Abstract
REM sleep behavior disorder (RBD) is a potentially injurious parasomnia characterized by dream enactment behavior and polysomnographic REM sleep atonia loss (REM sleep without atonia, RSWA), most commonly seen as a manifestation of an early alpha-synuclein-mediated neurodegenerative disease in older adults. However, RBD has also been reported to evolve following lesions in the brainstem or limbic system. To date, 44 cases of “lesional RBD” have been reported in the literature. Age of lesional RBD onset and male predominance is similar to presumably synuclein-mediated RBD. Lesions to either the left or right dorsal pons, superior medulla, or limbic system appear to be most strongly associated with development of RBD, supporting the localization of REM sleep atonia control to the locus subcoeruleus/sublateral dorsal nucleus (SubC/SLD) of the pons. A variety of etiologies including infarction/encephalomalacia, inflammatory/demyelinating disorders, autoimmune disease, vascular malformation, and neoplasm have been associated with the development of lesional RBD, suggesting lesion location is more important than etiology in the development of RBD. It remains unknown whether brain lesions interact with preexisting covert pontine synuclein deposits that are already present (i.e., whether lesional RBD requires a “two-hit” pathophysiology) or perhaps with other vulnerability factors that could predispose toward RBD development, since lesional RBD is much rarer than pontine lesions in the general population. The development of RBD following either a discrete lesion to the dorsal pontine location of the SubC/SLD or extraaxial lesions exerting mass effect on the brainstem suggests that disruption or disturbance of the SubC/SLD or its afferent/efferent projections to other structures in the REM atonia control network can cause RBD. Lesional RBD may be refractory to pharmacologic treatment with or without continued presence of the lesion, and resolution of RBD following effective treatment of the underlying etiology is variable, likely depending upon the degree of reversibility of damage or possibly due to permanent impact and alteration of REM atonia control networks following disturbance by a lesion even after its resolution. Patients who develop RBD along with focal neurologic deficits or in the context of subacutely evolving syndromic neurologic manifestations of encephalopathy, cognitive, autonomic, or movement disorder impairments should undergo brain magnetic resonance imaging to rule out a structural lesion as the cause of their RBD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Long before the initial description of REM sleep behavior disorder (RBD) in 1986 by Schenck and colleagues, aggressive or violent “oneiric” behaviors suggestive of dream enactment accompanied by REM atonia loss (REM sleep without atonia, RSWA) were reported by Jouvet and Delorme from Lyon in 1965 following bilateral experimental lesioning of the peri-locus coeruleus in cats, anticipating the eventual discovery of RBD in humans [1]. Following these seminal experiments, several centers throughout Europe, Japan, and the United States reported cases of RBD-like phenomena, including two young girls with brainstem tumors associated with the development of RBD in 1975 and 1986, before RBD was formally recognized in 1986 [2,3,4]. Since Jouvet and Delorme’s initial description of RBD-like phenomena in the cat, lesion studies in animals and RBD associated with brain lesions in humans have significantly furthered our understanding of brain networks implicated in the generation and maintenance of REM sleep atonia. The association between RBD and synuclein-mediated neurodegenerative diseases has become widely recognized, with most research on RBD focusing on neurodegeneration . However, the occurrence of RBD secondary to a brain lesion remains an important consideration in the differential diagnosis of abnormal nocturnal behaviors , especially in patients with a known history of autoimmune or vascular disease or those presenting with focal deficits on neurologic examination.
2 Diagnosis of Lesional RBD
There are currently no consensus diagnostic criteria for lesional RBD. Iranzo and Aparicio have suggested five possible criteria, including the onset and evolution of RBD associated with lesional brain pathology, that is, (1) temporally associated, (2) coincident with other lesion-associated symptoms, (3) located in a brainstem or limbic system area known to regulate REM sleep, (4) associated with remission or improvement of RBD symptoms paralleling lesion resolution, and (5) not better explained by another disorder, such as synucleinopathy, medication use, or withdrawal [5]. Brain imaging is not indicated in most newly diagnosed RBD patients, especially if they have symptoms suggestive of concurrent neurodegenerative disease. However, brain MRI should be strongly considered when RBD presents at a young age, with sudden onset of symptoms, or when accompanied by focal neurologic deficits on examination, to rule out a structural lesion as the etiology.
