Abstract
Rheumatoid arthritis (RA) is a chronic inflammatory disease associated with both environmental and genetic factors but of unknown cause. There are >100 associated gene loci, the most significant of which is HLA-DRB1 in the major histocompatibility complex region. Recent work has also highlighted important roles of the human mucosal microbiota, at both the gingival as well as the intestinal surfaces. Periodontal disease and alterations in the gingival microbiota, including overgrowth of Porphyromonas gingivalis, are associated with RA. A key hallmark of RA is serum anti-citrullinated protein antibodies reactive against a variety of posttranslationally citrullinated proteins, which are enriched in RA, particularly in patients with HLA-DRB1 risk alleles. Citrullination of arginine residues is catalyzed by peptidylarginine deiminases (PADs). Of note, P. gingivalis produces its own PAD enzyme (PPAD), which may contribute to the citrullination of native proteins. Differences in the intestinal microbiota, particularly overgrowth of Prevotella copri, are associated with early RA, perhaps compensating for the absence of HLA-DRB1 risk alleles in some patients. As the role of the microbiota in RA is elucidated, targeted interventions to manipulate the microbiome to prevent or treat RA may emerge.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The concept that rheumatoid arthritis (RA) could be mediated by infections is more than 100 years old, since Bailey suggested that the disease was likely mediated by bacterial toxins and indicated that the offending bacterium may reside in the gastrointestinal tract [1]. Indeed, the RA infection theory was the rationale for the development of sulfasalazine in the 1940s [2] as well as for several of the early trials evaluating antibiotics as a therapeutic tool (Table 15.1). Over the ensuing decades, the concept that RA was mediated by infections largely fell out of favor, because no single organism was clearly identified using candidate organism approaches. The pendulum has swung back. Beginning with the study by Vaahtovuo et al. [3], multiple investigators have used culture-independent technology to query mucosal populations at several different body surfaces, finding abnormalities that in many cases have been remarkably consistent and which lead to the conclusion that the oral and enteric microbiota predispose to the development of RA and the formation of its hallmark antibody, anti-cyclic citrullinated peptide antibodies (ACPAs).
Fecal Microbiota in RA
Multiple studies have evaluated the contents of the fecal microbiota in RA (Table 15.2). There is substantial heterogeneity in the published studies, primarily in the methodology used to identify the bacteria, the geographic location of the subjects, the use of immunomodulatory medications in the RA patients, and the source of the controls. The first three studies to evaluate the microbiota as a whole used fecal culture followed by various analytic techniques to identify anaerobic and aerobic organisms, as well as to identify a limited number of specific organisms through traditional methods [4,5,6]. These studies were limited in their ability to identify the vast majority of the bacteria present in the intestinal tract, and not surprisingly, few differences emerged. Shinebaum [4] reported increased C. perfringens in RA patients, a finding that was subsequently thought to be secondary to the use of nonsteroidal anti-inflammatory drugs (NSAIDs) on the basis of the observation that RA patients and osteoarthritis (OA) patients on NSAIDs had similar burden of this organism and both patient populations had a higher abundance of C. perfringens as compared to OA patients not taking NSAIDs [6]. Severijnen reported higher frequency of what was termed “coccoid rods” in RA patients [5]. None of these studies identified any bacteria that were lower in patients.
Although still widely used in clinical medicine, culture is a suboptimal modality to differentiate all of the components of a complex community of bacteria. It is generally cited that only about 20% of intestinal bacteria can be cultured [7]. Although the number may in fact be higher [8], culture and identification is nevertheless a highly labor-intensive approach; it has been estimated that to culture and identify the fecal community of bacteria would take about one person-year of laboratory effort [9]. In contrast, the process of sequencing of 16S ribosomal DNA and its analysis can be completed in a few days.
Thus, as the technology became available, genetic tools were used to compare the fecal microbiota of RA patients and controls. The first such study to do so was published by Vaahtovuo et al. [3]. This study was nevertheless limited by the use of specific genetic probes, rather than pan-bacterial markers that have since become state of the art. In addition, this early study was possibly limited by the use of patients with fibromyalgia as controls, as it has not been established whether their microbiota is representative of healthy adults. They observed four probe sets of bacteria to be reduced in RA ([1] Bacteroides/Porphyromonas/Prevotella, [2] B. fragilis, [3] Bifidobacterium, [4] Eubacterium rectale–Clostridium coccoides group) and did not identify any elevated probes. Today, we recognize that inclusion of both Bacteroides and Prevotella in a single probe set is a limitation, as these two genera constitute two distinct enterotypes, which tend to be inversely correlated with one another [10].
All subsequent studies used either sequencing of the 16S ribosomal DNA, whole-genome sequencing, or a combination of these approaches. As discussed elsewhere (Chap. 3), these approaches constitute far more comprehensive and relatively unbiased approaches to query the microbiota. The first of these metagenomics studies was the groundbreaking work published by Scher and colleagues in 2013 evaluating populations of subjects with new-onset RA (NORA ), long-standing or chronic RA (CRA), and healthy controls (HC) [11]. This study also included subjects with psoriatic arthritis, which is the topic of a different chapter (Chap. 18). One of the key findings was a striking increase in the abundance of a single organism, Prevotella copri , which had a fecal abundance upwards of 50% in some subjects and greater than 5% in 33/44 (75%) of NORA subjects compared to 6/28 (21%) of HC. Fecal carriage of P. copri was higher in RA patients without versus with the shared epitope (SE), a 5 amino acid sequence motif in residues 70–74 of the HLA-DRβ chain (QKRAA, QRRAA, or RRRAA) that is the genetic factor that confers the highest risk for RA susceptibility [12]. This latter finding suggests that the abundance of P. copri above a certain threshold may be needed to overcome the lack of genetic predisposition to RA. Interestingly, the abundance of P. copri in subjects with CRA was similar to that of healthy controls.
A subsequent study of NORA patients likewise suggested a role for intestinal P. copri in the etiopathogenesis of RA. Maeda et al. studied 17 subjects with NORA and 14 HC [13]. Principal component analysis of the sequencing of the 16S rDNA identified four clusters. One dominated by Prevotella was comprised only of RA patients. Most of the Prevotella sequences aligned closely with P. copri, and patients in the Prevotella cluster had elevated inflammatory markers when compared to patients in the remaining clusters.
A Chinese study of NORA patients did not identify significant differences in the abundance of fecal P. copri between patients and controls, indicating that geographic differences in genetics and diet likely also play important roles in determining microbial contributions to arthritis. In this study, 94 NORA patients and 80 HC underwent metagenomic shotgun sequencing. Taxa abundant in RA patients included Eggerthella lenta and Clostridium asparagiforme, while those abundant in controls included Klebsiella pneumoniae, Megamonas hypermegale, Sutterella wadsworthensis, and Bifidobacterium bifidum. Longitudinal evaluation of treated RA participants showed that baseline levels of some bacteria, particularly those containing certain virulence factors, were predictive of response to therapy. Using repeat specimens from 40 patients following initiation of therapy, the authors showed that changes in the gut microbiota did not correlate very well with response to therapy.
