Abstract
One of the paramount changes in human evolution was the development of large brain size with a tremendous impact on the nutritional behavior of our species. A larger brain demands more food intake to keep up with the need of the overall energy budget. This high demand for energy to maintain the brain metabolism forced early humans to move from a strictly vegetarian diet to more energy-rich diet. Changes in nutrient-rich energy diets evolving from an exclusively vegetarian to an omnivorous diet were among many evolutionary factors developed to maintain the high cost of a large human brain. Paleontological data indicates that fast brain evolution occurred with the appearance of Homo erectus 1.8 million years ago, which was related to critical changes in diet, body size, and foraging behavior. Then, the survival of more advanced humans depended on their ability to acquire energy for its daily use and storage, which was well balanced before the advent of modern humans. The energy balance of early humans is disrupted today by an excessive food intake, processed food, and an increase in sedentary life. Obesity pandemic has undoubtedly coincided with not only an increase in unhealthy eating habits but also with migratory movements of different ethnic communities to dissimilar environmental pressures. The heat producing of uncoupling proteins in mitochondria brown adipocyte tissue is believed to be a key driver behind the conquest of a variety of environments in mammals 65 million years ago. This ability to produce and maintain heat contributed to the evolution of mammals to explore and settle in uninhabitable territories throughout the planet by adjusting the thermoregulatory response to sharply different environments. It is also discussed in this chapter several early evolutionary hypotheses to explain the development of obesity and metabolic syndrome, the evolutionary changes from hominoids 20 million years ago to industrialized humans, and the effects on traits causing profound changes in the evolution of human nutritional requirements.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
One of the paramount changes in human evolution was the development of large brain size with a tremendous impact on the nutritional behavior of our species. A larger brain demands more food intake to keep up with the need of the overall energy budget. This high demand for energy to maintain the brain metabolism forced early humans to move from a strictly vegetarian diet to more energy-rich diet. Changes in nutrient-rich energy diets evolving from an exclusively vegetarian to an omnivorous diet were among many evolutionary factors developed to maintain the high cost of a large human brain. Paleontological data indicates that fast brain evolution occurred with the appearance of Homo erectus 1.8 million years ago, which was related to critical changes in diet, body size, and foraging behavior. Then, the survival of more advanced humans depended on their ability to acquire energy for its daily use and storage, which was well balanced before the advent of modern humans. The energy balance of early humans is disrupted today by an excessive food intake, processed food, and an increase in sedentary life. Obesity pandemic has undoubtedly coincided with not only an increase in unhealthy eating habits but also with migratory movements of different ethnic communities to dissimilar environmental pressures. The heat producing of uncoupling proteins in mitochondria brown adipocyte tissue is believed to be a key driver behind the conquest of a variety of environments in mammals 65 million years ago. This ability to produce and maintain heat contributed to the evolution of mammals to explore and settle in uninhabitable territories throughout the planet by adjusting the thermoregulatory response to sharply different environments. It is also discussed in this chapter several early evolutionary hypotheses to explain the development of obesity and metabolic syndrome, the evolutionary changes from hominoids 20 million years ago to industrialized humans, and the effects on traits causing profound changes in the evolution of human nutritional requirements.
2 Brain Evolution and Changes in Human Nutrition
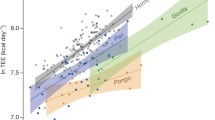
One of the chief characteristics of humans is that they are holding big brains, and the evolution of this large brain size has had significant implications for the nutritional biology of our species. On average, our brain size as part of the primates group is nearly double from mammals of the same body size. Throughout nearly 7 million years of evolution, the human brain has tripled in size, and the past 2 million years represents the most significant brain growth. The large human brain is energetically expensive and uses a more significant proportion of its energy budget on brain metabolism as compared with other primates with a lower energy budget. For example, humans consume 400 more calories than chimpanzees and 635 more calories than gorillas and 820 more calories than orangutans. Paleontological data pointed out that a rapid brain evolution occurred with the emergence of Homo erectus 1.8 million years ago. These posture changes are related to significant changes in diet, body size, and hunting behavior (Table 1.1). These alterations are dramatic enough that separated us from our close relatives, including the great apes or hominids, which are a taxonomic family of primates. They include seven species in four genera, Pongo, the Bornean and Sumatran orangutan; Gorilla, the Eastern and Western gorilla; Pan, the common chimpanzee and the bonobo; and Homo, the human and the near-human ancestors and relatives (e.g., the Neanderthal) (Chatterjee et al. 2009). The combination of larger brains, high reproductive output with slow childhood growth, changes in history of social behavior, and an extraordinary longevity separated us far apart from other apes (Isler and van Schaik 2012; Schuppli et al. 2012; van Schaik et al. 2012; van Woerden et al. 2012). Consistent with these observations, analysis from African human fossils indicates that significant changes in both brain size and diet were linked with the rise of early members of the genus Homo between 2.0 and 1.7 millions of years ago. The question that arises from these observations was then how much energy supply would be needed to maintain metabolism in these brains in a steady-state status? Changes in nutrient-rich energy diets evolving from an exclusively vegetarian to an omnivorous diet were among many evolutionary factors developed to maintain the high cost of a large human brain.
The fact that early genus Homo consumed more animal foods was a turning point in providing elevated levels of essential long-chain polyunsaturated fatty acids (docosahexaenoic acid and arachidonic acid) highly necessary for brain growth. This evolutionary adaptation forced humans to use a larger proportion of their resting energy budget on brain metabolism separating them again from other primates or non-primate mammal. One of the key features developed by humans was learning to share food, making social groups of early humans more resilient, spreading their diets, and obtaining more energy from rich foods such as meat. Humans also developed much larger deposits of body fat, which can be used to sustain them during periods of food scarcity. Also, compare with other primates, humans have a relatively small gastrointestinal tract and reduced colon allowing for greater energy allocation to reproduction and limiting the increase in basic metabolic rate. This type of adaptation is consistent with a high in energy and nutrient intake quickly to digest. Another important feature was the improved walking efficiency in the evolution of early H. erectus 1.8 million of years ago. Evidence also supports an important evolutionary adaptive change involving hunting and hoarding, which resulted in greater consumption of animal foods and sharing the prey within other social groups. Dietary changes to energy-dense foods and the discovery of cooking (of thermal and nonthermal food processing) in modern humans successfully increased the net energy gained. These were significant contributors to the evolutionary expansion of the hominin energy budget (humans and great apes together form a superfamily called hominoids). The genus H. erectus appears to develop a rapid rate of a bigger part of the central nervous system contained within the cranium and comprising of the forebrain (prosencephalon), midbrain (mesencephalon), and hindbrain (rhombencephalon). Finally, humans have smaller muscle mass and more fat tissue as compared with other primates helping to offset the high-energy demands of our brains. These high levels of adiposity in humans are especially prominent in infants to accommodate the growth of their large brains with enough supply of stored energy (Pontzer et al. 2016a, b). In summary, these evolutionary traits caused profound changes in the evolution of human nutritional requirements (Anton et al. 2014; Cordain et al. 2005; Eaton 2006; Garn and Leonard 1989; Leonard and Robertson 1992, 1994) separating us further apart from other primates in terms of distinctive nutritional needs (Leonard 2002; Leonard et al. 2007).
Through evolution time, our ancestors ate poorly, particularly during climate disadvantages, and they often had vitamin deficiencies, food-borne diseases, and neurotoxins. Dirt, grit, and fiber constituted a significant part of most early diets. With the advent of modern technologies, these food components diminished. The profound changes in the environmental components including diet and lifestyle circumstances introduced by agriculture and animal husbandry approximately 10,000 years ago are too recent on an evolutionary time scale for the human genome to change. The lack of agreement between our ancient genes adjusted to the earlier way of nutritional behaviors compared to the cultural patterns of contemporary Western life created the so-called diseases of modern civilizations. The evolutionary clash of our ancient genome with the nutritional variants of recently introduced processed foods may be the cause of the established chronic diseases of Western civilization. Food-processing procedures introduced during the Neolithic period was considered the last part of the Stone Age. The New Stone Age is a time limit in the development of human technology starting about 10,200 BC and ending between 4500 and 2000 BC. In addition, industrial development has essentially altered seven essential nutritional traits of ancestral hominin diets: (a) glycemic load, (b) fatty acid composition, (c) micronutrient density, (d) macronutrient composition, (e) sodium-potassium ratio, (f) acid-base balance, and (g) fiber content. From this point forward, the changes introduced by modern humans to industrially processed foods associated with less physical activity represented the springboard to a deviation of our natural nutritional environment unfamiliar to our genetic repertoire.
3 Definition of Obesity
As described above, the human genome has hardly changed since the emergence of modern humans leaving East Africa 70,000 years ago. Genetically, humans remain adapted for the foods consumed at that time in history. From the records, the proposal is that human ancestors obtained about 35% of their dietary energy from fats, 35% from carbohydrates, and 30% from protein. Saturated fats contributed approximately 7.5% total energy. Polyunsaturated fat intake was high, cholesterol consumption was significant, and carbohydrate came from uncultivated fruits and vegetables. The latter represented 50% energy consumption as compared with the 16% energy intake consumed today by Americans. While high levels of fruits and vegetables and minimal grain consumption constituted the ancestral diet, today’s diet is far apart from that regime. Honey included 2–3% energy intake as compared with the 15% added sugars which contribute to the present time. Also, fiber consumption in ancient humans was high. Although a significant progress was made in understanding ancient human diet, nutritionists are still searching for a unifying hypothesis on which to build a dietary strategy for prevention. Therefore, a better understanding of human evolutionary nutritional habits and its impact on contemporary nutritional requirements could help us with strategies to better define obesity and combat this malady.
