Abstract
This chapter characterizes and defines the clinical manifestations of hyperhidrosis, describes the main types of glands responsible for these symptoms, with their distribution in different areas of the body, and, finally, describes the main topical agents that can combat and control these symptoms.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Several dermatological diseases are perceived by those who have them as disgusting, even when they are not contagious. Like the obese, the patient with excessive sweating or hyperhidrosis is perceived by those around him as being guilty of causing their condition:
-
“He is very nervous and so does not stop sweating.”
-
“She does not care, she’s fat, so she sweats too much.”
-
“He is smelly, he does not take a shower.”
-
“She is rude because she does not perform proper foot hygiene.”
Hyperhidrosis sufferers, in turn, feel this constant judgment and their self-esteem is seriously affected. It is common to find patients with hyperhidrosis who have drastically changed their lives because of this condition. This critical situation is easier to understand when we know some phrases of hyperhidrosis obtained in surveys undertaken by consumer services departments of the manufacturers of antiperspirants :
“I just have a dream. Only one. One day I could wear a silk sweater.”
“I did not invite anyone to my wedding, I did not get married in the church and there was no party.”
“I did not want to be seen on the altar sweating without stopping.”
“My dream was to be a dentist like my father. I cannot be a dentist and have palmar hyperhidrosis.”
“My boyfriend told me, you stink.”
“My boss said, you have to stay hidden from customers. You cannot greet anyone shaking hands.”
Hyperhidrosis
Hyperhidrosis is a hidrosis, that is a disease of, the eccrine or apocrine sweat glands .
General aspects of the sweat glands.
Eccrine Glands
The eccrine glands and the eccrine bud of the epidermis are found all over the skin, except in the labial mucosa, nail bed, small vulval lips, in the glans, and inner face of the foreskin. They are found in greater numbers and are more developed in the palmar, plantar, and axillary regions (Fig. 13.1).
Eccrine glands are tubular glands, which have a secretory folded part and a duct that, coming out of the dermis, crosses the epidermis (acrosiringium) and opens directly on the surface of the skin. This hole is invisible except on the palms and soles of the feet where they can be recognized with a magnifying glass. The eccrine glands are innervated by cholinergic sympathetic fibers and secrete a variable amount of sweat after exogenous stimuli, such as the heat of the environment, or endogenously by metabolic changes.
The secretions of the eccrine glands are also affected by emotional factors or neurological injuries. Depending on the intensity of the stimuli, the secretion can be localized only in the palmoplantar and/or axillary or generalized regions. In the secretory phase, the glandular cells do not alter their shape and size, the secretion is almost immediate after the stimulus, and takes between 10 and 30 s from the secretory part to the sweat pore. If there is stimulation, it can have several hours of continuous activity. A high-intensity heat stimulus, such as exercise, can produce up to 3 L of sweat per hour.
Sweat
Sweat is a clear, odorless liquid that is 99.5% water. The main components are sodium, potassium, calcium, magnesium, chloride, urea, and lactate. Traces of amino acids, immunoglobulins, prostaglandins, vitamins, and systemically administered drugs can be found.
Secretory Function
The secretory function of the eccrine glands does not replace renal function, even partially. The primordial function of the eccrine glands is thermoregulation, that is, to maintain, through sweating, the temperature of the body.
Apocrine Glands
The apocrine glands originate from the primary epithelial bud together with the sebaceous glands and hairs. They differ from the eccrine glands, not only by embryogenesis but also in function, distribution, size, and type of secretion.
While the eccrine glands are indispensable for thermoregulation, the apocrine glands have an odorous function, which is not important for humans but is important for sexual behavior in animals.
The apocrine glands are found in the armpits, mammary region, sternal, periumbilical, pubic and anogenital regions, and exceptionally in the trunk and scalp. The ceruminous glands of the auditory channels, the Moll glands of the eyelids, and the mammary glands are modified apocrine glands. They are located in the reticular dermis and are on average ten times larger than the eccrine glands. The excretory canal opens into the infundibulum, near the follicular orifice. In puberty, due to hormonal influence, the apocrine glands increase in size and initiate their secretion.
