Abstract
Several clinical and hemodynamic variables potentially factor in the immediate post-procedural and long-term outcome following percutaneous coronary intervention. The proper identification and definition of risk is a crucial prerequisite to implement adequate supportive measures and potentially avoid procedural complications. Discriminating coronary lesions based on their complexity has important implications for procedural planning and to predict (and prevent) the onset of procedural complications. However, the characteristics of a coronary lesion should be contextualized with the clinical presentation and patients’ risk profile to get a 360° vision of PCI complexity.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Percutaneous coronary intervention
- Chronic total occlusion
- Bifurcation lesion
- Intravascular ultrasound
- Optical coherence tomography
- Quantitative coronary angiography
- EuroScore
- SYNTAX score
- Duke Jeopardy score
The cardiac catheterization laboratory at our hospital manages the invasive care of a wide range of cardiovascular pathological conditions, including coronary artery disease (CAD), peripheral artery disease, and structural heart disease. The center’s philosophy is based on the close interplay of clinical care according to international standards, innovation, and research. Local protocols are implemented and shared between different professional figures (i.e., physicians, nurses, technicians) involved in pre-procedural, procedural, and post-procedural patients’ management. A pre-procedural checklist is routinely adopted to verify the appropriateness of the indication, the correct preparation of the patient, and the absence of absolute or relative contraindications to each invasive procedure. One of the most important aspects is the implementation of a multidisciplinary Heart Team approach for the management of complex clinical cases. In keeping with guideline recommendations, the Heart Team is composed of interventional cardiologists, cardiac surgeons, clinical cardiologists, and anesthesiologists. Local meetings are regularly scheduled to discuss and select the most appropriate therapeutic strategy according to each patient’s profile. Being also an academic center, clinical research is of primary importance. Whenever possible and appropriate, and after providing detailed explanations on studies’ characteristics, consenting patients are enrolled in randomized controlled trials or multicenter registries. Single-center, investigator-driven observational studies are also conducted. Research is deemed as an instrument to improve daily clinical practice and overall quality of care.
Planning Coronary Intervention
Categorizing Coronary Lesions
-
Discriminating coronary lesions based on their complexity has important implications for procedural planning and to predict (and prevent) the onset of procedural complications. However, the characteristics of a coronary lesion should be contextualized with the clinical presentation and patients’ risk profile to get a 360° vision of PCI complexity.
-
The ACC/AHA angiographic classification of coronary lesions has been largely validated and investigated in the medical literature. Coding details of this classification system are shown in Table 8.1.
-
Kastrati et al. [1] investigated the prognostic value of the ACC/AHA classification system in 2944 patients undergoing PCI by dichotomization into type A/B1 and B2/C lesions (reflecting simple and complex anatomies, respectively). One-year event-free survival was 75.6% for patients with complex lesions and 81.1% for patients with simple lesions (P < 0.001) [1].
-
Coronary lesions at bifurcation sites, defined as the site of junction of a main vessel with a side branch, are frequently encountered in daily clinical practice and represent a major challenge for treatment by PCI. Bifurcation sites are prone to develop and favor the progression of atherosclerotic lesions due to flow disturbances and low shear stress [2].
-
The Medina classification system for bifurcations is a simple and widely used tool to categorize coronary bifurcation lesions [3]. Three components of a bifurcation are considered and scored “1” if affected by significant CAD, namely the proximal main branch, distal main branch, and side branch.
-
The International Classification for Patient Safety (ICPS) classification system for bifurcation lesions is a relatively more complex system to classify lesions localized at bifurcation sites. Seven different typologies of bifurcation lesions are considered by this system [4]. Figure 8.1 graphically represents the Medina and the Duke/ICPS classification system for lesions at bifurcation sites.
-
Additional potentially identifiable lesions during coronary angiography are chronic total occlusions (CTO). Up to 20% of coronary angiograms reveal the presence of a CTO [5].
-
A chronic total occlusion (CTO) is defined as the absence of anterograde flow in a coronary segment. Bridging, ipsilateral, or contralateral collaterals may fill the segments distal to the occlusion.
