Abstract
This chapter examines the stresses inherent to working within the US military, the human body’s reaction to these stresses, solutions used within the US military to address the problem of stresses (both conventional resilience-building programs as well as complementary and integrative health (CIH) approaches. We finish with recommendations for future leaders based on our findings. Stress is a major component of work and life. Military members are particularly affected by stress, given the potential exposure to combat environments. Traditional allopathic treatment options for service members suffering from stress have shown mostly limited benefits. More service members and Americans in general are practicing and/or participating in CIH modalities, such as meditation, yoga, and acupuncture. We identified evidence which strongly suggests that these modalities can help service members reduce acute and chronic stress, develop greater resilience, and enhance performance to meet the continuing demands of national security and defense. High-stress job participants who have benefited from these techniques include explosive ordnance disposal technicians, infantry members, and fighter pilots. Based on our findings, we recommend that (1) leaders should promote evidence-based CIH practices we have identified as first-line options for stress reduction, (2) teach these practices preventatively in military training schools, (3) deploy mindfulness-trained behavioral health providers to members’ job sites, and (4) develop business practices to offer workload credits to behavioral health providers participating in these innovative prevention practices. While CIH practices may not be useful for all service members, evidence suggests that a large population of military members can benefit from them.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Stress
- Mindfulness
- Yoga
- Tai chi
- Meditation
- Complementary and integrative health CIH
- Resilience
- Military
- Acupuncture
- Battlefield acupuncture
- Military complementary and integrative health recommendations
The American Psychological Association’s (APA) survey on “Stress in America” recently reported that 65% of Americans rated work as their top source of stress (APA, 2016). Although work is stressful for many American civilians, American’s military personnel experience the additional stress of involvement in worldwide operations, making theirs one of the most stressful occupations (careercast.com, 2014, 2015, 2016). In 2013, the US Army’s Mental Health Advisory Team––9 (MHAT-9) for Operation Enduring Freedom (OEF) in Afghanistan reported that approximately 10% of soldiers have experienced psychological distress. MHAT-9 (2013) identified several areas of concern for service members, including symptoms of depression, anxiety, post-traumatic stress disorder (PTSD) , sleep, suicidal ideation, and concussive events. Many service members experience stress even though they are not clinically diagnosed with a psychiatric disorder. MHAT-9 (2013) reported that service members experience stress due to uncertain redeployment dates, lack of time off, insufficient sleep, separation from family, and long periods of deployment. Combat missions and training injuries can also result in acute and chronic pain conditions, which are additional causes of the ongoing stress experienced by service members. Reservists who juggle between two jobs in the civilian and military worlds have additional stress in trying to bring equipoise to both their work and their home life.
Military service members face several obstacles to obtaining the mental health care that they need to support their recovery from the stress and traumas incurred during their service. Due to the stigma associated with mental health concerns in the military, service members may be less likely to seek behavioral health care. An unwillingness to participate in mental health programs combined with increasing health care costs suggest a need for additional approaches for addressing stress-related conditions in the military. Establishing more accessible, effective, and low-cost, evidence-based self-care interventions could help to address the behavioral health concerns of our service members and performance and readiness issues in the military.
Fortunately, the body of evidence is growing, and systematic reviews of the self-management literature are showing the breadth of the strategies being used, as well as the implementation of multiple modalities in combinations. When practiced properly, self-care stress management and stress-relieving practices appear to be of low risk with fewer adverse effects (Bellanti et al., 2016; Crawford et al., 2013).
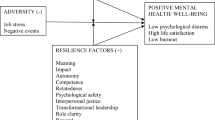
The high incidence of stress in military jobs coupled with the need for nonstigmatizing approaches to build resilience suggests the opportunity for mind–body practices. Mind–body practices introduced through training, coaching, or therapy can be used as ancillary approaches to conventional medical practices to aid service members in reducing stress. Practitioners could both assist and refer patients for treatments with behavioral health professionals while also consulting with leaders and their unit master to implement these performance enhancement approaches . Developing self-care stress management and resilience practices through training, coaching, or consultation for service and family members into the military direct care system or into the operational care environment will require innovations to the military business-practice models. These new business-practice models will affect how workload, costs, and outcomes are measured and valued. This chapter examines the effects of military work stress, the body’s response to stress, resilience in the military, research self-care complementary and integrative health (CIH) approaches (e.g. mindfulness approaches, acupuncture), application in military operations, and future directions for the use of mind–body practices in the military.
Psychological Distress in the Military
Military personnel representing a small portion of the American population make large sacrifices on behalf of the nation through combat deployments and separation from family and/or friends. For some service members and their families, military service may require the ultimate sacrifice of injury or death in combat. According to the Defense Casualty Analysis System (2017), 6896 service members have been killed, and 52,527 service members have been wounded in action since the start of OEF and continuing with Operation Iraqi Freedom (OIF) , Operation New Dawn (OND), and the currently active Operation Inherent Resolve (OIR) and Operation Freedom’s Sentinel (OFS) . These include injuries received during both hostile and nonhostile conditions. The impact of these tragedies on service members, their family, and community, as well as the nation at large, can no longer be viewed as simply a cause of disease (i.e. caffeine and nicotine addiction, substance abuse, obesity, pulmonary deployment disease), a psychological health condition (i.e., PTSD, depression), or merely personal or social distress (i.e., loss of purpose, unemployment, homelessness, suicide). The enormity of suffering by our service members who have completed their tours of duty must be taken as a call-to-action for improving military programs that can build resilience, readiness, hardiness, and well-being. This programming cannot be delayed or avoided. Sufficient evidence currently exists demonstrating the potential of mind–body programs to enable successful adaptability to psychological challenges faced by our military. Programming should focus on the implementation of these mind–body strategies for service members at all levels, from initial training programs to recovery and reintegration. The hope is that by integrating evidence-based mind–body programs into resiliency training at the outset, our military behavioral health care programs will find fewer incidences of trauma, PTSD, suicide, and other stress-related and mental health conditions to manage in ensuing years. Service members with greater resilience will experience fewer behavioral health challenges and improved overall well-being.
While psychological and physical health is a requirement for optimal human performance, the psychological health of military personnel must be considered when evaluating their overall well-being. Addressing the psychological health of military personnel presents a unique challenge. This is particularly true because some mental health problems may be under-addressed due to stigmatization. Because of the stigma associated with a lack of mental resilience in the military, service members are reluctant to seek help or take a proactive approach to addressing emotional trauma.
The US Department of Veteran Affairs National Center for PTSD has reported that approximately 11–20% of military personnel who served in Afghanistan and Iraq have PTSD (USDVA, 2016). Past research by RAND researchers has suggested the probable percentages of these conditions as follows: PTSD (13.8%), major depression (13.7%), and traumatic brain injury (TBI) (19.5%) (Schell & Marshall, 2008). Combat veterans may also suffer from other physical and psychological problems such as chronic pain and addiction. Research has shown that more than 45% of returning veterans report experiencing some pain (Gironda, Clark, Massengale, & Walker, 2006; Toblin, Quartana, Riviere, Walper, & Hoge, 2014 ). Approximately 7% percent of returning veterans met the criteria for substance abuse during 2004–2006 (Substance Abuse and Mental Health Services Administration, 2014). Just under half (47.3%) of the service members returning from Iraq and Afghanistan who have PTSD or depression have sought help for these conditions (Schell & Marshall, 2008). Those who did not seek care for mental health provided the following top reasons for not seeking behavioral health services: side effects of medication, possible harm to career, loss of security clearance, preference to rely on friends and/or family, and concerns that coworkers would have less confidence in the service member (Schell & Marshall, 2008). More than half of the service members needing treatment reported seeing a health professional regarding mental health conditions in the previous 12 months. However, almost half the service members who did present their condition to a health professional reported that they did not receive adequate treatment (e.g., receiving fewer than eight sessions of psychotherapy or insufficient pharmacological treatment) (Schell & Marshall, 2008).
In 2010, to address the health of the military armed forces , the Chairman of the Joint Chiefs of Staff established the Total Force Fitness Framework as the new paradigm to promote and maintain health, readiness, and performance in the Department of Defense (DoD) . Total Force Fitness encompasses eight integral domains of fitness: social, behavioral, physical, environmental, medical, spiritual, nutritional, and psychological. While residing as the Chairman of the Joint Chiefs of Staff, Admiral Mullen stated that “…the secret to optimal fitness lies in the constant awareness of the changing environment and the continuous pursuit of flexible adaptation to the inevitable shifts.” The application of the new paradigm continues to be a work in progress. This holistic view of fitness, set on building mind and body capacity, endurance, prevention or resistance to disease or personal/social distress, has been described in the Chairman’s instruction on the Total Force Fitness Framework (CJCSI , 2011; Mullen, 2010). The uses of mindfulness and acupuncture CIH programs for psychological distress are unlikely to stigmatize service members and are considered alternative or ancillary self-care approaches to traditional treatments. We propose that CIH programs (mind–body approaches such as meditation, yoga, tai chi, and acupuncture) (Lang et al., 2012; Hempel et al., 2014; Staples, Hamilton, & Uddo, 2013; Hempel, Taylor, Solloway, Miake-Lye, Beroes, Shanman, & Shekelle, 2014; Hempel, Taylor, Solloway, Miake-Lye, Beroes, Shanman, Booth, et al., 2014) may serve as both treatments for those presenting with mental health symptoms and as practices for self-awareness and other awareness and/or performance skills, while enhancing resilience, well-being, and readiness for service members and family members.