Innervation of the apocrine glands is sympathetic, with secretion induced by alpha and beta fibers being adrenergic and cholinergic. After stimulation, a yellowish-white viscous liquid containing varying amounts of cholesterol, triglycerides, fatty acids, cholesterol esters, and squalene is produced. Traces of ammonia, carbohydrates, and hormones such as dehydroepiandrosterone and androsterone can be found. The secretion, initially sterile and odorless, mainly occurs in the armpits. This secretion is decomposed by microorganisms, mainly Corynobacteria , which causes the appearance of odor. The odor is sui-generis and individually variable. It can be distinguished between continuous secretion from hormone or nervous/emotional stimulation.
Apocrine secretion diminishes with age, but it can persist into old age.
Eccrine Gland Disorders
Sweating is extremely variable from individual to individual, depends on age and race, and is influenced by endogenous and exogenous factors. Hyperhidrosis can be generalized or localized in some regions. Currently, neural hyperhidrosis is considered to be caused by:
-
Stimuli of the cortex (cortical hyperhidrosis) due to the presence of hyperhidrosis.
-
Stimuli that reach the hypothalamus (hypothalamic hyperhidrosis).
-
Lesions in the central or peripheral nervous system, or from the sweat glands themselves and non-neural hyperhidroses.
-
Hyperhidroses due to genetic alterations of the eccrine secretion.
Hyperhidroses of Neural or Non-neural Origin
Hyperhidrosis can be neural or non-neural in origin.
Hyperhidrosis of neural origin can be cortical, hypothalamic, gustatory, or caused by injuries to the spinal cord, trunk, and nerve fibers or reflexes. Non-neural hyperhidroses result from the action of heat on the skin, the action of drugs, altered bloodflow, or changes in the sweat glands themselves. Cortical or emotional hyperhidrosis is a more generalized hyperhidrosis in certain areas such as axillary, palmoplantar regions, and perineum-inguinal, and may eventually be a localized form.
It is frequently suggested that at least some cases of hyperhidrosis arise from autosomal dominant inheritance and therefore familial cases exist. The sweat glands are normal and there is no change in cholinesterase. It is assumed that specific nucleus impulses located in the cortex are processed by the hypothalamus from where they are led by the nerve pathways to the sympathetic fibers of the sweat glands , producing release of excessive amounts of acetylcholine with consequent increase in sweating. In fact, cortical hyperhidrosis improves during sleep, which would be explained by the diminution of the nerve impulses.
Generalized cortical hyperhidrosis occurs most often in the richer regions of the sweat glands , such as the scalp, forehead, groin, armpit, plantar region, and palms. In addition, it does not change in warmer environments, demonstrating no influence of thermally sensitive stimuli. When it occurs on the scalp and forehead it is unpleasant but usually does not bring secondary complications. In the groin area, it facilitates the installation of intertriginous eruptions, such as candidiasis or dermatophytosis (mycosis or tinea).
Axillary and palmo-plantar hyperhidrosis are the forms that cause major problems as they can alter the individual’s quality of life, hamper work, and alter the psychosocial behavior of the individual. Plantar hyperhidrosis, usually of early onset, may facilitate the onset of fungal infections and a grooved plantar hyperkeratosis.
Axillary hyperhidrosis begins after puberty. There is a racial variation according to the development of the sweat glands . It is constant and naturally intensifies with emotional factors, heat, and exercise. Axillary hyperhidrosis may be the patient’s main complaint, although 25% of cases also have discrete palmoplantar hyperhidrosis. Axillary hyperhidrosis, unlike palmoplantar hyperhidrosis, responds variably to thermal stimuli. It is to be noted that the apocrine glands are innervated by adrenergic fibers, unlike the eccrines, which are stimulated by cholinergic fibers.
Axillary hyperhidrosis may favor the appearance of pyogenic infections, erythrasma, candidiasis, and contact dermatitis caused by products used to reduce it.
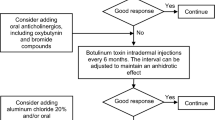
Treatment
In cortical hyperhidrosis, the patient should be informed about the influence of emotional factors, possibly prescribing tranquilizers such as diazepines .
Anticholinergic drugs can be used to provide relief. For plantar hyperhidrosis , it is necessary to wear cotton socks whenever possible, and leather-soled shoes, preferably a sandal type. Closed shoes with no openings would worsen the problem because they prevent air circulation. The leather sole absorbs the moisture. When bacterial or fungal secondary infections occur, specific treatments are indicated.