Over the last five decades, there has been a major widespread of obesity, which is associated with many comorbidities or metabolic syndrome, mostly in the Western world but reaching now a global dimension. The development of these chronic diseases in the culture of the west is related to high genetic components within different populations. As obesity rates soared between 1980 and 2017, the number of Americans who are obese has doubled. In the United States alone, 70% of the adult population is overweight, and 36% are obese. There are ~700 million obese people worldwide, and another ~2.1 or more billion who are overweight, according to the World Health Organization. There is today a financial burden in the United States with obesity-related healthcare costs. In 2005 and 2006 alone, 150–190 billion dollars was spent on obesity-related diseases. In 2010, no state had a prevalence of obesity less than 20%.
Thirty-six states had occurrence equal to or greater than 25%; 12 of these states (Alabama, Arkansas, Kentucky, Louisiana, Michigan, Mississippi, Missouri, Oklahoma, South Carolina, Tennessee, Texas, and West Virginia) had prevalence equal to or greater than 30%. The estimation is that by the year 2030, healthcare costs will increase by more than 50 billion dollars annually. There are more obese and overweight people on the planet than people suffering from malnutrition. In spite of the great progress made in the field of energy balance, our understanding of some basic mechanisms to combat this malady remains unclear. Obesity and its associated medical complications including type 2 diabetes, cardiovascular disease, dyslipidemia, mood disorders, reproductive disorders, hypertension, asthma, and potential for cancer development account for more than 300,000 deaths per year in the United States. Obesity treatment strategies often do not result in adequate, sustained weight loss, and the prevalence and severity of obesity in the United States and many other countries are progressively increasing (Ahima 2005). Current treatments include dietary changes, increased physical activity, prescription medications, weight loss surgery, and behavior modification. Most surgical and pharmacological treatments require lifestyle changes to achieve sustained weight loss fully. However, dangerous side effects may accompany these treatment strategies. In addition, some pharmacotherapies may not work in certain individuals. The complexity of the obese condition results from the interaction between environmental and predisposing genetic factors interacting with each other. Specifically, genes operate additively and through gene-gene interactions to influence body weight (Clement 2005). A more thorough understanding of the molecular mechanisms underlying the pathogenesis of obesity and regulation of energy metabolism is essential for the development of effective therapies. Therefore, it is necessary to characterize the molecular and behavioral mechanisms governing body weight to identify the abnormality or impairment in the regulation of the metabolic, physiological, and psychological mechanisms causing obesity.
One of the major obstacles encountered in the United States to combat the obesity prevalence is related to the fact that junk foods are the largest source of calories in the American diet. They include grain-based desserts like cookies, doughnuts, granola bars, sugary soda, and fruit juices, an excess of pasta and pizza, and pieces of bread with high sugar content to name some. What all these foods have in common, different from the same meals made in the 1950s, is that they are mainly the products of seven crops and farm foods. They are corn, soybeans, wheat, rice, sorghum, milk, and meat heavily subsidized through decades by the federal government, ensuring that junk foods are cheap and plentiful. As a matter of fact, between 1995 and 2010, the government contributed with $170 billion in agricultural subsidies to finance these foods. While many of these foods are not innately unhealthy, only a small percentage of them are eaten as is (New York Times, How the Government Supports Your Junk Food Habit, by Anahad O’Connor, July 19, 2016). All these products are converted to cheap foods and additives like corn sweeteners, industrial oils, processed meats, and refined carbohydrates. It is quite ironic that on the one hand, the government promotes healthy diets (organic fruits and vegetables) while at the same time has the complicity in supporting the industrial production of junk food leaving a very small fraction of its subsidies to support the production of fresh produce. The result is that taxpayers are paying for the privilege of making our country sick (Anahad O’Connor, New York Times). The subsidies program was started decades ago in part to support struggling farmers and to secure America’s food supply. Since 1995 the government has provided farmers with close to $300 billion in agricultural subsidies overall; today the grants program no longer helps its original purpose because it continues to give subsidies to large producers of grains, corn, sorghum, and oilseeds like soybeans instead of small farmers who grow fruits, nuts, and vegetables. In summary, we created an evolution to self-destruction (Fig. 1.1).
Evolution to self-destruction: The recent substantial increase in the prevalence of obesity in susceptible individuals has been mostly caused by our modern urban societies in which demand for physical activity is extremely reduced, and highly palatable and relatively cheap food is ubiquitously available. Geographic migrations with an adaptive thermogenesis added an additional variable to the confounding problem of obesity
Having described our ancient and modern diets, we can now define obesity as a state of excess adipose tissue mass, which translates into excessive body weight and an alteration of energy balance (this condition may not be confused with a body builder that can develop a remarkable overweight state without excessive body fatness). Energy balance is defined by the number of calories consumed versus the amount of energy used either via exercise, physical activity, or resting metabolism. Energy derived from food intake enters the plasma from the intestine and then to cells involved in energy consumption. Under normal conditions, any minor excess is dealt with by cells that function in energy storage. When the number of calories expended is the same with the number of calories consumed, the energy caloric balance is neutral, and no change in weight occurs. On the other hand when the number of calorie intake is greater than a number of calories expended, an energy balance disruption occurs (positive energy balance), and obesity develops. Therefore, obesity occurs as a result of a long-standing imbalance between energy intake and energy expenditure, which is influenced by a very complex set of biological pathway systems regulating appetite. We then can say that obesity is a “disorder of energy balance.” According to the World Health Organization (WHO), obesity is classified as class I for a BMI between 30 and 34.9 kg/m2, class II for a BMI between 35 and 39.9 kg/m2, and class III for a BMI ≥ 40 kg/m2 (Obesity: preventing and managing the global epidemic 2000). Class I obesity is associated with a moderate risk, class II with a high risk, and class III with a very high risk of mortality (Gonzalez et al. 2007). Anatomically obesity can be classified for the prevalence of visceral or subcutaneous deposition of fat. The ratio of waist circumference to hip circumference (WHR) is used to serve the purpose of defining the degree of central (i.e., visceral) vs. peripheral (i.e., subcutaneous) obesity. Visceral adiposity is a major risk factor for metabolic syndrome, while subcutaneous fat seems to be much more benign and in some cases even protective against the development of metabolic complications (Jensen 2008). The metabolic syndrome can be defined as a group of risk factors that increases blood pressure, high blood sugar, excess body fat around the waist, abnormal cholesterol, or triglyceride levels causing to increase the risk of heart disease, stroke, and diabetes. To understand the imbalance in obesity from the calorie in and calorie out is a complicated matter. While calories from food are easy to control, the way calories burn represents a different undertaking. It consists mainly of the energy required for the basal metabolism of the body, at rest, in the absence of external work. That’s called resting energy expenditure, which represents 60–70% of the total energy expenditure. However, it is highly variable from individual to individual. The second component is the physical activity that is the sum of basal activities of daily living and voluntary exercise. The third part of total energy expenditure, although small, is diet-induced thermogenesis, which is the energy associated with a postprandial rise in metabolic rate to process food during digestion, usually amounting about 10% of calories.
Obesity can also be caused by treating diseases with pharmacological treatments including steroids, antipsychotics, some antidepressants, and some anti-epileptics but could also be a consequence of some diseases or conditions, including polycystic ovary syndrome (PCOS), Cushing’s syndrome, hypothyroidism, hypothalamic defects, and growth hormone deficiency. Obesity is frequently associated with low androgen levels causing hypogonadism. Hyperinsulinemia is believed to be the primary etiological factor for the development of PCOS, but there are other factors involved as well such as obesity-induced hyperestrogenism and a male pattern adipokine gene expression observed in these women. Obesity also causes a reduction in growth hormone secretion in the pituitary gland. The decrease in growth hormone does not appear to translate into a similar reduction in IGF-1. Therefore it is unlikely that obesity represents a condition of growth hormone deficiency reflected at the tissue level. Both growth hormone deficiency and growth hormone excess are associated with increase in fat mass.
4 Nutritional Balance, Metabolic and Hedonic Set Point
The survival of all species depends on their ability to acquire energy for its daily use and storage. From an evolutionary standpoint, feeding or intake of calories from meal to meal is necessary to (a) satisfy nutritional and metabolic requirements and (b) prepare for periods of food shortage during seasonal changes. Energy balance is the relationship that exists between energy intake (i.e., calories taken from food and drink) and energy expenditure (i.e., calories being used for our daily energy requirements). Hence, the maintenance of this balance is achieved by the integration of (a) environmental signals (i.e., environmental cues steer individuals’ decisions concerning food intake and food choice), (b) physiological and metabolic signals (i.e., neurohormone, peripheral hormones, nutrient sensors, and key organs), (c) genetic makeup (i.e., multiple genetic interactions, epigenetic actions), and (d) social and hedonic influences (i.e., the drive to eat to obtain pleasure without an energy deficit). When this balance is disrupted, we witness either a weight gain or a weight loss. In the case of weight gain or positive energy balance, energy imbalance is caused by a higher calorie intake versus the number of calories burned.
However, defining when energy balance is disrupted represents a complex undertaking. For example, excessive food intake is likely to be the primary cause of positive energy balance (obese phenotype) driven by both nonconscious (homeostatic) and conscious (perceptual, emotional, and cognitive) phenomena processed in the brain. Functional neuroimaging in a few studies has provided evidence of functional differences between obese and lean individuals in the brain’s response to energy intake (DelParigi et al. 2005a). Connecting hyperphagia to actual weight gain has proved remarkably difficult (Stunkard et al. 1999; Tataranni et al. 2003). The experimental evidence connecting the relative contribution among people who have differences in energy intake, expenditure, and resting metabolic rate or due to physical activity to weight gain is limited. In addition, food intake and development of obesity involve diet composition (Astrup 1999; Astrup et al. 1997), energy density of food (Bell and Rolls 2001) (Drewnowski 2003), rate of meal consumption, taste preferences (Cooling and Blundell 2001), eating behavioral style (Keski-Rahkonen et al. 2003), and subphenotypes (DelParigi et al. 2005a, b), all of them contribute but complicate matters with some contradictory results. Within the United States, a significant decline in the percentage of energy from fat foods during the last two decades has paralleled with a massive increase in obesity. Therefore, diets high in fat do not seem to be the cause of high prevalence in excess body fat in our society, suggesting that decreases in fat content will not be the answer (Willett and Leibel 2002). The genetics of obesity is also partially understood because it is not clear whether obesity is caused by a single genetic mutation, by multiple allelic defects, and which one of those determines susceptibility to environmental factors including epigenetic contribution. Epigenetics is defined as a stable heritable traits or phenotypes that cannot be explained by changes in DNA sequence or changes to the genome that do not involve a change in the nucleotide sequence. This genetic change means features that are “on top of” or “in addition to” the traditional genetic basis for inheritance (those are shifts in a chromosome that affect gene activity and expression) (Pomp and Mohlke 2008). It’s hard to predict who will or will not develop obesity in an obesogenic environment. It depends on an individual combination of alleles in gene-gene interaction and how it reacts with the environment in a particular way. People who carry only one or some of these alleles may still not develop obesity because they either lack another allele in gene-gene interaction needed or are not exposed to the stimulating environment causing gene-environment interaction. Further clarification will be necessary to resolve the controversy that exists among genotypes and lifestyle (Holzapfel et al. 2010) or anatomical phenotype of obesity (Bauer et al. 2009; de Krom et al. 2009).