A North American study of CRA patients showed RA patients to be deficient in fecal Faecalibacterium prausnitzii and abundant for rare bacteria within the Actinobacteria phylum, primarily Collinsella and Eggerthella [14]. The latter finding is consistent with the study by Zhang et al. [15]. As discussed elsewhere (Chap. 19) in this textbook, F. prausnitzii has been shown to be decreased in adult and pediatric patients with inflammatory bowel disease [16], as well as in children with enthesitis-related arthritis [17, 18]. Its role in arthritis has been attributed to a variety of potential factors, such as its effects of development of regulatory T cells [19] and on the health of the enterocytes [20].
In summary, multiple studies have evaluated the fecal microbiota in RA patients. All of the studies that used sequencing methods to identify bacteria have identified substantial differences between RA patients and controls. Moreover, two of them, despite geographic heterogeneity, demonstrated depletion of Bacteroides [3, 11] and two showed increased abundance of P. copri [11, 13], findings which have not been observed in patients with CRA [11, 14]. The only exception to these general findings was a study conducted in China, in which Bacteroides was enriched in RA patients [15]. Additional commonalities described in this body of work include that two of these studies demonstrated expansion of a rare genus called Eggerthella [14, 15]. Finally, both studies that reported on the within-group (alpha) diversity of the samples demonstrated decreased diversity in RA patients, although in one of these studies, this finding was dependent upon the metric used [11, 14].
Several studies provided mechanisms by which the associated bacteria may predispose to arthritis. For example, one of the findings by Chen et al. was that a rare genus within the Actinobacteria phylum, Collinsella , was enriched in RA patients [14]. As part of the study, the authors introduced this organism into the collagen-induced arthritis model, finding that addition of Collinsella increased the frequency albeit not the severity of arthritis. They also found that mouse dendritic cells (DC) pre-cultured with Collinsella demonstrated more robust responses to collagen as compared to DC not cultured with Collinsella and that Collinsella increased the permeability of the CACO-2 intestinal cell line. Taken together, they proposed that a combination of decreased Faecalibacterium and increased Collinsella resulted in increased intestinal permeability, potentially permitting microbial components to enter the lamina propria and trigger dysfunctional immunity. Likewise, Scher et al. demonstrated that colonization of antibiotic-depleted mice with P. copri , the most abundant organism in their study, resulted in increased colitis induced by dextran sulfate [11]. Maeda et al. used fecal transplant to test the ability of Prevotella to induce arthritis in SKG mice injected with zymosan, finding that microbiota containing Prevotella were associated with the development of arthritis while microbiota lacking Prevotella—whether derived from RA patients or healthy controls—did not [13]. The Prevotella-exposed mice also had increased numbers of CD4+ and CD4 + IL-17+ T cells in the large intestine, and T cells derived from regional lymph nodes in these mice showed enhanced Th17 responses compared to T cells derived from mice exposed to control microbiota.
Thus, studies of the fecal microbiota in RA patients indicate expansion of P. copri in NORA patients and also show in animal systems that P. copri is pro-inflammatory and immunogenic. Pianta et al. demonstrated that P. copri is immunogenic in humans as well [21]. They used liquid chromatography mass spectroscopy to identify the peptidome from HLA-DR+ antigen-presenting cells. Among them was a peptide that matched to a portion of a 27-kD protein from P. copri (Pc-p27). Production of interferon-gamma following in vitro exposure to this peptide was observed in T cells from 17/40 (42%) of RA patients compared to 0/15 healthy controls and 0/10 patients with Lyme arthritis. Likewise, RA patients demonstrated increased levels of IgA antibodies against both the peptide and whole bacteria, with the levels of these antibodies correlating with those of inflammatory cytokines. Thus, P. copri is not only abundant in NORA but also appears to trigger mucosal immune reactions.
While there is compelling evidence that P. copri is likely involved in the initiation of RA, there are still multiple unanswered questions. It is not known what drives the expansion of Prevotella, nor what factors cause it evidently to return to normal in patients with long-standing disease. Would prevention of this expansion of P. copri be able to prevent this disease from starting, and would eradication of P. copri be a therapeutic option? The latter seems unlikely, in light of the absence of any studies showing expansion of this organism in patients with long-standing disease. Additionally, if P. copri induces mucosal immunity and inflammation, as the study by Scher suggested [11], why is subclinical gut inflammation a rare finding in patients with RA, as compared to patients with spondyloarthritis [22, 23]?
Periodontal Disease and Associated Microbiota in RA
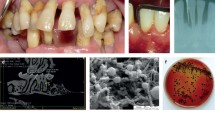
The gut is not the only habitat that has been associated with RA; the oral microbiota may also play an important role in the disease, particularly in the context of periodontal disease (PD). PD is fundamentally an infectious and inflammatory process [24, 25]. An early step in the initiation of PD is the development of a biofilm consisting of oral bacteria. This biofilm permits the expansion of pathogenic organisms, such as Porphyromonas gingivalis , that are not ordinarily present on the gingival surface in significant quantities [25]. P. gingivalis is a gram-negative anaerobic coccobacillus that can both elude host immune responses and cause local tissue destruction [25]. Deep sequencing of the gingival microbiota revealed that P. gingivalis is only present in subjects with PD, even among RA patients [26]. The host responds to the microbial challenge by generating an immunologic response, consisting of various innate and adaptive mediators of inflammation. This results in plaque formation and local gingival inflammation. As this progresses, the connective tissue attachment to the tooth is damaged, followed by the development of bone destruction [24]. Treatment of periodontitis typically consists of a procedure called scaling and root planning (SRP ), which consists of physical removal of the plaque, which is the nidus of the inflammatory process [27].
There is abundant epidemiologic evidence of an association between RA and PD [26, 28,29,30,31]. For example, a cross-sectional study conducted through the National Health and Nutrition Examination Survey III consisting of 4461 North American participants showed that RA patients were more likely to have PD compared to those without RA (OR 1.82 following adjustment for multiple potential confounders, including smoking status, 95% CI 1.04–3.20) [28]. Likewise, a cross-sectional study of 852 non-smoking adults in India referred for periodontal evaluation showed an incidence of RA of 4.4%, compared to 1% in the general population [29]. Small studies have found such an association as well [26, 30, 31], including those that were limited to patients with newly diagnosed disease [26, 31].