-
The total occlusion classification system and the Japanese-CTO (J-CTO) score are simple classification systems to categorize and predict the procedural complexity and the likelihood of successful revascularization in CTO PCI [6, 7].
-
Parameters considered by the first system are occlusion lasting more than 3 months, presence of side branch and their size, blunt stump, presence of bridging collaterals, and occlusion length.
-
The J-CTO score predicts successful wiring of a CTO within 30 min by considering the following variables: calcification, bending, blunt stump, occlusion length >20 mm, and previously failed lesion.
-
Advances in the field of invasive coronary imaging with intravascular ultrasound (IVUS) and optical coherence tomography (OCT) now allow for a more detailed characterization of lesion anatomy. Coronary plaques may be classified based on the presence of necrotic core, fibro-fatty tissue, fibrous tissue, or dense calcium with IVUS imaging.
-
Pathological intimal thickening, fibrotic and fibro-calcific plaques, and thick- or thin-cap fibro-atheromas can be further identifiable by IVUS-derived virtual histology [8].
-
Due to its higher spatial resolution, OCT can be used for detailed measurement of cap thickness and additional identification of specific cap features including macrophage accumulation, lipid volume, microcalcifications, plaque erosion or rupture (Fig. 8.2), neovascularization, and thrombus [9].
-
Invasive characterization of coronary lesions is of particular interest since some in vivo characteristics have been related to adverse clinical outcomes at follow-up. The landmark PROSPECT trial showed that the presence of a plaque burden of 70% or greater, a minimal luminal area of 4.0 mm2 or less, and a thin-cap fibro-atheroma independently predicted the 3-year cumulative rate of major adverse cardiovascular events in non-culprit lesions at the time of PCI [11].
Picture showing OCT characteristics of a ruptured and eroded plaque. Adapted with permission from Guagliumi G. et al. [10]
Quantitative Coronary Angiography
-
Quantitative coronary angiography (QCA) analysis after adequate acquisition and computerized processing of coronary angiograms is a widely established tool to objectively quantify the extent and severity of CAD. Indeed, qualitative analysis based on operator visual estimation may be affected by excess in intra- and inter-observer variability.
-
QCA analysis may overcome these limitations by using specific vessel edge detection algorithms that accurately identify the dimensions and course of the coronary vessels, thus providing operator-independent and objective measures of coronary anatomy [12].
-
Accurate measurements of vessel stenosis may avoid unnecessary interventions in nonsignificant lesions or may improve PCI results by providing accurate measures for proper stent selection.
-
Conventional 2D-QCA is based on the computerized analysis of two-dimensional cine angiograms. Recently, 3D-QCA tools allow for reconstruction of 3D rendered views from multiple angiographic X-ray projections; this is particularly useful to reduce potential errors of 2D-QCA such as foreshortening and out-of-plane magnification errors [13]. Moreover, 3D-QCA may be of particular value in specific anatomical contexts, like diseased coronary bifurcations, where a detailed reconstruction of spatial disease is crucial to plan PCI by selecting the most appropriate technique.
-
The first step to performing a reliable and reproducible QCA depends on the performance of high-quality coronary angiography. It is of fundamental importance to select at least two projections that are orthogonal with the segment of interest to avoid foreshortening. In addition, overlap of anatomic structures or angiographic catheters along the vessel course should be avoided. It is also important to include the proximal part of the angiographic catheter in the acquisition since the catheter is used for calibration of sizing.
-
Some additional tricks could improve the quality of QCA, such as cine angiogram acquisition during inspiration to increase the distinction between contrast-filled vessels and the background of image and the injection of intracoronary nitroglycerine to resolve vasospasm [14].
-
After selection of the end-diastolic frame in a clear, non-foreshortened view and after proper calibration of the catheter, the QCA software allows for the measurement of different parameters (Table 8.2) by automatic vessel edge detection algorithms.