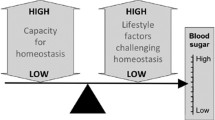
For quite some time, it has been suggested that there are two systems controlling eating behavior (Saper et al. 2002). The metabolic system is regulated by mediators such as leptin and ghrelin, neuropeptide Y (NPY), agouti-related peptide (AgRP), melanocortins, orexins, and melanin-concentrating hormone, among the important ones. The second one is the hedonic behavior that is regulated by taste and reward systems to certain foods (Fig. 1.2). Hence, one of the common questions regarding the epidemic of obesity in modern society is whether hedonic feeding overcomes metabolic feeding. It is well accepted that body weight is determined via both mechanisms, and recurrence of food consumption above the minimum energy requirements to fulfill basic metabolism is the hallmark of obesity. Metabolic needs drive food intake in response to changes in body energy status, which is dictated by the brain at the hypothalamic level and responsibly in determining the “body weight set point” to maintain energy homeostasis at a constant level. This programmed set point is regulated by a circuitry of neuronal cells in the hypothalamus and other specific brain regions. It is controlled mostly by leptin, insulin, and ghrelin acting on melanocortin anorectic neurons pro-opiomelanocortin/cocaine- and amphetamine-regulated transcript (POMC/CART) and orectic AgRP/NPY (Kim et al. 2014; Koch et al. 2015; Waterson and Horvath 2015). Another second order of neurons located in the lateral hypothalamus (LH) contains orexins and melanocyte-concentrating hormone (MCH); both peptides are potent stimulators of food intake (Ludwig et al. 2001; Flier 2004). The ventromedial hypothalamus (VMH), which is controlled by leptin through the regulation of brain-derived neurotrophic factor (BDNF), also regulates energy balance. The paraventricular nucleus (PVN) of the hypothalamus contains several groups of neurons all involved in energy balance regulation of corticotropin-releasing hormone (CRH) signaling in the PVN which increases leptin signaling in the VMH (Gotoh et al. 2005). Hypophysiotropic thyrotropin-releasing hormone (TRH) neurons expressing the leptin receptor (ObRb) are considered as one of the primary hypothalamic centers controlling food intake and energy homeostasis (Nillni 2010; Nillni and Sevarino 1999; Perello et al. 2006; Sanchez et al. 2004; Elmquist et al. 1998; Elias et al. 1999). Oxytocin produced in the PVN and vasopressin generated in the PVN and supraoptic nucleus together with the brain stem interacting with glucagon-like peptide-1 (GLP-1), cholecystokinin (CCK), serotonin, and melanocortin (see full description in Chap. 2) are all involved in the energy balance regulation (Fig. 1.3, Chap. 2). The metabolic body weight set point is genetically regulated, but exposure to a constant obesogenic environment may provoke allostatic adaptation and upward drift of the set point, leading to a new body weight set point of higher maintained body weight. However, an elevated body weight set point may also be achieved without changes in the metabolic homeostasis, but rather a sustained hedonic overeating is driven by the rewarding property of palatable foods, which is primarily controlled by the mesolimbic reward system and dopamine signaling (Rui 2013). The amygdala, prefrontal cortex, and ventral striatum (including the core and shell of the nucleus accumbens) are the networks linking hedonic effect. The reward system of the brain can override homeostatic metabolic signals. These two different response systems are heavily entangled (Murray et al. 2014). Therefore, research laboratories continue to search the contributive factors involved in homeostatic and hedonic mechanisms related to eating behavior. The peripheral hormones leptin, ghrelin, and insulin play a major role in food reward as demonstrated in studies done in laboratory animals and humans, which show relationships between hyperphagia and neural pathways involved in reward. These results have provoked questions pertaining the possibility of addictive-like features in food consumption.
Metabolic and hedonic obesity altering the body weight set point: The hypothalamus and brain stem interacting with peripheral organs and tissues are the homeostatic regulators of the body weight set point. Chronic deviation of body weight from its original set point provokes a compensatory increase or decrease in food intake (cumulative over an extended period) and energy expenditure (both resting and non-resting) in opposite direction to restore the original body weight set point. However, metabolic obesity, as defined by Yu and colleagues (Yu et al. 2015) results from an elevation of the metabolic set point characterized by an elevated body weight which is metabolically protected as a new normal body weight set point. Hedonic consumption, on the other hand, is ruled by the reward dopamine system to gratify the need of pleasure independent of the metabolic set point. Deviation of the reward system may lead to hedonic overeating in susceptible individuals (drifty genotype) leading to continued weight gain above the metabolic set point weight (hedonic obesity). (Figure reproduced with permission from Yu et al. (2015))
Neuronal components of body weight regulation: Body weight in adulthood is influenced by changes in the environment of subsequent generations affecting the genetic and epigenetic propensity for weight gain and modern lifestyle that promotes sedentary behaviors and provides an oversupply of energy-dense foods. Figure reproduced with permission from Berthoud (2011). The brain maintains the homeostasis through a number of hormonal and neural nutrient-sensing inputs and from the environment and lifestyle through the cognitive and emotional brain
From the hedonic side, dopamine depletion drastically impairs feeding and causes starvation in animals. Metabolic hormones including ghrelin and leptin can stimulate on ventral tegmental area midbrain dopamine neurons to affect feeding. This area is the origin of mesolimbic dopamine neurons that project to the nucleus accumbens (NAc) that in turn influences behavior. Therefore, peripheral hormones affecting the hypothalamus can also affect feeding behavior via action on the midbrain circuits (Narayanan et al. 2010). One potential hub for the hedonic behavior is the lateral hypothalamus LH, also called “feeding center.” Lesion in this region suppresses eating and causes weight loss (Delgado and Anand 1953), while electrical stimulation causes insatiable feeding (Delgado and Anand 1953). The LH stimulation is rewarding and leads to self-stimulation in animals (Olds and Milner 1954). The LH is one of the evolutionary oldest parts of the brain, and groundbreaking work of physiologists and psychologists from the middle of the last century demonstrated that the hypothalamus is essential for the control of motivated behaviors. The LH integrates large amounts of information and arranges adaptive responses including energy homeostasis by receiving metabolic state information through both neural and humoral routes and having direct access to behavioral, autonomic, and endocrine effector pathways.
Optogenetic (the combination of genetics and optics to control well-defined events within specific cells of living tissue) experiments further demonstrated the critical roles of the LH in behavior (Stuber and Wise 2016) (Berthoud and Munzberg 2011). The LH receives numerous inputs from reward-processing centers such as medial prefrontal cortex (mPFC), nucleus accumbens (NAc), bed nucleus of the stria terminalis (BNST), and dorsal raphe (DR). The LH likely integrates the hedonic and metabolic signals for eating. From the metabolic side, the anorexigenic hormone leptin can suppress the reward value of palatable food (Hommel et al. 2006). The presence of ObRB in ventral tegmental area (dopamine neurons) is critical for feeding behavior providing direct evidence of peripheral metabolic signals affecting dopamine activity. On the other hand, the hunger hormone ghrelin potentiates the hedonic response (Malik et al. 2008) by favoring food consumption and enhancing the hedonic and incentive responses to food-related cues. When an excess of weight is due to elevation of the metabolic set point, energy expenditure is supposed to fall onto the standard energy mass regression line. In contrast, when a steady-state weight is above the metabolic set point due to hedonic overeating, a persistent compensatory increase in energy expenditure per unit metabolic mass may be demonstrable (Fig. 1.2). Recognition of the two types of obesity origin may trigger to more effective treatment and prevention of obesity. In humans, the hedonic consumption of high-calorie food is a major driver for obesity (Volkow and Wise 2005). Similar to drugs food activates a common dopamine brain reward circuitry. Addiction and obesity result in habits that persist and strengthen despite the threat of catastrophic consequences. Feeding above the metabolic needs and drug use habits are imprinted behavioral preferences that reinforce properties of great and repetitive rewards. Palatable sugary foods raise glucose concentration in the blood and brain, and drugs with pharmacological agents activate the same brain reward circuitry. The magnitude and duration of increases in dopamine induced by either excess of food or drugs in the nucleus accumbens to maintain the level demand are an intensive target of an investigation. While hedonic and metabolic mechanisms are working together at any given time or any given individual, derangement in either or both may lead to obesity. Therefore, it should be taken into account for the management of obesity and treatment modalities whether the target is behavioral changes in the case of hedonic obesity or those related to changes in body weight set point because of metabolic obesity. Identification of the neural bases separating these two systems at the molecular, cellular, and neuron-neuron interaction is key to understand how they are coordinated, and dysregulated, under healthy and obesogenic conditions (Yu et al. 2015).