There are many potential explanations for this association. One potential association is that this reflects confounding by cigarette smoking. That is, cigarette smoking is a well-known risk factor for RA [32] and is also a risk factor for PD [33], so the association between RA and PD could potentially reflect confounding by the shared risk factor of cigarette smoking. Arguing against this possibility is that the large studies discussed above took smoking into account, either through statistical adjustment [28] or by excluding smokers [29], yet the association holds. Furthermore, as discussed below, it is plausible that cigarette smoking is not simply a shared risk factor for PD and RA, but drives the increased risk of RA through the intermediary of PD.
Another potential mechanism accounting for the association between PD and RA is the possibility that oral microbiota might end up in the synovium, triggering a local inflammatory process. For example, Reichert et al. found genetic material from P. gingivalis in the synovium of 7/42 (16.7%) of RA patients vs 4/114 (3.5%) of HC, p = 0.009 [34]. However, this does not appear to be a specific finding, as similar organisms were also observed in the synovium of subjects with OA [35], and others have found that bacterial DNA as a whole is present in subjects with a variety of disorders [36,37,38,39]. It was suggested that this finding reflects non-specific trapping of killed bacteria by inflamed joints [40].
A third potential mechanism is that the arthritic process , and its therapy, may contribute to PD. That is, the immunosuppressive therapy of RA might predispose to the bacterial overgrowth that defines PD, or the decreased mobility of the hand and wrist resulting from the disease process in RA could impair oral hygiene, thus contributing to PD. This explanation would not entirely account for the findings of severe PD in patients with NORA [26, 31], nor for data showing that antibodies again P. gingivalis develop prior to the development of symptoms associated with RA [41]. More importantly, the possibility that active RA results in PD would not account for the findings reported in several prospective studies, in which periodontal therapy consisting of SRP has been shown to be therapeutic for RA [42,43,44,45]. In open-label studies, Erciyas et al. reported improved Disease Activity Score (DAS) levels and inflammatory markers among 60 subjects with mild or moderate RA who underwent SRP [42]; Biyikoglu et al. reported improved DAS and inflammatory markers among the 10 of 15 RA patients who underwent SRP and completed the study [43]; and Ribeiro et al. observed improved ESR among 22 subjects with RA who underwent SRP, but not in a parallel albeit not evidently randomized group of 16 subjects who underwent dental cleaning alone [44]. Although these open-label studies were not without biases in their design and analysis, similar findings were reported in a randomized study published by Ortiz et al. [45]. In this study, 40 subjects with active RA on stable therapy and severe PD were randomized to receive treatment for the latter versus no additional care, stratifying for baseline use of tumor necrosis factor inhibitor (TNFi) therapy in 20 of the subjects. They found substantial improvements in multiple clinical and laboratory markers of RA regardless of background TNFi use in the SRP arm.
A fourth potential mechanism accounting for the link between PD and RA is that as PD is an inflammatory process, PD and RA may reflect similar immunoregulatory environments that therefore might tend to co-occur in the same population, not unlike the associations between spondyloarthritis and inflammatory bowel disease or psoriasis. This possibility is supported by shared genetics between RA and PD, particularly among HLA-DRB1 alleles containing the SE [46]. There are multiple schema for classifying HLA-DRB1 risk alleles in RA but studies have largely shifted to analysis of amino acid residues rather than alleles. Amino acid residues encoded at positions 11, 71, and 74 in HLA-DRB1 are thought to be most important in RA risk [47]. To our knowledge, the association between PD and the SE at the amino acid level has yet to be explored. Additional evidence for shared pathophysiologic mechanisms between RA and PD includes other genetic susceptibility factors [48], as well as findings that inflammation in periodontal tissue is mediated at least in part by cytokines such as interleukin (IL)-1, IL-6, and TNF, that have become therapeutic targets in RA [49]. However, the possibility that these shared mechanisms account for the association between PD and RA ultimately fail to account for the findings discussed above that treatment of PD results in improved clinical parameters in RA.
A fifth mechanism is that P. gingivalis may itself be the target of the immune system in RA. Several studies in patients with RA have shown elevated IgG antibodies directed against P. gingivalis [50,51,52,53,54]. However, other studies have reported contradictory findings [26, 55, 56], and the presence of these antibodies may reflect that this organism is present in the context of an inflammatory milieu without necessarily being pathogenic. Thus, although it is certainly plausible that there may be heterogeneity in the disease, with such antibodies contributing to the disease process in a subset of patients, the role of these antibodies in the pathogenesis of RA requires further study.
Finally, the association between PD and RA may be mediated by P. gingivalis, (the “2-hit” model of RA pathogenesis). According to this model, P. gingivalis contributes to RA through citrullination of proteins via its peptidylarginine deiminase (PAD) enzyme , resulting in the development of ACPAs [57]. ACPAs serve as diagnostic markers for RA, and third-generation ACPA assays have sensitivity ranging from 61.3 to 82.9 and specificity ranging from 93 to 97.6 for the diagnosis of RA [58]. Human proteins are not typically citrullinated. However, the PAD enzyme in humans and P. gingivalis converts the amino acid arginine into citrulline residues. Humans encode five PAD isotypes (PAD1-PAD4, and PAD6), of which PAD2 and PAD4 have been found in the synovial tissue and fluid of persons with RA, which may be a site where the citrullination occurs [59,60,61]. The significance of PAD in RA is underscored by studies showing that the PAD4 locus is associated with a ~ 2-fold risk of RA in a variety of populations [62,63,64,65]. P. gingivalis carries its own version of PAD (known as P. gingivalis PAD, or PPAD), possibly the only bacterial species that does so [66]. PPAD is capable of citrullinating human proteins [57]. There are several lines of evidence that this citrullination process may be directly pathogenic for the disease, rather than a bystander phenomenon. One is that in the collagen-induced arthritis model of RA, infection with P. gingivalis results in earlier onset and increased severity of the disease, findings that are abrogated if the P. gingivalis lacks PPAD [67]. Also, in the same model, tolerization with citrulline-containing peptides prior to induction of arthritis resulted in less disease severity and lower production of anti-CCP antibodies [68]. It is therefore of particular interest that cigarette smoking is associated only with anti-CCP+ RA [32], consistent with the possibility that cigarette smoking contributes to RA by inducing periodontitis. Of note, this association between P. gingivalis and RA may be limited to CCP+ disease, which is strongly associated with the major histocompatibility complex, particularly the SE [69, 70]. In contrast, P. copri appears to be more strongly linked to RA patients lacking the SE [11], who are often CCP-. Thus, the pathophysiology of these two subsets of RA may be different, which clearly could have implications with respect to diagnosis and treatment.
