Abstract
The establishment of imatinib as the standard therapy for CML marked the beginning of a new era of treatment. Due to occurring intolerance and resistance against the drug, the development of new inhibitors was promoted. This led to the second-generation inhibitors dasatinib, nilotinib, and bosutinib. Despite all achieved improvements, first- and second-generation inhibitors are ineffective against the BCR-ABL T315I “gatekeeper” mutation. In order to overcome this issue and to further improve the inhibitory effect, the third-generation inhibitor ponatinib was developed. Various clinical trials have been launched to study the effect of ponatinib in the clinical setting. Based on positive phase 1 and phase 2 trials, ponatinib was approved for the second-line treatment of CML and Ph+ ALL in December 2012 in the USA and in July 2013 in the European Union. The safety data of these trials particularly revealed a dose-dependent, increased risk for serious arterial occlusive events under treatment with ponatinib. Further trials investigate optimized dosing schemes to reduce side effects while maintaining clinical activity in CML and evaluate potential activity of the drug in other malignancies. In conclusion, ponatinib has proved to be a powerful BCR-ABL inhibitor, which exhibits clinical activity both in BCR-ABL wild-type and mutant CML, including the pan-resistant T315I mutation. Ponatinib should be used catiously with respect to increased cardiovascular risk. Despite previous TKI failure, chronic-phase CML patients can achieve sustained remissions using this drug, offering an important addition to therapeutic options in the treatment for CML.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Resistance to Treatment in CML
The establishment of imatinib as the standard therapy for CML in 2001 (Druker et al. 2001) fundamentally changed the clinical course of this disease. For many patients, CML became a chronic disorder and patients experiencing major molecular response (MMR) might not face a loss in life expectancy (Jain et al. 2013). However, this favorable prognosis is not true for all patients. Around 20–30% of patients treated with imatinib do not respond adequately to treatment (primary resistance) or relapse after initial response to imatinib (secondary resistance) (Druker et al. 2006; de Lavallade et al. 2008).
Resistance against imatinib or newer Abl inhibitors is caused by various mechanisms that can occur in combination, especially in advanced stages of disease (von Bubnoff et al. 2005; Lahaye et al. 2005; Nicolini et al. 2007). Patient-related causes for primary as well as secondary resistance are mainly non-compliance with the treatment regime (Darkow et al. 2007). However, inadequate serum levels can arise despite proper compliance from individual differences in the activity of imatinib-metabolizing enzymes such as CYP3A4. In addition, these enzymes can be induced by co-medication and nutritional habits (Floyd et al. 2003).
At the cellular level, the ability of the malignant clone to transport drug out of the cell or to hinder drug influx can result in drug resistance. For example, the proteins ABCB1 and MDR-1 are considered responsible for the increased efflux of imatinib from CML cells (Kuwazuru et al. 1990; Mahon et al. 2003; Thomas et al. 2004).
Just as the BCR-ABL fusion protein represents the causative event for CML, it is also the main reason for the development of resistance (Shah and Sawyers 2003). Mutations of this fusion gene result in changes in critical amino acids, such that inhibitors become ineffective (von Bubnoff et al. 2002; Branford et al. 2003). More than 90 different mutations of BCR-ABL in CML have been described in recent years (Soverini et al. 2011). However, the majority of observed mutations occur at specific positions. One study found 14 mutations in 95% of cases (Zhou et al. 2011), while another analysis described 20 mutations in 88% of cases (Branford et al. 2009). Hence, these common mutations are clinically most relevant and have directed the development of second- and third-generation inhibitors.
2 Second-Generation Inhibitors
After the approval of imatinib in 2002, second-generation BCR-ABL kinase inhibitors were developed. The need for these novel inhibitors became evident both from patients presenting with primary imatinib intolerance, or developing intolerance during treatment, and from primary or secondary imatinib resistance, many of them being the consequence of secondary mutations in BCR-ABL, which confer imatinib resistance.
