Abstract
Training of interventional radiologists has changed as the specialty has grown. The first training programs were fellowships limited to a small number of institutions and were non-standardized. Interventional radiology (IR) is now a primary specialty of medicine and has dedicated accredited IR residencies that can be accessed from both medical school and following diagnostic radiology training. These changes position IR well for the future.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
The most important individuals in any specialty are its trainees. Although medical students, residents, and fellows often feel that they are at the low end of the professional hierarchy, they are in reality far more valuable than their teachers. Without trainees there is no future. At any given moment, these are the people who have the most potential to make the greatest contributions over time. For this reason, training in interventional radiology (IR) has been a major focus of the specialty since its earliest years and continues to evolve and grow in importance. The purpose of this chapter is to briefly review the history of IR training as the backdrop for the latest step in evolution, the IR residency .
IR was not fully conceptualized or formed at a specific time or place but was gradually defined by many different individuals all over the world. The history of the specialty in the United States is just one of many histories, all equally fascinating and instructive. For the purposes of this chapter, training as it evolved in the United States will be discussed.
The influence of Europe on IR in the United States cannot be understated. Sven Seldinger (of the Karolinska Institutet in Sweden) invented percutaneous catheterization in 1953 [1]. Previous to that Berberich and Hirsch had demonstrated peripheral angiography and venography (1923), Egas Moniz of Portugal had described cerebral angiography (1927), Reynaldo dos Santos performed direct puncture aortography (1929), and Werner Forssmann of Germany catheterized his own heart (1929) [2, 3]. As a result, Europe was an early destination for radiologists seeking training in invasive diagnostic techniques [4].
In the 1960s, training in angiography could be obtained in only a few US centers. Among the first programs were those located at the University of Oregon (Charles Dotter), Stanford University in California (Herbert Abrams), and the University of Minnesota (Kurt Amplatz) [4]. Training was not standardized, and there was no formal regulation or certification. The length of training was also variable, with some programs requiring a 2-year commitment. Most trainees had already completed a diagnostic radiology (DR) residency . The graduates of these programs, as well as individuals originally from Europe, Latin America, and Asia created new training programs in other cities such that by the 1980s the then Society of Cardiovascular and Interventional Radiology (SCVIR , now Society of Interventional Radiology, SIR) recognized the need to develop a standardized curriculum. The SCVIR formed a committee to seek formal recognition of these training programs by the Accreditation Council of Graduate Medical Education (ACGME) [5].
Accreditation for Vascular and Interventional Radiology fellowships first became available from the ACGME in 1991. Eligibility for the fellowship required completion of a diagnostic radiology residency, with a fellowship duration of 1 year in length. Standards for faculty, resources, didactics, and clinical content had to be met in order for a program to receive accreditation. This was a new concept for IR fellowships, which had been used to self-regulation at the program level for many decades. In 1994, the American Board of Medical Specialties (ABMS) recognized Vascular and Interventional Radiology (VIR) as a subspecialty of Diagnostic Radiology, and the American Board of Radiology (ABR) began offering subspecialty certification in VIR by examination. Eligibility for examination was initially open to both interventionalists who had completed an ACGME fellowship and those who had not but was later restricted to graduates of accredited VIR fellowships. As a result, all VIR fellowships became accredited by the ACGME.
The impact of this first step, accreditation, was enormous. There was initially much controversy over the concept of any sort of specialization in diagnostic radiology and subsequently over certification of special competence. The issues of disenfranchisement of diagnostic radiologists performing interventional procedures who were not trained in VIR fellowships and the potential weakening of the structure of diagnostic radiology by differentiated subgroups were of great concern to both interventionalists and non-interventionalists alike. However, the uniformity of training brought by accreditation also solidified the educational community of IR. Without this initial unification, all subsequent changes would have been impossible.
Shortly after the recognition of VIR as a subspecialty, efforts to modify training were already underway. The primary intent of these efforts was to enhance training in non-procedural patient care. By the year 2000, becoming an IR required an internship (PGY 1), diagnostic radiology residency (PGY 2–5), and then a VIR fellowship (PGY 6). Even individuals with great interest in non-procedural care had little direct exposure to patient management during the 4 years between internship and fellowship. As IR practice was increasingly intervention based, with the interventions becoming more complex, the importance of this skill set was anticipated to grow with time.
The first attempt to provide more training in non-procedural patient care was the clinical pathway, proposed by the SIR in 2000 [6]. This 6-year program consisted of 16 months of training in non-radiology patient care specialties, 29 months of DR, 24 months of VIR, and 3 months of research. There was only limited implementation of this pathway, although it was successful in the few programs that offered it.
In 2005, the DIRECT (Diagnostic and Interventional Radiology-Enhanced Clinical Training) pathway was approved by the ABR as a pathway to specialty board certification in DR and subspecialty certification in VIR. This pathway, which required individual approval by the ABR, allowed for 24 months of training in non-procedural patient care, 27 months of DR, and 21 months of VIR. The initial intent of this pathway was to permit individuals transferring from other specialties into DR to apply 2 years of their other training toward the usual total of 6 years by reducing the DR rotations and to have more exposure to VIR. Several institutions developed successful programs that began at the PGY1 level, but overall the implementation of this pathway was also limited.
In 2006, the SIR initiated development of a proposal to further modify training as well as transition VIR from a subspecialty of DR to a primary specialty. As had been anticipated, IR was continuing to expand in breadth and complexity and with it the importance of non-procedural patient care. Practicing IRs were developing levels of content expertise that went well beyond their training in imaging and procedures, functioning as integral members of the clinical patient care team. The classic example was the IR who focused on cancer and was viewed first as a member of the cancer team and second as an IR.