The Body’s Response to Stress: Physiological Results of Chronic Psychological Distress
Stress can be defined as the state in which the demands of life (i.e., a person’s interaction with the physical and psychosocial environment) exceed one’s coping skills, resulting in psychophysiological consequences (Lazarus & Folkman, 1986; McEwen, 2007). While stress can have vast mental repercussions, chronic stress can also significantly alter the body’s biological processes. When a stressor is present, the body is designed to effectively manage this short-term (acute) stressor by altering its physiological mechanisms to respond with a flight, fight, or freeze response. However, persistent (chronic) stressors, such as a stressful work environment or deployment, may cause negative structural and biochemical changes to the brain, as well as other areas within the body, that can lead to disease and disability (McEwen, 2007).
The sympathetic nervous system responds immediately to perceived acute stressors through activation of the sympathoadrenomedullary (SAM) pathway resulting in increased activity of the sympathetic nervous system (SNS; e.g., increased heart rate and blood pressure, opened airways, dilated pupils). The SNS also stimulates secretion of epinephrine (adrenaline) from the adrenal medulla (Karlamangla, Singer, McEwen, Rowe, & Seeman, 2002). The perception of environmental and psychosocial stressors also activates a neuroendocrine response cascade through the hypothalamic–pituitary–adrenal (HPA) axis . The hypothalamus releases corticotrophin-releasing hormone (CRH) and vasopressin (De Kloet, Joëls, & Holsboer, 2005; Tafet & Bernardini, 2003). These two hormones help to coordinate behavioral and metabolic responses throughout the body. CRH induces the release of adrenocorticotropin (ACTH) from the anterior pituitary, which then induces the release of glucocorticoids (e.g., cortisol) from the adrenal cortex (De Kloet et al., 2005). When the stressor is no longer perceived, negative feedback loops within the HPA return the body to baseline.
Chronic stress leads to chronically elevated glucocorticoid levels and contributes to the development of conditions such as obesity, cognitive impairment, hypertension, diabetes, lipid imbalance, brain aging, loss of bone minerals, and immune system dysfunction (Karlamangla et al., 2002). Studies have found that prolonged stress also has consequences for brain functioning, related to changes in glucocorticoid and mineralocorticoid receptors in the brain, especially within the limbic system (McEwen, 1999). If stress becomes chronic, the hippocampus, which has a role in memory formation and modulation of emotional control and self-regulation, may atrophy due to glucocorticoid effects on neurogenesis. Hippocampal atrophy , in turn, can significantly impair memory functioning (McEwen, 1999) and the capacity for self-regulation (Hölzel et al., 2011). Repeated stress can also enhance activity of the amygdala, leading to heightened emotional reactivity; and decrease activity of the prefrontal cortex, leading to impairment in executive function, inhibitory control, and cognitive flexibility (McEwen, 2007). By considering the research on the physiology of stress, and the mechanisms and biomarkers of resilience to stress, we may be able to develop more effective mental health and performance enhancement approaches for our military who serve in stressful environments.
Resilience Biomarkers
Scientists have identified several possible biomarkers for resilience (Charney, 2004). One of these biomarkers is the ratio of dehydroepiandrosterone sulfate (DHEA-S) to cortisol. Cortisol and DHEA-S are both adrenal steroid hormones that are released as part of the HPA axis activation in response to stress. DHEA-S is a precursor to anabolic steroids and has both peripheral and central (i.e., brain) effects. Animal studies have suggested that DHEA-S plays a beneficial role in stressful conditions (Charney, 2004). This may, in part, be due to antiglucocorticoid effects, both peripherally and centrally (Morgan et al., 2004). A study on service members found that those who performed better under intense stress had higher DHEA-S to cortisol ratios during Survival, Evasion, Resistance, and Escape (SERE) training (Morgan et al., 2004).
Another potential biomarker of resilience is Neuropeptide Y (NPY) (Yehuda, Brand, & Yang, 2006). NPY has an anxiolytic effect and may help to mitigate the negative consequences of stress on the body. A variety of animal and human studies have suggested a role for NPY in the regulation of stress, anxiety, fear, learning, memory, and cardiovascular function (Schmeltzer, Herman, & Sah, 2016). Human studies have found decreased levels of NPY in patients with post-traumatic stress disorder (PTSD; summarized in Schmeltzer et al., 2016). A recent study by Yehuda et al. (2014) found that pretreatment DHEA-S/cortisol ratio and NPY levels were predictors of PTSD treatment response in combat veterans. In another relevant study, Norwegian navy cadets who were high in hardiness-challenge as well as commitment and control showed higher levels of NPY compared to those low in hardiness-challenge (Sandvik, Bartone, Hystad, Phillips, Thayer & Johnsen, 2013). As research on resilience biomarkers advances, we may find better ways to address resiliency through mind–body interventions.
Mind–Body Approaches : Complementary and Integrative Health Resilience Programs
The military must establish more psychological, couples, and family fitness programs to help service members and their families develop the knowledge, skills, abilities, and attitudes they need to effectively prepare for, and recover from, the severe stressors they inevitably encounter (Bates et al., 2010; Bowles et al., 2015). Military services and related organizations have separately adopted principles of the Total Force Fitness framework. This framework promotes concentration, self-awareness, and self-modulation to ultimately improve the fitness, resilience, and well-being of service members. Research in meditation, yoga, acupuncture, and perhaps tai chi and qigong shows that these CIH techniques could be beneficial for building behavioral fitness, resilience, and well-being.
Service members have already shown great interest in CIH therapies. Data collected from the Millennium Cohort Study from 2004 to 2006 found that 30% of active duty and reserve military personnel reported the use of a practitioner-assisted CIH therapy program, while 27% reported the use of a self-administered CIH therapy program (Jacobson et al., 2009). Among a civilian sample, Park (2013) found that 38.3% of adults had used a mind–body program within the last year. More recently, Clarke, Black, Stussman, Barnes, and Nahin (2015) found yoga to be the leading mind–body approach and meditation to be the third most often used approach.
Large portions of the military population who struggle with mental health problems underuse behavioral health clinics due to stigma (Hoge, Auchterlonie, & Milliken, 2006; Hoge et al., 2004; Sharp et al., 2015). Given that many military personnel are and will engage with CIH, these mind–body therapies provided in nonmedical settings like gyms, classrooms, or homes may serve as effective additional approaches for ancillary mental health treatment.
In 2010, the Office of The Army Surgeon General published its Pain Management Task Force final report. The report recommended Tier I nondrug complementary and integrative modalities be included as Tier 1 TRICARE benefits, and that these modalities be delivered in an interdisciplinary and multimodal approach. The Tier I modalities include acupuncture, yoga/yoga nidra, nonallopathic chiropractic care, biofeedback, and mind–body therapies (mediation, mindfulness). A patient could receive these modalities from a provider passively, or they could be taught to the patient as part of an active individualized self-care plan. The report lists Tier II nondrug modalities as movement therapy (tai chi, qigong, and martial arts), art, music, and aroma therapies, monochromatic near-infrared (MIRE) treatments, and cranial electrical stimulation (Office of The Army Surgeon General, 2010). In the mid-2010s tai chi and qigong were not considered medical therapies and were not covered benefits under the TRICARE program. However, tai chi and qigong were available within some parts of the Veterans Health Administration system of care and could be found in military medical care facilities.
Crawford et al. (2013) conducted a systematic review of multimodal training programs that could be applied to military populations that incorporated complementary and alternative self-management techniques as one component of interventions to reduce emotional stress. Their review focused only on RCTs, limiting their review to 116 trials. This review showed evidence of potential benefit of a multimodal approach for addressing anxiety, distress, and overall coping mechanisms in a broad spectrum of psychological and medical conditions such as cancer, HIV, chronic pain, heart disease, PTSD, and schizophrenia.
CIH approaches are offered to service members at locations such as the Malcolm Grow Military Medical Center, National Intrepid Center of Excellence, Naval Medical Center San Diego (NMCSD), Walter Reed National Military Medical Center (WRNMMC) , the Deployment Health Clinical Center, Fort Hood Resiliency Campus, and Fort Bliss Restoration and Resilience Center for Returning Service. CIH approaches are also being used throughout the Department of Veterans Affairs Medical Centers. Service members who are looking for techniques to improve their well-being, productivity at work, and work–life satisfaction can be prompted to take advantage of these programs. CIH programs provide a combination of mind–body skills of interest to service and family members, as well as skills that they may have already practiced within the military community. Many of these programs are easily taught, are easy to practice, can be done in any environment, are cost-effective, and can be individualized to the service member based on acceptability and personal choice.
The Relaxation Response and Meditation
A growing body of evidence demonstrates predictable and potential health and wellness benefits of a regular meditation practice. Meditation is a term encompassing a wide variety of practices and has been broadly defined to include any activity that will elicit the relaxation response—a mind–body state characterized as incompatible with the stress response (Benson & Proctor, 2010). The relaxation response is a mind–body state that allows the individual to decrease cognitive and somatic arousal, thus modifying the HPA axis and the autonomic nervous system (ANS; Khalsa, 2004a). Regular meditative practice leads to improved ANS regulation (Benson, Dryer, & Hartley, 1978; Benson, Greenwood, & Klemchuk, 1975; Wallace, Benson, & Wilson, 1971), attention and focus (Brefcynski-Lewis, Lutz, Schaefer, Levinson, & Davidson, 2007), social connection (Bob et al., 2012; Van Leeuwen, Singer, & Melloni, 2012), emotional regulation (Jazaieri et al., 2014), pain reduction (Khusid & Vythilingam, 2016b), and immune and inflammatory function associated with changes in genetic expression (Bhasin et al., 2013; Dusek et al., 2008). Mindfulness practices have also been shown to produce positive effects on psychological well-being (Carmody & Baer, 2008), reduce symptoms of depression and/or PTSD (Banks, Newman, & Saleem, 2015; Khusid & Vythilingam, 2016a), and enhance cognitive functioning (Jha, Krompinger, & Baime, 2007; Ortner, Kilner, & Zelazo, 2007; Zeidan, Johnson, Diamond, David, & Goolkasian, 2010).