Based on the positive results of phase 2 trials, the second-generation inhibitors dasatinib and nilotinib were approved as second-line therapy in imatinib-resistant or imatinib-intolerant CML and Ph+ ALL (Kantarjian et al. 2007; Talpaz et al. 2006). In March 2013, bosutinib was also approved for second-line treatment. Recently, phase 3 trials (DAISION for dasatinib; ENESTnd for nilotinib) reported earlier and deeper remissions compared to imatinib in newly diagnosed, chronic-phase CML patients, as well as lower rates of progression to accelerated phase or blast crisis along with good tolerability of the drugs (Kantarjian et al. 2010, 2011; Saglio et al. 2010). These trials consequently led to the approval of both second-generation inhibitors, dasatinib and nilotinib, for the first-line treatment of CML. Although all second-generation inhibitors proved to be effective against a variety of known secondary BCR-ABL mutations, each of these inhibitors still faces a distinct spectrum of vulnerable mutations (Zhou et al. 2011; Branford et al. 2009; Bradeen et al. 2006; von Bubnoff et al. 2006) (Table 1).
Most notably, despite their differences, all first- and second-generation inhibitors are ineffective against the BCR-ABL T315I mutation. The exchange of threonine at position 315 for the more bulky isoleucine leads to a steric hindrance, inhibiting binding of all these inhibitors. Unable to bind the kinase, most Abl inhibitors lose their ability to block BCR-ABL kinase activity. Twenty percent of patients who are imatinib-resistant because of a BCR-ABL mutation harbor the T315I “gatekeeper” mutation (O’Hare et al. 2007).
3 Ponatinib: A Third-Generation Inhibitor
The small molecule ponatinib was developed specifically to overcome resistance based on the T315I mutation. The integration of a linear carbon–carbon triple bond into the structure of the molecule to link two functional groups avoids the blocking effect of the isoleucine in the context of the T315I mutation (Fig. 1). Furthermore, sites for interaction between the inhibitor and the kinase were optimized and are distributed over a wide range of protein residues. This increases the affinity and thereby reduces the required serum drug level. In addition, increased binding affinity ensures effectiveness of the inhibitor, even in those cases where one of the drug-binding site is lost, due to a mutation (Zhou et al. 2011).
Initial preclinical studies of ponatinib—formerly referred to as AP24534—revealed the activity of the drug as a pan-BCR-ABL inhibitor in biochemical assays, in cell lines as well as in mouse models. In contrast to the previously approved first- and second-generation inhibitors, the activity profile of the new inhibitor included the T315I mutation. In addition, so-called compound mutants, defined by the co-occurrence of several concurrent mutations within the BCR-ABL fusion protein, were inhibited at a higher concentration by ponatinib (O’Hare et al. 2009).
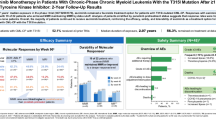
In 2012, the first phase 1 trial for ponatinib in previously therapy-refractory patients was published (Cortes et al. 2012). This study included 60 CML and 5 Ph+ ALL patients. The CML cases included 43 patients in chronic phase (CP), 9 in accelerated phase (AP), and 8 in blast phase (BP) and represented a highly pretreated collective (59/60 ≥ 2 TKIs; 41/60 ≥ 3 TKIs). Ponatinib was given once daily at doses ranging from 2 to 60 mg. Among the CP-CML patients, 98% achieved a complete hematologic remission (CHR), 72% achieved a major cytogenetic response (MCyR), and 44% achieved a major molecular response (MMR). Given the refractory nature of CML in these patients and the high degree of pretreatment, these numbers were quite remarkable.
It should be highlighted that 12 of the 43 CP patients (28%) carried the T315I mutation and therefore were refractory to first- or second-generation inhibitors. Under ponatinib therapy, 100% of these T315I patients achieved a major hematologic response (MHR), 92% achieved a MCyR, and 67% achieved a MMR. Of the 13 refractory CML cases, which lacked any BCR-ABL mutation, rates for CHR, MCyR, and MMR of 100, 62, and 15%, respectively, were observed. Patients with advanced CML (AP, BP) were analyzed together with the Ph+ ALL cohort in this study and responded to ponatinib as well. A MHR was achieved in 36%, MCyR in 32%, and MMR in 9% of patients. Thus, the novel third-generation inhibitor showed a clinically significant effect even in advanced-phase CML.
