Abstract
LRBA deficiency is an early-onset primary immunodeficiency (PID) caused by biallelic mutations in LRBA that abolish its protein expression. Clinically, LRBA deficiency presents with a broad clinical phenotype including immune dysregulation, recurrent infections, and hypogammaglobulinemia, accompanied by reduced expression of CTLA-4 as well as diminished numbers of regulatory T cells (Tregs), switched memory B cells, and plasmablasts. Currently, the diagnosis of LRBA deficiency is based on genome sequencing approaches, but screening diagnostic methods based on protein detection have also been implemented. LRBA-deficient patients frequently receive immune suppressive-based therapy and immunoglobulin replacement, since the implementation of HSCT as potential curative treatment for LRBA deficiency is still under debate. LRBA plays an essential role in the expression, function, and trafficking of CTLA-4 in Tregs, thereby controlling proinflammatory responses. However, the exact function of LRBA in other immune cells is not yet fully understood. Interestingly, LRBA-deficient mouse models do not mirror the human LRBA deficiency, as Lrba null mice do not present any clinical or immunological signs of disease and do not develop overt autoimmunity despite low levels of CTLA-4, reduced frequency of IL-10-producing B cells, and increased numbers of T follicular helper cells. In addition, Lrba null mice present normal B and T lymphocyte development and normal humoral response against T-dependent as well as T-independent antigens. Further analyses that elucidate the pathomechanisms of LRBA deficiency are needed in order to develop targeted therapies which improve the survival and quality life of LRBA-deficient patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
10.1 Introduction
Among the syndromes associated to immune dysregulation and antibody deficiency, we find a rare autosomal recessive disease known as lipopolysaccharide-responsive beige-like anchor (LRBA) deficiency. This syndrome was first described in 2012 in five children harboring four different homozygous mutations in LRBA, all of which abolished the LRBA protein expression [1]. LRBA deficiency presents early in life and is characterized by a wide spectrum of clinical manifestations ranging from autoimmunity, enteropathy, and organomegaly, to hypogammaglobulinemia, recurrent respiratory infections, polyendocrinopathy, growth retardation, and neurologic diseases [2,3,4,5]. Initially, LRBA deficiency was described as a monogenetic cause of common variable immunodeficiency (CVID) with autoimmune complications, as the first LRBA-deficient patients suffered mostly from recurrent infections and abnormalities in the B-cell compartment accompanied by autoimmune cytopenias [1]. However, further description from additional patients places LRBA deficiency into the expanding group of immunodysregulation syndromes due to the high frequency of different autoimmune manifestations that are observed in more than 90 affected patients described up to date worldwide.
10.2 Etiology
LRBA deficiency is caused by loss-of-protein biallelic mutations in LRBA. To date, around 50 different homozygous or compound heterozygous mutations in LRBA have been reported in the literature without showing any evident genotype-phenotype correlation [2, 3, 5]. These mutations include missense mutations, nonsense mutations, splice site mutations, deletions, and duplications, which are distributed throughout all LRBA protein domains affecting equally the protein stability [2, 3, 5]. However, residual LRBA expression has been detected in some patients harboring homozygous missense mutations at the c-terminus of the LRBA protein. One of them remains healthy at the age of 7 years, whereas the other patients present with a less severe clinical and immune phenotype [2, 6, 7]. In addition, LRBA deficiency affects similarly females and males, and there is no ethnical susceptibility reported so far.
10.3 Clinical Manifestations
Patients with LRBA deficiency manifest with a heterogeneous group of clinical symptoms and immunological findings, including:
-
Immune dysregulation is the main clinical feature of LRBA deficiency, since more than 90% of LRBA-deficient patients suffer from at least one autoimmune disorder. Inflammatory bowel disease-like (IBD-like) (Fig. 10.1), autoimmune hemolytic anemia (AIHA), and autoimmune thrombocytopenia (ITP) are the most frequent autoimmune entities affecting 62–76%, 57–70%, and 30–50% of the patients, respectively [2,3,4,5]. Chronic diarrhea and unresponsiveness to treatment have been related to growth failure observed in about 25% of LRBA-deficient patients. Juvenile idiopathic arthritis (JIA), neutropenia, chronic autoimmune hepatitis, eczema, type 1 diabetes (T1D), autoimmune thyroiditis, arthritis, uveitis, psoriasis, vitiligo, and alopecia can also occur but are less frequent [2,3,4,5]. Chronic erosive and nonerosive arthritis and polyendocrinopathy disorder have also been reported in three patients [8, 9]. Moreover, a history of atopic disorders has been documented in LRBA deficiency, such as food allergy, insect sting allergies, allergic dermatitis, urticaria, and asthma [5].
-
Organomegaly or lymphoproliferative disorders are observed in 76–86% of LRBA-deficient patients, including splenomegaly, lymphadenopathy, and hepatomegaly [2,3,4,5] (Fig. 10.1).
-
Recurrent infections are mostly affecting the upper and lower respiratory tract (70–76% of patients), including pneumonia, sinusitis, and otitis media [2,3,4,5]. These infections frequently caused parenchymal lung abnormalities such as lymphocytic infiltrates and bronchiectasis in the context of LRBA deficiency (Fig. 10.1). Bronchiolitis obliterans organizing pneumonia (BOOP) has been reported in one patient [10]. Up to date, LRBA-deficient patients do not show susceptibility to any particular pathogen, but all of them have presented at least one documented infection mostly associated to opportunistic microorganisms including, Campylobacter jejuni, Morganella morganii, Proteus mirabilis, Yersinia enterocolitica, Cryptosporidium parvum, Giardia lamblia, Legionella pneumophila, aspergillosis, and chronic mucocutaneous candidiasis (CMC) [2,3,4,5]. Infections caused by Staphylococcus aureus have also been reported [4].