3 Demographics of Lesional RBD
To date, 31 individual cases of structural lesion-associated RBD and 13 additional cases of RBD associated with stroke from one large series have been reported in the literature (Tables 9.1, 9.2, and 9.3) [2, 3, 5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Of these 44 RBD cases, 64% were men, similar to the male predominance in RBD with presumed synucleinopathy [7]. Average age of RBD diagnosis in these lesional patients was 56 (range 8–81) years, also similar to that of RBD with presumed synuclein-mediated disease. However, age of RBD onset may occur at different ages depending on etiology (neoplastic/iatrogenic , 38 years; inflammatory/autoimmune/genetic , 49 years; and vascular/infarction , 70 years) [4, 24]. Isolated RBD occurred in 77% of lesional RBD cases, while 10 patients presented with RBD in association with additional sleep/wake disorders, including status dissociatus [18], peduncular hallucinosis [27], sleepwalking [13, 20], restless legs syndrome [6, 24], narcolepsy [14, 28], and cataplexy [19] (Chap. 8 covers RBD associated with paraneoplastic and autoimmune disorders).
4 Etiology and Location of Lesional RBD Cases
The range of etiologies in lesional RBD cases is broad, although vascular lesions account for over half of reported cases, followed by inflammatory/autoimmune lesions and neoplasm. Ischemic stroke is the most common vascular cause, with the majority of infarcts occurring in the brainstem, especially in the dorsal pons [11, 22, 26, 27]. Additionally, the volume of stroke appears to be important in the development of post-stroke RBD, with smaller infarct volume being associated with RBD [22]. This association is most likely due to the small size (and small vascular territories) of vessels supplying regions thought to control REM muscle atonia (i.e., the brainstem), whereas large vessel infarctions with large vascular territories (i.e., middle cerebral artery) are not associated with regions thought to be associated with REM sleep. Laterality may not appear to be important, since both left and right pontine strokes have been reported in RBD patients [11, 26, 27]. Vascular lesional pathology , especially brainstem cavernomas and basilar aneurysms, may also result in RBD and other sleep/wake disturbances, presumably due to distortion of the tegmentoreticular tract [5, 6, 15].
Inflammatory/demyelinating lesions causing RBD typically occur in younger individuals and may be associated with lesions outside of the pontomedullary junction. Several cases of pontine multiple sclerosis (MS) lesions have been associated with the development of RBD [14, 17, 23]. Additionally, one case of CNS vasculitis and one inflammatory lesion of unknown etiology, both in the pons, have also been reported to cause RBD [13, 21] (Fig. 9.1). Autoimmune encephalitides can also cause RBD, with or without apparent structural pathology. In the first seminal descriptive case series of IgLON5 autoimmunity (with antibodies against IgLON5 (a member of the neuronal cell adhesion molecule superfamily)) described by Sabater and colleagues, four of eight cases had RBD [20]. Of these four, one of whom also had additional NREM parasomnia, two RBD patients had pathologic evidence for diffuse neurodegeneration with structural pathology in the brainstem. In these cases, autopsy showed predominant hyperphosphorylated neuronal tau deposits and neuronal loss predominantly in the prehypothalamic, hypothalamic, and pontine tegmentum regions in the vicinity of the pedunculopontine and raphe neurons and less intensely in magnocellular nuclei of reticular formation, likely explaining REM sleep atonia loss with clinical RBD (although brain MRI was normal) [20]. Additional cases of RBD associated with IgLON5 have also been reported by others having similar serologic evidence for autoimmunity against IgLON5 but lacking pathologic confirmation of structural neurodegenerative pathology [29, 30]. However, three cases of autoimmune encephalitis (two due to voltage-gated potassium channel (VGKC) autoantibodies , one with anti-Ma2 antibodies ) have been associated with RBD in the absence of pontine lesions [9, 15, 28]. Brain MRI revealed involvement of the limbic system in all three cases, suggesting that limbic system pathology may also influence emotionally charged dream enactment and REM sleep atonia control, which is plausible given the connectivity across the amygdala, hypothalamus, and brainstem that is hypothesized to result in emotion-triggered cataplexy in patients with narcolepsy type 1 [31, 32]. However, in the context of intact hypocretinergic neurons and lesional pathology in the pons causing REM atonia loss (RSWA), this “feed forward” influence of the limbic system would cause dream enactment rather than cataplexy. Please see Chap. 8 for a more in-depth review of RBD associated with autoimmunity.