To summarize, multiple explanations for the association between PD and RA have been proposed. The model that arguably is best supported by the data is that PD is mediated in large part by a limited set of organisms, one of which is P. gingivalis . This species has the unique capacity to citrullinate human proteins , which when modified are targeted by the immune system to form ACPAs, the hallmark antibody of RA. Cigarette smoking may play into this association largely by increasing the risk of PD, thus accounting for its association with anti-CCP+, but not anti-CCP-, RA. The most important clinical implication of this theory is that treatment of PD appears to result in improvement in the RA disease process. This model is shown in Fig. 15.1.
Overgrowth of pathogenic bacteria such as P. gingivalis (red) occurs in the gingiva, resulting in inflamed tissue. This bacterial overgrowth is associated with expression of PPAD, which converts the amino acid arginine into citrulline. Antibodies against citrulline (anti-CCPs) then deposit in synovial tissue, resulting in arthritis
Additional Microbiomes in RA
As detailed above, much of the literature on the microbiota in RA has centered on the enteric or gingival microbiota . One other habitat that may be relevant is the lung. Interstitial lung disease is common in RA patients [71], indicating that the lungs may be a source of inflammation. Perhaps due to relative inaccessibility, the microbiota of the lungs has not been studied extensively. Recently, Scher and colleagues performed bronchial alveolar lavage on 20 patients with NORA, 12 healthy controls, and 10 patients with sarcoidosis [72]. The RA patients demonstrated decreased alpha diversity and depletion of several families, such as Burkholderiaceae, Actinomycetaceae, and Spirochaetaceae. However, similar findings were seen in the patients with sarcoidosis, and principal coordinates analysis showed that the sarcoidosis and RA patients clustered together, apart from the controls. Thus, Scher concluded that these findings may reflect an inflammatory lung, rather than a specific RA, phenotype. This stands in contrast to the gut microbiota studies, where several of the findings—particularly the outgrowth of P. copri—appear to be unique to RA [11].
One final habitat that was evaluated in a single study is the salivary microbiota . Note that these results cannot be compared with those of the gingival microbiota, as these are two fairly distinct habitats [73]. Counterintuitively, Zhang et al. found P. gingivalis among multiple other organisms to be depleted in the saliva of NORA patients, while several species of Prevotella were elevated in the RA saliva [15]. Interestingly, the same study also found several species of Prevotella to be elevated in the control gingival plaques. Partial normalization of the oral microbiota was observed following introduction of immunosuppressive therapy.
Therapeutic Alterations of the Microbiota
Antibiotics
There have been numerous controlled studies of antibiotics as potential therapeutic agents in RA. As summarized in Table 15.1, this benefit was seen in multiple different classes of antibiotics, including fluoroquinolones, tetracyclines (minocycline > doxycycline, tetracycline), and sulfa antibiotics, including but not limited to sulfasalazine. The effectiveness of antibiotics may not necessarily be attributable to their antimicrobial activity, as many of them particularly the tetracyclines may contain intrinsic anti-inflammatory activity, such as inhibition of matrix metalloproteinases (MMPs) [74]. Indeed, O’Dell and colleagues suggested that the effectiveness of low-dose doxycycline in one study proved that the mechanism was through inhibition of MMPs [75], although none of these studies included an assessment of the microbiota. It has also been proposed that the effectiveness of tetracyclines and sulfa drugs is due to their ability to eradicate oral pathogens [40]. As we learn more about potential microbial contributing factors to RA, the possibility that antibiotics were effective due at least in part to antimicrobial activity becomes increasingly plausible. Whatever the mechanism of effectiveness, antibiotics are generally not considered optimal long-term therapy, due to risks such as resistance to antibiotics and development of Clostridium difficile colitis. The key perhaps is to find means of altering the microbiota that do not carry the risks associated with antibiotics. For example, as discussed above, specific therapy of periodontal disease appears to be effective therapy for RA [45] perhaps by eradicating P. gingivalis, an approach that has a better safety profile than long-term use of antibiotics.
Probiotics
There have been four small sample size RCTs of probiotics in RA (Table 15.3). A fifth study was published [76] but appears to be duplicative of one of the other four [77]. Although two of them reported positive findings, these effects were minimal. For example, Mandel et al. [78] reported efficacy on the basis of small effect sizes and non-statistically significant findings such as improved patient-reported ability to participate in daily activities in 4/22 (18%) in the probiotic arm as compared to 2/22 (9.1%) in the placebo arm, p = 0.53. Likewise, after excluding 14 of 60 subjects from the analysis due to failure to follow the protocol, Alipour et al. [77] reported that the swollen joint count decreased from a mean (25th–75th percentiles) of 0 (0–2) to 0 (0–1) in the intervention group, compared to a decrease in the placebo group from 1 (0–1.75) to 1 (0–1.75); the between-group p-value was not reported. They did, however, report that patients given the probiotic were more likely to have a EULAR response (8/22 [36%] vs 1/24 [4.2%], p = 0.007) as well as significantly lower inflammatory cytokine levels in the probiotic group. Overall, however, the effects of probiotics in RA appear to be small at best. As will be discussed in the individualized medicine chapter (Chap. 35), there are multiple reasons for this lack of substantial effects, including failure of the probiotic to alter the microbiota or the selection of the wrong probiotic.
Diet
Although dietary therapies can rapidly alter the microbiota [79, 80] dietary therapy has also not been found to be a successful therapeutic approach for RA. A Cochrane review evaluated 15 controlled dietary intervention studies in RA, including vegetarian, elemental, vegan, and Mediterranean diets [81]. There were no consistent benefits observed. The vegetarian and Mediterranean diets resulted in decreased pain, but no improvements in function or objective findings. Other interventions likewise failed to show substantial effects. The authors also noted substantial dropout in the treatment arms, which they attributed to diet unpalatability. The failure of some of these studies may pertain to some of them evidently being carbohydrate-rich diets, which might have the effect of increasing the abundance of Prevotella [79], which as noted above may not be optimal in patients with RA. Clearly, future interventions must be targeted towards eradicating known dysbiosis. An additional factor to consider is that a patient’s baseline microbiota may influence response to dietary therapy [82] and thus may need to be assessed as part of the intervention.
Concluding Remarks
Over 100 years ago, RA was considered to be an infectious disease. By the late twentieth century, this hypothesis had fallen out of favor, even though some clinical trials of antibiotics showed effectiveness. Currently, there is accumulating evidence that there are infectious triggers to RA. That two geographically distinct studies of newly diagnosed subjects with RA have both shown an abundance of P. copri in their intestines [11, 13], particularly in light of the data showing the same organism to be an immunologic target in RA [21], is highly suggestive that this organism may be part of the pathogenesis of the disease. Given that its abundance appears to be normal in established disease [11, 14], it remains to be seen whether attempts to target this organism therapeutically might bear fruit. In contrast, the gingival microbiota, particularly in patients with severe periodontal disease, appears to be a worthwhile therapeutic target. Whether antibiotics are effective due to their ability to eradicate oral pathogens is unclear, and few would advocate chronic use of antibiotics in light of the array of medications available today. However, just as routine screening of the eyes is part of the management of children with JIA, perhaps routine screening of the gingiva should be part of the care of RA patients, with appropriate local therapy as needed.