-
Hypogammaglobulinemia is observed in 50–80% of LRBA-deficient patients, presenting with reduction of one, two, or three immunoglobulin isotypes. Reductions of IgG alone, or in combination with low IgM and/or IgA, are the most frequently observed entities in LRBA deficiency [2]. Specific antibody response after vaccination is however variable.
-
Neurologic complications are reported in about 20% of patients with diagnosis of LRBA deficiency [3, 5]. They include unilateral optic nerve atrophy, granuloma-like lesions coupled with a demyelinating process, and cerebral granuloma associated with strabismus, hemiplegia, and seizures. Optic neuritis, brain abscess, cerebral and cerebellar atrophy, as well as parietal lobe lesion have also been reported [3, 5].
Intestinal, pulmonary, and splenic alterations in LRBA-deficient patients. (a) Colonoscopy revealing severe circular inflammation in the rectum, numerous ulcerations, and mucosal edema and erythema. (b) Magnetic resonance image of marked splenomegaly. (c) High-resolution chest-computed tomographic scan showing atypical, partly conflating patchy alveolar consolidations in both lungs. (d) Marked regression of alveolar consolidation 2 years after therapy and slight bilateral ground-glass infiltrates (Obtained from Gámez-Diaz et al. JACI, 2017)
LRBA deficiency resembles the overall picture of patients with cytotoxic T-lymphocyte antigen 4 (CTLA-4) insufficiency, which is caused by autosomal heterozygous mutations in CTLA-4 [11]. Both syndromes are characterized by the presence of autoantibody-mediated cytopenias, organomegaly, hypogammaglobulinemia, organ-specific autoimmunity, and lymphocytic infiltration of nonlymphoid organs [12]. However, the clinical onset of LRBA deficiency is characteristically in childhood (mean age of 5 year), whereas most CTLA-4-insufficient patients developed their first symptoms in adolescence or early adulthood [12, 13]. Although CTLA-4-insufficient patients are more prone to develop malignancies, several types of tumors have also been observed in patients with LRBA deficiency, including Burkitt lymphoma [7], Epstein-Barr virus lymphoma, lymphomatous central nervous system pseudotumor [1], dysplastic tubular adenoma and polyps [14], multifocal gastric cancer, and malignant melanoma [15]. Lower mortality and morbidity are reported in CTLA-4-insufficient patients suggesting additional roles of LRBA that are CTLA-4 independent. Disease penetrance is approximately 60% in CTLA-4 mutation carriers, while LRBA deficiency presents nearly complete penetrance [11,12,13]. Furthermore, the heterogeneity of the clinical phenotype in LRBA-deficient patients is also observed in affected members from the same family carrying an identical mutation in LRBA, as demonstrated in one child harboring a homozygous mutation in LRBA who is currently healthy despite having two affected siblings with the same mutation, suggesting the existence and influence of modifier genes and microbial/environmental triggers that are still unknown [2]. In addition, LRBA deficiency should also be considered as a clinical differential diagnosis of autoimmune lymphoproliferative syndrome (ALPS), immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX), and signal transducer and activator of transcription 3 (STAT3) gain-of-function (GOF) [16]. These syndromes share several clinical similarities including autoimmune cytopenias, multi-organ autoimmunity, organomegaly, and lymphoproliferation. However, ALPS is caused by mutations in FAS, FASL, CASP10 that lead to a defective lymphocyte apoptosis mediated through the Fas/Fas ligand (FASL) pathway [17], IPEX is caused by defective suppression capacity of regulatory T cells due to mutations in the transcription factor FOXP3 [18], and somatic GOF mutations in STAT3 confer increased STAT3 transcriptional activity, impair cytokine signaling, and diminish Treg compartment [16]. A comparison of the main characteristics of these PIDs is summarized (Table 10.1).
Absence of LRBA protein expression causes LRBA deficiency, but overexpression of LRBA is associated with cancer cell growth, particularly in the kidney, pancreas, colon, rectum, and lung [19]. However, the expression levels of LRBA varied greatly depending on the tumor type and developmental stage. These results indicate that LRBA might play a role in the suppression of apoptosis, thereby facilitating cell proliferation and cell survival [19]. Additionally, increased expression of LRBA has been observed in erythroid progenitor cells suggesting the possible involvement of LRBA in hematopoietic disorders [20]. Further analysis should focus on determining the potential role of LRBA in cancer development as anticancer therapeutic target.
10.4 Pathophysiology of LRBA Deficiency
Although the exact biological role of LRBA is not fully understood, a recent study has shown that LRBA is required for the post-translational expression and trafficking of CTLA-4 [7]. CTLA-4 is a protein receptor expressed in activated conventional T cells and in regulatory T cells (Tregs). Upon stimulation of the T-cell receptor (TCR), CTLA-4 is mobilized in vesicles to the cell surface where it captures the co-stimulatory molecules CD80 and CD86 from antigen-presenting cells (APC) by a mechanism called trans-endocytosis, thereby downregulating the proinflammatory response [21]. Several negative response elements or proteins that modulate the transcriptional or the post-translational expression of CTLA-4 have been identified. Among those, the AP-1 protein complex binds to a four-amino acid (YVKM) motif of the cytoplasmic tail of CTLA-4, allowing the trafficking of CTLA-4 to AP-1 containing vesicles to lysosomes for degradation [21]. In contrast, LRBA allows the recycling of CTLA-4 to AP-1containing vesicles to the cell membrane of Tregs by binding the YVKM motif of CTLA-4, thereby blocking the AP-1-binding site and controlling the T cell activation proinflammatory response [7]. In the absence of LRBA (as seen in LRBA deficiency), diminished CTLA-4 protein levels are observed due to increased CTLA-4 lysosomal degradation due to enhanced AP-1 binding. Low CTLA-4 levels might contribute to a defective regulation of the immune response and to the development of autoimmune manifestations and lymphoproliferation that are frequently observed in LRBA-deficient patients [7, 12] (Fig. 10.2).