In order to further investigate the primary response rates to ponatinib (45 mg once daily) and its safety, a phase 2 trial (PACE trial) was launched. In total 449 patients in all phases of CML (CP, AP, and BP) and Ph+ ALL, resistant or intolerant to dasatinib or nilotinib or with a known T315I mutation, were enrolled. In CP-CML patients (n = 267), the primary endpoint (MCyR at 12 months) was achieved in 56% of cases. In particular, patients carrying a T315I mutation responded better than those who were included because of resistance or intolerance (70% vs. 51%). In the CP-CML cohort, progression-free survival (PFS) and overall survival (OS) after twelve months were 80 and 94%, respectively. Furthermore, the study revealed that the response rates for MCyR, CCyR, and MMR of those patients decreased depending on the number of previously applied TKIs (Cortes et al. 2013). The primary endpoint (MHR after 12 months) was achieved in 55% of the AP CML and in 31% of the group containing BP CML and Ph+. Altogether, the results of the PACE trial confirm the efficacy of ponatinib in second-generation TKI-resistant or TKI-intolerant CML and Ph+ ALL patients at a dose of 45 mg daily. Importantly, the results confirm the efficacy of this new inhibitor against the “gatekeeper” T315I mutation. As the final data collection was scheduled for the end of 2017, an update of those results is expected in the near future.
Based on the two above-mentioned trials, ponatinib was approved for the second-line treatment of CML and Ph+ ALL in December 2012 in the USA and in July 2013 in the European Union. The approval in the EU covers patients in all phases of CML.
-
Who are resistant to dasatinib or nilotinib.
-
Who are intolerant to dasatinib or nilotinib and for whom subsequent treatment with imatinib is not clinically appropriate.
-
Who carry the T315I mutation.
The same terms apply to the approval for the use in Ph+ ALL except that nilotinib is not considered here.
A phase 3 trial (EPIC trial) opened in July 2012 strived to compare ponatinib (45 mg daily) with imatinib (400 mg daily) in first-line therapy of newly diagnosed CML in CP. This trial aimed to enroll 528 patients, but was terminated due to safety concerns in October 2013 after the inclusion of 307 patients. This decision was based on the safety results of the aforementioned trails, showing an increased concurrency of serious arterial occlusive events. Due to the premature termination of the trail, the interpretation of the trial results is limited. Based on the preliminary data, patients treated with ponatinib in first line seem to achieve an MMR earlier and in a higher proportion of patients. The analysis of the adverse events showed increased frequency of arterial occlusive events.
In the PACE and EPIC trial, the following non-hematologic adverse reactions were reported in descending order of frequency (any grade, PACE/EPIC): rash (34%/31%), dry skin (32%/17%), abdominal pain (22%/27%), headaches (19%/32%), increased lipase (18%/32%), fatigue (17%/20%), constipation (16%/27%), myalgia (16%/25%), nausea (16%/21%), arthralgia (13%/18%), increased alanine aminotransferase (10%/18%), pancreatitis (6%/n.a.), and hypertension (7%/13%). Hematologic adverse effects have been observed more frequently compared to other Abl kinase inhibitors (thrombocytopenia > neutropenia > anemia). Focusing on the serious adverse events of grades 3 and 4, the increase in lipase (10%/12% of CP-CML patients) and hematologic adverse effects (thrombocytopenia 41%/6%, neutropenia 16%/3%, anemia 10%/n.a.) should receive special attention (Cortes et al. 2013; Lipton et al. 2016). Furthermore, the occurrence of arterial thrombotic events in the PACE trial (5.1% cardiovascular serious adverse events, 2.4% cerebrovascular serious adverse events, and 2.0% peripheral vascular serious adverse events) has to be highlighted (Cortes et al. 2013).
