Abstract
The majority of patients with hyperhidrosis classify their quality of life as poor or very poor. Because the symptoms are manifested through the skin, the individual has his emotions exposed to others, often transforming a common social situation into an embarrassment. In general, the impact on patients’ quality of life depends not only on the sweat intensity, but also how well patients adapt to this situation, their psychic resources to deal with adverse situations, and the psychosocial context in which they are inserted. Because hyperhidrosis predominantly arises in childhood and adolescence, it can become responsible for greater damage to the mental health of patients with it, which in turn negatively influences the evolution of the disease. Because it causes high suffering and loss in the patient’s relational life, psychotherapy is an important form of treatment and follow-up, since it provides host, strengthening, and helps the development of skills for facing the adverse situations experienced by these patients.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
The association between anxiety, depressive symptomatology, and chronic diseases is not uncommon. The prevalence of anxiety or depression in people with changes in physical health is broad, about 18–35% and 15–61%, respectively. In addition, there is evidence that these emotional repercussions are associated with a decrease in quality of life , generating a significant impact in patients with hyperhidrosis (HH).
It is known that, although it isn’t considered a serious disease, the quality of life of patients with HH is considerably affected. The symptoms are manifested through the skin, the body’s means of communication with the external world, and it is through it that the individual has his emotions exposed to others, often transforming a common social situation into an embarrassment, generating greater vigilance of the individual in relation to the body itself and their contact with people.
Recent studies indicate that most HH patients classify their quality of life as poor or very poor, and that following treatment they perceive significant benefits, including improvement in quality of life related to physical and mental health. In general, the impact on the patients’ quality of life depends not only on the sweat intensity, but also how well patients adapt to this situation, their psychic resources to deal with adverse situations, and the psychosocial context in which they are inserted.
Currently there are specific questionnaires to evaluate quality of life in HH, and although there is still no consensus on the best way to assess the quality of life of these patients, studies show the importance of using these instruments to indicate the most appropriate treatment , whether clinical or surgical, and to verify the efficacy of the treatment performed.
Difficulties in adapting to the adverse situations imposed by the clinical manifestations of HH can be reflected in several areas, causing impairment in social life, academic and professional performance, and self-image, in addition to a greater tendency of these patients to develop mood changes associated with anxiety and depression . When exposed to chronic sources of stress , that damage becomes more frequent and requires continuous adaptation, causing subjective suffering to the patient.
Anxiety and stress are conditions commonly triggered by the appearance and development of a disease, and are considered aggravating factors for the degree of sweating.
Although there is little research to prove the cause and effect relationship of co-morbidities and psychological aggravating factors in patients with HH, some authors point out a higher prevalence of anxiety in those patients than in the general population and patients with other chronic diseases. Depressive symptoms are usually less prevalent and, when present, are associated with anxiety. Corroborating this idea, studies show a correlation among the indexes of anxiety, depression , and dermatological diseases, without necessarily establishing a cause and effect relationship.
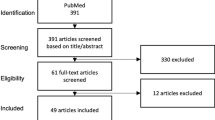
Since this topic doesn’t yet have a large literature, a study is being carried out in the Hyperhidrosis Outpatient Clinic of the Thoracic Surgery Service of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HCFMUSP). This research aims to evaluate the presence of anxiety and depression symptoms in patients with HH and its association with the perception of patients related to the degree of sweating, as well as the effect of clinical treatment on HH symptoms and its association with anxious and depressive symptomatology.
Because HH predominantly arises in childhood and adolescence, age groups considered important in the emotional development of the individual, and in which there is a certain predisposition to the development of some types of psychopathologies, it can become responsible for greater damage to the mental health of those younger people and negatively influence the evolution of the disease. However, it is important to note that the emotional repercussions, which may or may not affect HH patients, don’t necessarily indicate the presence of a psychiatric disorder.
Due to the fact that, on some occasions, HH is triggered by stress or emotions, patients are often characterized as anxious, timid, and unsafe individuals, eventually leading to diagnostic errors and stereotypes in this regard. However, HH is not only caused by emotional stimulation, so a misunderstanding of this relationship can generate a significant loss of confidence and reduce the capacity of the individual to discriminate between what is physiological and what is emotional, negatively influencing their coping with the condition and treatment of the disease, since many individuals live years believing that excessive sweating is due to anxiety , not the opposite, and because of this, they delay the search for a solution to the HH.
Thus, it is important that differential diagnoses be correctly defined and the indicate treatment is relevant to the needs and demands of the subject, so that the person can have a better quality of life and is better adapted to the social and environmental demands in their life. In addition, early treatment of HH can be considered preventive in order to avoid or aggravate psychic and social disorders, since HH is a risk factor for the development of these conditions, which are often reactive or overlap the process of the disease and are not the primary cause of this condition.