LRBA regulates CTLA-4 trafficking in Tregs. Upon activation of T cells, LRBA competes with higher affinity against AP-1 for binding the YVKM motif of the CTLA-4 tail. LRBA-CTLA-4 interaction is required to guide CTLA-4-containing vesicles to the cell surface in order to capture and engulf the co-stimulatory molecules CD80 and CD86 from the antigen-presenting cells (APC), thereby effectively controlling T-cell activation. In the absence of LRBA, the adaptor protein AP-1 binds to CTLA-4 leading to its lysosomal degradation (Modified from Sansom D. Science. 2015)
The mechanisms underlying the B-cell abnormalities and the antibody deficiency observed in patients with LRBA deficiency, have been attributed to the high apoptosis rate observed in LRBA-deficient B cells as a consequence of defective autophagy after serum deprivation [1]. Autophagy is a catabolic process that degrades long-lived proteins and organelles to guarantee protein homeostasis and protein quality control at steady state or especially during starvation or stress conditions, thereby supporting cell survival [22]. Interestingly, short- and long-lived plasma cells need to reshape and expand their endoplasmic reticulum (ER) in order to produce a high number of immunoglobulins after encountering an antigen [22]. This process causes severe oxidative, proteasome, and ER stress that can be counterbalanced by enhancing autophagy, thereby limiting the ER capacity and the immunoglobulin production, as well as promoting energy production and cell survival. However, when autophagy is defective, like in atg5-deficient cells, reduced B-cell survival and reduced ATP levels are observed [22], evidencing an essential role of autophagy during plasma cell differentiation. Therefore, defective autophagy in the absence of LRBA might explain the low numbers of switched memory B cells and plasmablasts.
10.5 Laboratory Findings
Immunologic abnormalities on the humoral response include decreased serum titers of IgG in 57–84% of the affected patients, solely or in combination with reduced IgM and IgA [2, 3]. Defective specific antibody response has been reported in 50–70% of LRBA-deficient patients. In addition, 40–60% of patients show a reduction of total B cells, affecting especially switched memory B cells and plasmablasts, which are detected in low counts in 80% and 90% of affected patients, respectively. In accordance, in vitro stimulated LRBA-deficient B cells failed to proliferate, differentiate into antibody-secreting cells (ASC), and induce expression of plasmablast markers, indicating defects in B-cell differentiation. Interestingly, nearly 80% of LRBA-deficient patients presented expansion of exhausted CD21low B cells, which are associated with autoimmune cytopenias in CVID [23]. T-cell counts and CD4:CD8 ratio are typically unaffected in the absence of LRBA. However, abnormal T-cell activation and in vitro hyperproliferation (upon CD3 stimulation) have been observed [7]. Aberrant regulatory T-cell functionality and reduction of the Tregs’ canonical markers, including CTLA-4, Helios, and CD25, are typical characteristics of LRBA deficiency [24]. Reduced numbers of Tregs have also been observed in about 70% of the cases [2, 24]. However, a recent study suggests that the frequency of Tregs in LRBA deficiency might be underestimated due to low CD25 expression levels, IL-2 consumption, CD4 lymphopenia, or immunosuppressive treatments that reduce FOXP3 expression [25]. Additionally, Tregs exist in human blood as FOXP3high or FOXP3low cells; therefore, low FOXP3 expression might not be indicative of low Treg numbers in LRBA deficiency [25]. In addition, elevated circulating T-follicular helper (TFH) cells biased toward a Th1-like phenotype have been observed in affected patients, reflecting the impaired control of TFH due to aberrant CTLA-4 expression in Tregs [24]. Finally, increased frequencies of of Th1-like, Th17 and Th22 cells along with increased expression of T-box transcription factor (TBET), runt-related transcription factor 1 (RUNX1) and T-cell memory phenotype (CD45RO) have also been reported [7, 26, 27].
10.6 Diagnosis
Due to the wide spectrum of clinical manifestations, LRBA deficiency should be suspected in patients presenting with hypogammaglobulinemia only (and be classified as an antibody-disorder disease), and/or autoimmune cytopenias (and be classified as an immune dysregulation syndrome), and/or inflammatory bowel disease (and be classified as enteropathy), or with a combination of all three. In addition, patients with clinical phenotypes of ALPS-Ph, IPEX-like, CTLA-4 insufficiency, and STAT3 GOF with FAS, FASL, CASP10, FOXP3, CTLA-4, and STAT3 wild-type sequences should be tested for LRBA deficiency. Currently, the diagnosis of LRBA deficiency relies on the identification of biallelic mutations in LRBA that are usually found by whole exome sequencing or targeted sequencing [2,3,4,5]. However, increased levels of LRBA protein in immune cells after stimulation can be detected by Western blotting or by flow cytometry and can be used to screen for LRBA deficiency when comparing with a healthy donor, since LRBA-biallelic mutation carriers, present complete absence or severely reduced LRBA protein. In fact, a flow cytometry-based test for LRBA deficiency has been recently pusblished. This test allows to discriminate with 94% sensitivity and 80% specificity LRBA-mutation carriers from LRBA-wild type patients [28]. Thus, LRBA protein detection might be useful as initial screening tool of suspected LRBA-deficient patients, narrowing down the amount of patients that need LRBA sequencing, thereby facilitating early diagnosis and accelerating treatment implementation [2]. Moreover, impaired CTLA-4 expression in Tregs can help to strengthen the diagnosis when suspecting LRBA deficiency. Interestingly, two functional assays allow discrimination of CTLA-4 from LRBA mutation carriers [25]. The first assay is based on the expression of CTLA-4 by memory Tregs (mTregs), in which mTregs of healthy donors express ten-fold more CTLA-4 than naïve conventional Tregs (nTcon). In contrast, mTregs from CTLA-4-insufficient and LRBA-deficient patients present only a five-fold and three-fold higher expression, respectively [25]. However, upon stimulation with CD3/CD28 beads, LRBA-deficient Tregs increase their CTLA-4 expression 20 to 30 times compared to baseline levels and even more when Tregs are treated with a lysosomal inhibitor such as bafilomycin [25]. Tregs from CTLA-4-insufficient patients on the other hand, keep a low CTLA-4 expression after stimulation, indicating that in LRBA deficiency the CTLA-4 translation is not affected. The second discriminating assay is based on the CTLA-4 trafficking in Tregs. Specifically, patients with CTLA-4 mutations present with severely reduced trans-endocytosis of CD80–CD86 molecules in Tregs, whereas this process is unaffected in LRBA-deficient patients [25]. Therefore, after clinical suspicion of LRBA deficiency, detection of LRBA protein, evaluation of CTLA-4 levels in mTregs, or measurement of CD80–CD86 trans-endocytosis depending on CTLA-4, might contribute to the diagnosis of LRBA deficiency and/or to monitor the efficacy of therapies such as in patients that underwent HSCT. The final diagnosis of LRBA deficiency relies however, on the identification of biallelic mutations in LRBA.