Abbreviations
- ACPA:
-
Anti-cyclic citrullinated peptide antibody
- CRA:
-
Chronic rheumatoid arthritis
- DAS:
-
Disease activity score
- DC:
-
Dendritic cells
- HC:
-
Healthy control
- IL:
-
Interleukin
- JIA:
-
Juvenile idiopathic arthritis
- MMP:
-
Matrix metalloproteinase
- NORA:
-
New-onset rheumatoid arthritis
- NSAID:
-
Nonsteroidal anti-inflammatory drug
- OA:
-
Osteoarthritis
- PAD:
-
Peptidylarginine deiminase
- PD:
-
Periodontal disease
- PPAD:
-
P. gingivalis peptidylarginine deiminase
- RA:
-
Rheumatoid arthritis
- SE:
-
Shared epitope
- SRP:
-
Scaling and root planning
- TNFi:
-
Tumor necrosis factor inhibitor
References
Bailey CF. The treatment of chronic rheumatic and rheumatoid arthritis by radiant heat and cataphoresis. Br Med J. 1909;1:13–5.
Mayberry J. The history of 5-ASA compounds and their use in ulcerative colitis--trailblazing discoveries in gastroenterology. J Gastrointestin Liver Dis. 2013;22:375–7.
Vaahtovuo J, Munukka E, Korkeamaki M, Luukkainen R, Toivanen P. Fecal microbiota in early rheumatoid arthritis. J Rheumatol. 2008;35:1500–5.
Shinebaum R, Neumann VC, Cooke EM, Wright V. Comparison of faecal florae in patients with rheumatoid arthritis and controls. Br J Rheumatol. 1987;26:329–33.
Severijnen AJ, Kool J, Swaak AJ, Hazenberg MP. Intestinal flora of patients with rheumatoid arthritis: induction of chronic arthritis in rats by cell wall fragments from isolated Eubacterium aerofaciens strains. Br J Rheumatol. 1990;29:433–9.
Dearlove SM, Barr K, Neumann V, Isdale A, Bird HA, Gooi HC, et al. The effect of non-steroidal anti-inflammatory drugs on faecal flora and bacterial antibody levels in rheumatoid arthritis. Br J Rheumatol. 1992;31(7):443.
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, et al. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–8.
Goodman AL, Kallstrom G, Faith JJ, Reyes A, Moore A, Dantas G, et al. Extensive personal human gut microbiota culture collections characterized and manipulated in gnotobiotic mice. Proc Natl Acad Sci U S A. 2011;108:6252–7.
Toivanen P. Normal intestinal microbiota in the aetiopathogenesis of rheumatoid arthritis. Ann Rheum Dis. 2003;62:807–11.
Arumugam M, Raes J, Pelletier E, Le Paslier D, Yamada T, Mende DR, et al. Enterotypes of the human gut microbiome. Nature. 2011;473:174–80.
Scher JU, Sczesnak A, Longman RS, Segata N, Ubeda C, Bielski C, et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife. 2013;2:e01202.
Gregersen PK, Silver J, Winchester RJ. The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum. 1987;30:1205–13.
Maeda Y, Kurakawa T, Umemoto E, Motooka D, Ito Y, Gotoh K, et al. Dysbiosis contributes to arthritis development via activation of autoreactive T cells in the intestine. Arthritis Rheumatol. 2016;68(11):2646–61.
Chen J, Wright K, Davis JM, Jeraldo P, Marietta EV, Murray J, et al. An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Med. 2016;8:43.
Zhang X, Zhang D, Jia H, Feng Q, Wang D, Liang D, et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med. 2015;21:895–905.
Cao Y, Shen J, Ran ZH. Association between Faecalibacterium prausnitzii reduction and inflammatory bowel disease: a meta-analysis and systematic review of the literature. Gastroenterol Res Pract. 2014;2014:872725.
Stoll ML, Kumar R, Morrow CD, Lefkowitz EJ, Cui X, Genin A, et al. Altered microbiota associated with abnormal humoral immune responses to commensal organisms in enthesitis-related arthritis. Arthritis Res Ther. 2014;16:486.
Di Paola M, Cavalieri D, Albanese D, Sordo M, Pindo M, Donati C, et al. Alteration of Fecal Microbiota profiles in juvenile idiopathic arthritis. Associations with HLA-B27 allele and disease status. Front Microbiol. 2016;7:1703.
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science. 2013;341:569–73.
Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer RJ. Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. 2008;27:104–19.
Pianta A, Arvikar S, Strle K, Drouin EE, Wang Q, Costello CE, et al. Evidence for immune relevance of Prevotella copri, a gut microbe, in patients with rheumatoid arthritis. Arthritis Rheumatol. 2016;69(5):964–75.
Cuvelier C, Barbatis C, Mielants H, De Vos M, Roels H, Veys E. Histopathology of intestinal inflammation related to reactive arthritis. Gut. 1987;28:394–401.
Hindryckx P, Laukens D, Serry G, Van Praet L, Cuvelier C, Mielants H, et al. Subclinical gut inflammation in spondyloarthritis is associated with a pro-angiogenic intestinal mucosal phenotype. Ann Rheum Dis. 2011;70:2044–8.
Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontology 2000. 2014;64:57–80.
Bingham CO 3rd, Moni M. Periodontal disease and rheumatoid arthritis: the evidence accumulates for complex pathobiologic interactions. Curr Opin Rheumatol. 2013;25:345–53.
Scher JU, Ubeda C, Equinda M, Khanin R, Buischi Y, Viale A, et al. Periodontal disease and the oral microbiota in new-onset rheumatoid arthritis. Arthritis Rheum. 2012;64(10):3083–94.
Scaling HD. Root planning is recommended in the nonsurgical treatment of chronic periodontitis. J Evid Based Dent Pract. 2016;16:56–8.
de Pablo P, Dietrich T, McAlindon TE. Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J Rheumatol. 2008;35:70–6.
Dev YP, Khuller N, Basavaraj P, Suresh G. Rheumatoid Arthritis among periodontitis patients in Baddi industrial Estate of Himachal Pradesh, India: a cross sectional study. J Clin Diagnos Res. 2013;7:2334–7.