We could argue that an energy-dense diet, high in saturated fat and sugar, should cause weight gain and increased adiposity but can be easily reversed by a more natural regimen of foods and lower calorie intake. However, it appears that these high-calorie diets, maintained long term, cause a profound change in the energy balance set point not so easy to reverse, particularly for those individuals who pass the 30 BMI mark. Diets containing long-chain saturated fats result in metabolic dysfunction with increased adiposity and body weight that are protected, so any subsequent weight loss through calorie restriction is difficult to maintain. The profound changes observed in the energy balance controlled by the hypothalamus result in the loss of central leptin and insulin sensitivity, which perpetuates the development of both obesity and peripheral insulin insensitivity. This hypothalamic dysfunction causes changes in the set point between energy intake and energy expenditure, which is protected by the brain at any cost. Continuous ingestion of an excess of high-calorie diet induces hypothalamic dysfunction, which includes an increase of oxidative stress; chronic atypical neuronal inflammation; endoplasmic reticulum (ER) stress; lipid metabolism; changes in neuronal cellular death, called apoptosis; neuronal rewiring; or neuronal and synaptic plasticity (see Chap. 4). All these hypothalamic changes induced by a high-calorie diet linked to inflammation increase the development of obesity. Although obesity is a consequence of the modern lifestyle society and other evolutionary and genetic factors, in my view, it is not a disease per se, a condition that over time leads to severe side effects including a range of metabolic diseases as depicted above. These diseases have increased in gigantic proportions in the United States and lesser degree in other countries, with no reversal despite educational programs and treatment options. These unsuccessful strategies are a consequence of a lack of knowledge about the precise pathology and etiology of metabolic disorders. Different independent studies had demonstrated that obesity has a strong genetic component when predisposed individuals are living in an obesogenic environment (Sorensen et al. 1989), signifying a potential gene-environment interaction (Speakman 2006). The most accepted model by different scientists is that obesity and its consequences are a result of a gene-environment interplay, an ancient genetic evolutionary selection to store fat efficiently that is poorly adapted to modern times. Interestingly, certain human populations are susceptible to obesity and metabolic syndrome (Caballero 2007), whereas others appear resistant to the forces inducing obesity (Beck-Nielsen 1999) (Neel 1962). Much emphasis has been placed on individuals and geographic populations suggesting that evolutionary traits play a key role in obesity and metabolic syndrome.
5 Evolutionary Traits
The high prevalence of obesity is seemingly a detrimental condition inconsistent with the evolutionary progress of all species including humans in their adaptation journey to new environments. Several early evolutionary hypotheses have been proposed to explain the development of obesity and metabolic syndrome. In 1962, James Neel introduced the first evolutionary explanation for the modern obesity epidemic that is founded on the notion that the development of diabetes or obesity is an adaptive trait incompatible with modern lifestyles. Neel’s “thrifty gene” hypothesis proposes that genes enable humans to efficiently collect and process food to store fat during periods of food abundance to save for times of food shortage. It would be advantageous for hunter-gatherer populations and childbearing women. Therefore, more obese individuals carrying the thrifty genes will better survive times of food shortage. Contrarily to this paradigm, in modern societies where the abundance of food is the norm, this genotype resulted on an incongruity between the environment in which the brain evolved and today’s environment with widespread of chronic obesity and diabetes. In that sense, this hypothesis represents a regression and inadequate in modern times as compared to our ancestors who undergone positive selection for genes that favored energy storage, a consequence of the cyclical episodes of famine and surplus after the advent of farming 10,000 years ago (Neel 1962, 1999). This hypothesis is based on the assumption that during human evolution, humans were always subjected to periods of feast and famine, favoring individuals who had more capacity for energy stores. This evolutionary trait allowed people more likely to survive and produce more offspring. In other words, evolution acted to select those genes in individuals who possessed high efficiency at storing fat during times of plenty.
However, in the modern environment, this genetic predisposition, which prepares us for a famine stage that never comes, an epidemic of obesity and diabetes with their induced maladies, made our society ill. We now know the genes determine the propensity for obesity or lack thereof. The dominance of obesity in modern human societies has two contributory components: a) an environmental change in the industrialized society that has happened around hundred years ago and a genetic predisposition that has its origins in our evolutionary history 2 million years ago. Around 70 percent of the variation among people in their amount of body fat is justified by inherited differences constructed into our genetic makeup and passed to next consecutive generations. According to the thrifty gene hypothesis, it was advantageous for early humans letting them store fat in times of plenty and survive in times of food scarcity. What could this hypothesis not explain in modern times is why isn’t everyone fat? John Speakman from Aberdeen University showed evidence that supporting the famine hypothesis has fundamental flaws, and he has come up with an alternative theory, nicknamed the “drifty gene” hypothesis or “predation release hypothesis.” To start, Speakman argues that famines weren’t a real threat before the advent of farming around 15,000 years ago. He suggests that there was not sufficient differential impact on survival of the lean and obese to cause such a powerful selective effect (most human populations have only experienced at most 100 famine events in their evolutionary history). Also, famines involve increases in total mortality that only rarely exceeded 10% of the population, and people in famines die of disease rather than starvation. He proposes that modern human distribution of obesity stems from a genetic drift in genes encoding the system that regulates metabolism controlling our body fatness. This drift may have started around 2 million years ago during the Paleolithic stage or Old Stone Age where our ancestors developed newer abilities to avoid being preyed upon, developing of cooking, encephalization, increase body size, expansion of new territory, and hunting (Table 1.1). In other words, the “drifty genotype” hypothesis argues that the prevalence of thrifty genes is not a result of positive selection for energy storage genes but, in reality, a genetic drift caused by the removal of predatory selection pressures.
To further counterbalance the long-held acceptance of the thrifty genotype hypothesis proposed by Neel as the most reliable model for the genetic basis of obesity, John Speakman in 2008 introduced the “drifty phenotype” or predation release hypothesis. For this interpretation in opposition to being selected for, obesogenic energy-efficient genes favoring fat storage are present in Western populations because early hominids removed the selection pressure previously exerted on them by predation. The concept of Speakman is that around 2 million years ago, the ancient ancestors, Homo habilis and Homo erectus, evolved to acquire the capability of using fire and stone tools, building weapons, and organizing social communities. For the first time in evolutionary history, an animal that was not the top predator in its ecosystem was able to remove the threat of predatory danger (Speakman 2008). This hypothesis then suggests that vital genes involved in the evasion of predators that include athletic fitness, speed, agility, stamina, and leanness were no longer needed in the life of modern humans but continue to be present for all other animals (Speiser et al. 2013; Spence et al. 2013). In other words, in the absence of predation selection pressure, genes that promote energy storage and obesity were not eliminated by natural selection. In fact, they were allowed to drift in the genetic journey of human evolution explaining why the obesity pandemic in modern Western societies has developed. Both theories, thrifty and drifty genotypes, assume that the selection pressures that ancestors of modern humans living in Western societies faced were the same. However, neither theory sufficiently explained the influence of globalization and population demographic changes that started 70,000 years ago from Africa. In the face of clear evidence, ethnic variation in obesity susceptibility and related metabolic syndrome demographics also plays a role. Having said that, although both the thrifty and drifty genotype hypotheses have considerable merit and may be responsible for the genetic susceptibility to obesity, in a particular group of individuals, neither theory can conclusively explain for the contemporary obesity pandemic in industrialized countries. The additional point is that obesity is not adaptive and may never even have existed in our evolutionary past, but it is evident today as a maladaptive by-product of positive selection on some other trait. For example, obesity may result from variation in brown adipose tissue (BAT) thermogenesis (see next topic). Another view is that most mutations in the genes that predispose us to obesity are neutral or not exacerbated, but they were drifted over evolutionary time leading some individuals to be obese while others resistant to obesity.
The general concept of Neel’s hypothesis is attractive as pointed out by Andrew Prentice (Prentice 2001) where “the genetic influences on body weight are the product of natural selection from lean times” suggesting that there is no advantage of fatness that had much to do with mortality. In his example with women from Africa, he found that food scarcity influences fertility by a cessation to ovulate, while higher body weight individuals have a greater reproductive achievement. With the advent of the agricultural society, periods of plenty increased. The advantage was that while thinner individuals are more likely to die, bear fewer children, and pass their genes to the next generation, the fatter or well-fed individuals instead were able to be more successful in generating offspring. The other problem with the Neel hypothesis was that if through our evolution it was advantageous to be fat conferring a survival trait, then why the highest percentage of people in society is not obese? Is this fact suggesting that not all of us inherit the thrifty genes? To summarize these concepts, we could say that the thrifty hypothesis is based on feast or famine events giving humans the advantage of being exceptionally efficient at storing fat which were more likely to survive. On the contrary, the drifty gene hypothesis claims that fatness was not a survival advantage but rather being a disadvantage when humans no longer had to run from predators; consequently, obesity drifted into the population. Other alternative hypotheses came along to contribute or complement the thrifty and drifty genotype hypotheses. The “thrifty phenotype hypothesis,” or Barker hypothesis, addresses the insufficiencies of thrifty gene hypothesis and also explains that newborns with low birth weight and poor nutrition in the uterus are especially prone to diabetes, obesity, heart disease, and other metabolic disorders later in life even when food is abundant in adulthood (Hales and Barker 1992). Barker proposes that the developing undernourished fetus suffering from energy shortage will allocate energy away from the pancreas in favor of other tissues such as the brain. There are additional hypotheses related to the same principle: “weather forecast model” where the fetal setting predicts the quality of the childhood environment, “maternal fitness model” where fetal environment uses nutritional signals to support its metabolism with the mother’s, “intergenerational phenotypic inertia model” where intrauterine nutritional signals are related to the history of the mother, and recent ancestors through epigenetic mechanisms: “predictive adaptive response model” where fetal environment predicts adult environment (Hales and Barker 1992; Bateson 2001).