10.7 Management and Treatment
The clinical management of patients with LRBA deficiency is mainly focused on controlling the hypogammaglobulinemia, infections, lymphoproliferation, and autoimmunity. Hypogammaglobulinemia is treated with subcutaneous or intravenous immunoglobulin replacement, in addition to antimicrobial treatment used to control the infectious trigger [2, 3]. Immunosuppressive therapy is used to control lymphoproliferation and autoimmunity and includes steroids, rituximab, hydroxychloroquine, mycophenolate mofetil, and azathioprine among other immunosuppressant agents that are not preventing the long-term deterioration of LRBA-deficient patients [2,3,4,5, 29, 30]. Therapy with sirolimus, however, was reported to improve completely the frequency and severity of diarrhea, allowing LRBA-deficient patients to recover weight [2, 3]. In addition, based on the recent knowledge of the contribution of CTLA-4 in the pathogenesis of LRBA deficiency, therapy with abatacept (a fusion protein composed of the Fc region of human IgG1 and the extracellular part of CTLA-4 that inhibits T-cell responses by competing for costimulatory ligands) has been included as a therapeutic option. In fact, a 5–8-year follow-up of two LRBA-deficient patients treated with abatacept showed improvement of the patient’s general clinical status such as their pulmonary function. In addition, reduction of soluble CD25, which is a marker for T-cell-mediated inflammation, increase of memory T cells, reduction of T follicular helper cells, and improvement of specific antibody response to polysaccharides were observed in LRBA-deficient patients under abatacept treatment [7]. At present, 12 LRBA-deficient patients with severe clinical courses of disease that were mostly unresponsive to immunosuppression treatment underwent hematopoietic stem cell transplantation (HSCT). Four out of the 12 patients died within 3 months after HSCT due to preexisting infections, graft failure, multi-organ failure, and thrombotic microangiopathy [31]. In contrast, the remaining eight patients presented with complete, good, or partial remission. Particularly, five of those patients showed full chimerism after HSCT, presenting a significant reduction of numbers and intensity of LRBA-related symptoms without relapse and without the necessity for immunosuppressants and immunoglobulin replacement, being therefore in complete or good remission [31]. The three remaining patients are in partial remission, presenting a chimerism of less than 90% and undergoing current immunosuppressive treatment [31]. Although HSCT treatment for LRBA-deficient patients needs to be evaluated in a bigger cohort to prove its efficacy, HSCT is currently recommended, if a suitable donor is present, before the patient presents long-term organ damage that may negatively affect the results of the HSCT.
10.8 Biological Characteristics of LRBA
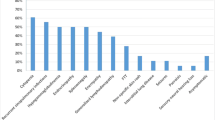
LRBA is a member of the BEACH domain-containing protein (BDCP) family along with eight other human proteins (Fig. 10.3). Among them are the lysosomal trafficking regulator (LYST), neurobeachin (NBEA), neurobeachin-like 1 (NBEAL1), neurobeachin-like 2 (NBEAL2), WD and FYVE zinc finger domain-containing protein 3 (WDFY3), WD and FYVE zinc finger domain-containing protein 4 (WDFY4), neutral sphingomyelinase activation-associated factor (NSMAF) also known as FAN, and WD repeat domain 81 (WDR81). In BDCPs, BEACH domains are located at the C-terminal end of the protein, usually preceded by a pleckstrin homology (PH) domain and followed by 4–16 repeats of WD dipeptide [32]. WD domain-containing proteins have been implicated in a wide range of cellular functions including cell cycle control, transcriptional regulation, signal transduction, autophagy, apoptosis, and vesicle trafficking [33, 34], whereas BEACH domain-containing proteins are mostly associated to act as scaffolding proteins. The N-terminal part of the BDCPs is weakly conserved, and only few domains have been identified so far. BDCPs are widely expressed in tissues, but little is known about their specific function and the molecular mechanisms through which they act. It has been suggested that they occupy individual and distinct physiological roles mainly involved in vesicle trafficking, cytokinesis, as well as receptor signaling, and that they might work as facilitators of protein-protein interactions [33, 34]. Mutations in genes encoding for BDCP members have been associated with different clinical entities, including a primary immunodeficiency known as Chediak-Higashi syndrome (CHS) and a megakaryocyte lineage disorder known as the gray platelet syndrome (GPS) [35, 36]. CHS is caused by biallelic mutations in LYST and it is characterized by hypopigmentation of the skin, eyes, and hair, prolonged bleeding times, recurrent infections, and abnormal natural killer and neutrophil function, since LYST has been suggested to be essential for sorting of cytotoxic granules [35]. On the other hand, patients with homozygous mutations in NBEAL-2 suffer from GPS, which is characterized by thrombocytopenia and enlarged platelets due to specific absence of alpha-granules [37].