Lesional RBD in the dorsal pontomedullary junction resulting from CNS vasculitis. Top panel. Coronal FLAIR intensity MRI sections at the level of the medulla and pons, showing a discrete longitudinally extensive hyperintense lesion at the level of the dorsomedial pons extending rostrally to the right superior pons ventral to the superior cerebellar peduncle. Bottom panel. The brainstem nuclei thought to be involved in REM sleep atonia regulation are shown on human brainstem templates. Letters for each template and corresponding MRI FLAIR image sections selected from our case represent cross-sectional views through the brainstem as shown in the midsagittal figure, with sections representing (A) the pontomesencephalic junction, (B) the upper/mid-pons, (C) the lower/mid-pons, and (D) the pontomedullary junction. The approximate location of the lesion is shown in the superimposed pink oval. VLPAG ventrolateral periaquaductal gray, LC locus coeruleus, LDT laterodorsal tegmental nucleus, LPT lateral pontine tegmentum, PC precoeruleus, PPN pedunculopontine nucleus, REM rapid eye movement, RN raphe nucleus, SLD sublaterodorsal nucleus, vlPAG ventrolateral part of the periaqueductal gray matter. As modified from Boeve BF, Silber MH, Saper C, et al. Pathophysiology of REM sleep behavior disorder and relevance to neurodegenerative disease. Brain 2007;130:2770–2788. Reprinted with permission from St. Louis EK, McCarter SJ, Boeve BF, Kantarci K, Rando A, Silber MH, Olson EJ, Tippmann-Peikert M, Mauerman M. REM sleep behavior disorder localizes to the dorsomedial pons. Neurology 2014;83(20):1871–3
Neoplasm is the third most common cause of lesional RBD, usually presenting as a cerebellopontine angle mass. Three cases of meningioma and one of neurinoma (schwannoma , typically known as an “acoustic neuroma ”) at the cerebellopontine angle have been reported to cause RBD, presumably secondary to mass effect and distortion of the brainstem tegmentoreticular tract [2, 15, 25]. While the majority of neoplasms associated with RBD have been extraaxial, one intraaxial case of diffuse large B-cell lymphoma at the pontomesencephalic junction has also been reported [10]. Similar to vascular and inflammatory lesions, extraaxial cerebellopontine neoplasms with mass effect on either side of the brainstem may cause RBD.
RBD has been reported to occur rarely in association with genetic conditions. However, RBD in these cases is likely secondary to selective lesions in the pons rather than the associated genetic condition per se. RBD has been reported in two patients with Wilson’s disease that had pontine/mesencephalic hyperintense brain lesions on MRI (with hypointensity of the basal ganglia on susceptibility-weighted imaging suggestive of copper deposition) [24]. Further, a patient with autosomal dominant adult onset leukodystrophy due to lamin B1 gene duplication with diffuse T2 hyperintensities longitudinally throughout the midbrain, pons, and medulla also had dream enactment behaviors [8]. Developmental malformation of the posterior fossa such as Chiari malformations may also lead to brainstem compression, thereby altering REM sleep atonia control networks that may result in RBD. In fact, one large series of patients with Chiari Type I and II malformations found that 23% of patients met polysomnographic criteria for RBD, significantly higher than would be expected in the general population (these patients were not included in the 40 cases mentioned above due to lack of reported individual patient data) [33].