Multiple meditative modalities, including transcendental meditation, mindfulness, guided imagery, progressive muscle relaxation, autogenic training, body scan, tai chi, qigong, loving kindness meditation, and yoga can successfully elicit the relaxation response (Benson & Proctor, 2010). Two main factors appear to link these diverse practices:
-
1.
A repetitive mental focusing tool. This can involve focus on an external stimulus or on one’s breath, a thought, or other bodily sensation such as physical movement.
-
2.
A quiet, aware, nonjudgmental attitude toward sensations that arise during the meditative practice. This practice involves trust in the process and freedom from worry, and allows the mind to drift to other areas of focus and simply acknowledge this shift and gently redirect the attention to the chosen mental focusing tool without giving the momentary distraction another thought (Benson, Beary, & Carol, 1974; Park et al., 2013).
Goyal and colleagues (2014) recently published a systematic review and meta-analysis evaluating the evidence regarding the benefit of meditation programs for psychological stress and well-being. Movement-based meditation programs, such as yoga and tai chi, were excluded. The review only evaluated randomized controlled trials (RCT) of structured meditation programs that used control groups where the time and attention provided to participants were comparable to the meditation group. The analysis was separated into nonspecific active controls and specific active controls that included interventions such as exercise and progressive muscle relaxation. The research team reviewed over 18,000 studies and found 46 trials totaling 3515 participants who met their strict criteria. The study found that meditation programs have moderate evidence for improvement in anxiety, depression, and pain, and low evidence for improvement in stress/distress, negative affect, and quality of life. Meditation interventions have been found to have comparable results to antidepressant interventions, with the added benefit that meditation lacks the adverse effects associated with antidepressants, and may be especially useful for patients who do not want to take medications. According to Goyal et al. (2014), the body of evidence remains insufficient to determine the effects of meditation on positive affect, attention, sleep, and substance use. One significant weakness in the studies evaluated was the short period of follow up, typically no more than a few months after the intervention. Meditation is based on regular practice, and much like regular exercise, the positive effects of mediation on psychological and physical health may continue to expand over time. When meditation practice becomes a long-term habit, there is the possibility for a profound benefit. More studies are needed to evaluate the potential clinical benefits of long-term practice on military health concerns (Millegan, Morrison, Bhakta, & Ram, 2014).
Resilience is strongly associated with cognitive reappraisal or the ability to monitor and assess negative thoughts and replace them with more positive ones (McRae, Ciesielski, & Gross, 2012). Reappraisal as a strategy for emotion regulation and resilience involves changing the way one views events or situations (Gross, 2002). Mindfulness practices have been shown to change self-perspectives associated with resilience. Hölzel et al. (2011) proposed a mechanism of action by which mindfulness meditation works to enhance the capacity for self-regulation. Specifically, Hölzel suggests that mindfulness practices focused on interoceptive awareness are associated with neuroplasticity in the brain, specifically within the anterior cingulate cortex, insula, temporoparietal junction, and frontolimbic network. Hölzel asserts that interoceptive awareness enhances the capacity for self-regulation and self-control, through a process of reappraisal, exposure, extinction, and reconsolidation, resulting in changes in self-perception. Mindfulness practices involving focused interoceptive awareness may work through these mechanisms of enhanced self-regulation and reappraisal to enhance resilience.
Although these two studies focused exclusively on meditation, many programs include meditation as part of a multimodal intervention combined with other biopsychosocial modalities such as movement-based mindfulness, cognitive behavioral therapy, positive psychology, sleep hygiene, and the promotion of social connection. The combination of multiple practices to improve stress management and resilience may produce synergistic benefits beyond any single-modality effort on its own, and should be evaluated in clinical trials.
Programs such as the Mind–Body Medicine program at the Naval Medical Center in San Diego (NMCSD) , California, are developing innovative ways to integrate meditation and other resiliency self-care modalities into health care plans. Mind–body practices are now part of the treatment protocol for emotional stress, chronic pain, and pregnancy, and are taught to assist in improving the resiliency of health care providers themselves. The core program lasts for 7 weeks and consists of weekly two-hour sessions. The program focuses on establishing a regular meditation practice, integrating sleep hygiene habits, cognitive restructuring, and positive psychology techniques, and strengthening social connections. An internal program evaluation (by the US Navy) of participants in a Mind–Body Medicine program at NMCSD showed that those who completed the program greatly value the experience, internalized the material, created a regular meditation habit, and demonstrated statistically significant improvement in depression, anxiety, overall functioning, and quality of life compared to controls (Millegan et al., 2016). The program was awarded the 2015 Military Health System Trailblazer Award, which recognizes the most promising novel initiatives that demonstrate a positive impact on health and readiness throughout the Armed Forces. Meditation programs at Departments of Veterans Affairs also show promise for reducing PTSD symptoms in veterans (Heffner, Crean, & Kemp, 2016).
The case of a US Marine suffering chronic pain from combat injuries and with no prior exposure to meditation illustrates how these principles can be effective. Four months after completing the meditation program, the Marine had sustained a daily meditation practice. He also reported that, even though the pain intensity remained the same, he experienced substantial improvements in emotional health, perceived disability, and quality of life (Millegan et al., 2014).
Nassif et al. (2015) also explored the effectiveness of meditation for relief of chronic pain in veterans. This study found that veterans with moderate traumatic brain injury (TBI) reported medium to large effects on reductions in pain intensity, and large effects on reducing the extent to which pain interfered with their daily life activities (walking, sleep, interpersonal relationship, and general enjoyment of life). This study concluded that meditation is a promising self-management approach for chronic pain in veterans, even those with moderate TBI.
CIH offers a wide variety of beneficial mind–body practices that offer service members a range of options, thus allowing service members to find the modalities they prefer and are most likely to incorporate into their self-care routines. Several DoD-sponsored websites have been created to offer mindfulness approaches. Examples of these include the Relax–Relax and the NMCSD Mind Body Medicine site (Navy and Marine Corps, n.d.; Naval Medical Center San Diego, 2016). The National Center for Telehealth & Technology (T2) has created multiple DoD-sponsored applications such as Breathe2Relax, Mindfulness Coach, and the Virtual Hope Box (See also Campise et al., Chap. 26, this volume). These resources have been developed to aid service members in gaining exposure to multiple modalities to provide assistance with maintaining a practice through recorded guided meditations and to download an electronic means of tracking progress while developing a habit.
The Use of Yoga
Yoga is a multidimensional system of practices, including physical exercises, breathing techniques, visualization techniques, and meditation/relaxation practices. The physical exercises and postures of yoga emphasize flexibility, strength, and endurance, and facilitate breathing techniques that can result in relaxing psychological and physiological changes.
Extensive research conducted outside the United States indicates that individuals who practice yoga experience many health benefits, including muscle endurance, flexibility, and maximal oxygen consumption (Tran, Holly, Lashbrook, & Amsterdam, 2001). Research on yoga practitioners has also reported positive results for the reduction of stress activation within the ANS (e.g., lowered secretion of cortisol and catecholamines; Khalsa, 2004b). The physiological counterbalance to stress is the relaxation response—a form of meditation (previously described) that results from practicing yoga. This response allows the individual to decrease cognitive and somatic arousal, thus modifying the HPA axis and the ANS.
In the civilian population , yoga interventions have been shown to produce many psychological and physiological benefits. A review study examining multiple schools of yoga from nine different countries found that 12 out of 17 studies reported positive psychological or physiological changes, and that yoga was a promising modality for stress reduction (Sharma, 2014). Reports have also shown that yoga can reduce stress for people who work in high-stress occupations, such as school employees (Nosaka & Okamura, 2015) and hospital staff (Bernstein et al., 2015). Studies have found yoga to be effective in improving sleep quality (Khalsa, 2004a), mood, psychological adjustment, physical and emotional awareness, trust (Dale et al., 2009), quality of life (Chung, Brooks, Rai, Balk, & Raie, 2012), flexibility (Chen et al., 2010), and physical health (Chung et al., 2012). Additionally, yoga has been found to decrease the symptoms of eating disorders (Dale et al., 2009), depression (Coeytaux et al., 2014; John, Sharma, Sharma, & Kankane, 2007; Vedamurthachar et al., 2006), anxiety (Bonadies, 2004; Chung et al., 2012; Stoller, Greuel, Cimini, Fowler, & Koomar, 2012), and migraines (John et al., 2007). Studies of patients with breast cancer found yoga reduced symptoms of depression, anxiety, and postchemotherapy nausea frequency when compared against a control or comparison group (Rao, Nagarathna et al., 2007; Rao, Raghuram, Nagendra, Gopinath et al., 2009; Rao, Raghuram, Nagendra, Usharani et al., 2015). Researchers who evaluated the effects of yoga on patients with breast cancer undergoing radiotherapy found that the yoga group reported decreases in anxiety and perceived stress. These patients had lower salivary cortisol levels, suggesting lower levels of stress (Vadiraja et al., 2009). Yoga practices may also be helpful to civilian adults who have suffered from traumatic brain injuries. After participating in weekly yoga classes for several months, adults with TBI showed improvements in respiratory functioning, and reported increases in physical and psychological well-being (Silverthorne, Khalsa, Gueth, DeAvilla, & Pansini, 2012). Importantly, researchers are exploring the effects of yoga in military and veteran populations who experience high levels of stress.