What commonly occurs in the clinic when assessing HH patients who manifest some associated emotional symptom is the diagnosis of adjustment disorders described in the ICD-10 ( International Statistical Classification of Diseases and Related Health Problems, 10th edition ) and DSM ( Diagnostic and Statistical Manual of Mental Disorders ) diagnostic manuals. Adjustment disorders are characterized by the presence of emotional and behavioral symptoms in response to an identifiable stressor . Such a disorder may present as depressed mood; anxiety; anxiety and depression ; behavioral disturbance; or even mixed disturbance of emotions and conduct, characterized as a state of subjective suffering and emotional disturbance, which can lead to impairments in the social and professional performance of the individual. According to the DSM-5, symptomatic responses to an identifiable stressor should occur within 3 months of the onset of the stressor event, and do not last more than 6 months after the stressor and its consequences cease.
In cases in which the stressor is persistent, adjustment disorders can progress to the chronic form, causing significant suffering and impairment in the patients’ quality of life , and eventually to their family members and people living with them. It is understood that when emotional symptoms fall within the diagnostic criteria of adjustment disorders, patients tend to exhibit emotional and behavioral symptoms in response to the stress of having a medical condition that causes harm in different spheres of the subject’s life until the symptoms of HH are treated.
Preliminary data from the study being conducted in our unit has been relevant in supporting this idea, pointing out that 5 weeks after the beginning of clinical treatment for symptoms of HH it is already possible to measure and compare levels of intensity of anxiety and depressive symptomatology before and after treatment, indicating a decrease in the anxious and depressive symptoms , concomitant with the improvement of the clinical symptoms of HH in a significant number of the patients. Based on these data, Table 9.1 shows the main anxious and depressive symptoms reported by patients with HH symptoms.
Currently, there are several instruments available to evaluate emotional symptoms that help professionals to perform better screening and diagnosis processes, which favor the planning of more effective interventions, and with significantly more favorable results to solve the psychic problem presented concomitant with clinical manifestations of HH. For proper choice of the evaluation instrument it is important that the professional considers the characteristics and symptoms presented by the patient and also knows the characteristics of application and correction of the instruments.
In addition to the use of instruments, clinical interviews of the patient are also necessary, considering the areas of life that are negatively affected by HH, the individual’s understanding of the disease, treatment expectations, and whether the emotional and social damage, eventually presented by the patient, are only reactive to the presence of HH, if the disease is an aggravating factor of the pre-existing emotional symptoms , or if it has triggered more severe emotional losses.
The possibility that emotional symptoms are a transient condition, as in the case of adjustment disorders , doesn’t mean that they don’t need to be treated. Because these symptoms cause high suffering and loss in the patient’s relational life, with his environment and with himself, psychotherapy is an important form of treatment and follow-up of these patients, since it provides host, strengthening, and helps the development of skills for facing the situations experienced by HH patients.
By favoring the emergence of psychic coping resources, the psychologist assists in the development of resilient behaviors, aiming at overcoming crises and adversities to which these individuals are exposed, strengthening individual attributes and environmental resources in a process that results in overcoming and managing these situations. Thus, the relationship between resilience and the disease situation is contextualized as the individual’s ability to deal with his diagnosis and its implications, adapting and evolving positively and creatively.
Suggested Reading
Andrade Filho LO, Campos JRM, Jatene FB, Kauffman P, Kusniek S, Werebe EC, Wolosker N. Quality of life, before and after thoracic sympathectomy: report on 378 operated patients. Ann Thorac Surg. 2003;76:886–91.
Campbell TPDA, Campos JRM, Kauffman P, Krutman M, Puech-Leão P, Schvartsman C, Wolosker N. Efficacy and quality of life outcomes of oxybutynin for treating palmar hyperhidrosis in children younger than 14 years old. Pediatr Dermatol. 2014;31:48–53.
Dias LIN, Miranda ECM, Mussi RK, Toro IFC, Mussi RK. Relation between anxiety, depression and quality of life with the intensity of reflex sweating after thoracic sympathectomy by video-surgery for the treatment of primary hyperhidrosis. Rev Col Bras Cir. 2016;43:354–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Kamikava, D.Y.F. (2018). Anxiety, Depression, and Hyperhidrosis. In: Loureiro, M., Campos, J., Wolosker, N., Kauffman, P. (eds) Hyperhidrosis. Springer, Cham. https://doi.org/10.1007/978-3-319-89527-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-89527-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-89526-0
Online ISBN: 978-3-319-89527-7
eBook Packages: MedicineMedicine (R0)