Hypothalamic or Thermal Hyperhidrosis
Hypothalamic or thermal hyperhidrosis is caused by stimulation of the hypothalamic temperature-regulating centers that may possibly present an increased sensitivity. In this way, minimal stimulation can trigger intense hyperhidrosis. The main source of stimulation of the hypothalamus is an increase in temperature due to exogenous (heat) or endogenous causes: exercise and diseases that cause a temperature rise, infections, particularly tuberculosis, malaria, brucellosis, and lymphomas. In addition, a large number of conditions can cause hypothalamic hyperhidrosis, including metabolic changes (hyperpituitarism, hyperthyroidism), diabetes mellitus, gout, obesity, pregnancy, menopause, hypoglycemia, porphyrias, alcoholism. In diabetes, hyperhidrosis may occur in episodes of hypoglycemia.
Hypothalamic hyperhidrosis can be caused by the following drugs: antipyretics, non-hormonal anti-inflammatory drugs (acetylsalicylic acid, indomethacin, piroxicam, sulindac, naproxen), anticholinergics (acetylcholine, fisiostigmine, pilocarpine, methacholine), adrenergics (epinephrine, norepinephrine, dopamine, isoproterenol), drugs acting on the central nervous system (amitriptyline, amphetamine, caffeine, chlorpromazine, doxepin, phenothiazine, fluoxetine, haloperidol, yohimbine, nortriptyline), paroxic toxic substances for chronic arsenicism, and illicit drugs.
It should be noted that hypothalamic hyperhidrosis does not diminish during sleep and may become even more intense.
Treatment of hypothalamic hyperhidrosis is symptomatic or oriented towards correcting its cause.
Topical Treatment
It should be noted that while there is no definitive topical treatment, there are control treatments for hyperhidrosis, such as antiperspirants and deodorants that are widely used in the armpits for most of the population.
Antiperspirants are used to control sweating; they reduce sweating and therefore alter local bacterial growth.
Deodorants are made to fight the bad odor generated by the bacteria present in the microbiome. They basically contain antibacterial and fragrance aspects. Deodorants with potent antiperspirant properties can significantly improve the quality of life of millions of people worldwide.
Focal hyperhidrosis affects 2% of the population worldwide and only 40% of these people seek medical attention for treatment. The use of aluminum and its derivatives as an antiperspirant is already advised by the majority of dermatologists.
Aluminum chloride was the first antiperspirant active ingredient used with good efficacy. However, it has the drawback of causing skin irritation, blemishes, and tissue damage due to the pH of the aqueous solutions of this substance.
Aluminum hydrochloride has thus emerged to minimize the drawbacks of aluminum chloride. Their solutions have a pH closer to that of the skin and cause less damage to the tissues. The mechanism of action of the antiperspirants is the diffusion of the salt by the sweat duct which, after slow neutralization of the acidic solution of metallic salt, produces a gel or mucopolysaccharide complex. This obstruction prevents sweat from escaping and remains until the normal processes of cell renewal replace the affected keratin. There is no evidence of permanent damage to sweat glands , especially since normal sweating resumes immediately after discontinuation of the product.
Adverse Effects
Occasionally, the daily use of antiperspirants can irritate the skin, causing a burning sensation. The onset of irritation may occur immediately or after days or weeks of use. However, the cure begins to be observed within 3 days after the total withdrawal of the irritant.
Antiperspirants and Breast Cancer
Antiperspirants are products that inhibit or decrease perspiration. The difference between a deodorant and antiperspirant is that the former serves to remove the odor of the armpits, while the latter is responsible for reducing the amount of sweat produced. Most of the antiperspirants also work as deodorants , but most deodorants do not act as antiperspirants.
According to a technical opinion published by ANVISA (the Brazilian National Agency of Sanitary Surveillance), there no significant data in the scientific literature to date relating the aluminum salts present in antiperspirant formulae with the incidence of breast cancer .
Change history
29 December 2018
Correction to: M. P. Loureiro et al. (eds.), Hyperhidrosis https://doi.org/10.1007/978-3-319-89527-7
Suggested Reading
Wolosker N, Fukuda JM. Editorial—current treatment of hyperhidrosis. J Vasc Bras. 2015;14(4):279–81.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Purcelli, M. (2018). Hyperhidrosis and Topical Agents. In: Loureiro, M., Campos, J., Wolosker, N., Kauffman, P. (eds) Hyperhidrosis. Springer, Cham. https://doi.org/10.1007/978-3-319-89527-7_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-89527-7_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-89526-0
Online ISBN: 978-3-319-89527-7
eBook Packages: MedicineMedicine (R0)