Results of civilian programs have influenced the implementation of yoga programs for active duty, reservists, and veterans. Several studies have shown the benefits of various types of yoga on active duty and veteran populations. One study, which supported the use of hatha yoga for proactive health, evaluated the effects of a 3-week yoga intervention on Air Force and Army service members deployed in a forward-operating base in Iraq. This study concluded that the yoga treatment program resulted in decreased state and trait anxiety below already normal pretest scores, suggesting a positive effect on stress reduction in a particularly stressful operating area. The practice of yoga in this population also resulted in higher overall quality-of-life levels when compared to a control group (Stoller et al., 2012).
Yoga may also be an effective therapy for the reduction of PTSD symptoms. In a pilot study, veterans attended a yoga program twice a week for 6 weeks totaling 12 one-hour sessions. In this study, veterans experience a significant decrease in PTSD hyperarousal symptoms and aspects of sleep quality, though not total PTSD scores. (Staples et al., 2013). Military combat veterans who participated in weekly yoga nidra meditation (a deep relaxed state between awake and sleep, in which one remains conscious) reported decreased rage, emotional reactivity, and anxiety. They also reported increased self-efficacy, self-awareness, and relaxation (Stankovic, 2011). A study involving a yoga intervention for 12 subjects who were either current or former military personnel with PTSD found reduced PTSD symptoms for participants (Johnston et al., 2015). In a comprehensive 2014 review of nondrug pain care modalities, the authors concluded the literature supports a weak recommendation of yoga to treat chronic low back pain, osteoarthritis pain, fibromyalgia, chronic migraine, and tension headaches. Yoga was demonstrated to be a safe and variably effective practice (Lee, Crawford, & Schoomaker, 2014).
The Use of Tai Chi and Qigong
“Tai chi and qigong are centuries-old, related mind and body practices. They involve certain postures and gentle movements with mental focus, breathing, and relaxation. The movements can be adapted or practiced while walking, standing, or sitting. In contrast to qigong, tai chi movements, if practiced quickly, can be a form of combat or self-defense” (National Center for Complementary and Integrative Health, 2016). The Department of Veterans Affairs Health Services Research and Development Services, Evidence-based Synthesis Program , Quality Enhancement Research Institute (QUERI), published its Evidence Map of Tai Chi in September 2014 (Hempel, Taylor, Solloway, Miake-Lye, Beroes, Shanman & Shekelle, 2014). The report by Hempel, Taylor, Solloway, Miake-Lye, Beroes, Shanman, & Shekelle (2014) synthesizes information from 107 systematic reviews published in peer-reviewed literature to inform VA leaders during policy deliberations. As a practice, tai chi is designed to incorporate low-impact movements with a focus on the breath and mind to achieve greater awareness, inner peace, and well-being (Hempel et al. 2014). The authors report statistical significance for health effects for COPD, pain, balance, confidence, depression, and muscle strength––but caution––there are few high-quality, randomized control trials. To date, no research has been published on the effects of tai chi or qigong on a military population.
The report by Hempel et al. (2014) found no evidence to support tai chi as an effective treatment for diabetes, aerobic capacity, falls in institutions, or life participation. In a comprehensive 2014 systematic review, 3145 RCTs were identified for self-care movement therapies for chronic pain. After screening, seven qigong and ten tai chi RCTs were detailed by the authors and then accessed by a panel of experts. The experts gave tai chi a weak recommendation in its application in chronic low back pain, osteoarthritis pain, fibromyalgia, chronic migraine, and tension headaches. For qigong, the expert panel concluded the quantity and quality of the evidence was insufficient to make a recommendation for its use in chronic pain syndromes studied: neck pain, fibromyalgia, and complex regional pain syndrome (Lee et al., 2014).
In a 2015 RAND Corporation report , Ayer et al. noted tai chi was an alternative care modality offered to patients referred for problems associated with post-traumatic stress disorder and traumatic brain injury at the National Intrepid Center of Excellence, Bethesda, MD. In 2016, tai chi was offered within the Integrative Health and Wellness Program at the Washington DC Veterans Affairs Medical Center (Integrative Health and Wellness Program, 2016). Clinician advisory bodies and administrators there, in coordination with the VA National Credentialing Office, approved procedures by which the credentials of tai chi practitioners could be reviewed so that these modalities could be offered to medical center beneficiaries receiving wellness program services (Integrative Health and Wellness Program, 2016). The US Military installations that host Morale, Welfare, and Recreation (MWR) programs can offer tai chi on military bases. In 2014, Air Force policy categorized tai chi as a “fitness program beyond core” that can be made available at the squadron or flight commander’s discretion for a fee (Air Force Fitness and Sports Programs, 2014).
The Use of Acupuncture for Pain and PTSD
While Western medicine emphasizes medication in most medical settings as the mainstay of treatment for pain, patients increasingly request CIH therapies when traditional therapies fail. Though the evidence for acupuncture is mixed due to limitations in methodology and feasibility, it is a popular CIH therapy in the United States for both acute and chronic pain (Acupuncture: EBM Guidelines, 2014; NIH Consensus Development Panel, 1998). A recent evidence-based synthesis review reported that back pain, headaches, and chronic pain had the most literature supporting acupuncture therapy. In addition, acupuncture therapy also positively affected pain, overall wellness, and mental health (Hempel et al., 2014). An extensive meta-analysis compiled in 2010 also found compelling evidence that acupuncture is useful in treating chronic back and neck pain, and recommends acupuncture as a reasonable referral option” (Vickers et al., 2010). In the past, the American Pain Society and the American College of Physicians (ACP) had issued clinical practice guidelines recommending acupuncture as one of several CIH approaches that physicians should consider when patients with chronic low back pain do not respond to pain medication or other standard approaches (Chou & Huffman, 2007). The newest clinical practice guideline from the ACP now recommends nonpharmacological therapies (including acupuncture, massage, and osteopathic manipulation) as first-line for acute, subacute, and chronic low back pain (Qaseem, Wilt, McLean, & Forciea, 2017). The US Department of Veterans Affairs Opioid Safety Initiative recommends the use of acupuncture as a first-tier approach to treatment of chronic pain syndromes as part of an initiative to reduce the use of addictive opioids in treating pain (U.S. Department of Veterans Affairs, 2014).
Auriculotherapy (ear acupuncture) uses somatotopic representations of the human body (homunculus) via corresponding points on the ear. Auricular acupuncture, coined “Battlefield Acupuncture” because of its effective use in combat, has been studied for its use in treating both acute and chronic pain. This type of acupuncture is being used by a growing number of clinicians to treat pain conditions in both combat and noncombat environments (Niemtzow, 2007).
Research has been limited in the field of auriculotherapy. A small, randomized controlled trial (RCT) of 94 female patients with acute migraines demonstrated that auriculotherapy provided short-term pain relief when specific auricular acupoints were used (Allais et al., 2011). Interestingly, the therapeutic efficacy of somatic acupuncture (acupuncture done on the body itself) was not increased with the addition of auriculotherapy in a study of cervical myofascial pain (Ceccherelli et al., 2006). In addition, evidence from Cochrane reviews concerning the use of acupuncture for lower back pain and neck disorders illustrates that acupuncture has a moderate effect at best for short-term results (Furlan et al., 2005; Trinh, Graham, Irnich, Cameron, & Forget, 2016). Auriculotherapy has also proven to be effective for chronic pain in patients with cancer who report pain intensity decreasing by 36% from baseline after 2 months versus placebo (Hinman et al., 2014). In addition to auriculotherapy, patients have also used somatic acupuncture to treat chronic pain. According to Vickers et al. (2012), when compared with placebo, acupuncture demonstrated larger decreases in osteoarthritis pain, chronic headaches, and back and neck pain. Additional RCTs reinforced these findings (Berman et al., 2004; Khusid, 2015; Vickers et al., 2004).
The use of acupuncture has expanded to include treatment for psychiatric disorders, such as post-traumatic stress disorder (PTSD). Moderate evidence supports acupuncture use for PTSD treatment. A large systematic review of RCTs in 2013 stated that the evidence for using acupuncture as a treatment for PTSD is “encouraging” but not fully formed (Hempel, Taylor, Solloway, Miake-Lye, Beroes, Shanman, Booth, et al., 2014). However, as early as 2007, a RCT with three arms (acupuncture versus cognitive behavioral therapy (CBT) versus wait-list controls) yielded a large treatment effect in favor of acupuncture over control. Furthermore, both acupuncture and CBT maintained symptom reduction at a 3-month follow-up (Kim et al., 2013). A 2007 study illustrated that manual stimulation of acupuncture points (acupoint tapping) combined with psychological exposure resulted in rapid attenuation of threat responses to innocuous stimuli (Hollifield, Sinclair-Lian, Warner, & Hammerschlag, 2007). More recently, a 2014 randomized effectiveness trial examining 55 service members found that a brief course of acupuncture reduced symptoms of PTSD (Engel et al., 2014).
Acupuncture, in both somatic and auriculotherapy forms, is widely used throughout the United States and the world for various ailments and diagnoses. Given its relative safety and low cost, acupuncture is widely accepted as an adjunct treatment for pain and has become an emerging option for PTSD. Acupuncture may be a form of treatment that behavioral health providers could add to their skill sets. Initial evidence is promising and supports the current use of acupuncture as standard-of-care treatment in the military. Rigorous studies are needed to further define the mechanisms of action and clinical benefits of acupuncture for pain and PTSD.