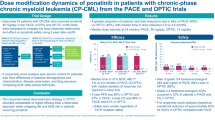
In order to improve the safety information about ponatinib with particular focus on the arterial thrombotic events, the available data of patients treated with ponatinib in the respective clinical trials (phase 1 trial, 81 patients; phase 2 PACE trial, 449 patients; phase 3 EPIC trial 153 patients) were recently analyzed retrospectively. A total of 671 patients were included in the multivariate analysis. The strongest independent predictors for the arterial thrombotic events were history of ischemic disease, dose intensity of ponatinib, and age. According to this analysis, a 15-mg/d decrease in ponatinib dose intensity results in a 33% reduction in the risk of an arterial occlusive event (Dorer et al. 2016). In the PACE phase 2 trial, 68% of the patients required dose reductions to 30 or 15 mg once daily during the course of therapy. The follow-up of these patients showed that the efficacy was retained at lower doses in most cases (Cortes et al. 2015). Along with this information, the current prescribing information recommends to consider dose reduction to 30 or 15 mg in patients achieving major cytogenetic response after patient’s individual risk assessment taking into account cardiovascular risk factors, individual tolerability, time to cytogenetic response, and molecular response (status: 11/2016 FDA; 09/2017 EMA).
Based on the experience regarding the improved response rates achieved by ponatinib as well as the dose-related risk for adverse events (pancreatitis, arterial occlusive events, rash), further studies were initiated.
First, a phase 2 trial (OPTIC trial/NCT02467270) assays the activity and risk of three different starting doses of ponatinib (45/30/15 mg) in CP-CML patients who received at least two different TKI before. To address the safety concerns especially in higher doses of ponatinib, the drug will be reduced to 15 mg daily upon an achievement of MCyR. This trial aims to enroll 450 patients.
Second, a phase 3 trial (OPTIC-2L trial/NCT02627677) compares two doses of ponatinib (30 mg/15 mg once daily) and nilotinib 400 mg twice daily in CP-CML following resistance to imatinib. Again, a dose reduction of ponatinib (30–15 mg; 15–10 mg) is implemented in the study protocol after reaching MMR. A total of 600 patients will be included and randomized according to a 1:2:1 scheme.
Furthermore, a single-armed phase 2 trial (OPUS trial/NCT02398825) examines the activity and risk profile of 30 mg ponatinib, which will as well be adjusted to 15 mg daily once an MMR has been achieved.
In addition to the use of ponatinib in CML and Ph+ ALL, other diseases could potentially benefit from the treatment with this drug as well. Preclinical studies reported that ponatinib inhibits not only BCR-ABL but also RET, FLT3, KIT, SRC, as well as members of receptor kinase families VEGFR, FGFR, and PDGFR (O’Hare et al. 2009). Following these findings, in vitro as well as in vivo studies / mouse xenograft models investigated the effect of ponatinib in AML as well as breast cancer cell lines and carcinoma of the endometrium, bladder, stomach, colon, lung, and medullary thyroid. In these neoplasms, ponatinib was shown to inhibit proliferation and additionally to induce apoptosis in FLT3-ITD-driven AML. The activity of ponatinib in these preclinical studies constitutes the rational to examine ponatinib in a variety of additional cancer entities (Falco et al. 2013; Gozgit et al. 2011, 2012; Zirm et al. 2012). Respective clinical trials on FLT3-ITD positive AML, non-small cell lung cancer (NSCLC), glioblastoma, thyroid cancer, and others are currently evaluating the significance of ponatinib in those disease entities.
In conclusion, ponatinib constitutes a powerful BCR-ABL inhibitor and has been approved for the treatment of CML patients resistant or intolerant to imatinib, dasatinib, or nilotinib. It displays clinical activity both in wild-type and in BCR-ABL mutant CML, including activity against the T315I mutation. Ponatinib induces high rates of remission. On the other hand, it causes an increased risk for serious adverse events, especially arterial thrombotic events. Current clinical trials investigate optimized dosing schemes in order to reduce the occurrence of these adverse events while maintaining its clinical activity. Despite previous TKI failure, chronic-phase CML patients can achieve sustained remissions using the novel drug. For patients with advanced CML or Ph+ ALL, ponatinib therapy can successfully bridge the time to allogeneic stem cell transplantation.