-
QCA measurements can also be integrated and defined by quantitative IVUS analysis (diameters and areas, lesion length) before stent placement. Indeed, IVUS -guided PCI has the potential to highlight some adverse plaque features before (i.e., heavy calcification, high thrombotic burden) and after stent implantation (i.e., edge dissection, incomplete stent apposition) that may prevent and reduce immediate and long-term adverse events following PCI.
Determinants of Risk and Prognostic Indexes
-
Clinical risk defines the probability or the potential hazard of complications or adverse outcomes following a therapeutic intervention. Categorization and estimation of a patient’s clinical risk profile are often challenging due to the stochastic and time-varying nature of risk [15]. Indeed, several factors, including clinical, procedural, and technique-related variables, may potentially jeopardize the clinical outcomes (Table 8.3).
-
Risk scores may represent helpful clinical aids to properly categorize and predict patients’ risk. Indeed, risk scores are obtained with mathematical models that, by weighting and integrating the hazard conferred by specific pre-procedural clinical characteristics, estimate the risk for procedural complications or adverse outcomes.
-
Beyond risk score assessment, a careful evaluation of some simple pre-procedural parameters is of primary importance to preserve safety:
-
Blood parameters (hemoglobin levels, platelet count, coagulation status, renal function)
-
Hypersensitivity to drugs or contrast medium
-
Previous vascular interventions or complications at access sites
-
Antithrombotic therapy at the time of the intervention (dual-antiplatelet therapy, single-antiplatelet agent, chronic oral anticoagulant)
-
Patent venous access for administration of fluids or drugs in case of complications
-
Myocardium at Risk Scores
-
Myocardium at risk scores are useful tools to estimate the amount of myocardium jeopardized by underling CAD. Such scores introduce a weighting factor for coronary lesions in relation to their location in the coronary tree. The weighting factor is attributed in relationship to the extent of blood supplied to the myocardium. Indeed, the concept that the amount of myocardium jeopardized could represent a prognostic determinant in patients undergoing revascularization is straightforward but challenging to define numerically.
-
Among different myocardium at risk scores, three principal scores have been more extensively investigated and validated in the literature, including the Jeopardy score from Duke University, the Myocardial Jeopardy Index from the Bypass Angioplasty Revascularization Investigation (BARI) trial , and the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH score) [16].
-
The Duke Jeopardy score subdivides the coronary tree into six arterial segments, namely the left anterior descending, major anterolateral (diagonal) branch, first major septal perforator branch, circumflex artery, major marginal branch, and posterior descending artery. Two points are assigned for each diseased coronary segment (defined as a diameter reduction ≥75%) and no points are given to the right coronary artery in patients with left dominance.
-
In the Myocardial Jeopardy Index from the BARI trial , the terminal portion of the left anterior descending, left circumflex, and right coronary arteries as well as the terminal portion of major branches (diagonals, obtuse marginals, posterior descending, and posterolateral branches) are assigned a score between 0 and 3 based on vessel length/diameter. A score of 0 is attributed to insignificant or inconspicuous arteries while a score of 3 is conferred to large arteries (i.e., extending more than two-thirds of the base-to-apex distance). Septal branches are arbitrarily assigned a maximum total score of 3. All segmental scores affected by CAD (≥50% stenosis) are summed and divided by the total score to calculate the jeopardized myocardium subtended by CAD.
-
The APPROACH score estimates the myocardium at risk by dividing the left ventricle into regions at jeopardy on the basis of the myocardium perfused by each coronary artery as identified in pathological studies in humans (Fig. 8.3).
-
The external validation of the above-described scores has been performed in a large unselected cohort of >20,000 patients [16]. All the three myocardium at risk scores showed good predictive ability for the estimation of 1-year mortality. The APPROACH score performed slightly better in patients undergoing PCI or medically treated. The BARI and APPROACH scores have also been validated in the setting of acute myocardial infarction. Both scores were significantly related to the infarct transmurality and infarct endocardial surface area as assessed by cardiac magnetic resonance imaging [17].