Feasibility and Relevance of Meditation in an Operational Setting
Although evidence exists regarding health benefits of meditation for people coping with chronic stress and numerous health conditions (Crawford et al., 2013; Goyal et al., 2014; Samuelson et al., 2010), questions remain as to whether mind–body programs can have a positive impact in an operational setting among healthy, young service members, and whether it is possible to convince young service members to begin and sustain a meditation practice. A research team from Georgetown University set out to answer these questions (Johnson et al., 2014). They implemented Mindfulness-Based Mind Fitness Training (MMFT) among infantry Marines undergoing precombat deployment training with evaluation specifically focused on the Marines’ response to the high-intensity Infantry Immersive Trainer (IIT). MMFT is an 8-week course administered through eight 2-hour sessions and a 4-hour workshop. The course refines mindfulness skills in order to emphasize the developments of introspective awareness, attentional control, and tolerance of present-moment experiences. Participants were expected to practice 30 min of mindfulness exercises daily throughout the program (Johnson et al., 2014). In this MMFT study, eight Marine infantry platoons were randomly selected and further randomized to receive either MMFT along with predeployment training or training as usual. The sample was tested at baseline, 8 weeks after baseline, during the IIT, and after its completion. The results showed that those who participated in MMFT exhibited greater heart rate reactivity during combat drills and enhanced recovery of heart rate and breathing rate after stressful training. Those who participated in MMFT had lower plasma NPY levels after training, suggesting more efficient self-regulation. They also demonstrated attenuated blood oxygen level dependent signal in the right insula and anterior cingulate on fMRI, suggesting that MMFT Marines did not need to expend as much cognitive effort to downregulate negative emotions and control impulsive actions (Johnson et al., 2014).
A later study demonstrated that MMFT participants could sustain performance on the Sustained Attention to Response Task (SART) after participating in high-demand training compared to controls (Jha et al., 2015). Military service members have a strong tradition of valuing physical fitness to maintain a ready fighting force. The experience of MMFT suggests that emphasizing meditation as a form of “mental fitness” may be a particularly powerful strategy for engaging this population in mindfulness practice.
Mindfulness, Sports Psychology, CBT Multimodal Application with Fighter Pilots and EOD Technicians
Integrating mindfulness and sport psychology skills into military populations who rely on skills related to processing information flow and prioritizing decision-making in milliseconds is essential for optimal performance. Such mental skills are vital tools in preparing for and strengthening physical and psychological recovery from challenges, traumatic experiences, exertion, stress, anxiety, and a number of other experiences. Furthermore, when talent, skills, athleticism, and physical fitness become uniform at the master level, mental skills will separate the elite. In developing and enhancing mental skills to prepare for high stress environments, fighter pilots and explosive ordnance disposal (EOD) technicians can become more elite in their confidence to face challenges and overcome struggles.
A variety of exercises can aid in enhancing mental skills. According to Janelle and Hatfield (2008), arousal regulation, as well as more acute focus and attention, can enhance both military and sport performance. Training such mental skills enhances and maximizes perceptual–cognitive autonomous decision-making in duty training, thus eliciting an increase in the level of performance (Ward et al., 2008). When fighter pilots and EOD technicians master their decision and reaction times with information available, they must also remain calm, poised, and extremely focused.
Multimindfulness-based approaches are being used for performance enhancement within military operations. Such training has already been established for professional athletes (Lavallee, Kremer, Moran, & Williams, 2004). It has also been established for a unique military population in a program called the Performance Improvement Program (PIP; Gassaway & Christopherson, 2014). PIP specifically targeted the needs of F-16 fighter pilots and Explosive Ordnance Disposal (EOD) technicians who tend to work in higher stress and more technologically saturated environments than most military members. PIP was created at Luke Air Force Base to develop better functioning, resilience, and mission readiness. This training is an integration of mindfulness, sports psychology, and cognitive–behavioral therapy. PIP participants met for 60–90 min sessions once or twice a week for 8–12 weeks.
Participation in PIP resulted in improvements in test scores for instructor pilots, despite baseline scores already being in the 90th percentile on the Trail Making Test––Forms A & B. The student pilots who attended PIP training improved their reaction time, ability to divide attention, and motor dexterity. Additionally, anecdotal reports from the student pilots included improvements in sleep, daily stress, and confidence (Gassaway & Christopherson, 2014).
EOD technicians who completed the program were tested using an EOD acuity test specifically designed for mission/duty-simulated tasks in addition to the Trail Making Test––Forms A & B. PIP participants made less mental errors and performed with greater efficiency than their control group peers in the EOD acuity test. Results also showed significant improvement in motor dexterity, visual scanning, divided attention, and processing speed (Gassaway & Christopherson, 2014). Processing speed is particularly important, in an occupation such as EOD and fighter pilots, where a split second can mean the difference between life and death.
Performance Improvement Program training was associated with better capabilities of: overcoming stress, diversifying skills across domains, regulating arousal level, increasing confidence and physical and psychological awareness, improving goal-setting skills, more positive self-talk, imagery for performance improvement, improving focus and attention skills, and decreasing reaction time (Gassaway & Christopherson, 2014). Using the skills (Mindfulness, Sport Psychology, Cognitive Behavioral Therapy) from PIP training, fighter pilots and EOD technicians enhanced their performance, demonstrated resiliency, and outperformed their colleagues. Programs such as PIP may benefit military personnel across a variety of well-being dimensions (See also Bowles et al., Chap 14, this volume).
Future Directions and Conclusion
Mindfulness techniques and related alternative approaches continue to grow in popularity of use in both military and civilian sectors of the population, with promising research supporting their use. Mindfulness approaches, and their utilization of the relaxation response and other such skills, would potentially benefit service members and their families. Mindfulness approaches may provide stress reduction and performance improvements by mitigating prolonged negative stress that can reduce physical and psychological effectiveness. Service members, veterans, and their families, who are adversely impacted by OEF, OIF, OND, OIR, and OFS, may not desire mental health treatments due to stigmatization or not having access to treatment. In the case of individuals who do not desire mental health treatment, evidence-based alternative treatment options such as meditation, yoga, acupuncture, etc. may offer immense benefits as resilience-building tools. These mind–body practices may also prove useful for those who are receiving treatment provided by mental health care providers. To date, research has been done in a variety of populations and shows varying degrees of improvements in perceived stress, physiological stress, sleep assessment, and mood states after participation in yoga, meditation, acupuncture, tai chi, and qigong. Both meditation and yoga research studies suggest promising results in the field of mindfulness. When provided in conjunction with traditional mental health treatment, yoga and meditation interventions offer a unique self-management approach for a military population. While less research has been conducted in tai chi and qigong, Chinese medical approaches such as acupuncture have been found to be an effective alternative approach to treat pain and PTSD in veterans.
Questions remain about translating research findings into practice, whether it is in military clinical practice aimed at mitigating symptoms of disease or condition, or if it is in programs aimed at improving performance, or building strength through hardiness, resilience resulting in greater well-being capacity. The future application of mind–body modalities perhaps bifurcates into two interdependent pathways––clinical practice and military life.
In clinical practice, translational research requires participation by clinicians who understand the nature of military populations, their problems, their resources, constraints, and limitations of the operational and Garrison clinical settings. These clinicians will be qualified to make good decisions about indications for the use of mind–body modalities, dosing, methods of delivery, and the measures of cost, patient satisfaction, and effectiveness.
Additionally, in the military life space, translational research requires the participation of the military leaders, military family members, and community leaders who understand the nature of the population and operational circumstances. This understanding would include this population’s state of fitness and the essential capabilities needed in garrison (home base/home port), field, deployment settings, and mobilized situations. Further understanding of military life space limitations, opportunities, constraints, and priorities is also significant to ensure proper allocation of resources to programs that deliver and train mind–body practices to support and improve the performance of the total force effectively.
Because military service may require prolonged exposure to high stress environments, military leadership must continue searching for strategies to mitigate this stress for mission effectiveness and long-term health of service members. We advocate for the greater use of mindfulness approaches in the US DoD, VA, intelligence community, and other parts of the government and civilian community to function as ancillary treatments for behavioral health and performance enhancement in operational settings. Acupuncture should continue to be expanded for use across medical treatment facilities with training for behavioral health providers for pain reduction and PTSD. Tai chi and qigong should continue to be encouraged as alternative cross-training for military and government fitness programs.
Further research is needed for the complementary and integrative health approaches addressed in this chapter. Most existing studies were conducted in specific populations, under unique controlled conditions, and without the use of a randomized control group, and more research has probably been performed outside the United States. Future research interventions should be designed to be practical and employ easy-to-learn mindfulness practices or examine alternative approaches that are realistic to practice or administer by a practitioner.
Policy changes need to be made to provide service members with nonclinical and/or clinical practitioners, as suggested in the following recommendations:
-
Leaders and providers can encourage service members to attend mindfulness resilience-building education as a first option to reduce stress and/or to improve performance. Training should be held in locations outside of behavioral health such as performance enhancement centers or inside their organization with the unit master resilience trainer or master mindfulness trainer (trained in mindfulness).
-
Leaders can establish locations for service members to recharge through mindfulness resilience-building techniques in their established operating areas, during regular training cycles, and in military schools. We need to establish these programs in standard settings to build fitness, resilience, and well-being to enable successful adaptability and prevention of physical and psychological conditions as well as social conditions.
-
Behavioral health care providers and nonclinical providers such as master mindfulness trainers need to be co-located at these centers to reduce stigmatization, and to determine if a behavioral health condition warrants further treatment.
-
Behavioral health care providers in primary care settings can offer effective CIH approaches to service and family members in this and other medical settings. With this innovative approach, business practices for workload can be applied to assure these CIH practices are offered in military medicine.