Interestingly, as we recognize that obesity is a result of gene-environment interactions and that predisposition to obesity lies predominantly in our evolutionary past, the concept that human metabolism runs on old unmodified genes and unprepared for modern eating habits is actively debated. A diet based on foraging (collecting wild plants and pursuing wild animals), which represents a diet high in proteins and low in carbohydrates, should make us of a lean phenotype; however, that premise is more complicated than a simple hunter-gatherer’s diet. Hunting and gathering were the most successful of human adaptation, occupying at least 90 percent of human history. Following the development of agriculture, which relies on agricultural societies, and domesticated species, hunter-gatherers were displaced or conquered by farming or pastoralist groups in most parts of the world. Table 1.1 summarizes dynamic transitions through human evolution (Bellisari 2008). The deleterious changes seen in our modern society are the result of the interaction between the evolutionary human biology and development of culture over the long period of human evolution. The encephalization (the tendency for a species to evolve larger brains through time involving a change of function from noncortical parts of the brain to the cortex) of humans evolved in complex genetic and physiological systems to protect against starvation and defend stored body fat. Besides, the advantage of technological development providing access to significant quantities of mass-produced high-calorie food caused an increase in consumption. The latter event associated with reduced physical effort, the decrease in physical labor, transportation devices abolishing starvation, and heavy manual work all contributed to the current state of obesity in our society.
With the arrival of the industrial and agricultural revolution, maximizing energy intake and minimizing physical effort and energy expenditure became the norm causing a dramatic decline in nutritional health. Combined with the high genetic predisposition (O’Rahilly and Farooqi 2006) and efficient metabolic system for energy accumulation, storage, and protection (Woods and Seeley 2000), the high rates of obesity became a new trend in modern society. The factors contributing to obesity in a community with unnatural access to calories and processed food are multiple and in great part due to an exacerbation of our evolutionary genes to promote survival. Genes enhancing obesity bring up an interesting observation because obesity seems to cause with time a host of negative consequences. During evolution by natural selection, all species, including humans, develop genes throughout the natural selection, which favors advantages in dealing with the environment, not disadvantages. Therefore, how is it possible for us to become an obese species if obesity is a negative trait that will threaten our survival and should have eliminated us as species? But, in modern society only 36% of the people are obese, and the rest have average weight or slightly overweight. It is important to point out that we cannot entirely compare us with a certain group of animals that accumulate body fat in amounts that would be considered obese in humans. The most typical examples are hibernating animals, which deposit large fat stores before entering hibernation, and migratory birds, which store similar stores before starting on migratory journeys. It is clear that these situations of temporary obesity, as a mechanism of survival in anticipation of a future shortfall of energy, are well established and do not cause future obesity in those animals. It will be catastrophic for hibernating animals to be unable to feed in winter and for migratory birds to be unable to feed enough before flying over oceans. A lack of genes favoring fat accumulation will exterminate these species. Therefore, primitive humans had a more complex set of evolutionary genes to contemplate survival during periods of starvation (see below).
Why understanding these evolutionary factors is important to grasp the meaning of obesity today? In part because medical research is focusing on the contribution that nutritional programming (a process through which a stimulus during a critical window of time lastingly effects following structure, function or developmental schedule of the organism) has to disease in later life. The idea of the thrifty phenotype, first proposed by Hales and Barker (1992), used in medical research today goes in opposition to the thrifty genotype model, to interpret associations between early-life experience and adult health status. However, one of the caveats in the thrifty phenotype hypothesis is that it fails to explain why plasticity is lost so early in development in species with extensive growth, maybe because developing animals cannot maintain phenotypic plasticity during growth. Allowing the preservation of maternal strategy in offspring phenotype buffered against environmental fluctuations during the most sensitive period of development ensures a logical adaptation of growth to the state of the environment. Therefore, strategies in public health oriented for improving birth weight may be more effective if they target maternal development rather than nutrition during pregnancy. In addition, based on the thrifty phenotype hypothesis, several evolutionary models proposed include (1) the weather forecast model of Bateson, (2) the maternal fitness model of Wells, (3) the intergenerational phenotypic inertia model of Kuzawa, and (4) the predictive adaptive response model (Gluckman and Hanson 2006) (Wells 2007). From all these models, the weather forecast model is widely accepted because it proposes that developing organisms respond to cues of environmental quality and that mismatches between this forecast and subsequent reality generate significant adverse effects on adult phenotype. For more reading see Gluckman’s work (2006). One of the recent hypotheses, a consequence of the progress in molecular biology, is the thrifty epigenome hypothesis that claims that there are epigenetic modifications in response to environmental conditions (Stoger 2008) susceptibly to epigenetic variations corresponding epigenotypes with the potential to be inherited across generations. Furthermore, recent evidence suggests that early prenatal or postnatal environmental changes cause permanent metabolic modifications that are in part due to epigenetic changes in essential genes and areas of the central nervous system involved in the control of energy balance. This interaction between genetic and environmental factors including nutrition, maternal health, unknown chemicals, and lifestyle during the prenatal or perinatal period has influenced the development of energy balance causing unwanted changes. In studies done in both humans and animal models, prenatal or perinatal nutritional manipulations lead to chronic metabolic alteration affecting leptin sensitivity, glucose metabolism, and in turn energy expenditure and feeding behavior. These metabolic flaws may be a result of abnormal development of appetite-regulating neuronal circuits due to perinatal programming (Contreras et al. 2013).
“Genetically unknown foods hypothesis” proposes that obesity and diabetes occur when populations are introduced to new foods that they haven’t adapted to (Baschetti 1998). That is the case when certain “new-world populations that kept to traditional dietary habits were virtually free from diabetes”; then, after they began eating some foods that are common in Europe, the disease reached epidemic proportions. This hypothesis certainly has a lot of merits, especially as in modern times, processed fatty and sugary (natural and synthetic) foods were introduced and heavily consumed in society today, a diet that does not match with our homeostatic gene repertoire for energy balance. Another group proposes that insulin resistance is believed to have evolved as an adaptation to periodic starvation, and therefore they propose a hypothesis that insulin resistance is a socio-ecological adaptation that mediates two phenotypic transitions. A reproductive strategy deals from a large number of offspring with little investment in each to a smaller number of offspring with more investment in each (Watve and Yajnik 2007).
Multiple and intricate mechanisms have evolved to control energy balance to maintain body weight. Energy intake has to match energy expenditure to keep body weight at a constant level, but also macronutrient intake must balance macronutrient oxidation. This situation of equilibrated balance seems to be predominantly difficult to achieve in individuals with low-fat oxidation, low energy expenditure, low sympathetic activity, or low levels of spontaneous physical activity. All of these factors, among many, explain the tendency of some people to gain weight. Since there is a considerable variability in weight change in different individuals as observed when energy surplus is imposed experimentally or spontaneously, recent data suggest a strong genetic influence on body weight regulation when normal physiology is subjected to an “obesogenic” environment. In the modern world, we no longer eat only when metabolically hungry; on the contrary, we frequently eat in the complete absence of appetite and in spite of having large fat reserves in our bodies. Therefore, hedonic eating that refers to the participation of cognitive, reward, and emotional factors disrupts the homeostatic model for the regulation of energy balance. Although substantial progress has been made in recognizing the metabolic signals and neural circuitry between the brain stem and hypothalamus representing the homeostatic metabolic regulator (Berthoud 2011) (Galgani and Ravussin 2008), the neural pathways located in cortico-limbic structures responsible for hedonic behavior are much less understood. Figure 1.3 depicts a brief integration of major components of body weight regulation in an obesogenic environment as described by Berthoud (2011).
6 Thermogenesis and Human Migration
Among the various physiological mechanisms, homeotherms (animals that maintain body temperature generally above of the environment at a constant level through metabolic activity) utilize the heat production to maintain body temperature in their adaptation to different environments. BAT is responsible for the thermogenic mechanisms involved in energy expenditure. BAT in mitochondria uniquely express uncoupled protein 1 (UCP1), an inner mitochondrial membrane protein that uncouples ATP synthesis from oxidative phosphorylation, liberating energy in the form of heat (Lowell and Spiegelman 2000). It is important during cold stress by producing heat using lipids and glucose as metabolic fuels. Additionally, white adipose tissue (WAT) or beige cells have also been found to exhibit a thermogenic action similar to BAT. The heat producing of uncoupling proteins in BAT mitochondria is believed to be a key driver behind the conquest of a variety of environments in mammals 65 million years ago (Oelkrug et al. 2013; Saito et al. 2008). This ability to produce and maintain heat contributed to the evolution of mammals to explore and settle in uninhabitable territories throughout the planet (Saito et al. 2008) by adjusting the thermoregulatory response to sharply different environments. The impact of BAT thermogenesis to survival was critical in a way that it probably drove mammalian placental radiation at the end of the Cretaceous. It was a global event that led to mammals displacing the dinosaurs as the dominant class of animal on earth (Oelkrug et al. 2013).
One of the latest hypotheses to explain obesity (Sellayah et al. 2014) proposes that the current obesity pandemic in industrialized countries is also a result of the differential exposure of human ancestors to environmental factors that began when humans left Africa around 70,000 years ago and then migrated through the globe by settling in varied climates. They noted that diabetes and obesity are unequally distributed among populations from different parts of the world. This striking finding is related to the fact that survival in colder parts of the world amplified genes that help preserve body temperature. A higher metabolic rate that keeps the body warm would confer some resistance to obesity. Genes adapted for warmer climates would lower the metabolic rate, burn calories at a slower pace, and make the body more inclined to accumulate fat. It is therefore proposed that genetic factors played a role in ancestral environmental exposures in a way that affected energy expenditure even in groups of peoples from heterogeneous populations. These environmental pressures caused a great selection giving an advantage of cold-adapted genes. The high basic metabolic rate was seen in arctic people (Leonard et al. 2002), intermediate in white Europeans, and lowest in African-Americans (Weyer et al. 1999; Wong et al. 1999). The obesity rates in white Europeans with similar lifestyles and caloric intake, but in different regions of Europe, were seen to have a significant disparity. For example, among Scandinavian countries, whose population’s ancestry has generations of genetic adaptation to extreme cold, some have much lower rates of obesity than the rest of Europe, despite having similar lifestyles and consuming similar calorie foods.