The APPROACH score for the quantification of myocardium at risk. Reprinted with permission from Graham MM et al. [16]
EuroScore, SYNTAX, and SYNTAX II Scores
-
The European System for Cardiac Operative Risk Evaluation (EuroSCORE) is a multi-parametric risk score that was originally conceived to estimate the risk of operative mortality in patients undergoing cardiac surgery. The score was derived from a large cohort of 19,030 adult patients undergoing cardiac surgery (63.6% undergoing isolated coronary surgery and 29.8% valve operations) at 132 surgical centers in 8 European states [18]. Overall, in-hospital mortality was 4.8% in the study cohort.
-
Independent predictors of mortality among several explored clinical parameters were identified by multivariate logistic regression analysis and were integrated into a simple integer and additive risk score. Subsequently, a different and more sophisticated way to obtain the risk estimate (logistic EuroSCORE, calculated by resolving the original equations) has been introduced [19].
-
Finally, in 2011, a new version of the score (EuroSCORE II) has been introduced to update the previous models. The EuroSCORE II was derived from 22,381 consecutive patients undergoing major cardiac surgery in 154 hospitals in 43 countries between May and July 2010, reflecting a more contemporary dataset [20]. In the validation cohort, the EuroSCORE II was well calibrated and showed good discrimination. An online and user-friendly calculator of the score has been provided at http://euroscore.org/calc.html.
-
Being derived and validated from surgical series, the EuroSCORE underwent subsequent validation in patients treated with PCI confirming the good discrimination and predictive performance in large series of patients undergoing percutaneous revascularization [21,22,23].
-
The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) score is an a priori-defined angiographic tool that attempts to numerically quantify the complexity and burden of coronary artery disease.
-
The SYNTAX score was firstly introduced in the landmark SYNTAX trial and is endorsed by international guidelines to guide the clinical decision-making between PCI and coronary artery bypass grafting (CABG) [24]. International guidelines recommendations [25, 26] based on the SYNTAX score are summarized in Table 8.4.
-
For the score calculation, different anatomical and pathological characteristics are taken into account. The anatomical location of a lesion and, consequently, the extent of blood supplied to the myocardium are weighted.
-
Further characteristics, including coronary disease involving bifurcations (according to Medina classification) or trifurcations, angiographic characterization according to ACC/AHA classification, and CTO characteristics (duration, length, blunt stump, presence of bridging collaterals or side branch), are identified.
-
Finally, presence of aorto-ostial lesions, severe tortuosity, lesion length >20 mm, heavy calcification, thrombus, and diffuse or small-vessel disease are graded to refine and obtain the final score.
-
A simple online calculator of the score is available at http://www.syntaxscore.com/calculator/start.htm.
-
Two simple rules must be taken into account when interventionalists focus on the calculation of the score. First, only coronary segments with atheromatous disease determining a stenosis ≥50% in vessels ≥1.5 mm must be considered and scored. Sequential lesions must be considered as separate only if the distance among them is more than 3 vessel reference diameters apart.
-
Despite being adopted in daily clinical practice on the basis of extensive clinical research and guideline endorsement, the SYNTAX score has some principal limitations. First, calculation of the score relies on the quality of angiograms and sometimes may become time consuming such as in complex coronary anatomies.
-
The moderate reproducibility, both in terms of intra- and inter-observer variability, affects the consistency and clinical credibility of the score.
-
Finally, being a pure angiographic tool without integration of clinical variables with prognostic impact in patients undergoing either percutaneous or surgical revascularization, the score may suffer from poor calibration. In addition, the SYNTAX score does not account for clinical presentation (i.e., acute coronary syndrome) or the extent of inducible ischemia/vitality of myocardium.
-
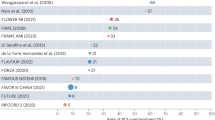
To overcome some of these limitations, different derived scores have been developed and introduced by integrating the anatomical SYNTAX score with clinical variables and functional parameters (Fig. 8.4, Table 8.5).
-
Among combined (clinical and angiographic) scores, the SYNTAX II score [32] represents one of the latest tools to guide the individualized decision-making process between CABG and PCI in patients with complex CAD. The score is built on the integration of both the anatomical SYNTAX score and clinical variables affecting mortality in CABG- versus PCI-treated patients or vice versa (interaction terms).