Finally, iatrogenic causes of RBD may occur in patients who had instrumentation near the brainstem in the posterior fossa. While RBD can certainly occur in patients with cavernomas, RBD, along with status dissociatus, occurred following cavernoma resection at the pontomesencephalic junction [18]. Another patient developed RBD after resection of a posterior fossa epidermoid cyst with associated brainstem signal change on MRI, while a 10-year-old girl began exhibiting dream enactment behavior and REM sleep without atonia following the resection of a midline cerebellar astrocytoma [3, 15]. Interestingly, RBD associated with neoplasm and iatrogenic causes (such as the removal of a posterior fossa mass) appears to occur relatively more frequently in children than other causes of RBD, perhaps except for narcolepsy type 1. As such, the development of RBD in a child should prompt neuroimaging of the posterior fossa. Similarly, physicians should be aware of the risk of children developing RBD following the resection of posterior fossa tumors.
5 Treatment and Outcomes of Lesional RBD Patients
Response to treatment of lesional RBD cases is highly variable, probably due to different etiologies and treatment responsiveness and whether the lesion resolves or persists. Interestingly, similar to synuclein-associated RBD, lesional RBD may also respond to symptomatic therapy with either melatonin or clonazepam [34]. Tumor resection and/or chemotherapy in three patients resulted in remission or significant reduction of dream enactment, whereas RBD outcomes were variable in two other patients treated with clonazepam and/or melatonin whose meningiomas were not resected [15, 25]. Similarly, in some patients with MS, RBD symptoms improved with MRI-documented lesion remission, whereas others continued to have RBD symptoms despite MS-specific therapy and despite symptomatic treatment of RBD with melatonin or clonazepam [17, 23, 35]. In both cases of VGKC autoantibody-associated RBD, dream-enacting behavior (DEB) improved with immunosuppression, whereas immunosuppression had no effect on RBD and narcolepsy symptoms in a case associated with anti-Ma2 receptor encephalitis [9, 15, 28]. Unfortunately, RBD associated with anti-IgLON5 antibodies often portends a poor prognosis and is largely unresponsive to immunosuppression, although recent evidence has also emerged of a more heterogeneous and favorable course in IgLON5 autoimmunity syndrome following immunotherapy [29]. In patients with vascular lesions, treatment response was also variable. Ultimately, we recommend initial definitive treatment of the underlying etiology causing lesional RBD when possible and feasible, as well as symptomatic pharmacologic treatment with melatonin or clonazepam to prevent injury, especially in cases where treatment for the underlying lesional cause is not possible or successful.
More than 80% of patients with presumed synuclein-mediated RBD undergo phenoconversion to a defined, clinically overt neurodegenerative disease over longitudinal follow-up [36, 37], yet thus far, available follow-up data on lesional RBD patients does not suggest that these patients develop parkinsonism, cognitive impairment, or non-motor features suggesting development of an eventual neurodegenerative disease. In the largest reported series of lesional RBD, none of the patients developed parkinsonian features or cognitive impairment suggestive of synucleinopathy over an average of 45.4 ± 35.2 months of follow-up [15]. Additionally, another patient with RBD attributed to a pontine cavernoma had a normal 123I-FP-CIT SPECT scan, which is often abnormal in presumably synuclein-mediated RBD, implicating the cavernoma as the sole culprit for that patient’s dream enactment [28, 38]. Thus, current available evidence suggests that the brain lesion causes disturbance in REM sleep atonia control that leads to clinically overt RBD symptoms. However, it remains possible that in a subset of patients with what appears to be lesional RBD, there could be interaction between brain lesions and covert underlying synuclein deposits in the brainstem, unveiling earlier clinical expression than would otherwise be seen, similar to some current hypotheses concerning antidepressant-associated RBD. Additional longitudinal follow-up outcome studies of larger series of patients with lesional RBD will be necessary to determine if there is any relationship to underlying covert synucleinopathy.