Joseph R, Rajappan S, Nath SG, Paul BJ. Association between chronic periodontitis and rheumatoid arthritis: a hospital-based case-control study. Rheumatol Int. 2013;33:103–9.
Wolff B, Berger T, Frese C, Max R, Blank N, Lorenz HM, et al. Oral status in patients with early rheumatoid arthritis: a prospective, case-control study. Rheumatology (Oxford). 2014;53:526–31.
Klareskog L, Stolt P, Lundberg K, Kallberg H, Bengtsson C, Grunewald J, et al. A new model for an etiology of rheumatoid arthritis: smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum. 2006;54:38–46.
Kinane DF, Chestnutt IG. Smoking and periodontal disease. Crit Rev Oral Biol Med. 2000;11:356–65.
Reichert S, Haffner M, Keysser G, Schafer C, Stein JM, Schaller HG, et al. Detection of oral bacterial DNA in synovial fluid. J Clin Periodontol. 2013;40:591–8.
Temoin S, Chakaki A, Askari A, El-Halaby A, Fitzgerald S, Marcus RE, et al. Identification of oral bacterial DNA in synovial fluid of patients with arthritis with native and failed prosthetic joints. J Clin Rheumatol. 2012;18:117–21.
Johnson S, Sidebottom D, Bruckner F, Collins D. Identification of mycoplasma fermentans in synovial fluid samples from arthritis patients with inflammatory disease. J Clin Microbiol. 2000;38:90–3.
Johnson SM, Bruckner F, Collins D. Distribution of mycoplasma pneumoniae and mycoplasma salivarium in the synovial fluid of arthritis patients. J Clin Microbiol. 2007;45:953–7.
Wilkinson NZ, Kingsley GH, Jones HW, Sieper J, Braun J, Ward ME. The detection of DNA from a range of bacterial species in the joints of patients with a variety of arthritides using a nested, broad-range polymerase chain reaction. Rheumatology (Oxford). 1999;38:260–6.
van der Heijden IM, Wilbrink B, Tchetverikov I, Schrijver IA, Schouls LM, Hazenberg MP, et al. Presence of bacterial DNA and bacterial peptidoglycans in joints of patients with rheumatoid arthritis and other arthritides. Arthritis Rheum. 2000;43:593–8.
Sandhya P, Danda D, Sharma D, Scaria V. Does the buck stop with the bugs?: an overview of microbial dysbiosis in rheumatoid arthritis. Int J Rheum Dis. 2016;19:8–20.
Johansson L, Sherina N, Kharlamova N, Potempa B, Larsson B, Israelsson L, et al. Concentration of antibodies against Porphyromonas gingivalis is increased before the onset of symptoms of rheumatoid arthritis. Arthritis Res Ther. 2016;18:201.
Erciyas K, Sezer U, Ustun K, Pehlivan Y, Kisacik B, Senyurt SZ, et al. Effects of periodontal therapy on disease activity and systemic inflammation in rheumatoid arthritis patients. Oral Dis. 2013;19:394–400.
Biyikoglu B, Buduneli N, Aksu K, Nalbantsoy A, Lappin DF, Evrenosoglu E, et al. Periodontal therapy in chronic periodontitis lowers gingival crevicular fluid interleukin-1beta and DAS28 in rheumatoid arthritis patients. Rheumatol Int. 2013;33:2607–16.
Ribeiro J, Leao A, Novaes AB. Periodontal infection as a possible severity factor for rheumatoid arthritis. J Clin Periodontol. 2005;32:412–6.
Ortiz P, Bissada NF, Palomo L, Han YW, Al-Zahrani MS, Panneerselvam A, et al. Periodontal therapy reduces the severity of active rheumatoid arthritis in patients treated with or without tumor necrosis factor inhibitors. J Periodontol. 2009;80:535–40.
Bonfil JJ, Dillier FL, Mercier P, Reviron D, Foti B, Sambuc R, et al. A “case control” study on the role of HLA DR4 in severe periodontitis and rapidly progressive periodontitis. Identification of types and subtypes using molecular biology (PCR.SSO). J Clin Periodontol. 1999;26:77–84.
Raychaudhuri S, Sandor C, Stahl EA, Freudenberg J, Lee HS, Jia X, et al. Five amino acids in three HLA proteins explain most of the association between MHC and seropositive rheumatoid arthritis. Nat Genet. 2012;44:291–6.
Schaefer AS, Jochens A, Dommisch H, Graetz C, Jockel-Schneider Y, Harks I, et al. A large candidate-gene association study suggests genetic variants at IRF5 and PRDM1 to be associated with aggressive periodontitis. J Clin Periodontol. 2014;41:1122–31.
Preshaw PM, Taylor JJ. How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis? J Clin Periodontol. 2011;38(Suppl 11):60–84.
Okada M, Kobayashi T, Ito S, Yokoyama T, Komatsu Y, Abe A, et al. Antibody responses to periodontopathic bacteria in relation to rheumatoid arthritis in Japanese adults. J Periodontol. 2011;82:1433–41.
Ogrendik M, Kokino S, Ozdemir F, Bird PS, Hamlet S. Serum antibodies to oral anaerobic bacteria in patients with rheumatoid arthritis. MedGenMed. 2005;7:2.
Mikuls TR, Payne JB, Reinhardt RA, Thiele GM, Maziarz E, Cannella AC, et al. Antibody responses to Porphyromonas gingivalis (P. Gingivalis) in subjects with rheumatoid arthritis and periodontitis. Int Immunopharmacol. 2009;9:38–42.
Kharlamova N, Jiang X, Sherina N, Potempa B, Israelsson L, Quirke AM, et al. Antibodies to Porphyromonas gingivalis indicate interaction between oral infection, smoking, and risk genes in rheumatoid arthritis Etiology. Arthritis Rheumatol. 2016;68:604–13.
Hitchon CA, Chandad F, Ferucci ED, Willemze A, Ioan-Facsinay A, van der Woude D, et al. Antibodies to porphyromonas gingivalis are associated with anticitrullinated protein antibodies in patients with rheumatoid arthritis and their relatives. J Rheumatol. 2010;37:1105–12.
Mikuls TR, Payne JB, Yu F, Thiele GM, Reynolds RJ, Cannon GW, et al. Periodontitis and Porphyromonas gingivalis in patients with rheumatoid arthritis. Arthritis Rheumatol. 2014;66:1090–100.
Seror R, Le Gall-David S, Bonnaure-Mallet M, Schaeverbeke T, Cantagrel A, Minet J, et al. Association of anti-porphyromonas gingivalis antibody Titers with Nonsmoking status in early rheumatoid arthritis: results from the prospective French cohort of patients with early rheumatoid arthritis. Arthritis Rheumatol. 2015;67:1729–37.