-
The score was derived using a Cox proportional hazards model in patients enrolled in the SYNTAX trial (n = 1800) and was externally validated in the DELTA registry (n = 2891).
-
Eight clinical variables are considered in the calculation of the score, including age, creatinine clearance, left ventricular ejection fraction (LVEF) , presence of unprotected left main CAD, peripheral vascular disease, female sex, and chronic obstructive pulmonary disease.
-
Nomograms of the score have been developed to simplify the calculation and bedside application of the score (Fig. 8.5). An online calculator is also available at http://www.syntaxscore.com/calculator/start.htm.
-
Beyond statistical performance, the meaningful message coming from the development of the SYNTAX II score is that to achieve similar mortality after revascularization with either CABG or PCI, the threshold value of the SYNTAX score to select the most appropriate revascularization strategy may vary according to the clinical and anatomical characteristics of patients (i.e., lower anatomical SYNTAX score in older patients). Therefore, when evaluating the complexity of CAD and selecting a subsequent revascularization strategy, patients’ clinical profile must be carefully evaluated since it represents a strong determinant of prognosis in concert with the anatomical complexity as evaluated with the SYNTAX score.
Integration of the anatomical SYNTAX score with clinical and functional parameters. Reprinted with permission from Capodanno et al. [27]. Abbreviations: ACEF age, creatinine, ejection fraction, CABG coronary artery bypass grafting, Compos compositional, CrCl creatinine clearance, CSS clinical SYNTAX score, FSS functional SYNTAX score, GRC global risk classification, MI myocardial infarction, MDRD modification of diet in renal disease, SrCr serum creatinine, SYNTAX SYNergy between PCI with TAXus and cardiac surgery
SYNTAX score II nomograms. Reprinted with permission from Farooq et al. [32]. Abbreviations: CrCl creatinine clearance, LVEF left ventricular ejection fraction, COPD chronic obstructive pulmonary disease, PVD peripheral vascular disease
High-Risk PCI and Supportive Measures
-
Categorization and definition of high risk in patients undergoing PCI remain elusive. Investigators and clinical researchers, both in observational studies and randomized trials, often used disparate definitions of high-risk PCI reflecting the lack of a common, standardized, and widely accepted definition [33].
-
The Complex and Higher-Risk Indicated Patients (CHIP) initiative is aiming at prospectively identifying higher risk patients undergoing PCI who potentially have the most to gain from timely performed PCI (Ajay J. Kirtane, Slide Presentation, 2015, CHIP meeting).
-
In a paradigmatic example, performing high-risk PCI has been compared to an attempt to repair a damaged car engine while it is turned on and the car is trying to slowly move from a steep cliff into the ocean at its base [34]. Beyond this analogy, a high-risk PCI patient could be identified in the presence of reduced cardiac reserve and limited ability to withstand arrhythmias, transient occlusion of coronary arteries, or distal embolization of atherogenic material.
-
In this scenario, cardiogenic shock at presentation and large areas of myocardium at jeopardy are two hallmark features of patients undergoing high-risk PCI. Data from the large CathPCI Registry (1,208,137 PCI procedures at 1252 US hospitals) clearly showed that clinical acuity (i.e., presence of cardiogenic shock or procedure urgency) is a strong determinant of in-hospital mortality [35].
-
Moreover, presence of a CTO, subacute stent thrombosis, and left main lesion location were identified as significant angiographic predictors of short-term mortality. Interestingly, the large CathPCI database has been used to develop a risk model that is able to predict short-term mortality following PCI. The correct identification of risk is crucial since adequate supportive measures could be adopted in the high-risk PCI context like mechanical support of cardiac function.
-
Results of randomized trials exploring the prophylactic use of mechanical supportive strategies (i.e., intra-aortic balloon pump , Impella, and TandemHeart devices) in high-risk PCI context have been equivocal (Table 8.6). This is probably a consequence of poor study design with underpowered sample size, inaccurate and varying definitions of high-risk patients, and limited follow-up to assess and identify differences in hard clinical endpoints like mortality.