References
Bradeen HA et al (2006) Comparison of imatinib mesylate, dasatinib (BMS-354825), and nilotinib (AMN107) in an N-ethyl-N-nitrosourea (ENU)-based mutagenesis screen: high efficacy of drug combinations. Blood 108(7):2332–2338
Branford S, Rudzki Z, Walsh S, Parkinson I, Grigg A, Szer J et al (2003) Detection of BCR-ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood 102(1):276–283
Branford S, Melo JV, Hughes TP (2009) Selecting optimal second-line tyrosine kinase inhibitor therapy for chronic myeloid leukemia patients after imatinib failure: does the BCR-ABL mutation status really matter? Blood 114(27):5426–5435
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I et al (2012) Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med 367(22):2075–2088
Cortes JE et al (2013) A phase 2 trial of ponatinib in Philadelphia chromosome–positive leukemias. N Engl J Med 369:1783–1796
Cortes J, Kim DW, Pinilla-Ibarz J, le Coutre PD, Paquette R, Chuah C et al (2015) Ponatinib efficacy and safety in heavily pretreated leukemia patients: 3-year results of the PACE trial [abstract P234]. Haematologica 100:64
Darkow T, Henk HJ, Thomas SK, Feng W, Baladi J-F, Goldberg GA et al (2007) Treatment interruptions and non-adherence with imatinib and associated healthcare costs: a retrospective analysis among managed care patients with chronic myelogenous leukaemia. Pharmacoeconomics 25(6):481–496
de Lavallade H, Apperley JF, Khorashad JS, Milojkovic D, Reid AG, Bua M et al (2008) Imatinib for newly diagnosed patients with chronic myeloid leukemia: incidence of sustained responses in an intention-to-treat analysis. J Clin Oncol 26(20):3358–3363
Dorer DJ, Knickerbocker RK, Baccarani M, Cortes JE, Hochhaus A, Talpaz M, Haluska FG (2016) Impact of dose intensity of ponatinib on selected adverse events: multivariate analyses from a pooled population of clinical trial patients. Leuk Res 48:84–91
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM et al (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 344(14):1031–1037
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N et al (2006) Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 355(23):2408–2417
Falco VD, Buonocore P, Muthu M, Torregrossa L, Basolo F, Billaud M et al (2013) Ponatinib (AP24534) is a novel potent inhibitor of oncogenic RET mutants associated with thyroid cancer. J Clin Endocrinol Metab (Internet). 22 Mar 2013 (cited 29 Apr 2013). Available from http://jcem.endojournals.org/content/early/2013/03/21/jc.2012-2672
Floyd MD, Gervasini G, Masica AL, Mayo G, George AL Jr, Bhat K et al (2003) Genotype-phenotype associations for common CYP3A4 and CYP3A5 variants in the basal and induced metabolism of midazolam in European- and African-American men and women. Pharmacogenetics 13(10):595–606
Gozgit JM, Wong MJ, Wardwell S, Tyner JW, Loriaux MM, Mohemmad QK et al (2011) Potent activity of ponatinib (AP24534) in models of FLT3-driven acute myeloid leukemia and other hematologic malignancies. Mol Cancer Ther 10(6):1028–1035
Gozgit JM, Wong MJ, Moran L, Wardwell S, Mohemmad QK, Narasimhan NI et al (2012) Ponatinib (AP24534), a multitargeted Pan-FGFR inhibitor with activity in multiple FGFR-amplified or mutated cancer models. Mol Cancer Ther 11(3):690–699
Jain P, Kantarjian H, Cortes J (2013) Chronic myeloid leukemia: overview of new agents and comparative analysis. Curr Treat Options Oncol 14(2):127–143
Kantarjian HM, Giles F, Gattermann N, Bhalla K, Alimena G, Palandri F et al (2007) Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome–positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood 110(10):3540–3546
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M et al (2010) Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 362(24):2260–2270
Kantarjian HM, Hochhaus A, Saglio G, De Souza C, Flinn IW, Stenke L et al (2011) Nilotinib versus imatinib for the treatment of patients with newly diagnosed chronic phase, Philadelphia chromosome-positive, chronic myeloid leukaemia: 24-month minimum follow-up of the phase 3 randomised ENESTnd trial. Lancet Oncol 12(9):841–851