6 Pathophysiologic Lessons Learned from Lesional RBD
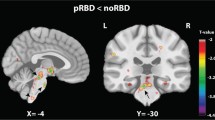
While the pathophysiology of RBD and anatomy of REM sleep control networks are discussed in great detail in other chapters of this textbook, lesional RBD has also contributed to our understanding of the control of REM sleep in humans. Evidence from studies in the cat, rat, and mouse suggest that glutamatergic neurons in the dorsal pontine sublateral dorsal nucleus (SLD) , also known as subcoeruleus (SubC) , located at the pontomesencephalic junction, are key in generation of REM sleep atonia [39,40,41] (Fig. 9.1). SLD glutamatergic neurons project to the trigeminal nucleus, ventromedial medulla, and spinal cord, synapsing on GABAA, GABAB, and glycinergic premotoneurons in the ventromedial medulla (gigantocellularis nucleus), resulting in hyperpolarization of trigeminal and spinal cord motoneurons and resulting in normal, physiologic REM sleep atonia [32, 39,40,41,42,43,44,45,46,47,48]. Genetic inactivation of the rat glutamate SLD leads to the development of RBD with relative preservation of daily REM sleep quantity, further suggesting that the SLD is necessary for the generation and maintenance of REM muscle atonia, but not the sleep state itself [47].
Of the 29 individually reported cases of lesional RBD, all but three cases involve lesions directly within the pontomesencephalic junction or below, or mass effect from an extraaxial lesion compressing the pons, furthering evidence for location of the SLD/SubC at the pontomesencephalic junction with descending projections through the tegmentoreticular tract to the inhibitory medullary gigantocellular nucleus [39, 44]. The three cases of RBD without brainstem lesions seen on brain imaging had limbic system involvement. While it is possible these patients had damage to the brainstem not visible with current imaging modalities, recent evidence suggests that lateral hypothalamic and forebrain structures project to the SLD and influence the onset and maintenance of REM sleep and REM sleep atonia, suggesting that patients with isolated supratentorial limbic lesions may have had RBD evolve due to disruption of this circuit [40].
Interestingly, intraaxial lesions are more likely to cause RBD as well as other symptoms (such as narcolepsy, cataplexy, status dissociatus, sleepwalking, and peduncular hallucinosis), while extraaxial lesions appear to cause DEB alone. Extraaxial lesions likely displace longitudinal tracts such as the tegmentoreticular or reticulospinal tracts distal to the SLD, causing incomplete REM sleep muscle atonia, whereas intraaxial brainstem lesions may damage nuclei directly or damage structures superior to the SLD involved in the generation of REM sleep, leading to several sleep/wake abnormalities other than RBD [44, 47]. Of reported lesional RBD cases, the majority are not bilateral, with lesions on either side of the brainstem leading to RBD, suggesting that a unilateral lesion is sufficient to cause RSWA and RBD symptoms, similar to a previous lesional study showing that unilateral ventral mesopontine junction lesions were sufficient to cause RSWA in cats [12, 49]. Given the diversity of causative pathologies seen in lesional RBD cases, and recent evidence of genetic inactivation of the glutamate SLD leading to RBD symptoms, location of the lesion and not the underlying disease process (i.e., inflammatory/demyelinative, infarct, vascular malformation, tumor, surgery, etc.) appears to be the principle factor related to the development of RBD [47]. However, some patients have complete remission of RBD symptoms with radiographic remission of lesions (i.e., as in MS) [23], while other patients continue to have RBD symptoms despite radiographic remission (i.e., a case of vasculitis) [21]. Mechanistic difference between disease processes may result in transient or permanent damage, and varying degrees of damage may impact nuclei directly, projections within the REM atonia control network, or both, leading to variable influences on persistence or resolution of RBD symptoms irrespective of grossly visible lesion persistence on neuroimaging.