-
Accordingly, current European and American guidelines conferred an intermediate class of indication (class IIa or IIb) for the use of invasive supportive devices in the setting of high-risk PCI.
Conclusions
Several clinical and hemodynamic variables potentially factor in the immediate post-procedural and long-term outcome following PCI. The proper identification and definition of risk is a crucial prerequisite to implement adequate supportive measures and potentially avoid procedural complications.
References
Kastrati A, Schömig A, Elezi S, Dirschinger J, Mehilli J, Schühlen H, Blasini R, Neumann FJ. Prognostic value of the modified American college of Cardiology/American heart association stenosis morphology classification for long-term angiographic and clinical outcome after coronary stent placement. Circulation. 1999;100(12):1285–90.
Nakazawa G, Yazdani SK, Finn AV, Vorpahl M, Kolodgie FD, Virmani R. Pathological findings at bifurcation lesions: the impact of flow distribution on atherosclerosis and arterial healing after stent implantation. J Am Coll Cardiol. 2010;55(16):1679–87. https://doi.org/10.1016/j.jacc.2010.01.021.
Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006;59(2):183.
Popma J, Leon M, Topol EJ. Atlas of interventional cardiology. Philadelphia, PA: Saunders; 1994.
Strauss BH, Shuvy M, Wijeysundera HC. Revascularization of chronic total occlusions: time to reconsider? J Am Coll Cardiol. 2014;64(12):1281–9. https://doi.org/10.1016/j.jacc.2014.06.1181.
Hamburger JN, Serruys PW, Scabra-Gomes R, Simon R, Koolen JJ, Fleck E, Mathey D, Sievert H, Rutsch W, Buchwald A, Marco J, Al-Kasab SM, Pizulli L, Hamm C, Corcos T, Reifart N, Hanrath P, Taeymans Y. Recanalization of total coronary occlusions using a laser guide wire (the European TOTAL Surveillance Study). Am J Cardiol. 1997;80(11):1419–23.
Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, Kato K, Shibata Y, Hiasa Y, Doi O, Yamashita T, Hinohara T, Tanaka H, Mitsudo K, J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–21. https://doi.org/10.1016/j.jcin.2010.09.024.
Sinclair H, Veerasamy M, Bourantas C, Egred M, Nair A, Calvert PA, Brugaletta S, Mintz GS, Kunadian V. The role of virtual histology intravascular ultrasound in the identification of coronary artery plaque vulnerability in acute coronary syndromes. Cardiol Rev. 2016;24(6):303–9.
Koskinas KC, Ughi GJ, Windecker S, Tearney GJ, Räber L. Intracoronary imaging of coronary atherosclerosis: validation for diagnosis, prognosis and treatment. Eur Heart J. 2016;37(6):524–35a-c. https://doi.org/10.1093/eurheartj/ehv642.
Guagliumi G, Capodanno D, Saia F, Musumeci G, Tarantini G, Garbo R, Tumminello G, Sirbu V, Coccato M, Fineschi M, Trani C, De Benedictis M, Limbruno U, De Luca L, Niccoli G, Bezerra H, Ladich E, Costa M, Biondi Zoccai G, Virmani R, Trial Investigators OCTAVIA. Mechanisms of atherothrombosis and vascular response to primary percutaneous coronary intervention in women versus men with acute myocardial infarction: results of the OCTAVIA study. JACC Cardiovasc Interv. 2014;7(9):958–68. https://doi.org/10.1016/j.jcin.2014.05.011.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, Mehran R, McPherson J, Farhat N, Marso SP, Parise H, Templin B, White R, Zhang Z, Serruys PW, PROSPECT Investigators. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011 Jan 20;364(3):226–35. https://doi.org/10.1056/NEJMoa1002358.