Wegner N, Wait R, Sroka A, Eick S, Nguyen KA, Lundberg K, et al. Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and alpha-enolase: implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum. 2010;62:2662–72.
Taylor P, Gartemann J, Hsieh J, Creeden J. A systematic review of serum biomarkers anti-cyclic citrullinated peptide and rheumatoid factor as tests for rheumatoid arthritis. Autoimmune Dis. 2011;2011:815038.
Foulquier C, Sebbag M, Clavel C, Chapuy-Regaud S, Al Badine R, Mechin MC, et al. Peptidyl arginine deiminase type 2 (PAD-2) and PAD-4 but not PAD-1, PAD-3, and PAD-6 are expressed in rheumatoid arthritis synovium in close association with tissue inflammation. Arthritis Rheum. 2007;56:3541–53.
Chang X, Yamada R, Suzuki A, Sawada T, Yoshino S, Tokuhiro S, et al. Localization of peptidylarginine deiminase 4 (PADI4) and citrullinated protein in synovial tissue of rheumatoid arthritis. Rheumatology (Oxford). 2005;44:40–50.
Kinloch A, Lundberg K, Wait R, Wegner N, Lim NH, Zendman AJ, et al. Synovial fluid is a site of citrullination of autoantigens in inflammatory arthritis. Arthritis Rheum. 2008;58:2287–95.
Suzuki A, Yamada R, Chang X, Tokuhiro S, Sawada T, Suzuki M, et al. Functional haplotypes of PADI4, encoding citrullinating enzyme peptidylarginine deiminase 4, are associated with rheumatoid arthritis. Nat Genet. 2003;34:395–402.
Poor G, Nagy ZB, Schmidt Z, Brozik M, Meretey K, Gergely P Jr. Genetic background of anticyclic citrullinated peptide autoantibody production in Hungarian patients with rheumatoid arthritis. Ann N Y Acad Sci. 2007;1110:23–32.
Du Y, Liu X, Guo JP, Liu X, Li R, Zhao Y, et al. Association between PADI4 gene polymorphisms and anti-cyclic citrullinated peptide antibody positive rheumatoid arthritis in a large Chinese Han cohort. Clin Exp Rheumatol. 2014;32:377–82.
Yamamoto K, Yamada R. Genome-wide single nucleotide polymorphism analyses of rheumatoid arthritis. J Autoimmun. 2005;25(Suppl):12–5.
Gabarrini G, de Smit M, Westra J, Brouwer E, Vissink A, Zhou K, et al. The peptidylarginine deiminase gene is a conserved feature of Porphyromonas gingivalis. Sci Rep. 2015;5:13936.
Maresz KJ, Hellvard A, Sroka A, Adamowicz K, Bielecka E, Koziel J, et al. Porphyromonas gingivalis facilitates the development and progression of destructive arthritis through its unique bacterial peptidylarginine deiminase (PAD). PLoS Pathog. 2013;9:e1003627.
Kuhn KA, Kulik L, Tomooka B, Braschler KJ, Arend WP, Robinson WH, et al. Antibodies against citrullinated proteins enhance tissue injury in experimental autoimmune arthritis. J Clin Investig. 2006;116:961–73.
Cui J, Taylor KE, Destefano AL, Criswell LA, Izmailova ES, Parker A, et al. Genome-wide association study of determinants of anti-cyclic citrullinated peptide antibody titer in adults with rheumatoid arthritis. Mol Med. 2009;15:136–43.
Kokkonen H, Brink M, Hansson M, Lassen E, Mathsson-Alm L, Holmdahl R, et al. Associations of antibodies against citrullinated peptides with human leukocyte antigen-shared epitope and smoking prior to the development of rheumatoid arthritis. Arthritis Res Ther. 2015;17:125.
Doyle TJ, Dellaripa PF, Batra K, Frits ML, Iannaccone CK, Hatabu H, et al. Functional impact of a spectrum of interstitial lung abnormalities in rheumatoid arthritis. Chest. 2014;146:41–50.
Scher JU, Joshua V, Artacho A, Abdollahi-Roodsaz S, Ockinger J, Kullberg S, et al. The lung microbiota in early rheumatoid arthritis and autoimmunity. Microbiome. 2016;4:60.
Segata N, Haake SK, Mannon P, Lemon KP, Waldron L, Gevers D, et al. Composition of the adult digestive tract bacterial microbiome based on seven mouth surfaces, tonsils, throat and stool samples. Genome Biol. 2012;13:R42.
Nordstrom D, Lindy O, Lauhio A, Sorsa T, Santavirta S, Konttinen YT. Anti-collagenolytic mechanism of action of doxycycline treatment in rheumatoid arthritis. Rheumatol Int. 1998;17:175–80.
O’Dell JR, Elliott JR, Mallek JA, Mikuls TR, Weaver CA, Glickstein S, et al. Treatment of early seropositive rheumatoid arthritis: doxycycline plus methotrexate versus methotrexate alone. Arthritis Rheum. 2006;54:621–7.
Vaghef-Mehrabany E, Alipour B, Homayouni-Rad A, Sharif SK, Asghari-Jafarabadi M, Zavvari S. Probiotic supplementation improves inflammatory status in patients with rheumatoid arthritis. Nutrition. 2014;30:430–5.
Alipour B, Homayouni-Rad A, Vaghef-Mehrabany E, Sharif SK, Vaghef-Mehrabany L, Asghari-Jafarabadi M, et al. Effects of lactobacillus casei supplementation on disease activity and inflammatory cytokines in rheumatoid arthritis patients: a randomized double-blind clinical trial. Int J Rheum Dis. 2014;17:519–27.
Mandel DR, Eichas K, Holmes J. Bacillus coagulans: a viable adjunct therapy for relieving symptoms of rheumatoid arthritis according to a randomized, controlled trial. BMC Complement Altern Med. 2010;10(1):1.
Wu GD, Chen J, Hoffmann C, Bittinger K, Chen YY, Keilbaugh SA, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science. 2011;334:105–8.
David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–63.
Hagen KB, Byfuglien MG, Falzon L, Olsen SU, Smedslund G. Dietary interventions for rheumatoid arthritis. Cochrane Database Syst Rev. 2009;1:CD006400.
Kang C, Zhang Y, Zhu X, Liu K, Wang X, Chen M, et al. Healthy subjects differentially respond to dietary capsaicin correlating with the specific gut enterotypes. J Clin Endocrinol Metab. 2016;101(12):4681–9. jc20162786.
Borg AA, Davis MJ, Fowler PD, Shadforth MF, Dawes PT. Rifampicin in early rheumatoid arthritis. Scand J Rheumatol. 1993;22:39–42.
Ogrendik M. Levofloxacin treatment in patients with rheumatoid arthritis receiving methotrexate. South Med J. 2007;100:135–9.