Conclusions
Lesional RBD typically occurs following insult to the brainstem, especially when involving the dorsal pons or projections of the dorsal pontine sublateral dorsal nucleus and/or medullary nucleus magnocellularis, supporting growing evidence for pontine governance of REM sleep atonia. A variety of pathological processes have been implicated in lesional RBD, suggesting that lesion location rather than etiology is the primary determining factor in the development of RBD. Lesional RBD typically evolves acutely or subacutely, with or without additional accompanying focal neurological symptoms and signs suggestive of brainstem dysfunction, but in the case of a slowly growing tumor (e.g., a cerebellopontine angle mass, such as an acoustic neuroma), RBD can evolve more indolently and chronically, so a careful neurological history and examination need to be performed in all patients with RBD. In patients with abrupt onset of focal neurological symptoms and associated DEB, especially in children, a brainstem lesion or limbic encephalitis must be considered with prompt brain MRI to exclude lesional pathology, as treatment of the underlying condition, such as resection of a tumor, or immunotherapy to decrease inflammation, may improve or resolve DEB and potentially prevent other neurological complications associated with a structural brain lesion. Patients who suffer brainstem injury through infarct or inflammatory processes should also be queried about possible dream enactment and followed carefully for possible development of RBD so that timely therapy may be initiated to prevent injury.
References
Jouvet M, Delorme F. Locus coeruleus et sommeil paradoxal. C R Soc Biol. 1965;159:895–9.
De Barros-Ferreira M, Chodkiewicz JP, Lairy GC, Salzarulo P. Disorganized relations of tonic and phasic events of REM sleep in a case of brain-stem tumour. Electroencephalogr Clin Neurophysiol. 1975;38(2):203–7.
Schenck CH, Bundlie SR, Smith SA, Ettinger MG, Mahowald MW. REM behavior disorder in a 10 year old girl and aperiodic REM and NREM sleep movements in an 8 year old brother. Sleep Res. 1986;15:162.
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986;9(2):293–308.
Iranzo A, Aparicio J. A lesson from anatomy: focal brain lesions causing REM sleep behavior disorder. Sleep Med. 2009;10(1):9–12.
Felix S, Thobois S, Peter-Derex L. Rapid eye movement sleep ҫ disorder symptomatic of a brain stem cavernoma. J Sleep Res. 2016;25(2):211–5.
Fernandez-Arcos A, Iranzo A, Serradell M, Gaig C, Santamaria J. The clinical phenotype of idiopathic rapid eye movement sleep behavior disorder at presentation: a study in 203 consecutive patients. Sleep. 2016;39(1):121–32.
Flanagan EP, Gavrilova RH, Boeve BF, Kumar N, Jelsing EJ, Silber MH. Adult-onset autosomal dominant leukodystrophy presenting with REM sleep behavior disorder. Neurology. 2013;80(1):118–20.
Iranzo A, Graus F, Clover L, Morera J, Bruna J, Vilar C, et al. Rapid eye movement sleep behavior disorder and potassium channel antibody-associated limbic encephalitis. Ann Neurol. 2006;59(1):178–81.
Jianhua C, Xiuqin L, Quancai C, Heyang S, Yan H. Rapid eye movement sleep behavior disorder in a patient with brainstem lymphoma. Intern Med. 2013;52(5):617–21.
Kimura K, Tachibana N, Kohyama J, Otsuka Y, Fukazawa S, Waki R. A discrete pontine ischemic lesion could cause REM sleep behavior disorder. Neurology. 2000;55(6):894–5.
Lai YY, Hsieh KC, Nguyen D, Peever J, Siegel JM. Neurotoxic lesions at the ventral mesopontine junction change sleep time and muscle activity during sleep: an animal model of motor disorders in sleep. Neuroscience. 2008;154(2):431–43.
Limousin N, Dehais C, Gout O, Heran F, Oudiette D, Arnulf I. A brainstem inflammatory lesion causing REM sleep behavior disorder and sleepwalking (parasomnia overlap disorder). Sleep Med. 2009;10(9):1059–62.
Mathis J, Hess CW, Bassetti C. Isolated mediotegmental lesion causing narcolepsy and rapid eye movement sleep ҫ disorder: a case evidencing a common pathway in narcolepsy and rapid eye movement sleep ҫ disorder. J Neurol Neurosurg Psychiatry. 2007;78(4):427–9.
McCarter SJ, Tippmann-Peikert M, Sandness DJ, Flanagan EP, Kantarci K, Boeve BF, et al. Neuroimaging-evident lesional pathology associated with REM sleep behavior disorder. Sleep Med. 2015;16(12):1502–10.