Garrone P, Biondi-Zoccai G, Salvetti I, Sina N, Sheiban I, Stella PR, Agostoni P. Quantitative coronary angiography in the current era: principles and applications. J Interv Cardiol. 2009;22(6):527–36. https://doi.org/10.1111/j.1540-8183.2009.00491.x.
Pantos I, Efstathopoulos EP, Katritsis DG. Two and three-dimensional quantitative coronary angiography. Cardiol Clin. 2009;27(3):491–502. https://doi.org/10.1016/j.ccl.2009.03.008.
Tomasello SD, Costanzo L, Galassi AR. Quantitative coronary angiography in the interventional cardiology. In: Kiraç SF, editor. Chapter book in “Advances in the Diagnosis of Coronary Atherosclerosis”. London: InTech; 2011. ISBN 978-953-307-286-9.
Capodanno D. Beyond the SYNTAX score—advantages and limitations of other risk assessment systems in left main percutaneous coronary intervention. Circ J. 2013;77(5):1131–8.
Graham MM, Faris PD, Ghali WA, Galbraith PD, Norris CM, Badry JT, Mitchell LB, Curtis MJ, Knudtson ML, APPROACH Investigators (Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease. Validation of three myocardial jeopardy scores in a population-based cardiac catheterization cohort. Am Heart J. 2001;142(2):254–61.
Ortiz-Pérez JT, Meyers SN, Lee DC, Kansal P, Klocke FJ, Holly TA, Davidson CJ, Bonow RO, Wu E. Angiographic estimates of myocardium at risk during acute myocardial infarction: validation study using cardiac magnetic resonance imaging. Eur Heart J. 2007;28(14):1750–8.
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999 Jul;16(1):9–13.
Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24(9):882–3.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, Lockowandt U. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–44.; discussion 744-5. https://doi.org/10.1093/ejcts/ezs043.
Romagnoli E, Burzotta F, Trani C, Siviglia M, Biondi-Zoccai GG, Niccoli G, Leone AM, Porto I, Mazzari MA, Mongiardo R, Rebuzzi AG, Schiavoni G, Crea F. EuroSCORE as predictor of in-hospital mortality after percutaneous coronary intervention. Heart. 2009;95(1):43–8. https://doi.org/10.1136/hrt.2007.134114.
Schwietz T, Spyridopoulos I, Pfeiffer S, Laskowski R, Palm S, DE Rosa S, Jens K, Zeiher AM, Schächinger V, Fichtlscherer S, Lehmann R. Risk stratification following complex PCI: clinical versus anatomical risk stratification including “post PCI residual SYNTAX-score” as quantification of incomplete revascularization. J Interv Cardiol. 2013;26(1):29–37. https://doi.org/10.1111/j.1540-8183.2013.12014.x.
Capodanno D, Dipasqua F, Marcantoni C, Ministeri M, Zanoli L, Rastelli S, Romano G, Sanfilippo M, Tamburino C. EuroSCORE II versus additive and logistic EuroSCORE in patients undergoing percutaneous coronary intervention. Am J Cardiol. 2013;112(3):323–9. https://doi.org/10.1016/j.amjcard.2013.03.032.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW, Investigators SYNTAX. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–72. https://doi.org/10.1056/NEJMoa0804626.
Authors/Task Force members, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Jüni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541–619. https://doi.org/10.1093/eurheartj/ehu278.
Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44-122. doi: https://doi.org/10.1016/j.jacc.2011.08.007.
Capodanno D. Lost in calculation: the clinical SYNTAX score goes logistic. Eur Heart J. 2012;33(24):3008–10. https://doi.org/10.1093/eurheartj/ehs346.
Nam CW, Mangiacapra F, Entjes R, Chung IS, Sels JW, Tonino PA, De Bruyne B, Pijls NH, Fearon WF, Study Investigators FAME. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J Am Coll Cardiol. 2011;58(12):1211–8. https://doi.org/10.1016/j.jacc.2011.06.020.
Capodanno D, Caggegi A, Miano M, et al. Global risk classification and clinical SYNTAX (synergy between percutaneous coronary intervention with TAXUS and cardiac surgery) score in patients undergoing percutaneous or surgical left main revascularization. J Am Coll Cardiol Intv. 2011;4:287–97.
