Abstract
As outlined in previous chapters, men with a history of prostate cancer face increased rates of morbidity associated with both their cancer and the side effects of its treatment. Prostate cancer and its treatment can result in altered body composition, increased fatigue, reduced physical activity, fitness and performance, which in turn create considerable and complex health risks. Moreover, obesity has been linked to cancer-related mortality and aggressive prostate cancer and poor prognosis, specifically. The benefits of energy balance among prostate cancer survivors include reduced fatigue, improved quality of life scores, and greater muscular strength.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Physical Activity
- Weight Loss
- Planned Behavior Therapy
- Transtheoretical Model
- Social Cognitive Theory
- Energy Balance Messaging
Introduction
Prostate cancer and its treatment create health risks [1, 2], which are considerably exacerbated by obesity [3,4,5]. The proportion of men with a history of prostate cancer who are engaged in regular exercise points to a potential value in focusing on the promotion of effective behavior change among this population [1, 6, 7]. Some studies have indicated high interest in health promotion programs [6], suggesting that messages regarding the potential benefits of physical activity are being heard and acted upon at least by some men with a history of prostate cancer [8]. However, until now, most energy balance interventions in the U.S. have been designed for female breast cancer survivors or survivors in general, rather than specifically for prostate cancer survivors [9,10,11]. Interventions that are designed for women, or that do not specifically address the issues related to prostate cancer and the barriers that men often face in making changes in dietary and physical activity are unlikely to be optimally effective. Thus, it is important to identify appropriate strategies to communicate with prostate cancer survivors about ways to reduce their risk of cancer progression and improve outcomes. In this chapter, we outline many of the important factors to consider in planning for such an undertaking, and effective communication modalities to promote energy balance among men with a prostate cancer history.
Norms, attitudes and practices related to both diet and physical activity are not universal, and thus one might expect people’s trajectory through behavior change to be shaped by factors such as social position, age and gender [12,13,14]. As such, it is important to consider the facilitators and barriers to any behavior change messaging for intervention implementation. Prior research has identified a range of potential barriers to achieving sustained and effective behavior change to achieve energy balance among prostate cancer survivors. For example:
-
Older cancer survivors (age 65 and above) have been found to be less physically active than younger counterparts [15]; the average age at diagnosis for prostate cancer is approximately 66 years [16].
-
Weight-based stigma, sedentary lifestyle and lack of work-life balance have been identified as barriers to weight-loss among men who are obese [17].
-
Men have been found to be less motivated to partake in weight loss strategies focused on dietary modifications than physical activity [17, 18].
-
Prostate cancer survivors’ adherence to an exercise program was found to be lower for men with severe hormonal symptoms and low perceived ability to perform daily tasks and leisure activities [19].
-
Among men with a history of prostate cancer, work demands and the cost of healthy food have been highlighted as barriers to dietary behavior changes [20].
Effective energy-balance messaging will require engagement with such factors to present meaningful objectives for change and address potential difficulties in attaining them.
Efficacy of Evidence-Based, Theory-Driven Energy Balance Interventions Among Prostate Cancer Survivors
Reviews of the energy balance intervention literature have indicated potential for improvements in an array of physical and mental health outcomes for cancer survivors [9]. Achieving these outcomes may be facilitated by the integration of behavioral theories in the development of interventions, allowing for a stronger assessment of factors influencing behavior change [21]. However, there is inconsistent evidence of the extent to which behavioral theories have informed and/or driven interventions to improve diet and exercise among cancer survivors [22]. This section explores the utilization of behavioral theories to develop and test energy balance interventions among cancer survivors.
Among the most popular theories in diet and physical activity interventions for cancer survivors are the Theory of Planned Behavior , Transtheoretical Model , and Social Cognitive Theory [22,23,24,25]. According to the Theory of Planned Behavior, behavioral intention is the most important direct influence on behavior change [26]; messages are therefore to be designed to create and maintain a positive intention towards the desired change. Intention to perform a behavior depends on several factors, including one’s attitude toward changing a behavior, beliefs about others’ perceived approval or disapproval of a behavior, and perceived control over the ability to enact behavior change. Somewhat in contrast, the Transtheoretical Model emphasizes the extent to which individuals balance the pros and cons of changing a behavior as they go through the six stages of change, spanning from precontemplation to termination of a behavior [27]. Lastly, Social Cognitive Theory posits that the interplay between individuals and their environments—known as reciprocal determinism—impacts personal and collective behaviors and emphasizes an individual’s potential to facilitate changes in his or her environment [28]. While each theory conceptualizes behavior change in a somewhat different way, all three provide strong frameworks from which to design energy balance interventions that address barriers to physical activity and dietary change among prostate cancer survivors. Energy balance messaging for men with a history of prostate cancer should have at its foundation an understanding of men’s attitudes towards any modifications of diet and/or physical activity being posed, as well as the extent to which success is seen as being within their control, the environment within which an individual change will occur, and the man’s relationship to that environment. The benefits and potential negative implications of changes being promoted should be acknowledged and addressed, and considerations given not only to individual factors but also social context for making any changes.