Peter A, Hansen ML, Merkl A, Voigtlander S, Bajbouj M, Danker-Hopfe H. REM sleep behavior disorder and excessive startle reaction to visual stimuli in a patient with pontine lesions. Sleep Med. 2008;9(6):697–700.
Plazzi G, Montagna P. Remitting REM sleep behavior disorder as the initial sign of multiple sclerosis. Sleep Med. 2002;3(5):437–9.
Provini F, Vetrugno R, Pastorelli F, Lombardi C, Plazzi G, Marliani AF, et al. Status dissociatus after surgery for tegmental ponto-mesencephalic cavernoma: a state-dependent disorder of motor control during sleep. Mov Disord. 2004;19(6):719–23.
Reynolds TQ, Roy A. Isolated cataplexy and REM sleep behavior disorder after pontine stroke. J Clin Sleep Med. 2011;7(2):211–3.
Sabater L, Gaig C, Gelpi E, Bataller L, Lewerenz J, Torres-Vega E, et al. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol. 2014;13(6):575–86.
St Louis EK, McCarter SJ, Boeve BF, Silber MH, Kantarci K, Benarroch EE, et al. Lesional REM sleep behavior disorder localizes to the dorsomedial pons. Neurology. 2014;83(20):1871–3.
Tang WK, Hermann DM, Chen YK, Liang HJ, Liu XX, Chu WC, et al. Brainstem infarcts predict REM sleep behavior disorder in acute ischemic stroke. BMC Neurol. 2014;14:88.
Tippmann-Peikert M, Boeve BF, Keegan BM. REM sleep behavior disorder initiated by acute brainstem multiple sclerosis. Neurology. 2006;66(8):1277–9.
Tribl GG, Bor-Seng-Shu E, Trindade MC, Lucato LT, Teixeira MJ, Barbosa ER. Wilson’s disease presenting as rapid eye movement sleep behavior disorder: a possible window to early treatment. Arq Neuropsiquiatr. 2014;72(9):653–8.
Zambelis T, Paparrigopoulos T, Soldatos CR. REM sleep ҫ disorder associated with a neurinoma of the left pontocerebellar angle. J Neurol Neurosurg Psychiatry. 2002;72(6):821–2.
Zhang X, Wang LN. REM sleep behavior disorder in a patient with pontine stroke. Sleep Med. 2009;10(1):143–6.
Geddes MR, Tie Y, Gabrieli JD, McGinnis SM, Golby AJ, Whitfield-Gabrieli S. Altered functional connectivity in lesional peduncular hallucinosis with REM sleep behavior disorder. Cortex. 2016;74:96–106.
Compta Y, Iranzo A, Santamaria J, Casamitjana R, Graus F. REM sleep behavior disorder and narcoleptic features in anti-Ma2-associated encephalitis. Sleep. 2007;30(6):767–9.
Honorat JA, Komorowski L, Josephs KA, Fechner K, St Louis EK, Hinson SR, et al. IgLON5 antibody: neurological accompaniments and outcomes in 20 patients. Neurol Neuroimmunol Neuroinflamm. 2017;4(5):e385.
Hogl B, Heidbreder A, Santamaria J, Graus F, Poewe W. IgLON5 autoimmunity and abnormal ҫs during sleep. Lancet. 2015;385(9977):1590.
Dauvilliers Y, Siegel JM, Lopez R, Torontali ZA, Peever JH. Cataplexy—clinical aspects, pathophysiology and management strategy. Nat Rev Neurol. 2014;10(7):386–95.
Luppi PH, Clement O, Sapin E, Garcia SV, Peyron C, Fort P. Animal models of REM dysfunctions: what they tell us about the cause of narcolepsy and RBD? Arch Ital Biol. 2014;152(2–3):118–28.
Henriques PSA, Pratesi R. Sleep apnea and REM sleep behavior disorder in patients with Chiari malformations. Arq Neuropsiquiatr. 2008;66(2B):344–9.