A proposal for a new specialty and training program was presented to the ABR in 2007, which then worked with the SIR and multiple other stakeholders in DR over the next 5 years. A refined and carefully vetted proposal was ultimately approved by the member boards of the ABMS in 2012. The fundamental feature of the proposal was the unique combination of imaging expertise, procedural expertise, and non-procedural patient care that differentiated IR from all other primary specialties. The ABMS approved a new ABR certificate that included both IR and DR (the IR/DR certificate). With approval of the new certificate, the ABMS also approved the concept of a dedicated residency. The overarching significance of the ABMS approval of IR as a primary specialty of medicine was the affirmation by all other ABMS boards that competency in non-procedural patient care was not only a unique feature of IR but expected of individuals trained in IR. In essence, from the outside looking in, non-procedural patient care was recognized as an essential part of IR.
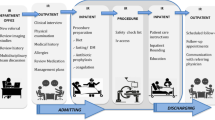
In 2015, the ACGME approved the structure of the training that fulfilled the requirements for IR/DR certification and began accrediting the first programs. Termed the IR residency, this training will have replaced all current VIR fellowships by the year 2020. As this training results in eligibility for a single certificate that includes two specialties (IR and DR), there are several features that are unique to these training programs. For example, the majority of these programs reside in DR departments and have shared leadership between DR (for the DR portions of the training) and IR (for the IR years). There are two basic configurations, the integrated and independent programs.
The integrated program requires a 1-year internship, preferably in surgery, followed by 5 years in a single department. The first 3 years are identical to the first 3 years of DR training, after which the resident spends the majority of the next 2 years in IR or IR-related rotations. One rotation in an ICU is mandated. Entry into integrated residencies is from medical school. This is a major change from the traditional entry from DR residency. For the first time, medical students who are procedurally oriented can consider IR as a career option directly from medical school (although they still must complete an internship).
The independent programs require a 1 year internship and completion of a DR residency. The standard independent IR residency is 2 years in length and also requires one ICU rotation. However, residents who receive extra IR training during DR residency in a formal early specialization in IR (ESIR) pathway are eligible for advanced placement into the second year of the IR residency. The independent program provides great flexibility, as residents can move between institutions (DR residency in one place, IR residency in another), whereas integrated residents much complete both DR and IR in the same institution. The independent pathway allows DR programs without IR residencies to remain competitive, as their graduates can still train in IR. If these programs can offer ESIR , their residents will be able to complete all of their training in the same time frame as integrated residents. Lastly, this pathway provides a training option in IR for those who develop and interest after starting DR.
The certification process is the same regardless of the residency, in that IR residents in both the integrated and independent programs take the same DR core examination as the DR residents. Subsequently, certification in IR/DR requires passing a combined computerized and oral examination after completion of training. The oral examination is considered an essential tool for assessing competency in IR, and was therefore retained for this certificate, although it has been dropped for DR.
The IR/DR certificate is unusual in that it indicates competency in two ABR primary specialties, IR and DR. This is a foundational concept, in that the IR/DR certificate can be used as the parent specialty certificate for other DR subspecialties, such as pediatric radiology or neuroradiology. More important, it emphasizes that general imaging competency is unique to IR compared to all other specialties that perform image-guided interventions. This competency is the special feature that IR brings to medicine and which all of the ABMS member boards wanted preserved in the IR specialty certificate.
IR training has been evolving for the entire history of the specialty and will continue to evolve. With each change new opportunities arise, as well as challenges. Initial accreditation of fellowships unified training programs and made system-wide changes feasible. Recognition as a specialty was based on the importance of non-procedural patient care and maintaining imaging competency. The next steps may be development of areas of content expertise to a level that would benefit from training beyond residency. Perhaps oncology or vascular fellowships would produce individuals with special competency in these areas. However, the very same issues that arose when the idea of recognized VIR fellowships was debated in the 1980s are likely to surface again; concerns about disenfranchising IRs who do not seek additional training or weakening of the structure of IR by allowing subgroups to differentiate. As in the past, IR will find a way, and this exciting specialty will continue to innovate, advance care, and lead in image-guided interventions.
References
Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol. 1953;39:368–76.
Grigg ERN. The RSNA historic symposium on American Radiology: then and now. Radiology. 1971;100:1–26.
Berberich J, Hirsch S. Die Rontgenographische Darstellung der Arterien und Venen im lebenden Menschen. Klin Wchnschr. 1923;49:2226.
Baum S, Athanasoulis C. The beginnings of the Society of Interventional Radiology (SIR, née SCVIR, SCVR). J Vasc Interv Radiol. 2003;14:837–40.
Ferris EJ, Baron MG, Becker GJ, Gardiner GA Jr, Levin D. Cardiovascular and interventional radiology fellowship training programs. Radiology. 1989;170:959–60.
Kaufman JA. The interventional radiology/diagnostic radiology certificate and interventional radiology residency. Radiology. 2014;273:318–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Kaufman, J.A. (2018). Evolution of IR Training. In: Keefe, N., Haskal, Z., Park, A., Angle, J. (eds) IR Playbook. Springer, Cham. https://doi.org/10.1007/978-3-319-71300-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-71300-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-71299-4
Online ISBN: 978-3-319-71300-7
eBook Packages: MedicineMedicine (R0)