Ogrendik M. Effects of clarithromycin in patients with active rheumatoid arthritis. Curr Med Res Opin. 2007;23:515–22.
Saviola G, Abdi-Ali L, Campostrini L, Sacco S, Baiardi P, Manfredi M, et al. Clarithromycin in rheumatoid arthritis: the addition to methotrexate and low-dose methylprednisolone induces a significant additive value--a 24-month single-blind pilot study. Rheumatol Int. 2013;33:2833–8.
Ogrendik M. Efficacy of roxithromycin in adult patients with rheumatoid arthritis who had not received disease-modifying antirheumatic drugs: a 3-month, randomized, double-blind, placebo-controlled trial. Clin Ther. 2009;31:1754–64.
Ogrendik M, Karagoz N. Treatment of rheumatoid arthritis with roxithromycin: a randomized trial. Postgrad Med. 2011;123:220–7.
Sreekanth VR, Handa R, Wali JP, Aggarwal P, Dwivedi SN. Doxycycline in the treatment of rheumatoid arthritis--a pilot study. J Assoc Physicians India. 2000;48:804–7.
St Clair EW, Wilkinson WE, Pisetsky DS, Sexton DJ, Drew R, Kraus VB, et al. The effects of intravenous doxycycline therapy for rheumatoid arthritis: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2001;44:1043–7.
van der Laan W, Molenaar E, Ronday K, Verheijen J, Breedveld F, Greenwald R, et al. Lack of effect of doxycycline on disease activity and joint damage in patients with rheumatoid arthritis. A double blind, placebo controlled trial. J Rheumatol. 2001;28:1967–74.
Pillemer S, Gulko P, Ligier S, Yarboro C, Gourley M, Goldbach-Mansky R, et al. Pilot clinical trial of intravenous doxycycline versus placebo for rheumatoid arthritis. J Rheumatol. 2003;30:41–3.
Kloppenburg M, Breedveld FC, Terwiel JP, Mallee C, Dijkmans BA. Minocycline in active rheumatoid arthritis. A double-blind, placebo-controlled trial. Arthritis Rheum. 1994;37:629–36.
Tilley BC, Alarcon GS, Heyse SP, Trentham DE, Neuner R, Kaplan DA, et al. Minocycline in rheumatoid arthritis. A 48-week, double-blind, placebo-controlled trial. MIRA trial group. Ann Intern Med. 1995;122:81–9.
O’Dell JR, Haire CE, Palmer W, Drymalski W, Wees S, Blakely K, et al. Treatment of early rheumatoid arthritis with minocycline or placebo: results of a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 1997;40:842–8.
O’Dell JR, Blakely KW, Mallek JA, Eckhoff PJ, Leff RD, Wees SJ, et al. Treatment of early seropositive rheumatoid arthritis: a two-year, double-blind comparison of minocycline and hydroxychloroquine. Arthritis Rheum. 2001;44:2235–41.
Skinner M, Cathcart ES, Mills JA, Pinals RS. Tetracycline in the treatment of rheumatoid arthritis. A double blind controlled study. Arthritis Rheum. 1971;14:727–32.
Gompels LL, Smith A, Charles PJ, Rogers W, Soon-Shiong J, Mitchell A, et al. Single-blind randomized trial of combination antibiotic therapy in rheumatoid arthritis. J Rheumatol. 2006;33:224–7.
Smith A, Dore C, Charles P, Vallance A, Potier T, Mackworth-Young C. Randomised double-blind trial of combination antibiotic therapy in rheumatoid arthritis. Int J Rheumatol. 2011;2011:585497.
Harkness JA, Griffin AJ, Heinrich I, Gibson T, Grahame R. A double-blind comparative study of metronidazole and placebo in rheumatoid arthritis. Rheumatol Rehabil. 1982;21:231–4.
Marshall DA, Hunter JA, Capell HA. Double blind, placebo controlled study of metronidazole as a disease modifying agent in the treatment of rheumatoid arthritis. Ann Rheum Dis. 1992;51:758–60.
Ogrendik M, Hakguder A, Keser N. Treatment of rheumatoid arthritis with ornidazole. A randomized, double-blind, placebo-controlled study. Rheumatology (Oxford). 2006;45:636–7.
Ash G, Baker R, Rajapakse C, Swinson DR. Study of sulphamethoxazole in rheumatoid arthritis. Br J Rheumatol. 1986;25:285–7.
Wojtulewski JA, Gow PJ, Walter J, Grahame R, Gibson T, Panayi GS, et al. Clotrimazole in rheumatoid arthritis. Ann Rheum Dis. 1980;39:469–72.
Neumann VC, Grindulis KA, Hubball S, McConkey B, Wright V. Comparison between penicillamine and sulphasalazine in rheumatoid arthritis: Leeds-Birmingham trial. Br Med J. 1983;287:1099–102.
Pullar T, Hunter JA, Capell HA. Sulphasalazine in rheumatoid arthritis: a double blind comparison of sulphasalazine with placebo and sodium aurothiomalate. Br Med J. 1983;287:1102–4.
Pinals RS, Kaplan SB, Lawson JG, Hepburn B. Sulfasalazine in rheumatoid arthritis. A double-blind, placebo-controlled trial. Arthritis Rheum. 1986;29:1427–34.
Williams HJ, Ward JR, Dahl SL, Clegg DO, Willkens RF, Oglesby T, et al. A controlled trial comparing sulfasalazine, gold sodium thiomalate, and placebo in rheumatoid arthritis. Arthritis Rheum. 1988;31:702–13.
Hannonen P, Mottonen T, Hakola M, Oka M. Sulfasalazine in early rheumatoid arthritis. A 48-week double-blind, prospective, placebo-controlled study. Arthritis Rheum. 1993;36:1501–9.
Hatakka K, Martio J, Korpela M, Herranen M, Poussa T, Laasanen T, et al. Effects of probiotic therapy on the activity and activation of mild rheumatoid arthritis--a pilot study. Scand J Rheumatol. 2003;32:211–5.
Pineda Mde L, Thompson SF, Summers K, de Leon F, Pope J, Reid G. A randomized, double-blinded, placebo-controlled pilot study of probiotics in active rheumatoid arthritis. Med Sci Monit. 2011;17:CR347–54.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Stoll, M.L., Bridges, S.L., Danila, M.I. (2018). Rheumatoid Arthritis. In: Ragab, G., Atkinson, T., Stoll, M. (eds) The Microbiome in Rheumatic Diseases and Infection. Springer, Cham. https://doi.org/10.1007/978-3-319-79026-8_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-79026-8_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-79025-1
Online ISBN: 978-3-319-79026-8
eBook Packages: MedicineMedicine (R0)