Mindfulness approaches need to be designed so that components of such interventions can be practiced virtually any time to mitigate stressors. While conducting mindfulness research, the intervention should use a self-management approach, which allows individuals to use the treatment to maintain a desired mental and physical fitness state when faced with future stressors. Mind–body practices can provide both the benefit of relaxation and increased ability to manage stress, with less, if any, stigmatization. These approaches can also have a positive impact on almost all members of the military who are open to these techniques by enhancing performance, resilience, and overall well-being.
References
Acupuncture: EBM Guidelines (2014, February 7). Acupuncture. Retrieved from http://www.essentialevidenceplus.com/content/ebmg_ebm/393
Air Force Fitness and Sports Programs (2014). Air Force Instruction 34–266. Retrieved from http://static.e-publishing.af.mil/production/1/af_a1/publication/afi34-266/afi34-266.pdf
Allais, G., Romoli, M., Rolando, S., Airola, G., Gabellari, I. C., Allais, R., & Benedetto, C. (2011). Ear acupuncture in the treatment of migraine attacks: A randomized trial on the efficacy of appropriate versus inappropriate acupoints. Neurological Sciences, 32, 173–175.
American Psychological Association. (2016). Stress in America: The impact of discrimination. Stress in America Survey. Retrieved from http://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf
Banks, K., Newman, E., & Saleem, J. (2015). An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: A systematic review. Journal of Clinical Psychology, 71, 935–963.
Bates, M. J., Bowles, S. V., Hammermeister, J., Stokes, C., Pinder, E., Moore, M., … Burbelo, G. (2010). Psychological fitness. Military Medicine, 175, 21–38.
Bellanti, D., Boyd, C. Khorsan, R., Smith, K., Elfenbaum, P., York, A., … Crawford, C. (2016). Biopsychosocial training programs for the self-management of emotional stress: A systematic review of randomized clinical trials. Retrieved from http://www.samueli.org/wp-content/uploads/2017/02/CRIMM-Final-Report-26SEP16.pdf
Benson, H., Beary, J. H., & Carol, M. P. (1974). The relaxation response. Psychiatry, 37, 37–46.
Benson, H., Dryer, T., & Hartley, L. H. (1978). Decreased VO2 consumption during exercise with elicitation of the relaxation response. Journal of Human Stress, 4, 38–42.
Benson, H., Greenwood, M. M., & Klemchuk, H. (1975). The relaxation response: Psychophysiologic aspects and clinical applications. International Journal of Psychiatry in Medicine, 6, 87–98.
Benson, H., & Proctor, W. (2010). Relaxation revolution: The science and genetics of mind body healing. New York: Simon and Schuster.
Berman, B. M., Lao, L., Langenberg, P., Lee, W. L., Gilpin, A. M., & Hochberg, M. C. (2004). Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: A randomized, controlled trial. Annals of Internal Medicine, 14, 901–910.
Bernstein, A. M., Kobs, A., Bar, J., Fay, S., Doyle, J., Golubic, M., & Roizen, M. F. (2015). Yoga for stress management among intensive care unit staff: A pilot study. Alternative & Complementary Therapies, 21, 111–115. https://doi.org/10.1089/act.2015.28999.amb
Bhasin, M. K., Dusek, J. A., Chang, B. H., Joseph, M. G., Denninger, J. W., Fricchione, G. L., … Liberermann, T. A. (2013). Relaxation response induces temoporal transciptome changes in energy metabolism, insulin secretion and inflammatory pathways. Public Library of Science One. https://doi.org/10.1371/journal.pone.0062817
Bob, P., Zimmerman, E. M., Hamilton, E. A., Sheftel, J. G., Bajo, S. D., Raboch, J., … Konopka, L. M. (2012). Conscious attention, meditation, and bilateral information transfer. Clinical EEG and Neuroscience, 44, 39–43.
Bonadies, V. (2004). A yoga therapy program for AIDS-related pain and anxiety: Implications for therapeutic recreation. Therapeutic Recreation Journal, 38, 148–166.
Bowles, S. V., Pollock, L. D., Moore, M., Wadsworth, S. M., Cato, C., Dekle, J. W., … Bates, M. J. (2015). Total force fitness: The military family fitness model. Military Medicine, 180, 246–258.
Brefcynski-Lewis, J. A., Lutz, A., Schaefer, H. S., Levinson, D. B., & Davidson, R. J. (2007). Neural correlates of attentional expertise in long-term meditation practitioners. Proceedings of the National Academy of Sciences, 104, 11483–11488.
CareerCast.com. (2014). The most stressful jobs of 2014. In Career Cast. Retrieved from http://www.careercast.com/jobs-rated/most-stressful-jobs-2014
CareerCast.com. (2015). The most stressful jobs of 2015. In Career Cast. Retrieved from http://www.careercast.com/jobs-rated/most-stressful-jobs-2015
CareerCast.com. (2016). The most stressful jobs of 2016. In CareerCast. Retrieved from http://www.careercast.com/jobs-rated/most-stressful-jobs-2016.
Carmody, J., & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31, 23–33.
Ceccherelli, F., Tortora, P., Nassimbeni, C., Casale, R., Gagliardi, G., & Giron, G. (2006). The therapeutic efficacy of somatic acupuncture is not increased by auriculotherapy: A randomized, blind control study in cervical myofascial pain. Complementary Therapies in Medicine, 14, 47–52.
Chairman of the Joint Chiefs of Staff Instruction (2011). Chairman’s total force fitness framework. CJCSI 3405.01. 1 September 2011. Retrieved from http://www.dtic.mil/cjcs_directives/cdata/unlimit/3405_01.pdf
Charney, D. S. (2004). Psychobiological mechanisms of resilience and vulnerability. American Journal of Psychiatry, 161, 195–216. Retrieved from: https://ils.unc.edu/bmh/neoref/this.dir.unneeded/schizophrenia/review/tmp/426.pdf
Chen, K. M., Fan, J. T., Wang, H. H., Wu, S. J., Li, C. H., & Lin, H. S. (2010). Silver yoga exercises improved physical fitness of transitional frail elders. Nursing Research, 59, 364–370.
Chou, R., & Huffman, L. H. (2007). Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Annals of Internal Medicine, 147, 492–504.
Chung, S., Brooks, M. M., Rai, M., Balk, J. L., & Raie, S. (2012). Effect of Sahaja yoga meditation on quality of life, anxiety and blood pressure control. The Journal of Alternative and Complementary Medicine, 18, 589–596. https://doi.org/10.1089/acm.2011.0038
Clarke, T. C., Black, L. I., Stussman, B. J., Barnes, P. M., & Nahin, R. L. (2015). Trends in the use of complementary health approaches among adults: United States, 2002–2012. National Health Statistics Reports, 79, 1–16.
Coeytaux, R. R., McDuffie, J., Goode, A., Cassel, S., Porter, W. D., Sharma, P., & Williams, J. W. W., Jr. (2014). Evidence map of yoga for high-impact conditions affecting veterans. VA-Evidence-Based Synthesis Program Project, #09-010. Washington (DC): Department of Veterans Affairs.
Crawford, C., Wallerstedt, D. B., Khorsan, R., Clausen, S. S., Jonas, W. B., & Walter, J. A. G. (2013). A systematic review of biopsychosocial training programs for the self-management of emotional stress: Potential applications for the military. Evidence Based Complementary Alternative Medicine, 2013, 1–23.
Dale, L. P., Mattison, A. M., Greening, K., Galen, G., Neace, W. P., & Matacin, M. L. (2009). Yoga workshop impacts psychological functioning and mood of women with self-reported history of eating disorders. Eating Disorders, 17, 422–434. https://doi.org/10.1080/10640260903210222
De Kloet, E. R., Joëls, M., & Holsboer, F. (2005). Stress and the brain: From adaptation to disease. Nature Reviews Neuroscience, 6, 463–475.
Defense Casualty Analysis System. (2017). Conflict casualties. Retrieved March 3, 2017 from: https://www.dmdc.osd.mil/dcas/pages/report_sum_reason.xhtml
Dusek, J. A., Out, H. H., Wohlhueter, A. L., Bhasin, M., Zerbini, L. F., Joseph, M. G., … Libermann, T. A. (2008). Genomic counter-stress changes induced by the relaxation response. Public Library of Science One, 3(7), e2576.
Engel, C. C., Cordova, E. H., Benedek, D. M., Liu, X., Gore, K. L., Goertz, C., … Ursano, R. J. (2014). Randomized effectiveness trial of a brief course of acupuncture for posttraumatic stress disorder. Medical Care, 52, S57–S64.
Furlan, A. D., Van Tulder, M. W., Cherkin, D. C., Tsukayama, H., Lao, L., Koes, B. W., & Berman, B. M. (2005). Acupuncture and dry-needling for low back pain. Cochrane Database Systematic Reviews, 1. https://doi.org/10.1002/14651858.CD001351.pub2
Gassaway, J. B., & Christopherson, C. (2014). Performance Improvement Program (PIP) training. Psynopsis: Canadian Psychological Association Magazine, 36, 49–51.
Gironda, R. J., Clark, M. E., Massengale, J. P., & Walker, R. L. (2006). Pain among veterans of operations enduring freedom and Iraqi freedom. Pain Medicine, 7(4), 339–343.
Goyal, M., Singh, S., Sibinga, E. M. S., Gould, N. F., Rowland-Seymour, A., Sharma, R., … Haythornthwaite, J. A. (2014). Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. Journal of the American Medical Association Internal Medicine, 174, 357–368. https://doi.org/10.1001/jamainternmed.2013.13018
Gross, J. J. (2002). Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology, 39, 281–291.