A summary of their demographic hypothesis is depicted in Fig. 1.4, which shows the historic human migration out of Africa 70,000 years ago (Sellayah et al. 2014). By 60,000 years ago, humans populated Central Asia, and from that location, they migrated to northeast into Siberia and Northeast Asia. In this new environment, human acquired genes for cold adaptation with a higher resting metabolic rates and thus more resistance to obesity. The second group of migrants from Central Asia moved north and west into Europe, which also forced them to acquire genes for cold adaptation, displacing the resident Neanderthals. A third group migrated into Australia and maintained genes for heat adaptation. The Aborigines in Australia from that migration then develop a low resting metabolic rate and an increased propensity for obesity and type 2 diabetes. From the Northeast of Asia, a group crossed the Bering Strait 20,000 years ago into Alaska. Some of their descendants still live in the Canadian Arctic and are highly resistant to cold with an exceptionally high resting metabolic rate. Migration through the Pacific coast to North America and Mexico encountered hotter climates and reacquired genes for heat adaptation. The Pima Indians, which are the descendants of these groups, have the highest rates of obesity and cardiovascular disease in the world. Their evolutionary cousins, the Yaghan from Tierra del Fuego whose ancestors continued the southern migration toward the Antarctic South American Cone, probably recuperated their high BAT capability producing high resting metabolic rates and a thinner phenotype. The overall concept of this hypothesis is that ethnic differences, which resulted from different migrations to cold, mild, and hot environments 70,000 years ago, produced different genetic adaptations and susceptibilities to obesity and metabolic syndrome particularly in those individuals with a low basic metabolic rate.
Historical human migration and the impact of thermogenesis: This figure depicts the impact that ancient human migration 70,000 years ago from Africa has on selection of genes for heat and cold adaptation and the consequences in the prevalence of obesity in modern society. Individuals who migrated to cold regions acquired genes for cold adaptation, conferring them higher resting metabolic rates and thus more resistance to obesity. On the contrary, individuals who migrated to warm climates have low resting metabolic rates and an increased propensity for obesity and type 2 diabetes. (Figure reproduced with permission from Sellayah et al. (2014))
7 Conclusions and Further Thoughts
To put all these hypotheses in perspective, the contributing factors causing the global obesity pandemic we are witnessing in today’s human society reside in three distinct attributes. The first one is the environmental changes that occurred through the industrial revolution and beyond. The second one is a genetic tendency that has its origins in our evolutionary traits (genetically determined characteristics). The third is lifestyle changes introducing an excess of sedentary life in the way daily work is performed in most settings. To untangle these aspects is rather complicated because of the multiple factors involved. Understanding the evolutionary mechanisms that allow for obesity to take place in human society is highly relevant to clinical and public health management of the epidemic. The thrifty genotype hypothesis posits that although the modern environment is different from the evolutionary environment, the body is still adapted to the past where it was advantageous to store fat against future food insecurity. These genes enable individuals to efficiently collect and process food to deposit fat during periods of food abundance to provide energy for periods of famine.
From the above description, we can conclude that there are several competing hypotheses for the evolutionary origins of the widespread obesity from gene to life conditions, ethnic groups, and migrations to different climates. Although in appearance some of the hypotheses appear incompatible, complementary features among them do exist. For example, the thrifty epigenome hypothesis is believed to be a link between the thrifty gene and thrifty phenotype hypotheses (Genne-Bacon 2014). The called behavioral switch hypothesis is also in some regards compatible with the thrifty family of hypotheses (Watve and Yajnik 2007). It proposes an integration of both social and physiological mechanisms into a combined theory for the evolutionary origins of insulin resistance and obesity. It argues that metabolic diseases are by-products of a socio-ecological adaptation that switches between both reproductive and socio-behavioral strategies. This hypothesis justifies the modern pandemic of metabolic diseases as based on extreme environmental incentives: population density, urbanization, social competition, caloric access, and sedentary lifestyles exaggerated broadly to a degree never before seen in human evolutionary history (Watve and Yajnik 2007). The lack of food available is an important factor in mediating the switch between reproductive and lifestyle strategies. Changes in energy balance set point are still an important evolutionary component in the behavioral switch hypothesis. Selection for thrifty genes could have been the hallmark of a predation release/freedom from selective group providing metabolic thriftiness and weight control to avoid predation. Once predator threat was eliminated because of human social progress, there was no more selection for leanness. This means that there is room for more than one hypothesis to be corrected depending upon the nature of the natural pressures of the environment. Although, in general, the thrifty gene hypothesis has been accepted as the central hypothesis, it has impacted the way research and clinical management of obesity and diabetes are conducted.
According to Sellayah and colleagues (Sellayah et al. 2014) that propose current obesity pandemic is a result of the differential exposure of the ancestors to environmental factors that began when they left Africa around 70,000 years ago and migrated through the globe, the thrifty and drifty genotype hypotheses do not answer all questions. They claim that a lack of full understanding of the genetic basis for ethnic variability could also represent an obstacle in the interpretation of susceptibility to obesity in the developed world that caused an obesity pandemic. According to this hypothesis, obesity pandemic has certainly coincided with not only an increase in unhealthy eating habits but also a bulk of immigration of various ethnicities with different BAT energy requirements of basic metabolic rate. They argue that the thrifty and drifty genotype hypotheses assume that the selection pressures faced by the ancestors living today in all countries are the same, while they argue that this is not an accurate statement. For example, the descendants of early humans who remained in Africa and those who migrated to similar environments such as Black Americans and Pacific Islanders maintained heat adaption genes. On the other hand, those groups who migrated to colder regions including Europe and Siberia such as Caucasians and Chinese acquired genes for cold adaptation. Siberians who migrated to the American continent and established in subtropical and tropical regions in North, Central, and South America lost their cold-adaptive genes and developed genes for heat adaptation. They propose that positive selection for cold adaptation provided Caucasians and East Asians such as Chinese, Japanese, and Koreans with efficient BAT and UCP1 function with higher metabolic rate and resistance to obesity. On the opposite side, Africans and South Asians, whose ancestors did not need to evolve efficient BAT and UCP1 function, have a major propensity for obesity because of their more sedentary and hypercaloric Western lifestyle. The evolutionary origins of obesity as briefly described here to explain the global obesity epidemic are still at odds with ways how scientists struggle to understand the biological, cultural, and evolutionary basis of this condition. Furthermore, a better understanding of the interaction between physical activity and the endocrine system regulating metabolism in lean and obese could potentially help the evolutionary pathways that our ancestors took and develop tools to combat this condition. Any one theory could not explain an evolutionary tendency to become obese since humans in different parts of the world experienced different evolutionary pressures, so what’s true in one population of migrants might not apply to another living in a different climate. It is important to consider that evolutionary changes can be evident in a single generation when one or more alleles from genetic variants could change. The genetics of obesity has many influences over time and not just starvation or plenty or cold or warm. Another important negative consequence of the obesity state is the endocrine disarray seen in the overall metabolism of obese individuals. Modern obese humans have many endocrine changes in the hypothalamic-pituitary-endocrine axis homeostasis including low androgen levels (hypogonadism), polycystic ovary syndrome (PCOS), reduction in GH secretion by the pituitary gland, changes in cortisol levels, and thyroid dysfunction that is frequently associated with changes in body weight and composition, body temperature, energy expenditure, adipose tissue, food intake, and glucose and lipid metabolism. All these topics are discussed in detail throughout the different chapters of this book. Besides from being a fascinating academic pursuit, understanding human evolution is exceedingly important to comprehend the health of modern humans.
Questions
-
1.
Define the changes seen in the modern human brain.
-
2.
How is obesity defined, and what does energy balance regulation mean?
-
3.
What is the difference between metabolic and hedonic behavior in the control of body weight?
-
4.
Describe the role of thermogenesis in human migration.
-
5.
Which one is the best genetic hypothesis to define obesity in the modern world?
References
Ahima, R. S. (2005). Central actions of adipocyte hormones. Trends in Endocrinology and Metabolism: TEM, 307–313.
Anton, S. C., Potts, R., & Aiello, L. C. (2014). Human evolution. Evolution of early Homo: An integrated biological perspective. Science, 1236828. https://doi.org/10.1126/science.1236828.
Astrup, A. (1999). Macronutrient balances and obesity: The role of diet and physical activity. Public Health Nutrition, 341–347.
Astrup, A., Toubro, S., Raben, A., & Skov, A. R. (1997). The role of low-fat diets and fat substitutes in body weight management: What have we learned from clinical studies? Journal of the American Dietetic Association, S82–S87.
Baschetti, R. (1998). Diabetes epidemic in newly westernized populations: Is it due to thrifty genes or to genetically unknown foods? Journal of the Royal Society of Medicine, 622–625.
Bateson, P. (2001). Fetal experience and good adult design. International Journal of Epidemiology, 928–934.
Bauer, F., Elbers, C. C., Adan, R. A., Loos, R. J., Onland-Moret, N. C., Grobbee, D. E., van Vliet-Ostaptchouk, J. V., Wijmenga, C., & van der Schouw, Y. T. (2009). Obesity genes identified in genome-wide association studies are associated with adiposity measures and potentially with nutrient-specific food preference. The American Journal of Clinical Nutrition, 951–959. https://doi.org/10.3945/ajcn.2009.27781.
Beck-Nielsen, H. (1999). General characteristics of the insulin resistance syndrome: Prevalence and heritability. European Group for the study of Insulin Resistance (EGIR) Drugs, 7–10, 75–82.
Bell, E. A., & Rolls, B. J. (2001). Energy density of foods affects energy intake across multiple levels of fat content in lean and obese women. The American Journal of Clinical Nutrition, 1010–1018.
Bellisari, A. (2008). Evolutionary origins of obesity. Obesity Reviews: An Official Journal of the International Association for the Study of Obesity, 165–180. https://doi.org/10.1111/j.1467-789X.2007.00392.x.
Berthoud, H. R. (2011). Metabolic and hedonic drives in the neural control of appetite: Who is the boss? Current Opinion in Neurobiology, 888–896. https://doi.org/10.1016/j.conb.2011.09.004.
Berthoud, H. R., & Munzberg, H. (2011). The lateral hypothalamus as integrator of metabolic and environmental needs: From electrical self-stimulation to opto-genetics. Physiology & Behavior, 29–39. https://doi.org/10.1016/j.physbeh.2011.04.051.