In humans, LRBA is located in the region 31.3 of chromosome 4, and it shares 90% homology with its murine counterpart. According to the Ensembl (www.ensembl.org) and NCBI (National Center for Biotechnology Information: www.ncbi.nlm.nih.gov) databases, human LRBA encodes two protein transcripts, LRBA-001 (ENST00000510413; NP_001186211) and LRBA-002 (ENST00000357115; NP_006717), that are translated into proteins of 2851 aa and 2863 aa, respectively. The two isoforms differ in exon 39, which is absent in isoform 1. The biological relevance of the human isoforms and their expression in the different human tissues have not yet been evaluated. However, LRBA mRNA has been detected in several human tissues including the spleen, lymph node, thymus, tonsil, bone marrow, fetal liver, heart, placenta, lung, liver, skeletal muscle, kidney, and pancreas [1]. Finally, a homology analysis revealed that LRBA is highly conserved among species.
Computational predictions suggest that human LRBA is located in the cytosol, at the plasma membrane, in the endoplasmic reticulum, and in the Golgi apparatus. In accordance, in vitro analysis of plasmids containing BEACH-WD domains of LRBA fused to green fluorescent protein (GFP), localized predominately in the cytosol of murine macrophages at steady state [38]. However, upon LPS stimulation, LRBA associated with the endoplasmic reticulum (ER), Golgi complex, plasma membrane, and within lysosomes [38]. Furthermore, studies using ImageStream showed localization of LRBA within recycling endosomes and the trans-Golgi network in normal human T cells, suggesting a role of LRBA in vesicle trafficking [7]. In fact, trafficking of transferring receptor (CD71) and CTLA-4 was found reduced in the absence of LRBA despite normal trafficking of CD28, ICOS, PD-1, and CD154-containing vesicles, indicating a role of LRBA in specific trafficking routes [7].
10.9 LRBA Deficiency Mouse Model
Human and murine LRBA share 90% of protein homology indicating an essential role of LRBA during evolution. Similar to humans, LRBA is broadly expressed in murine tissues and it is upregulated two to four folds in immune cells after LPS stimulation [1, 38]. The immune phenotype of LRBA knockout (KO) mice has been recently described [39, 40]. Remarkably, mice lacking LRBA remain healthy after 2-year follow-up under specific pathogenic conditions (SPF) without developing overt disease or increased disease severity after antigenic challenging [39, 40]. Human and murine LRBA deficiencies are similar in terms of a trend towards growth retardation and abnormalities in the regulatory T-cell compartment, including severely diminished CTLA-4 expression and, in less extent, reduction of CD25 and Helios. Frequencies and functionality of Tregs are, however, different. Reduced numbers of Tregs and poor Treg suppression capacity have been observed in LRBA-deficient patients, whereas LRBA KO mice showed comparable numbers to their wild-type littermates [2, 24, 40]. In addition, LRBA KO mice presented normal development and repartition of T-cell subsets in the thymus and spleen, correlating with normal frequencies of CD4+ and CD8+ cells in the blood of LRBA-deficient patients. However, a skewing of peripheral T cells towards a memory phenotype (CD45RO+) is observed in the absence of human or murine LRBA [2, 7]. Memory T cells play a critical role in host defense, but increased numbers are frequently associated with dysregulated Treg functionality, as found in patients with colorectal and gastric cancers [41, 42]. Moreover, an increased frequency of T follicular helper cells that is associated with an ineffective regulation of antibody response has been recently observed in the peripheral blood of LRBA-deficient patients [24], as well as in the Peyer’s patches of LRBA KO mice after acute infection with Salmonella typhimurium despite normal findings on intestinal histological analysis [40].
The findings on NK cells in humans and mice lacking LRBA are controversial. In humans, normal counts of CD16+ CD56+ cells are observed as normal in most LRBA-deficient patients as well as in LRBA KO mice [2, 3, 39, 40]. Using a CD107a translocation assay, the NK cell cytotoxic activity was found regular in LRBA-deficient patients despite LRBA being associated with endosomal trafficking [1]. In contrast, murine LRBA-deficient NK cells impaired granzyme B secretion and activation of NKG2D and NKp46 signaling, suggesting a pivotal role of LRBA in antiviral and antitumoral responses [43]. However, LRBA KO mice mounted normal response against lymphocytic choriomeningitis virus (LCMV) in an acute and chronic infection setting [39, 40], and none of the LRBA patients’ cohorts reported so far showed any predisposition to viral infections and/or to malignancies [2, 3, 5]. In addition, the defective NK cell functionality in LRBA KO mice was associated with resistance to lethal graft-versus-host disease (GvHD), encouraging physicians to treat LRBA-deficient patients with HSCT [43]. However, up to date, 12 patients with LRBA deficiency have been treated with HSCT resulting in 5 complete/good remissions, 3 partial remissions, and 4 deaths [31], confirming the complexity of LRBA deficiency and the need to further analyze the role of LRBA not only in human NK cells but also in other relevant immune actors involved in the GvHD response. This information will help clinicians to decide on the benefits of treating LRBA-deficient patients with HSCT.
The main differences between human and mice lacking LRBA were observed in the B-cell compartment, since total serum IgG and IgM and specific T-dependent and T-independent antibodies and antibody-secreting cells (ASCs) were found to be normal in LRBA KO mice, whereas 60–80% of LRBA-deficient patients suffer from hypogammaglobulinemia and present with poor specific antibody response [2, 40].