McCarter SJ, Boswell CL, St Louis EK, Dueffert LG, Slocumb N, Boeve BF, et al. Treatment outcomes in REM sleep behavior disorder. Sleep Med. 2013;14(3):237–42.
Gomez-Choco MJ, Iranzo A, Blanco Y, Graus F, Santamaria J, Saiz A. Prevalence of restless legs syndrome and REM sleep behavior disorder in multiple sclerosis. Mult Scler. 2007;13(6):805–8.
Iranzo A, Tolosa E, Gelpi E, Molinuevo JL, Valldeoriola F, Serradell M, et al. Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep ҫ disorder: an observational cohort study. Lancet Neurol. 2013;12(5):443–53.
Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013;14(8):744–8.
Iranzo A, Valldeoriola F, Lomena F, Molinuevo JL, Serradell M, Salamero M, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep ҫ disorder: a prospective study. Lancet Neurol. 2011;10(9):797–805.
Fraigne JJ, Torontali ZA, Snow MB, Peever JH. REM sleep at its Core—circuits, neurotransmitters, and pathophysiology. Front Neurol. 2015;6:123.
Luppi PH, Clement O, Fort P. Paradoxical (REM) sleep genesis by the brainstem is under hypothalamic control. Curr Opin Neurobiol. 2013;23(5):786–92.
Peever J, Luppi PH, Montplaisir J. Breakdown in REM sleep circuitry underlies REM sleep behavior disorder. Trends Neurosci. 2014;37(5):279–88.
Brooks PL, Peever JH. Glycinergic and GABA(A)-mediated inhibition of somatic motoneurons does not mediate rapid eye movement sleep motor atonia. J Neurosci. 2008;28(14):3535–45.
Brooks PL, Peever JH. Identification of the transmitter and receptor mechanisms responsible for REM sleep paralysis. J Neurosci. 2012;32(29):9785–95.
Carroll C, Landau ME. Effects of pontine lesions on REM sleep. Curr Neurol Neurosci Rep. 2014;14(7):460.
Luppi PH, Gervasoni D, Verret L, Goutagny R, Peyron C, Salvert D, et al. Paradoxical (REM) sleep genesis: the switch from an aminergic-cholinergic to a GABAergic-glutamatergic hypothesis. J Physiol Paris. 2006;100(5–6):271–83.
Soja PJ, Lopez-Rodriguez F, Morales FR, Chase MH. The postsynaptic inhibitory control of lumbar motoneurons during the atonia of active sleep: effect of strychnine on motoneuron properties. J Neurosci. 1991;11(9):2804–11.
Valencia Garcia S, Libourel PA, Lazarus M, Grassi D, Luppi PH, Fort P. Genetic inactivation of glutamate neurons in the rat sublaterodorsal tegmental nucleus recapitulates REM sleep ҫ disorder. Brain. 2017;140(Pt 2):414–28.
Weng FJ, Williams RH, Hawryluk JM, Lu J, Scammell TE, Saper CB, et al. Carbachol excites sublaterodorsal nucleus neurons projecting to the spinal cord. J Physiol. 2014;592(Pt 7):1601–17.
Hendricks JC, Morrison AR, Mann GL. Different behaviors during paradoxical sleep without Atonia depend on pontine lesion site. Brain Res. 1982;239(1):81–105.
Acknowledgments
The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 1 UL1 RR024150-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Disclosures
No off-label medication use.
The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 1 UL1 RR024150-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
SJ McCarter reports no disclosures.
EK St. Louis reports that he receives research support from the Mayo Clinic Center for Translational Science Activities (CTSA), supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 1 UL1 RR024150-01.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
McCarter, S.J., St. Louis, E.K. (2019). Lesional RBD. In: Schenck, C., Högl, B., Videnovic, A. (eds) Rapid-Eye-Movement Sleep Behavior Disorder. Springer, Cham. https://doi.org/10.1007/978-3-319-90152-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-90152-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-90151-0
Online ISBN: 978-3-319-90152-7
eBook Packages: MedicineMedicine (R0)