Caballero, B. (2007). The global epidemic of obesity: An overview. Epidemiologic Reviews, 1–5. https://doi.org/10.1093/epirev/mxm012.
Chatterjee, H. J., Ho, S. Y., Barnes, I., & Groves, C. (2009). Estimating the phylogeny and divergence times of primates using a supermatrix approach. BMC Evolutionary Biology, 259. https://doi.org/10.1186/1471-2148-9-259.
Clement, K. (2005). Genetics of human obesity. The Proceedings of the Nutrition Society, 133–142.
Contreras, C., Novelle, M. G., Leis, R., Dieguez, C., Skrede, S., & Lopez, M. (2013). Effects of neonatal programming on hypothalamic mechanisms controlling energy balance. Hormone and Metabolic Research, 935–944. https://doi.org/10.1055/s-0033-1351281.
Cooling, J., & Blundell, J. E. (2001). High-fat and low-fat phenotypes: Habitual eating of high- and low-fat foods not related to taste preference for fat. European Journal of Clinical Nutrition, 1016–1021. https://doi.org/10.1038/sj.ejcn.1601262.
Cordain, L., Eaton, S. B., Sebastian, A., Mann, N., Lindeberg, S., Watkins, B. A., O'Keefe, J. H., & Brand-Miller, J. (2005). Origins and evolution of the western diet: Health implications for the 21st century. The American Journal of Clinical Nutrition, 341–354.
de Krom, M., Bauer, F., Collier, D., Adan, R. A., & la Fleur, S. E. (2009). Genetic variation and effects on human eating behavior. Annual Review of Nutrition, 283–304. https://doi.org/10.1146/annurev-nutr-080508-141124.
Delgado, J. M., & Anand, B. K. (1953). Increase of food intake induced by electrical stimulation of the lateral hypothalamus. The American Journal of Physiology, 162–168.
DelParigi, A., Pannacciulli, N., Le, D. N., & Tataranni, P. A. (2005a). In pursuit of neural risk factors for weight gain in humans. Neurobiology of Aging, 50–55. https://doi.org/10.1016/j.neurobiolaging.2005.09.008.
DelParigi, A., Chen, K., Salbe, A. D., Reiman, E. M., & Tataranni, P. A. (2005b). Sensory experience of food and obesity: A positron emission tomography study of the brain regions affected by tasting a liquid meal after a prolonged fast. NeuroImage, 436–443. https://doi.org/10.1016/j.neuroimage.2004.08.035.
Drewnowski, A. (2003). The role of energy density. Lipids, 109–115.
Eaton, S. B. (2006). The ancestral human diet: What was it and should it be a paradigm for contemporary nutrition? The Proceedings of the Nutrition Society, 1–6.
Elias, C. F., Aschkenasi, C., Lee, C., Kelly, J., Ahima, R. S., Bjorbaek, C., Flier, J. S., Saper, C. B., & Elmquist, J. K. (1999). Leptin differentially regulates NPY and POMC neurons projecting to the lateral hypothalamic area. Neuron, 775–786.
Elmquist, J. K., Bjorbaek, C., Ahima, R. S., Flier, J. S., & Saper, C. B. (1998). Distributions of leptin receptor mRNA isoforms in the rat brain. The Journal of Comparative Neurology, 535–547.
Flier, J. S. (2004). Obesity wars: Molecular progress confronts an expanding epidemic. Cell, 337–350.
Galgani, J., & Ravussin, E. (2008). Energy metabolism, fuel selection and body weight regulation. International Journal of Obesity, (2005), S109–S119. https://doi.org/10.1038/ijo.2008.246.
Garn, S. M., & Leonard, W. R. (1989). What did our ancestors eat? Nutrition Reviews, 337–345.
Genne-Bacon, E. A. (2014). Thinking evolutionarily about obesity. The Yale Journal of Biology and Medicine, 99–112.
Gluckman, P. D., & Hanson, M. A. (2006). Evolution, development and timing of puberty. Trends in endocrinology and metabolism: TEM, 7–12. https://doi.org/10.1016/j.tem.2005.11.006.
Gonzalez, R., Sarr, M. G., Smith, C. D., Baghai, M., Kendrick, M., Szomstein, S., Rosenthal, R., & Murr, M. M. (2007). Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. Journal of the American College of Surgeons, 47–55. https://doi.org/10.1016/j.jamcollsurg.2006.09.023.
Gotoh, K., Fukagawa, K., Fukagawa, T., Noguchi, H., Kakuma, T., Sakata, T., & Yoshimatsu, H. (2005). Glucagon-like peptide-1, corticotropin-releasing hormone, and hypothalamic neuronal histamine interact in the leptin-signaling pathway to regulate feeding behavior. The FASEB Journal, 1131–1133. https://doi.org/10.1096/fj.04-2384fje.
Hales, C. N., & Barker, D. J. (1992). Type 2 (non-insulin-dependent) diabetes mellitus: The thrifty phenotype hypothesis. Diabetologia, 595–601.
Holzapfel, C., Grallert, H., Huth, C., Wahl, S., Fischer, B., Doring, A., Ruckert, I. M., Hinney, A., Hebebrand, J., Wichmann, H. E., Hauner, H., Illig, T., & Heid, I. M. (2010). Genes and lifestyle factors in obesity: Results from 12,462 subjects from MONICA/KORA. International Journal of Obesity, (2005), 1538–1545. https://doi.org/10.1038/ijo.2010.79.
Hommel, J. D., Trinko, R., Sears, R. M., Georgescu, D., Liu, Z. W., Gao, X. B., Thurmon, J. J., Marinelli, M., & DiLeone, R. J. (2006). Leptin receptor signaling in midbrain dopamine neurons regulates feeding. Neuron, 801–810. https://doi.org/10.1016/j.neuron.2006.08.023.
Isler, K., & van Schaik, C. P. (2012). Allomaternal care, life history and brain size evolution in mammals. Journal of Human Evolution, 63, 52. https://doi.org/10.1016/j.jhevol.2012.03.009.
Jensen, M. D. (2008). Role of body fat distribution and the metabolic complications of obesity. The Journal of Clinical Endocrinology and Metabolism, S57–S63. https://doi.org/10.1210/jc.2008-1585.
Keski-Rahkonen, A., Kaprio, J., Rissanen, A., Virkkunen, M., & Rose, R. J. (2003). Breakfast skipping and health-compromising behaviors in adolescents and adults. European Journal of Clinical Nutrition, 842–853. https://doi.org/10.1038/sj.ejcn.1601618.
Kim, J. G., Suyama, S., Koch, M., Jin, S., Argente-Arizon, P., Argente, J., Liu, Z. W., Zimmer, M. R., Jeong, J. K., Szigeti-Buck, K., Gao, Y., Garcia-Caceres, C., Yi, C. X., Salmaso, N., Vaccarino, F. M., Chowen, J., Diano, S., Dietrich, M. O., Tschop, M. H., & Horvath, T. L. (2014). Leptin signaling in astrocytes regulates hypothalamic neuronal circuits and feeding. Nature Neuroscience, 908–910. https://doi.org/10.1038/nn.3725.
Koch, M., Varela, L., Kim, J. G., Kim, J. D., Hernandez-Nuno, F., Simonds, S. E., Castorena, C. M., Vianna, C. R., Elmquist, J. K., Morozov, Y. M., Rakic, P., Bechmann, I., Cowley, M. A., Szigeti-Buck, K., Dietrich, M. O., Gao, X. B., Diano, S., & Horvath, T. L. (2015). Hypothalamic POMC neurons promote cannabinoid-induced feeding. Nature, 45–50. https://doi.org/10.1038/nature14260.
Leonard, W. R. (2002). Food for thought. Dietary change was a driving force in human evolution. Scientific American, 106–115.
Leonard, W. R., & Robertson, M. L. (1992). Nutritional requirements and human evolution: A bioenergetics model. American Journal of Human Biology: Official Journal of the Human Biology Council, 179–195. https://doi.org/10.1002/ajhb.1310040204.
Leonard, W. R., & Robertson, M. L. (1994). Evolutionary perspectives on human nutrition: The influence of brain and body size on diet and metabolism. American Journal of Human Biology: Official Journal of the Human Biology Council, 77–88. https://doi.org/10.1002/ajhb.1310060111.
Leonard, W. R., Sorensen, M. V., Galloway, V. A., Spencer, G. J., Mosher, M. J., Osipova, L., & Spitsyn, V. A. (2002). Climatic influences on basal metabolic rates among circumpolar populations. American Journal of Human Biology: The Official Journal of the Human Biology Council, 609–620. https://doi.org/10.1002/ajhb.10072.
Leonard, W. R., Snodgrass, J. J., & Robertson, M. L. (2007). Effects of brain evolution on human nutrition and metabolism. Annual Review of Nutrition, 27, 311. https://doi.org/10.1146/annurev.nutr.27.061406.093659.
Lowell, B. B., & Spiegelman, B. M. (2000). Towards a molecular understanding of adaptive thermogenesis. Nature, 652–660. https://doi.org/10.1038/35007527.
Ludwig, D. S., Tritos, N. A., Mastaitis, J. W., Kulkarni, R., Kokkotou, E., Elmquist, J., Lowell, B., Flier, J. S., & Maratos-Flier, E. (2001). Melanin-concentrating hormone overexpression in transgenic mice leads to obesity and insulin resistance. The Journal of Clinical Investigation, 379–386. https://doi.org/10.1172/JCI10660.
Malik, S., McGlone, F., Bedrossian, D., & Dagher, A. (2008). Ghrelin modulates brain activity in areas that control appetitive behavior. Cell Metabolism, 400–409. https://doi.org/10.1016/j.cmet.2008.03.007.
Murray, S., Tulloch, A., Gold, M. S., & Avena, N. M. (2014). Hormonal and neural mechanisms of food reward, eating behaviour and obesity. Nature Reviews Endocrinology, 540–552. https://doi.org/10.1038/nrendo.2014.91.
