Abstract
The patient is a 44-year-old African-American female who presented with severe, lancinating occipital pain. Her medical history was notable for a motor vehicle collision resulting in a whiplash injury and a Chiari malformation for which she underwent decompression surgery. The pain was predominantly right-sided and described as constant, stabbing, and sharp and made worse with palpation and neck movement. The patient was neurologically intact on physical examination, although had a positive Tinel’s sign with exquisite tenderness to palpation over the greater occipital nerve on the right side predominantly, as well as the left side to some degree. She achieved notable but transient pain relief with selective occipital nerve blocks and transcutaneous electrical nerve stimulation. Anticonvulsant medications resulted in pain relief initially, but were less effective over time.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Occipital neuralgia
- Occipital nerve stimulation
- Greater occipital nerve
- Cervicogenic headache
- Neuromodulation
- Refractory
Representative Case History
The patient is a 44-year-old African-American female who presented with severe, lancinating occipital pain. Her medical history was notable for a motor vehicle collision resulting in a whiplash injury and a Chiari malformation for which she underwent decompression surgery. The pain was predominantly right-sided and described as constant, stabbing, and sharp and made worse with palpation and neck movement. The patient was neurologically intact on physical examination, although had a positive Tinel’s sign with exquisite tenderness to palpation over the greater occipital nerve on the right side predominantly, as well as the left side to some degree. She achieved notable but transient pain relief with selective occipital nerve blocks and transcutaneous electrical nerve stimulation. Anticonvulsant medications resulted in pain relief initially, but were less effective over time.
Overview
Occipital neuralgia (ON) is a pain disorder described by the International Headache Society as sharp, shooting, or stabbing pain which manifests along the distribution of the greater (GON) , lesser (LON) , or third occipital nerves [1]. It can be unilateral or bilateral and presents with recurring paroxysmal episodes lasting for a few seconds to a minute. The pain is often elicited with palpation of the affected nerve branches or even with certain movements of the head and neck. It may also be associated with dysesthesias or allodynia. Frequently, nerve blocks will be done and produce temporary relief of symptoms, but lack of efficacy of the block does not necessarily exclude ON as a diagnosis [2, 3].
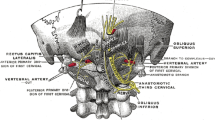
Knowledge of the anatomy of the occipital nerves is essential to understanding the diagnosis and treatment of ON. The dorsal ramus of C2 emerges between the atlas and axis and curves inferiorly and obliquely before giving off a medial branch, the GON [4]. The GON then pierces the semispinalis capitis and trapezius to supply the occipital skin toward the scalp vertex and is often accompanied by the occipital artery. The LON similarly arises from the C2 dorsal ramus, with an occasional contribution from the C3 dorsal ramus, and ascends the posterior border of the sternocleidomastoid before piercing the posterior triangle of the neck to innervate the mastoid region [4, 5]. The third occipital nerve arises from the superficial medial branch of the C3 dorsal ramus and innervates the suboccipital region [6]. A variable pain distribution in ON may be explained by the convergence between cervical and trigeminal afferents in the pars caudalis of the spinal trigeminal nucleus [4].
There are a variety of potential etiologies of ON, although most presentations are idiopathic [5]. However, ON can occur as a result of trauma or compression of the occipital nerves or upper cervical dorsal root ganglion. Thus, a thorough history and physical exam are important, as are radiographic imaging such as flexion/extension x-rays or occasionally a cervical MRI. ON may also arise from a neoplastic process. In addition, pain in the posterior scalp can be associated with a number of headache and non-headache disorders, although ON tends to be distinguished by the localized tenderness in the distribution of the occipital nerves.
Initial treatment measures are conservative and include alternating warm or cold compresses and physical therapy or massage to alleviate muscle tension [7]. Medications such as antiepileptics and antidepressants may decrease the frequency and severity of ON pain when taken regularly, and anti-inflammatories may alleviate pain during acute episodes [7]. Local anesthetic blocks and steroid injections can be both diagnostic and therapeutic, although the benefit is usually transient. Pulsed radiofrequency has gained popularity as an effective nondestructive treatment, but these effects are also short-lived [8]. There are numerous surgical treatment options for ON, including occipital neurectomy, C2 ganglionectomy, and rhizotomy, although these procedures tend to be invasive and destructive and confer variable benefit [9]. As such, occipital nerve stimulation (ONS) has emerged as an additional treatment modality for patients with medically refractory ON and has been demonstrated to provide excellent and sustained pain relief with low complication rates [10, 11]. ONS is also a reversible and adjustable treatment that does not produce numbness, unlike the lesioning procedures described above.
