculous meningitis. J Infect Dis. 2005;192:2134–41.
Youssef F, Afifi S, Azab A, et al. Differentiation of tuberculous meningitis from acute bacterial meningitis using simple clinical and laboratory parameters. Diagn Microbiol Infect Dis. 2006;55:275–8.
Thwaites GE. Advances in the diagnosis and treatment of tuberculous meningitis. Curr Opin Neurol. 2013;26:295–300.
Donald PR. Cerebrospinal fluid concentrations of antituberculous agents in adults and children. Tuberculosis (Edinb). 2010;90:279–92.
Donald PR, Schoeman JF, Vanzyl LE, et al. Intensive short-course chemotherapy in the management of tuberculous meningitis. Int J Tuberc Lung Dis. 1998;2:704–11.
van Toorn R, Schaaf HS, Laubscher JA, et al. Short intensified treatment in children with drug-susceptible tuberculous meningitis. Pediatr Infect Dis J. 2014;33:248–52.
Seddon JA, Visser DH, Bartens M, et al. Impact of drug resistance on clinical outcome in children with tuberculous meningitis. Pediatr Infect Dis J. 2012;31:711–6.
Heemskerk AD, Bang ND, Mai NT, et al. Intensified antituberculosis therapy in adults with tuberculous meningitis. N Engl J Med. 2016;374:124–34.
Heemskerk AD, Nguyen MTH, Dang HTM, et al. Clinical outcomes of patients with drug-resistant tuberculous meningitis treated with an intensified antituberculosis regimen. Clin Infect Dis. 2017;65:20–8.
Ruslami R, Ganiem AR, Dian S, et al. Intensified regimen containing rifampicin and moxifloxacin for tuberculous meningitis: an open-label, randomised controlled phase 2 trial. Lancet Infect Dis. 2013;13:27–35.
Rizvi I, Garg RK, Malhotra HS, et al. Ventriculo-peritoneal shunt surgery for tuberculous meningitis: a systematic review. J Neurol Sci. 2017;375:255–63.
Yadav YR, Parihar VS, Todorov M, et al. Role of endoscopic third ventriculostomy in tuberculous meningitis with hydrocephalus. Asian J Neurosurg. 2016;11:325–9.
Goyal P, Srivastava C, Ojha BK, et al. A randomized study of ventriculoperitoneal shunt versus endoscopic third ventriculostomy for the management of tubercular meningitis with hydrocephalus. Childs Nerv Syst. 2014;30:851–7.
Wilkinson RJ, Rohlwink U, Misra UK, et al. Tuberculous meningitis. Nat Rev Neurol. 2017;13:581–98.
Dooley DP, Carpenter JL, Rademachen S. Adjunctive corticosteroid therapy for tuberculosis: a critical reappraisal of the literature. Clin Infect Dis. 1997;25:872–87.
Schoeman JF, Van Zyl LE, Laubscher JA, Donald PR. Effect of corticosteroids on intracranial pressure, computed tomographic findings, and clinical outcome in young children with tuberculous meningitis. Pediatrics. 1997;99:226–31.
Thwaites GE, Nguyen DB, Nguyen HD, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004;351:1741–51.
Prasad K, Singh MB. Corticosteroids for managing tuberculous meningitis. Cochrane Database Syst Rev. 2016;4:CD002244. https://doi.org/10.1002/14651858.CD002244.pub4.
Misra UK, Kalita J, Nair PP. Role of aspirin in tuberculous meningitis: a randomized open label placebo controlled trial. J Neurol Sci. 2010;293:12–7.
Schoeman JF, Janse van Rensburg A, Laubsher JA, et al. The role of aspirin in childhood tuberculous meningitis. J Child Neurol. 2011;26:956–62.
Schoeman JF, Springer P, Ravenscroft A, et al. Adjuvant thalidomide therapy of childhood tuberculous meningitis: possible anti-inflammatory role. J Child Neurol. 2000;15:497–503.
van Toorn R, du Plessis A-M, Schaaf HS, Buys H, Hewlett RH, Schoeman JF. Clinicoradiologic response of neurologic tuberculous mass lesions in children treated with thalidomide. Pediatr Infect Dis J. 2015;34:214–8.
McHugh SM, Rifkin IR, Deighton J, et al. The immunosuppressive drug thalidomide induces T helper cell type 2 (Th2) and concomitantly inhibits Th1 cytokine production in mitogen- and antigen-stimulated human peripheral blood mononuclear cell cultures. Clin Exp Immunol. 1995;99:160–7.
Paravar T, Lee DJ. Thalidomide: mechanisms of action. Int Rev Immunol. 2008;27:111–35.
Schoeman JF, Andronikou S, Stefan DC, et al. Tuberculous meningitis related optic neuritis: recovery of vision with thalidomide in 4 consecutive cases. J Child Neurol. 2010;25:822–8.
Schoeman JF, Fieggen G, Seller N, et al. Intractable intracranial tuberculous infection responsive to thalidomide: report of four cases. J Child Neurol. 2006;21:301–8.
Molton JS, Huggan PJ, Archuleta S. Infliximab therapy in two cases of severe neurotuberculosis paradoxical reaction. Med J Aust. 2015;202:156–7.
Hosoglu S, Gevik MF, Balik I, et al. Predictors of outcome in patients with tuberculous meningitis. Int J Tuberc Lung Dis. 2002;6:64–70.
Thwaites GE, Simmons CP, Than Ha Quyen N, et al. Pathophysiology and prognosis in Vietnamese adults with tuberculous meningitis. J Infect Dis. 2003;188:1105–15.
van Toorn R, Springer P, Laubscher JA, et al. Value of different staging systems for predicting neurological outcome in childhood tuberculous meningitis. Int J Tuberc Lung Dis. 2012;16:628–32.
Wait JW, Schoeman JF. Behavioural profiles after tuberculous meningitis. J Trop Pediatr. 2010;56:166–71.
Hokey DA, Ginsberg A. The current state of tuberculosis vaccines. Hum Vaccine Immunother. 2013;9:2142–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Starke, J.R., Cruz, A.T. (2018). Challenges in Tuberculous Meningitis. In: Hasbun, R. (eds) Meningitis and Encephalitis. Springer, Cham. https://doi.org/10.1007/978-3-319-92678-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-92678-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92677-3
Online ISBN: 978-3-319-92678-0
eBook Packages: MedicineMedicine (R0)