Abstract
PET/MR imaging has the ability to detect the increase in adipocytes in the bone marrow which occurs as a consequence of irradiation. The effects of irradiation of bone marrow on FDG uptake are important in determining the evaluation of bone metastases following radiation therapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
History
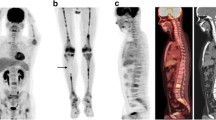
A 54-year-old female presents for restaging of cervical cancer 6 months following radiation treatment to the pelvis and chemotherapy (Fig. 18.1).
Diagnosis
Radiation effect on bone marrow
Findings
-
Decreased T1 signal in L5 vertebra and the sacrum (white arrowheads) with corresponding increased T2 signal (white thin arrows) indicating increase of adipocytes in the bone marrow.
-
No changes are detected on STIR images.
-
PET fusion shows decreased FDG uptake in L5 vertebra and the sacrum (white curved arrow) as a result of radiation therapy.
-
PET sagittal image also shows decreased FDG uptake in L5 vertebra and the sacrum (black wide arrow) with generalized increased FDG uptake in the remainder of the vertebrae as a result of chemotherapy-induced bone marrow stimulation.
Discussion
Knowledge of the evolution of bone marrow changes following radiation therapy is important in differentiating between normal postradiation changes from other marrow abnormalities. In addition, bone marrow changes may help to determine if the patient is able to undergo further antineoplastic therapy such as chemotherapy. MRI has the ability to detect the increase in adipocytes in the bone marrow which occurs as a consequence of radiation therapy. Increase in adipocytes is indicative of loss of myeloid tissue . Radiation-induced changes of bone marrow as detected by MRI are determined by both the radiation dose length of administration and the time interval following radiation treatment.
Initially, changes in the bone marrow are detected by increased signal on STIR imaging reflecting edema and necrosis. Between 3 and 6 weeks as fatty cells start to migrate, there is heterogeneous marrow signal with increased signal on T1-weighted images and the normalization of STIR hyperintensity. After 6 weeks marrow cellularity is further replaced by fatty tissue and mild increased signal on T2-weighted images. Fat sensitive T1-weighted images show increased bone marrow signal but may appear hypointense in signal. MRI changes in the marrow are most prominent 5–6 years following therapy, while complete recovery may take up to 10–23 years after treatment with high radiation doses.
Knowing the effects of irradiated bone marrow on FDG PET/MR imaging is important in evaluating bone metastases following radiation therapy . Acute or subacute changes in FDG uptake on PET/MR following radiation can occur and make therapy response determination more difficult. Irradiated bone marrow initially has a transient rise in FDG uptake during the first 1–3 weeks reflecting inflammation. Afterward, there is a quick decline in uptake to severely decreased FDG uptake in the bone marrow reflecting replacement by adipocyte tissue. Often this decreased uptake appears more pronounced with the administration of chemotherapy agents and granulocyte-stimulating factors that dramatically increase FDG uptake in normal marrow. Return to normal FDG uptake in the irradiated bone marrow may take years. Thus, the evaluation of bone marrow in assessing treatment response using FDG PET/MR should be interpreted with caution within the first few weeks following radiation therapy. Ultimately, serial imaging may be needed to determine the significance of abnormal PET and MR findings.
Suggested Reading
Casamassima F, Caramella CR, Tinacci E, Villari N, Ruggiero M. Hematopoietic bone marrow recovery after radiation therapy: MRI evaluation. Blood. 1989;73:1677–81.
Higashi T, Fisher SJ, Brown RS, Nakada K, Walter GL, Wahl RL. Evaluation of the effect of local irradiation on normal rodent bone marrow metabolism using FDG: preclinical PET studies. J Nucl Med. 2000;41(12):2026–35.
Stevens SK, Moore SG, Kaplan D. Early and late bone-marrow changes after irradiation: MR evaluation. AJR Am J Roentgenol. 1990;154(4):754–0.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Pouldar, D., Matthews, R. (2018). Radiation Effect on Bone Marrow. In: PET/MR Imaging . Springer, Cham. https://doi.org/10.1007/978-3-319-65106-4_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-65106-4_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-65105-7
Online ISBN: 978-3-319-65106-4
eBook Packages: MedicineMedicine (R0)