Narayanan, N. S., Guarnieri, D. J., & DiLeone, R. J. (2010). Metabolic hormones, dopamine circuits, and feeding. Frontiers in Neuroendocrinology, 104–112. https://doi.org/10.1016/j.yfrne.2009.10.004.
Neel, J. V. (1962). Diabetes mellitus: A "thrifty" genotype rendered detrimental by "progress"? American Journal of Human Genetics, 353–362.
Neel, J. V. (1999). The "thrifty genotype" in 1998. Nutrition Reviews, S2–S9.
Nillni, E. A. (2010). Regulation of the hypothalamic thyrotropin releasing hormone (TRH) neuron by neuronal and peripheral inputs. Frontiers in Neuroendocrinology, 134–156. doi: S0091-3022(10)00002-6 [pii]. https://doi.org/10.1016/j.yfrne.2010.01.001.
Nillni, E. A., & Sevarino, K. A. (1999). The biology of pro-thyrotropin-releasing hormone-derived peptides. Endocrine Reviews, 599–648.
Obesity: preventing and managing the global epidemic. (2000). Report of a WHO consultation. World Health Organization technical report series:i–xii, 1–253.
Oelkrug, R., Goetze, N., Exner, C., Lee, Y., Ganjam, G. K., Kutschke, M., Muller, S., Stohr, S., Tschop, M. H., Crichton, P. G., Heldmaier, G., Jastroch, M., & Meyer, C. W. (2013). Brown fat in a protoendothermic mammal fuels eutherian evolution. Nature Communications, 2140. https://doi.org/10.1038/ncomms3140.
Olds, J., & Milner, P. (1954). Positive reinforcement produced by electrical stimulation of septal area and other regions of rat brain. Journal of Comparative and Physiological Psychology, 419–427.
O'Rahilly, S., & Farooqi, I. S. (2006). Genetics of obesity. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 1095–1105. https://doi.org/10.1098/rstb.2006.1850.
Perello, M., Stuart, R. C., & Nillni, E. A. (2006). The role of intracerebroventricular administration of leptin in the stimulation of prothyrotropin releasing hormone neurons in the hypothalamic paraventricular nucleus. Endocrinology, 3296–3306.
Pomp, D., & Mohlke, K. L. (2008). Obesity genes: So close and yet so far. Journal of Biology, 36. https://doi.org/10.1186/jbiol93.
Pontzer, H., Brown, M. H., Raichlen, D. A., Dunsworth, H., Hare, B., Walker, K., Luke, A., Dugas, L. R., Durazo-Arvizu, R., Schoeller, D., Plange-Rhule, J., Bovet, P., Forrester, T. E., Lambert, E. V., Thompson, M. E., Shumaker, R. W., & Ross, S. R. (2016a). Metabolic acceleration and the evolution of human brain size and life history. Nature, 390–392. https://doi.org/10.1038/nature17654.
Pontzer, H., Durazo-Arvizu, R., Dugas, L. R., Plange-Rhule, J., Bovet, P., Forrester, T. E., Lambert, E. V., Cooper, R. S., Schoeller, D. A., & Luke, A. (2016b). Constrained total energy expenditure and metabolic adaptation to physical activity in adult humans. Current Biology, 410–417. https://doi.org/10.1016/j.cub.2015.12.046.
Prentice, A. M. (2001). Obesity and its potential mechanistic basis. British Medical Bulletin, 51–67.
Rui, L. (2013). Brain regulation of energy balance and body weight. Reviews in Endocrine & Metabolic Disorders, 387–407. https://doi.org/10.1007/s11154-013-9261-9.
Saito, S., Saito, C. T., & Shingai, R. (2008). Adaptive evolution of the uncoupling protein 1 gene contributed to the acquisition of novel nonshivering thermogenesis in ancestral eutherian mammals. Gene, 37–44. https://doi.org/10.1016/j.gene.2007.10.018.
Sanchez, V. C., Goldstein, J., Stuart, R. C., Hovanesian, V., Huo, L., Munzberg, H., Friedman, T. C., Bjorbaek, C., & Nillni, E. A. (2004). Regulation of hypothalamic prohormone convertases 1 and 2 and effects on processing of prothyrotropin-releasing hormone. The Journal of Clinical Investigation, 357–369.
Saper, C. B., Chou, T. C., & Elmquist, J. K. (2002). The need to feed: Homeostatic and hedonic control of eating. Neuron, 199–211.
Schuppli, C., Isler, K., & van Schaik, C. P. (2012). How to explain the unusually late age at skill competence among humans. Journal of Human Evolution, 843–850. https://doi.org/10.1016/j.jhevol.2012.08.009.
Sellayah, D., Cagampang, F. R., & Cox, R. D. (2014). On the evolutionary origins of obesity: A new hypothesis. Endocrinology, 1573–1588. https://doi.org/10.1210/en.2013-2103.
Sorensen, T. I., Price, R. A., Stunkard, A. J., & Schulsinger, F. (1989). Genetics of obesity in adult adoptees and their biological siblings. BMJ, 87–90.
Speakman, J. R. (2006). Thrifty genes for obesity and the metabolic syndrome--time to call off the search? Diabetes & Vascular Disease Research, 7–11. https://doi.org/10.3132/dvdr.2006.010.
Speakman, J. R. (2008). Thrifty genes for obesity, an attractive but flawed idea, and an alternative perspective: The 'drifty gene' hypothesis. International Journal of Obesity, (2005), 1611–1617. https://doi.org/10.1038/ijo.2008.161.
Speiser, D. I., Lampe, R. I., Lovdahl, V. R., Carrillo-Zazueta, B., Rivera, A. S., & Oakley, T. H. (2013). Evasion of predators contributes to the maintenance of male eyes in sexually dimorphic Euphilomedes ostracods (Crustacea). Integrative and Comparative Biology, 78–88. https://doi.org/10.1093/icb/ict025.
Spence, R., Wootton, R. J., Barber, I., Przybylski, M., & Smith, C. (2013). Ecological causes of morphological evolution in the three-spined stickleback. Ecology and Evolution, 1717–1726. https://doi.org/10.1002/ece3.581.
Stoger, R. (2008). The thrifty epigenotype: An acquired and heritable predisposition for obesity and diabetes? BioEssays: News and Reviews in Molecular, Cellular and Developmental Biology, 156–166. https://doi.org/10.1002/bies.20700.
Stuber, G. D., & Wise, R. A. (2016). Lateral hypothalamic circuits for feeding and reward. Nature Neuroscience, 198–205. https://doi.org/10.1038/nn.4220.
Stunkard, A. J., Berkowitz, R. I., Stallings, V. A., & Schoeller, D. A. (1999). Energy intake, not energy output, is a determinant of body size in infants. The American Journal of Clinical Nutrition, 524–530.
Tataranni, P. A., Harper, I. T., Snitker, S., Del Parigi, A., Vozarova, B., Bunt, J., Bogardus, C., & Ravussin, E. (2003). Body weight gain in free-living pima Indians: Effect of energy intake vs expenditure. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity, 1578–1583. https://doi.org/10.1038/sj.ijo.0802469.
van Schaik, C. P., Isler, K., & Burkart, J. M. (2012). Explaining brain size variation: From social to cultural brain. Trends in Cognitive Sciences, 277–284. https://doi.org/10.1016/j.tics.2012.04.004.
van Woerden, J. T., Willems, E. P., van Schaik, C. P., & Isler, K. (2012). Large brains buffer energetic effects of seasonal habitats in catarrhine primates. Evolution: International Journal of Organic Evolution, 191–199. https://doi.org/10.1111/j.1558-5646.2011.01434.x.
Volkow, N. D., & Wise, R. A. (2005). How can drug addiction help us understand obesity? Nature Neuroscience, 555–560. https://doi.org/10.1038/nn1452.
Waterson, M. J., & Horvath, T. L. (2015). Neuronal regulation of energy homeostasis: Beyond the hypothalamus and feeding. Cell Metabolism, 962–970. https://doi.org/10.1016/j.cmet.2015.09.026.
Watve, M. G., & Yajnik, C. S. (2007). Evolutionary origins of insulin resistance: A behavioral switch hypothesis. BMC Evolutionary Biology, 61. https://doi.org/10.1186/1471-2148-7-61.
Wells, J. C. (2007). Environmental quality, developmental plasticity and the thrifty phenotype: A review of evolutionary models. Evolutionary Bioinformatics Online, 109–120.
Weyer, C., Snitker, S., Bogardus, C., & Ravussin, E. (1999). Energy metabolism in African Americans: Potential risk factors for obesity. The American Journal of Clinical Nutrition, 13–20.
Willett, W. C., & Leibel, R. L. (2002). Dietary fat is not a major determinant of body fat. The American Journal of Medicine, 47S–59S.
Wong, W. W., Butte, N. F., Ellis, K. J., Hergenroeder, A. C., Hill, R. B., Stuff, J. E., & Smith, E. O. (1999). Pubertal African-American girls expend less energy at rest and during physical activity than Caucasian girls. The Journal of Clinical Endocrinology and Metabolism, 906–911. https://doi.org/10.1210/jcem.84.3.5517.
Woods, S. C., & Seeley, R. J. (2000). Adiposity signals and the control of energy homeostasis. Nutrition, 894–902.
Yu, Y. H., Vasselli, J. R., Zhang, Y., Mechanick, J. I., Korner, J., & Peterli, R. (2015). Metabolic vs. hedonic obesity: A conceptual distinction and its clinical implications. Obesity Reviews : An Official Journal of the International Association for the Study of Obesity, 234–247. https://doi.org/10.1111/obr.12246.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Nillni, E.A. (2018). The Evolution from Lean to Obese State and the Influence of Modern Human Society. In: Nillni, E. (eds) Textbook of Energy Balance, Neuropeptide Hormones, and Neuroendocrine Function. Springer, Cham. https://doi.org/10.1007/978-3-319-89506-2_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-89506-2_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-89505-5
Online ISBN: 978-3-319-89506-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)