Heffner, K. L., Crean, H. F., & Kemp, J. E. (2016). Meditation programs for veterans with posttraumatic stress disorder: Aggregate findings from a multi-site evaluation. Psychological Trauma: Theory, Research, Practice, And Policy, 8, 365–374.
Hempel, S., Taylor, S. L., Marshall, N. J., Miake-Lye, I. M., Beroes, J. M., Shanman, R., Solloway, M. R., & Skelle, P. G. (2014). Evidence map of mindfulness. VA-Evidence-Based Synthesis Program Project, #05–226. Washington, DC: Department of Veterans Affairs.
Hempel, S, Taylor SL, Solloway MR, Miake-Lye IM, Beroes JM, Shanman R, Booth MJ, Siroka AM, & Shekelle PG (2014a). Evidence map of acupuncture. Evidence-Based Synthesis Program Reports. Washington, DC: Department of Veterans Affairs.
Hempel, S., Taylor, S. L., Solloway, M. R., Miake-Lye, I. M., Beroes, J. M., Shanman, R., & Shekelle, P. G. (2014b). Evidence map of Tai chi. VA-Evidence-Based Synthesis Program Project, #05-226. Washington, DC: Department of Veterans Affairs.
Hinman, R. S., McCrory, P., Pirotta, M., Relf, I., Forbes, A., Crossley, K. M., … Bennell, K. L. (2014). Acupuncture for chronic knee pain: A randomized clinical trial. Journal of the American Medical Association, 312, 1313–1322.
Hoge, C. W., Auchterlonie, J. L., & Milliken, C. S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq and Afghanistan. Journal of the American Medical Association, 259, 1023–1032. https://doi.org/10.1001/jama.295.9.1023
Hoge, C. W., Castro, C. A., Messer, S. C., McGurk, D., Cotting, D. I., & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351, 13–22.
Hollifield, M., Sinclair-Lian, N., Warner, T. D., & Hammerschlag, R. (2007). Acupuncture for posttraumatic stress disorder: A randomized controlled pilot trial. The Journal of Nervous and Mental Disease, 195, 504–513.
Hölzel, B. K., Lazar, S. W., Gar, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6, 537–559.
Integrative Health and Wellness Program, Washington D.C. VA Medical Center (2016). Weekly group schedule as of July 21, 2016. Retrieved from http://www.washingtondc.va.gov/Wellness/IHW_Schedule_for_web.pdf
Jacobson, I. G., White, M. R., Smith, T. C., Smith, B., Wells, T. S., Gackstetter, G. D., & Boyko, E. J. (2009). Self-reported health symptoms and conditions among complementary and alternative medicine users in a large military cohort. Annals of Epidemiology, 19, 613–622.
Janelle, C. M., & Hatfield, B. D. (2008). Visual attention and brain processes that underlie expert performance: Implications for sport and military psychology. Military Psychology, 20, S39–S69.
Jazaieri, H., McGonigal, K., Jinpa, T., Doty, J., Gross, J., & Goldin, P. (2014). A randomized controlled trial of compassion cultivation training: Effects on mindfulness, affect, and emotion regulation. Motivation and Emotion, 38, 23–35.
Jha, A. P., Krompinger, J., & Baime, M. J. (2007). Mindfulness training modifies subsystems of attention. Cognitive, Affective and Behavioral Neuroscience, 7, 109–119.
Jha, A. P., Morrison, A. B., Dainer-Best, J., Parker, S., Rostrub, N., & Stanley, E. A. (2015). Minds “at attention”: Mindfulness training curbs attentional lapses in military cohorts. PloS One. https://doi.org/10.1371/journal.pone.0116889
John, P. J., Sharma, N., Sharma, C. M., & Kankane, A. (2007). Effectiveness of yoga therapy in the treatment of migraine without aura: A randomized controlled trial. Headache: The Journal of Head and Face Pain, 47, 654–661. https://doi.org/10.1111/j.1526-4610.2007.00789.x
Johnson, D. C., Thorn, N. H., Stanley, E. A., Simmons, A. N., Shih, P. B., Thompson, W. K., … Paulus, M. P. (2014). Modifying resilience mechanisms in at-risk individuals: A controlled study of mindfulness training in Marines preparing for deployment. American Journal of Psychiatry, 171, 844–853.
Johnston, J. M., Minami, T., Greenwald, D., Li, C., Reinhardt, K., & Khalsa, S. S. (2015). Yoga for military service personnel with PTSD: A single arm study. Psychological Trauma: Theory, Research, Practice, and Policy, 7, 555–562.
Karlamangla, A. S., Singer, B. H., McEwen, B. S., Rowe, J. W., & Seeman, T. E. (2002). Allostatic load as a predictor of functional decline: MacArthur studies of successful aging. Journal of Clinical Epidemiology, 55, 696–710.
Khalsa, S. B. S. (2004a). Treatment of chronic insomnia with yoga: A preliminary study with sleep-wake diaries. Applied Psychophysiology and Biofeedback, 29, 269–278. https://doi.org/10.1007/s10484-004-0387-0
Khalsa, S. B. S. (2004b). Yoga as a therapeutic intervention: A bibliometric analysis of published research studies. Indian Journal of Physiological Pharmacology, 48, 269–285.
Khusid, M. A. (2015). Clinical indications for acupuncture in chronic post-traumatic headache management. Military Medicine, 180, 132–136.
Khusid, M. A., & Vythilingam, M. (2016a). The emerging role of mindfulness meditation as effective self-management strategy, Part 1: Clinical implications for depression, post-traumatic stress disorder, and anxiety. Military Medicine, 181, 961–968.
Khusid, M. A., & Vythilingam, M. (2016b). The emerging role of mindfulness meditation as effective self-management strategy, Part 2: Clinical implications for chronic pain, substance misuse, and insomnia. Military Medicine, 181, 969–975.
Kim, Y. D., Heo, I., Shin, B. C., Crawford, C., Kang, H. W., & Lim, J. H. (2013). Acupuncture for posttraumatic stress disorder: A systematic review of randomized controlled trials and prospective clinical trials. Evidence-based Complementary and Alternative Medicine, 2013, 1–11.
Lang, A. J., Strauss, J. L., Bomyea, J., Bormann, J. E., Hickman, S. D., Good, R. C., & Essex, M. (2012). The theoretical and empirical basis for meditation as an intervention for PTSD. Behavior Modification, 36, 759–786. https://doi.org/10.1177/0145445512441200
Lavallee, D., Kremer, J., Moran, A. P., & Williams, M. (2004). Sport psychology: Contemporary themes. New York: Palgrave MacMillan.
Lazarus, R. S., & Folkman, S. (1986). Cognitive theories of stress and the issue of circularity. In M. H. Appley & R. Trumbull (Eds.), Dynamics of stress. Physiological, psychological, and social perspectives (pp. 63–80). New York: Plenum.
Lee, C., Crawford, C., & Schoomaker, E. (2014). Movement therapies for self-management of chronic pain symptoms. Pain Medicine, 15, S40–S53.
McEwen, B. S. (1999). Stress and hippocampal plasticity. Annual Review of Neuroscience, 22, 105–122.
McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87, 873–904.
McRae, K., Ciesielski, B., & Gross, J. J. (2012). Unpacking cognitive reappraisal: Goals, tactics, and outcomes. Emotion, 12, 250–255.
Mental Health Advisory Team 9. (2013). Mental health advisory team 9 [MHAT-9]: Operation Enduring Freedom (OEF) 2013 – Afghanistan. Retrieved from http://armymedicine.mil/Pages/Reports.aspx
Millegan, J., Morrison, T., Bhakta, J., & Ram, V. (2014). Mind body medicine in the care of a U.S. Marine with chronic pain: A case report. Military Medicine, 179. http://militarymedicine.amsus.org/doi/full/10.7205/MILMED-D-14-00130
Millegan, J., Ram V., Bhakta J. P., Brown A., Weits G., Hess L. (2016). Integrating mind body medicine into the military healthcare delivery system. Poster session presented at the meeting of the American Psychological Association, Denver, CO.
Morgan, C. A., Southwick, S., Hazlett, G., Rasmusson, A., Hoyt, G., Zimolo, Z., & Charney, D. (2004). Relationships among plasma dehydroepiandrosterone sulfate and cortisol levels, symptoms of dissociation, and objective performance in humans exposed to acute stress. Archives of General Psychiatry, 61, 819–825.
Mullen, M. (2010). On total force fitness in war and peace. Military Medicine, 175, 1–2.
Nassif, T. H., Chapman, J. C., Sandbrink, F., Norris, D. O., Soltes, K. L., Reinhard, M. J., & Blackman, M. (2015). Mindfulness meditation and chronic pain management in Iraq and Afghanistan veterans with traumatic brain injury: A pilot study. Military Behavioral Health, 4, 82–89.
National Center for Complementary and Integrative Health. (2016) Tai Chi and Qi Gong: In Depth (NCCIH Publication No. D322). Retrieved from https://nccih.nih.gov/health/taichi/introduction.htm#hed1https://nccih.nih.gov/health/taichi/introduction.htm-hed1
Naval Medical Center San Diego. (2016). Mind body medicine. Retrieved from http://www.med.navy.mil/sites/nmcsd/Pages/Care/Mind-Body-Medicine.aspx
Navy and Marine Corps Public Promotion and Wellness Department (NMCPHC). (n.d.) RelaxRelax. Retrieved from http://www.med.navy.mil/sites/nmcphc/health-promotion/psychological-emotional-wellbeing/relax-relax/pages/index.html
Niemtzow, R. C. (2007). Battlefield acupuncture. Medical Acupuncture, 19. https://doi.org/10.1089/acu.2007.0603
NIH Consensus Development Panel on Acupuncture. (1998). Acupuncture. Journal of the American Medical Association., 280, 1518–1524.