Moreover, serum and secretory IgA levels were surprisingly increased in LRBA KO mice regardless of age or treatment of the mice [40]. In addition, and contrary to what has been observed in LRBA-deficient patients, B-cell subsets from LRBA KO mice were found to be normal in terms of frequency and distribution in the bone marrow (pro-, pre-, and immature and mature B cells) and in the spleen (transitional, follicular and marginal zone B cells). Only B-1a cells were severely reduced in the peritoneum of LRBA KO mice in comparison with their WT littermates [40]. B-1 cells secrete spontaneously natural antibodies against either self-antigens or against pathogen-expressed molecules [44]. In addition, peritoneal B-1 cells are considered as the major source of IL-10 production in the B-cell lineage that is implicated in the regulation of tissue homeostasis [45]. Interestingly, IgA-secreting B-1 cells existing in the intestinal lamina propria are derived from peritoneal B-1 cells in an IL-5 and microbiota-dependent manner [46, 47]. This indicates that early exposure to commensal microbiota might be crucial for the development of local IgA-producing B-1 cells and therefore the maintenance of intestinal homeostasis. These observations reveal a possible role of LRBA in the development and/or maintenance of B-1a cells and in the production or regulation of IgA.
10.10 Summary and Outlook
Biallelic loss-of-protein mutations in LRBA cause an early-onset syndrome presenting with immunodeficiency and immune dysregulation, known as LRBA deficiency. Affected patients suffer mostly from autoimmune cytopenias, enteropathy, and lymphoproliferation, resembling the clinical picture of patients with CTLA-4 insufficiency, ALPS, IPEX, and STAT-3 GOF. Although the genetic diagnosis is required for any of the above syndromes, screening diagnostic tests based on the detection of LRBA protein in immune cells after stimulation might be useful to reduce the diagnostic delay, allowing timely clinical interventions. Moreover, a follow-up of bigger LRBA deficiency patients’ cohorts would provide definitive evidence on the efficacy of HSCT and CTLA-4-Ig fusion protein for the treatment of LRBA deficiency.
Although the biological role of LRBA in immunity is not completely understood, autoimmune manifestations are explained by reduced CTLA-4 expression on Tregs and activated Tcon cells as consequence of high CTLA-4 lysosomal degradation in the absence of LRBA. In addition, patients with LRBA deficiency present recurrent infections and hypogammaglobulinemia due to the low numbers of switched memory B cells and plasmablasts due to defective autophagy and increased apoptosis of B cells after encountering an antigen. These findings on T- and B-cell compartments demonstrate an essential role of LRBA in immune tolerance and in the maintenance of humoral immunity. However, the underlying molecular mechanisms involved in the regulation of CTLA-4 as well as in autophagy/apoptosis processes need further evaluation. Contrary to human LRBA deficiency, LRBA KO mice do not present evident signs of disease despite low levels of CTLA-4, reduced frequency of IL-10-producing B cells, and increased numbers of T follicular helper cells. Interestingly, increased levels of IgA were found in mice lacking LRBA. Future studies to elucidate the role of LRBA in the regulation of IgA, and its involvement on mucosal immunity, and on B-1 cell migration are needed. Finally, investigations on clarifying the discrepancies between human and murine LRBA deficiency should be addressed.
References
Lopez-Herrera G, Tampella G, Pan-Hammarstrom Q, Herholz P, Trujillo-Vargas CM, Phadwal K, et al. Deleterious mutations in LRBA are associated with a syndrome of immune deficiency and autoimmunity. Am J Hum Genet. 2012;90(6):986–1001.
Gamez-Diaz L, August D, Stepensky P, Revel-Vilk S, Seidel MG, Noriko M, et al. The extended phenotype of LPS-responsive beige-like anchor protein (LRBA) deficiency. J Allergy Clin Immunol. 2016;137(1):223–30.
Alkhairy OK, Abolhassani H, Rezaei N, Fang M, Andersen KK, Chavoshzadeh Z, et al. Spectrum of phenotypes associated with mutations in LRBA. J Clin Immunol. 2016;36(1):33–45.
Kostel Bal S, Haskologlu S, Serwas NK, Islamoglu C, Aytekin C, Kendirli T, et al. Multiple presentations of LRBA deficiency: a single-center experience. J Clin Immunol. 2017;37:790–800.
Azizi G, Abolhassani H, Mahdaviani SA, Chavoshzadeh Z, Eshghi P, Yazdani R, et al. Clinical, immunologic, molecular analyses and outcomes of iranian patients with LRBA deficiency: a longitudinal study. Pediatr Allergy Immunol. 2017;28(5):478–84.
Serwas NK, Kansu A, Santos-Valente E, Kuloglu Z, Demir A, Yaman A, et al. Atypical manifestation of LRBA deficiency with predominant IBD-like phenotype. Inflamm Bowel Dis. 2015;21(1):40–7.
Lo B, Zhang K, Lu W, Zheng L, Zhang Q, Kanellopoulou C, et al. AUTOIMMUNE DISEASE. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science. 2015;349(6246):436–40.
Levy E, Stolzenberg MC, Bruneau J, Breton S, Neven B, Sauvion S, et al. LRBA deficiency with autoimmunity and early onset chronic erosive polyarthritis. Clin Immunol. 2016;168:88–93.
Bakhtiar S, Ruemmele F, Charbit-Henrion F, Levy E, Rieux-Laucat F, Cerf-Bensussan N, et al. Atypical manifestation of LPS-responsive beige-like anchor deficiency syndrome as an autoimmune endocrine disorder without enteropathy and immunodeficiency. Front Pediatr. 2016;4:98.