Differential Diagnosis
-
Tension headache
-
Cluster headache
-
Migraine headache
-
Hemicrania continua
-
Cervicogenic headache
-
Myofascial pain
-
Chiari malformation
-
C1–C2 degenerative arthritis
-
Neoplasm involving the posterior fossa or C2 nerve root
-
Systemic vasculitis or inflammatory lesions of the C2 nerve root or greater occipital nerve
-
Giant cell arteritis involving the occipital arteries
-
Postherpetic neuralgia involving the C2 nerve root or greater occipital nerve
-
Metabolic disorders including diabetes
-
Infection
Diagnostic Workup
The clinical history is important to distinguish ON from other headache disorders, primarily based on the distribution and characteristics of pain. Pain from true ON tends to be sharp and stabbing with paroxysmal attacks. It can be elicited with palpation of the neck and/or occiput and triggered with neck movements. In contrast, dull, aching, and throbbing pain that is more diffuse and harder to localize to the occipital nerves is less likely to be ON. Patients may report avoiding washing or brushing their hair, or wearing hats. Although the majority of ON cases are idiopathic, it is important to ask about prior head or neck trauma, neck surgery, or other systemic disorders.
A physical exam should demonstrate pain on palpation of the occipital region. There may also be allodynia with stimulation of other regions of the scalp or hair. A positive Tinel’s sign is frequently elicited over the affected nerve that reproduces the patient’s pain. The neck and occipital region should be examined for irregularities or scars from previous head or neck trauma or surgery.
An initial diagnostic workup includes head and neck imaging (MRI or CT) to rule out a structural cause for the patient’s symptoms, such as a tumor, degenerative cervical spine disease, or a Chiari malformation, as well as flexion/extension cervical X-rays to rule out instability. Additional testing may include blood work for systemic inflammatory or metabolic processes, if the clinical history is suggestive of these etiologies. Local anesthetic block of the GON and/or LON is both diagnostic and therapeutic. However, it is important to recognize that other headache types may also respond to occipital nerve blocks [12].
Case Management
The patient had a history of a whiplash injury and Chiari decompression prior to the onset of her symptoms, which may complicate the diagnosis of ON as these pathologies can present with neck pain and posterior headaches. However, the characteristics of her occipital pain and physical exam findings were most consistent with a diagnosis of ON. Conservative management was first attempted with medications, including gabapentin (800 mg TID) and amitriptyline (25 mg daily). Topiramate was tried but was ineffective. Local anesthetic blocks and transcutaneous electrical nerve stimulation resulted in significant but transient benefit. A decision was then made to proceed with an occipital nerve stimulation trial.
After a pain psychology evaluation confirmed the patient’s candidacy for surgical intervention, a trial stimulator lead was placed. The patient was positioned supine with a shoulder bump, under MAC and local anesthesia, and an 8-contract trial percutaneous spinal cord stimulator electrode was inserted from a stab incision in the right posterior auricular region, extending across the occiput bilaterally at the level of the posterior arch of C1, as confirmed with intraoperative fluoroscopy. The lead position also corresponded with the location of the patient’s positive Tinel’s sign, which was marked preoperatively. The patient was awoken during the trial procedure and tested to confirm adequate coverage of her pain. The trial leads were externalized and secured, and she was sent home with multiple stimulation program options for 7 days. Trial stimulation resulted in greater than 50% pain relief (Fig. 39.1).
One month later, the patient underwent permanent ONS lead implantation, performed in the same manner described above. Again, an 8-contact percutaneous spinal cord stimulator electrode was inserted through a small incision in the right posterior auricular region of the scalp. The lead was secured with an anchor, which was sutured to the fascia, and a strain relief loop was placed. The lead was then tunneled to the right infraclavicular region and connected to a rechargeable, implantable pulse generator. Impedances were checked, the generator was secured to the fascia, and the wounds were irrigated and closed in sequential layers. Postoperative x-rays confirmed good positioning of the lead (Fig. 39.2).
The patient maintained the same benefit from her permanent stimulator as from the trial and was able to be more active in her daily life. In follow-up, she has described significant and near-complete resolution of her pain, without requiring oral pain medications.
Alternative Management Options
-
Conservative therapy with anticonvulsants and antidepressants was first tried and failed, despite adjustments in medication types and dosages. Further medical therapy alone would likely be ineffective.
-
Occipital neurectomy of the greater and/or lesser occipital nerves could be attempted, although would be difficult due to the previous scar tissue from the Chiari decompression. These procedures also have a high rate of pain recurrence, and the proximal nerve stump may develop a painful neuroma.