Nosaka, M., & Okamura, H. (2015). A single session of an integrated yoga program as a stress management tool for school employees: Comparison of daily practice and nondaily practice of a yoga therapy program. The Journal of Alternative and Complementary Medicine, 21, 444–449.
Office of The Army Surgeon General (2010). Pain management task force final report (Report no. 650–0145-00 A). Retrieved from http://www.regenesisbio.com/pdfs/journal/pain_management_task_force_report.pdf.
Ortner, C. N. M., Kilner, S. J., & Zelazo, P. D. (2007). Mindfulness meditation and reduced emotional interference on a cognitive task. Motivation and Emotion, 31, 271.
Park, C. (2013). Mind-body CAM interventions: Current status and considerations for integration into clinical health psychology. Journal of Clinical Psychology, 69, 45–63. https://doi.org/10.1002/jclp.21910
Park, E., Traeger, L., Vranceanu, A. M., Scult, M., Lerner, J. A., Benson, H., … Fricchione, G. L. (2013). The development of a patient-centered program based on the relaxation response: The relaxation response resiliency program (3RP). Psychosomatics, 54, 165–174.
Qaseem, A., Wilt, T. J., McLean, R. M., & Forciea, M. A. (2017). Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the american college of physicians noninvasive treatments for acute, subacute, and chronic low back pain. Annals of Internal Medicine, 166, 214–241.
Rao, M. R., Nagarathna, R., Nagendra, H. R., Gopinath, K. S., Srinath, B. S., Ravi, B. D., … Nalini, R. (2007). Effects of an integrated yoga programme on chemotherapy-induced nausea and emesis in breast cancer patients. European Journal of Cancer Care, 16, 462–474.
Rao, M. R., Raghuram, N., Nagendra, H. R., Gopinath, K. S., Srinath, B. S., Diwakar, R. B., … Varambally, S. (2009). Anxiolytic effects of a yoga program in early breast cancer patients undergoing conventional treatment: A randomized controlled trial. Complementary Therapies in Medicine, 17, 1–8.
Rao, R. M., Raghuram, N., Nagendra, H. R., Usharani, M. R., Gopinath, K. S., Diwakar, R. B., … Rao, N. (2015). Effects of an integrated yoga program on self-reported depression scores in breast cancer patients undergoing conventional treatment: A randomized controlled trial. Indian Journal of Palliative Care, 21, 174.
Samuelson, M., Foret, M., Baim, M., Lerner, J., Fricchione, G., Benson, H., … Yeung, A. (2010). Exploring the effective of a comprehensive mind-body intervention for medical symptom relief. The Journal of Alternative and Complementary Medicine, 16, 187–192.
Sandvik, A. M., Bartone, P. T., Hystad, W. W., Phillips, T. M., Thayer, J. F., & Johnsen, B. H. (2013).Psychological hardiness predicts neuroimmunological responses to stress. Psychology, Health & Medicine, 18, 705–713.
Schell, T. L., & Marshall, G. N. (2008). Survey of individuals previously deployed for OEF/OIF. In T. Tanielian & L. H. Jaycox (Eds.), Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery (pp. 87–115). Santa Monica, CA: RAND Center for Military Health Policy Research.
Schmeltzer, S. N., Herman, J. P., & Sah, R. (2016). Neuropeptide Y (NPY) and posttraumatic stress disorder (PTSD): A translational update. Experimental Neurology, 284, 196–210.
Sharma, M. (2014). Yoga as an alternative and complementary approach for stress management: A systematic review. Journal of Evidence-Based Complementary & Alternative Medicine, 19, 59–67. https://doi.org/10.1177/2156587213503344
Sharp, M., Fear, N. T., Rona, R. J., Wessely, S., Greenberg, N., Jones, N., & Goodwin, L. (2015). Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiologic Reviews, 37, 144–162.
Silverthorne, C., Khalsa, S. B., Gueth, R., DeAvilla, N., & Pansini, J. (2012). Respiratory, physical, and psychological benefits of breath-focused yoga for adults with severe traumatic brain injury (TBI): A brief pilot study report. International Journal of Yoga Therapy, 22, 47–52.
Stankovic, L. (2011). Transforming trauma: A qualitative feasibility study of integrative restoration (iRest) yoga Nidra on combat-related post-traumatic stress disorder. International Journal of Yoga Therapy, 21, 23–37.
Staples, J. K., Hamilton, M. F., & Uddo, M. (2013). A yoga program for the symptoms of post-traumatic stress disorder in veterans. Military Medicine, 178, 854–860. https://doi.org/10.7205/MILMED-D-12-00536
Stoller, C. C., Greuel, J. H., Cimini, L. S., Fowler, M. S., & Koomar, J. A. (2012). Effects of sensory-enhanced yoga on symptoms of combat stress in deployed military personnel. American Journal of Occupational Therapy, 66, 59–68. https://doi.org/10.5014/ajot.2012.001230
Substance Abuse and Mental Health Services Administration. (2014). Veterans and military families. Retrieved from http://www.samhsa.gov/veterans-military-families
Tafet, G. E., & Bernardini, R. (2003). Psychoneuroendocrinological links between chronic stress and depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 27, 893–903.
Toblin, R. L., Quartana, P. J., Riviere, L. A., Walper, K. C., & Hoge, C. W. (2014). Chronic pain and opioid use in US soldiers after combat deployment. Journal of the American Medical Association, 174, 1400–1401.
Tran, M. D., Holly, R. G., Lashbrook, J., & Amsterdam, E. A. (2001). Effects of hatha yoga practice on the health-related aspects of physical fitness. Preventative Cardiology, 4, 165–170.
Trinh, K., Graham, N., Irnich, D., Cameron, I. D., & Forget, M. (2016). Acupuncture for neck disorders (review). Cochrane Database of Systematic Reviews, 5, Art. No: CD004870. https://doi.org/10.1002/14651858.CD004870.pub4
U.S. Department of Veterans Affairs. (2014). VA initiative shows early promise in reducing use of opioids for chronic pain. Retrieved from https://www.va.gov/opa/pressrel/pressrelease.cfm?id=2529
U.S. Department of Veterans Affairs. (2016). How common is PTSD? In PTSD: National center for PTSD. Retrieved from: http://www.ptsd.va.gov/public/PTSD-overview/basics/how-common-is-ptsd.asp
Vadiraja, H. S., Raghavendra, R. M., Nagarathna, R., Nagendra, H. R., Rekha, M., Vanitha, N., … Kumar, V. (2009). Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: A randomized controlled trial. Integrative Cancer Therapies, 8, 37–46.
Van Leeuwen, S., Singer, W., & Melloni, L. (2012). Meditation increases the depth of information processing and improves the allocation of attention in space. Frontiers in Human Neuroscience, 6, 1–16.
Vedamurthachar, A., Janakiramaiah, N., Hegde, J. M., Shetty, T. K., Subbakrishna, D. K., Sureshbabu, S. V., & Gangadhar, B. N. (2006). Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. Journal of Affective Disorders, 94, 249–253. https://doi.org/10.1016/j.jad.2006.04.025
Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., MacPherson, H., Foster, N. E., … & Acupuncture Trialists’ Collaboration. (2012). Acupuncture for chronic pain: Individual patient data meta-analysis. Archives of Internal Medicine, 172, 1444–1453.
Vickers, A. J., Cronin, A. M., Maschino, A. C., Lewith, G., Macpherson, H., Victor, N., … Linde, K. (2010). Individual patient data meta-analysis of acupuncture for chronic pain: Protocol of the Acupuncture Trialists’ Collaboration. Trials, 11, 90.
Vickers, A. J., Rees, R. W., Zollman, C. E., McCarney, R., Smith, C. M., Ellis, N., … Van Haselen, R. (2004). Acupuncture for chronic headache in primary care: Large, pragmatic, randomized trial. British Medical Journal, 328, 744. https://doi.org/10.1136/bmj.38029.421863.EB
Wallace, R. K., Benson, H., & Wilson, A. F. (1971). A wakeful hypometabolic physiologic state. American Journal of Physiology, 221, 795–799.
Ward, P., Farrow, D., Harris, K. R., Williams, A. M., Eccles, D. W., & Ericsson, K. A. (2008). Training perceptual-cognitive skills: Can sport psychology research inform military decision training? Military Psychology, 20(suppl.1), S71–S102. https://doi.org/10.1080/08995600701804814
Yehuda, R., Brand, S., & Yang, R. (2006). Plasma neuropeptide Y concentrations in combat exposed veterans: Relationship to trauma exposure, recovery from PTSD, and coping. Biological Psychiatry, 59, 660–663.
Yehuda, R., Pratchett, L. C., Elmes, M. W., Lehrner, A., Daskalakis, N. P., Koch, E., … Bierer, L. M. (2014). Glucocorticoid-related predictors and correlates of post-traumatic stress disorder treatment response in combat veterans. Interface Focus, 4, 20140048.
Zeidan, F., Johnson, S. K., Diamond, B. J., David, Z., & Goolkasian, P. (2010). Mindfulness meditation improves cognition: Evidence of brief mental training. Consciousness and Cognition, 19, 597–605.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Bowles, S.V. et al. (2017). The Use of Mindfulness and Acupuncture in the American Military. In: Bowles, S., Bartone, P. (eds) Handbook of Military Psychology. Springer, Cham. https://doi.org/10.1007/978-3-319-66192-6_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-66192-6_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-66190-2
Online ISBN: 978-3-319-66192-6
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)