Shokri S, Nabavi M, Hirschmugl T, Aghamohammadi A, Arshi S, Bemanian MH, et al. LPS-responsive beige-like anchor gene mutation associated with possible bronchiolitis obliterans organizing pneumonia associated with hypogammaglobulinemia and normal IgM phenotype and low number of B cells. Acta Med Iran. 2016;54(10):620–3.
Schubert D, Bode C, Kenefeck R, Hou TZ, Wing JB, Kennedy A, et al. Autosomal dominant immune dysregulation syndrome in humans with CTLA4 mutations. Nat Med. 2014;20(12):1410–6.
Lo B, Fritz JM, Su HC, Uzel G, Jordan MB, Lenardo MJ. CHAI and LATAIE: new genetic diseases of CTLA-4 checkpoint insufficiency. Blood. 2016;128(8):1037–42.
Schwab C, Gabrysch A, Olbrich P, Patiño V, Warnatz K, Wolff D, Hoshino A, Kobayashi M, Imai K, Takagi M, Dybedal I, Haddock JA, Sansom DM, Lucena JM, Seidl M, Schmitt-Graeff A, Reiser V, Emmerich F, Frede N, Bulashevska A, Salzer U, Schubert D, Hayakawa S, Okada S, Kanariou M, Kucuk ZY, Chapdelaine H, Petruzelkova L, Sumnik Z, Sediva A, Slatter M, Arkwright PD, Cant A, Lorenz HM, Giese T, Lougaris V, Plebani A, Price C, Sullivan KE, Moutschen M, Litzman J, Freiberger T, van de Veerdonk FL, Recher M, Albert MH, Hauck F, Seneviratne S, Pachlopnik Schmid J, Kolios A, Unglik G, Klemann C, Speckmann C, Ehl S, Leichtner A, Blumberg R, Franke A, Snapper S, Zeissig S, Cunningham-Rundles C, Giulino-Roth L, Elemento O, Dückers G, Niehues T, Fronkova E, Kanderová V, Platt CD, Chou J, Chatila TA, Geha R, McDermott E, Bunn S, Kurzai M, Schulz A, Alsina L, Casals F, Deyà-Martinez A, Hambleton S, Kanegane H, Taskén K, Neth O, Grimbacher B. Phenotype, penetrance, and treatment of 133 cytotoxic T-lymphocyte antigen 4-insufficient subjects. J Allergy Clin Immunol. 2018; https://doi.org/10.1016/j.jaci.2018.02.055. [pii: S0091-6749(18)30630-4. Epub ahead of print. PubMed PMID: 29729943; PubMed Central PMCID: PMC6215742].
Tesi B, Priftakis P, Lindgren F, Chiang SC, Kartalis N, Lofstedt A, et al. Successful hematopoietic stem cell transplantation in a patient with LPS-responsive beige-like anchor (LRBA) gene mutation. J Clin Immunol. 2016;36(5):480–9.
Bratanic N, Kovac J, Pohar K, Trebusak Podkrajsek K, Ihan A, Battelino T, et al. Multifocal gastric adenocarcinoma in a patient with LRBA deficiency. Orphanet J Rare Dis. 2017;12(1):131.
Milner JD, Vogel TP, Forbes L, Ma CA, Stray-Pedersen A, Niemela JE, et al. Early-onset lymphoproliferation and autoimmunity caused by germline STAT3 gain-of-function mutations. Blood. 2015;125(4):591–9.
Neven B, Magerus-Chatinet A, Florkin B, Gobert D, Lambotte O, De Somer L, et al. A survey of 90 patients with autoimmune lymphoproliferative syndrome related to TNFRSF6 mutation. Blood. 2011;118(18):4798–807.
Barzaghi F, Passerini L, Bacchetta R. Immune dysregulation, polyendocrinopathy, enteropathy, x-linked syndrome: a paradigm of immunodeficiency with autoimmunity. Front Immunol. 2012;3:211.
Wang JW, Gamsby JJ, Highfill SL, Mora LB, Bloom GC, Yeatman TJ, et al. Deregulated expression of LRBA facilitates cancer cell growth. Oncogene. 2004;23(23):4089–97.
Fujishima N, Hirokawa M, Aiba N, Ichikawa Y, Fujishima M, Komatsuda A, et al. Gene expression profiling of human erythroid progenitors by micro-serial analysis of gene expression. Int J Hematol. 2004;80(3):239–45.
Sansom DM. IMMUNOLOGY. Moving CTLA-4 from the trash to recycling. Science. 2015;349(6246):377–8.
Pengo N, Scolari M, Oliva L, Milan E, Mainoldi F, Raimondi A, et al. Plasma cells require autophagy for sustainable immunoglobulin production. Nat Immunol. 2013;14(3):298–305.
Warnatz K, Wehr C, Drager R, Schmidt S, Eibel H, Schlesier M, et al. Expansion of CD19(hi)CD21(lo/neg) B cells in common variable immunodeficiency (CVID) patients with autoimmune cytopenia. Immunobiology. 2002;206(5):502–13.
Charbonnier LM, Janssen E, Chou J, Ohsumi TK, Keles S, Hsu JT, et al. Regulatory T-cell deficiency and immune dysregulation, polyendocrinopathy, enteropathy, X-linked-like disorder caused by loss-of-function mutations in LRBA. J Allergy Clin Immunol. 2015;135(1):217–27.
Hou TZ, Verma N, Wanders J, Kennedy A, Soskic B, Janman D, et al. Identifying functional defects in patients with immune dysregulation due to LRBA and CTLA-4 mutations. Blood. 2017;129(11):1458–68.
Azizi G, Mirshafiey A, Abolhassani H, Yazdani R, Ghanavatinejad A, Noorbakhsh F, Rezaei N, Aghamohammadi A. The imbalance of circulating T helper subsets and regulatory T cells in patients with LRBA deficiency: correlation with disease severity. J Cell Physiol. 2018;233(11):8767–77. https://doi.org/10.1002/jcp.26772. [Epub 2018 May 28. PubMed PMID: 29806698].