-
C2 ganglionectomy avoids the issues of nerve regeneration and neuroma formation that occur with neurectomy and would result in complete sensory loss in the C2 distribution. This procedure is more invasive and technically complicated and may result in a painful deafferentation syndrome.
-
Rhizotomy could be attempted as a last resort, although it is more invasive and technically complicated than all other therapeutic measures. Selective dorsal rhizotomies are usually attempted to minimize sensory loss.
Key Points
-
Occipital neuralgia is characterized by severe, paroxysmal, sharp, and stabbing pain in the distribution of the greater, lesser, and/or third occipital nerves.
-
Diagnosis is confirmed by occipital tenderness and a positive Tinel’s sign along the occipital nerve and is relieved with local anesthetic blocks.
-
First-line treatment consists of medical management with antiepileptic and/or antidepressant medications.
-
Medically refractory occipital neuralgia is best managed with occipital nerve stimulation, a procedure that is relatively easy to perform, is associated with low surgical risk, and confers excellent and lasting clinical benefit.
-
Surgical lesioning procedures may be considered as alternative therapies but are much more invasive and technically challenging. They tend to produce permanent numbness but can also result in painful deafferentation syndromes.
References
The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33:629–808. https://doi.org/10.1177/0333102413485658.
Tobin JA, Flitman SS. Occipital nerve blocks: effect of symptomatic medication: overuse and headache type on failure rate. Headache. 2009;49:1479–85. https://doi.org/10.1111/j.1526-4610.2009.01549.x.
Tobin J, Flitman S. Occipital nerve blocks: when and what to inject? Headache. 2009;49:1521–33. https://doi.org/10.1111/j.1526-4610.2009.01493.x.
Johnstone CS, Sundaraj R. Occipital nerve stimulation for the treatment of occipital neuralgia-eight case studies. Neuromodulation. 2006;9:41–7. https://doi.org/10.1111/j.1525-1403.2006.00041.x.
Cesmebasi A, Muhleman MA, Hulsberg P, Gielecki J, Matusz P, Tubbs RS, Loukas M. Occipital neuralgia: anatomic considerations. Clin Anat. 2015;28:101–8. https://doi.org/10.1002/ca.22468.
Bogduk N. Cervicogenic headache: anatomic basis and pathophysiologic mechanisms. Curr Pain Headache Rep. 2001;5:382–6.
Vanelderen P, Lataster A, Levy R, Mekhail N, van Kleef M, Van Zundert J. 8. Occipital neuralgia. Pain Pract. 2010;10:137–44. https://doi.org/10.1111/j.1533-2500.2009.00355.x.
Cohen SP, Peterlin BL, Fulton L, Neely ET, Kurihara C, Gupta A, Mali J, Fu DC, Jacobs MB, Plunkett AR, Verdun AJ, Stojanovic MP, Hanling S, Constantinescu O, White RL, McLean BC, Pasquina PF, Zhao Z. Randomized, double-blind, comparative-effectiveness study comparing pulsed radiofrequency to steroid injections for occipital neuralgia or migraine with occipital nerve tenderness. Pain. 2015;156:2585–94. https://doi.org/10.1097/j.pain.0000000000000373.
Slavin KV, Nersesyan H, Wess C. Peripheral neurostimulation for treatment of intractable occipital neuralgia. Neurosurgery. 2006;58:112–119; discussion 112-119.
Weiner RL, Reed KL. Peripheral neurostimulation for control of intractable occipital neuralgia. Neuromodulation. 1999;2:217–21. https://doi.org/10.1046/j.1525-1403.1999.00217.x.
Sweet JA, Mitchell LS, Narouze S, Sharan AD, Falowski SM, Schwalb JM, Machado A, Rosenow JM, Petersen EA, Hayek SM, Arle JE, Pilitsis JG. Occipital nerve stimulation for the treatment of patients with medically refractory occipital neuralgia: congress of neurological surgeons systematic review and evidence-based guideline. Neurosurgery. 2015;77:332–41. https://doi.org/10.1227/NEU.0000000000000872.
Bovim G, Sand T. Cervicogenic headache, migraine without aura and tension-type headache. Diagnostic blockade of greater occipital and supra-orbital nerves. Pain. 1992;51:43–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Staudt, M.D., Sweet, J.A. (2018). Representative Clinical Case: Occipital Neuralgia. In: Suen, J., Petersen, E. (eds) Diagnosis and Management of Head and Face Pain. Springer, Cham. https://doi.org/10.1007/978-3-319-90999-8_39
Download citation
DOI: https://doi.org/10.1007/978-3-319-90999-8_39
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-90998-1
Online ISBN: 978-3-319-90999-8
eBook Packages: MedicineMedicine (R0)