Kuwazuru Y, Yoshimura A, Hanada S, Ichikawa M, Saito T, Uozumi K et al (1990) Expression of the multidrug transporter, P-glycoprotein, in chronic myelogenous leukaemia cells in blast crisis. Br J Haematol 74(1):24–29
Lahaye T, Riehm B, Berger U, Paschka P, Müller MC, Kreil S et al (2005) Response and resistance in 300 patients with BCR-ABL–positive leukemias treated with imatinib in a single center. Cancer 103(8):1659–1669
Lipton JH, Chuah C, Guerci-Bresler A, Rosti G, Simpson D, Assouline S et al (2016) Ponatinib versus imatinib for newly diagnosed chronic myeloid leukaemia: an international, randomised, open-label, phase 3 trial. Lancet Oncol 17(5):612–21
Mahon F-X, Belloc F, Lagarde V, Chollet C, Moreau-Gaudry F, Reiffers J et al (2003) MDR1 gene overexpression confers resistance to imatinib mesylate in leukemia cell line models. Blood 101(6):2368–2373
Nicolini FE, Chabane K, Tigaud I, Michallet M, Magaud J-P, Hayette S (2007) BCR-ABL mutant kinetics in CML patients treated with dasatinib. Leuk Res 31(6):865–868
O’Hare T, Eide CA, Deininger MWN (2007) Bcr-Abl kinase domain mutations, drug resistance, and the road to a cure for chronic myeloid leukemia. Blood 110(7):2242–2249
O’Hare T, Shakespeare WC, Zhu X, Eide CA, Rivera VM, Wang F et al (2009) AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell 16(5):401–412
Redaelli S, Mologni L, Rostagno R, Piazza R, Magistroni V, Ceccon M et al (2012) Three novel patient-derived BCR-ABL mutants show different sensitivity to second and third generation tyrosine kinase inhibitors. Am J Hematol 87(11):E125–E128
Saglio G, Kim D-W, Issaragrisil S, le Coutre P, Etienne G, Lobo C et al (2010) Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med 362(24):2251–2259
Shah NP, Sawyers CL (2003) Mechanisms of resistance to STI571 in Philadelphia chromosome-associated leukemias. Oncogene 22(47):7389–7395
Soverini S, Hochhaus A, Nicolini FE, Gruber F, Lange T, Saglio G et al (2011) BCR-ABL kinase domain mutation analysis in chronic myeloid leukemia patients treated with tyrosine kinase inhibitors: recommendations from an expert panel on behalf of European LeukemiaNet. Blood 118(5):1208–1215
Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoll J, Paquette R et al (2006) Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 354(24):2531–2541
Thomas J, Wang L, Clark RE, Pirmohamed M (2004) Active transport of imatinib into and out of cells: implications for drug resistance. Blood 104(12):3739–3745
von Bubnoff N et al (2002) BCR-ABL gene mutations in relation to clinical resistance of Philadelphia-chromosome-positive leukaemia to STI571: a prospective study. Lancet 359(9305):487–491
von Bubnoff N, Veach DR, van der Kuip H, Aulitzky WE, Sänger J, Seipel P et al (2005) A cell-based screen for resistance of Bcr-Abl-positive leukemia identifies the mutation pattern for PD166326, an alternative Abl kinase inhibitor. Blood 105(4):1652–1659
von Bubnoff N et al (2006) Bcr-Abl resistance screening predicts a limited spectrum of point mutations to be associated with clinical resistance to the Abl kinase inhibitor nilotinib (AMN107). Blood 108(4):1328–1333
Zhou T, Commodore L, Huang W-S, Wang Y, Thomas M, Keats J et al (2011) Structural mechanism of the pan-BCR-ABL inhibitor ponatinib (AP24534): lessons for overcoming kinase inhibitor resistance. Chem Biol Drug Des 77(1):1–11
Zirm E, Spies-Weisshart B, Heidel F, Schnetzke U, Böhmer F-D, Hochhaus A et al (2012) Ponatinib may overcome resistance of FLT3-ITD harbouring additional point mutations, notably the previously refractory F691I mutation. Br J Haematol 157(4):483–492
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Wehrle, J., von Bubnoff, N. (2018). Ponatinib: A Third-Generation Inhibitor for the Treatment of CML. In: Martens, U. (eds) Small Molecules in Hematology. Recent Results in Cancer Research, vol 212. Springer, Cham. https://doi.org/10.1007/978-3-319-91439-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-91439-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-91438-1
Online ISBN: 978-3-319-91439-8
eBook Packages: MedicineMedicine (R0)