Serruys PW, Farooq V, Vranckx P, et al. A global risk approach to identify patients with left main or 3-vessel disease who could safely and efficaciously be treated with percutaneous coronary intervention: the SYNTAX Trial at 3 years. JACC Cardiovasc Interv. 2012;5:606–17.
Farooq V, Vergouwe Y, Raber L, et al. Combined anatomical and clinical factors for the long-term risk stratification of patients undergoing percutaneous coronary intervention: the logistic clinical SYNTAX Score. Eur Heart J. 2012;33:3098–104.
Farooq V, van Klaveren D, Steyerberg EW, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX Score II. Lancet. 2013;381:639–50.
Myat A, Patel N, Tehrani S, Banning AP, Redwood SR, Bhatt DL. Percutaneous circulatory assist devices for high-risk coronary intervention. JACC Cardiovasc Interv. 2015;8(2):229–44. https://doi.org/10.1016/j.jcin.2014.07.030.
O’Neill WW. What is high-risk PCI, and how do you safely perform it? J Invasive Cardiol. 2011;23(10):425–6.
Brennan JM, Curtis JP, Dai D, Fitzgerald S, Khandelwal AK, Spertus JA, Rao SV, Singh M, Shaw RE, Ho KK, Krone RJ, Weintraub WS, Weaver WD, Peterson ED, National Cardiovascular Data Registry. Enhanced mortality risk prediction with a focus on high-risk percutaneous coronary intervention: results from 1,208,137 procedures in the NCDR (National Cardiovascular Data Registry). JACC Cardiovasc Interv. 2013;6(8):790–9. https://doi.org/10.1016/j.jcin.2013.03.020.
Perera D, Stables R, Thomas M, Booth J, Pitt M, Blackman D, de Belder A, Redwood S, BCIS-1 Investigators. Elective intra-aortic balloon counterpulsation during high-risk percutaneous coronary intervention: a randomized controlled trial. JAMA. 2010;304(8):867–74. https://doi.org/10.1001/jama.2010.1190.
Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J, de Waha A, Richardt G, Hennersdorf M, Empen K, Fuernau G, Desch S, Eitel I, Hambrecht R, Lauer B, Böhm M, Ebelt H, Schneider S, Werdan K, Schuler G, Intraaortic Balloon Pump in cardiogenic shock II (IABP-SHOCK II) trial investigators. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. Lancet. 2013;382(9905):1638–45. https://doi.org/10.1016/S0140-6736(13)61783-3.
Seyfarth M, Sibbing D, Bauer I, Fröhlich G, Bott-Flügel L, Byrne R, Dirschinger J, Kastrati A, Schömig A. A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J Am Coll Cardiol. 2008;52(19):1584–8. https://doi.org/10.1016/j.jacc.2008.05.065.
O’Neill WW, Kleiman NS, Moses J, Henriques JP, Dixon S, Massaro J, Palacios I, Maini B, Mulukutla S, Dzavík V, Popma J, Douglas PS, Ohman M. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation. 2012;126(14):1717–27. https://doi.org/10.1161/CIRCULATIONAHA.112.098194.
Thiele H, Sick P, Boudriot E, Diederich KW, Hambrecht R, Niebauer J, Schuler G. Randomized comparison of intra-aortic balloon support with a percutaneous left ventricular assist device in patients with revascularized acute myocardial infarction complicated by cardiogenic shock. Eur Heart J. 2005;26(13):1276–83.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Buccheri, S., Capodanno, D. (2018). Planning Coronary Intervention: The “Golden Rules”—Patient Checklist and Troubleshooting. In: Myat, A., Clarke, S., Curzen, N., Windecker, S., Gurbel, P.A. (eds) The Interventional Cardiology Training Manual. Springer, Cham. https://doi.org/10.1007/978-3-319-71635-0_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-71635-0_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-71633-6
Online ISBN: 978-3-319-71635-0
eBook Packages: MedicineMedicine (R0)