De Bruyne M, Bogaert DJ, Venken K, Van den Bossche L, Bonroy C, Roels L, Tavernier SJ, van de Vijver E, Driessen A, van Gijn M, Gámez-Diaz L, Elewaut D, Grimbacher B, Haerynck F, Moes N, Dullaers M. A novel LPS-responsive beige-like anchor protein (LRBA) mutation presents with normal cytotoxic T lymphocyte-associated protein 4 (CTLA-4) and overactive TH17 immunity. J Allergy Clin Immunol. 2018. pii: S0091-6749(18)31270-3. doi: https://doi.org/10.1016/j.jaci.2018.08.026. [Epub ahead of print. PubMed PMID: 30193839].
Gámez-Díaz L, Sigmund EC, Reiser V, Vach W, Jung S, Grimbacher B. Rapid flow cytometry-based test for the diagnosis of lipopolysaccharide responsive beige-like anchor (LRBA) deficiency. Front Immunol. 2018;9:720. https://doi.org/10.3389/fimmu.2018.00720. [eCollection 2018. PubMed PMID: 29740429; PubMed Central PMCID: PMC5925005].
Azizi G, Abolhassani H, Yazdani R, Mohammadikhajehdehi S, Parvaneh N, Negahdari B, et al. New therapeutic approach by sirolimus for enteropathy treatment in patients with LRBA deficiency. Eur Ann Allergy Clin Immunol. 2017;49(5):235–9.
Seidel MG, Hirschmugl T, Gamez-Diaz L, Schwinger W, Serwas N, Deutschmann A, et al. Long-term remission after allogeneic hematopoietic stem cell transplantation in LPS-responsive beige-like anchor (LRBA) deficiency. J Allergy Clin Immunol. 2015;135(5):1384–90.e1–8.
Seidel MG, Bohm K, Dogu F, Worth A, Thrasher A, Florkin B, et al. Treatment of severe forms of LPS-responsive beige-like anchor protein deficiency with allogeneic hematopoietic stem cell transplantation. J Allergy Clin Immunol. 2018;141:770–775.e1.
Cullinane AR, Schaffer AA, Huizing M. The BEACH is hot: a LYST of emerging roles for BEACH-domain containing proteins in human disease. Traffic. 2013;14(7):749–66.
Smith TF, Gaitatzes C, Saxena K, Neer EJ. The WD repeat: a common architecture for diverse functions. Trends Biochem Sci. 1999;24(5):181–5.
Li D, Roberts R. WD-repeat proteins: structure characteristics, biological function, and their involvement in human diseases. Cell Mol Life Sci. 2001;58(14):2085–97.
Introne W, Boissy RE, Gahl WA. Clinical, molecular, and cell biological aspects of Chediak-Higashi syndrome. Mol Genet Metab. 1999;68(2):283–303.
Nurden A et al. Blood Reviews. 2007.
Kerr WG, Heller M, Herzenberg LA. Analysis of lipopolysaccharide-response genes in B-lineage cells demonstrates that they can have differentiation stage-restricted expression and contain SH2 domains. Proc Natl Acad Sci U S A. 1996;93(9):3947–52.
Wang JW, Howson J, Haller E, Kerr WG. Identification of a novel lipopolysaccharide-inducible gene with key features of both A kinase anchor proteins and chs1/beige proteins. J Immunol. 2001;166(7):4586–95.
Burnett DL, Parish IA, Masle-Farquhar E, Brink R, Goodnow CC. Murine LRBA deficiency causes CTLA-4 deficiency in Tregs without progression to immune dysregulation. Immunol Cell Biol. 2017;95(9):775–88.
Gamez-Diaz L, Neumann J, Jager F, Proietti M, Felber F, Soulas-Sprauel P, et al. Immunological phenotype of the murine Lrba knockout. Immunol Cell Biol. 2017;95:789–802.
Perrone G, Ruffini PA, Catalano V, Spino C, Santini D, Muretto P, et al. Intratumoural FOXP3-positive regulatory T cells are associated with adverse prognosis in radically resected gastric cancer. Eur J Cancer. 2008;44(13):1875–82.
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pages C, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313(5795):1960–4.
Park MY, Sudan R, Srivastava N, Neelam S, Youngs C, Wang JW, et al. LRBA is essential for allogeneic responses in bone marrow transplantation. Sci Rep. 2016;6:36568.
Martin F, Oliver AM, Kearney JF. Marginal zone and B1 B cells unite in the early response against T-independent blood-borne particulate antigens. Immunity. 2001;14(5):617–29.
Baumgarth N. The double life of a B-1 cell: self-reactivity selects for protective effector functions. Nat Rev Immunol. 2011;11(1):34–46.
Beagley KW, Murray AM, McGhee JR, Eldridge JH. Peritoneal cavity CD5 (Bla) B cells: cytokine induced IgA secretion and homing to intestinal lamina propria in SCID mice. Immunol Cell Biol. 1995;73(5):425–32.
Kroese FG, Ammerlaan WA, Kantor AB. Evidence that intestinal IgA plasma cells in mu, kappa transgenic mice are derived from B-1 (Ly-1 B) cells. Int Immunol. 1993;5(10):1317–27.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gámez-Díaz, L. (2019). LRBA Deficiency. In: D'Elios, M., Rizzi, M. (eds) Humoral Primary Immunodeficiencies. Rare Diseases of the Immune System. Springer, Cham. https://doi.org/10.1007/978-3-319-91785-6_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-91785-6_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-91784-9
Online ISBN: 978-3-319-91785-6
eBook Packages: MedicineMedicine (R0)