Physical activity interventions that have at their foundation substantive behavior change theory have been shown to enhance effectiveness among breast cancer survivors [22]. Nevertheless, only a limited number of energy balance interventions targeting cancer survivors have explicitly integrated theoretical constructs; even fewer have measured these constructs to evaluate their effectiveness, and fewer still have been designed and implemented with prostate cancer survivors. Husebø and colleagues [25] conducted a systematic review and meta-analysis examining theoretical predictors of adherence to exercise programs targeting cancer survivors. Of the 12 studies reviewed, 9 utilized the Theory of Planned Behavior and 5 applied the Transtheoretical Model’s stages of change for exercise (2 studies used both theories). Results from their meta-analysis indicated that exercise stage of change is a strong predictor of exercise adherence among cancer survivors, while perceived behavioral control and intention to engage in exercise were significantly correlated with exercise adherence. Interestingly, only one study focused exclusively on prostate cancer survivors; this study found intention and exercise stage of change to be statistically significant predictors of exercise adherence [29]. A more recent systematic review and meta-analysis assessing 12 diet and exercise interventions for cancer survivors utilizing Social Cognitive Theory as their theoretical framework established that, while findings support the theory’s efficacy in changing behavior among cancer survivors, most trials failed to properly measure utilized constructs [23]. The review also identified self-efficacy—an individual’s belief that he/she can achieve an outcome of interest [30]—as the only construct associated with positive behavior change in both diet and physical activity among reviewed studies that reported assessing the impact of theoretical constructs in their interventions. It is important to note that only 3 of the 12 randomized controlled trials in their analysis included prostate cancer survivors. Of these, only one diet-specific intervention was delivered exclusively to prostate cancer survivors [31].
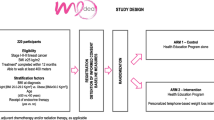
As evidenced by the literature, there is a need for additional theoretically informed evidence as to how to promote energy balance among prostate cancer survivors. In light of this growing interest, a recent cluster randomized controlled trial conducted in Australia—known as the ENGAGE study —utilized Social Cognitive Theory to design a 12-week clinician referral-based exercise intervention targeting recently diagnosed prostate cancer survivors [32]. While primary and secondary outcomes focus on physical activity participation, physical functioning, quality of life, anxiety and depression, researchers are also interested in exploring the mediating effects of self-efficacy, outcome expectations, goals and socio-cultural factors on these outcomes. Results from the analysis of adherence predictors suggest the incorporation of behavioral change techniques informed by Social Cognitive Theory may explain high adherence levels (80.3%) among participants in the exercise training intervention arm of the study [19]. Designing intervention messaging around key aspects of the theory allows for a rigorous examination (and potential modification) of the effects of key components that is otherwise not possible.
Energy Balance Messaging for Prostate Cancer Survivors
Effectively communicating the importance of energy balance to prostate cancer survivors is an essential part of achieving positive outcomes and improved health. As such, messages should be tailored to meet men’s interests and attitudes, and directed towards goals that are seen as most important and understood to be achievable. Although improved cancer prognosis as a result of weight loss may be critical to some prostate cancer survivors, discussing the benefits of energy balance from other vantage points may yield better outcomes among others. The following section discusses several messaging approaches.
A common theme in several studies focusing on dietary and exercise patterns among prostate cancer survivors is the importance of the concept of masculinity in understanding the behavioral patterns in question, as well as existing facilitators and barriers to change. Literature suggests dominant ideals of masculinity impact food choices and many times conflict with healthier eating habits, which in turn may contribute to poorer prostate cancer prognosis [33]. Among foods considered to be emblems of masculinity are red meat and dairy, both of which have been associated with an increased risk of prostate cancer [34]. Findings in a study exploring the influence of healthfulness on prostate cancer survivors’ diets highlight the importance of understanding masculine dietary patterns, as these may impact receptiveness to dietary interventions [20]. Participants described a preference towards consuming red meat, and the idea of eating for pleasure rather than for health promotion, both of which may prove problematic for dietary interventions aimed at prostate cancer survivors. The relevance of certain food types to constructs of masculinity were echoed in a recent study assessing men’s needs and interests, with 64% of men reporting daily dairy consumption and 26% reporting daily red meat consumption [35]. As such, messages should emphasize the importance of not only encouraging eating in moderation as a vehicle for weight loss, but also promoting healthy foods that taste good (identified as an important factor in men’s dietary decisions) as alternatives to red meat and dairy [20].
Concepts of masculinity also impact how men view and engage in physical activity. Multiple studies suggest men view exercise as a more masculine approach to weight loss than dieting, as it allows for men to not only lose weight but also be more muscular, fitter and stronger [17, 18]. Lewis et al. [17] also note obese men’s notion that weight loss is about “balancing energy in versus energy out,” which should be achievable by increasing physical activity without necessarily changing one’s diet. These qualitative findings were echoed in a recent study reporting that 64% of surveyed men have resorted to physical activity for weight loss [35], while only 21% of women in another study using a similar survey format reported using physical activity to lose weight [36]. Similar trends have been observed among prostate cancer survivors: when compared to female cancer survivors, male cancer survivors were 30% more likely to meet the American Cancer Society’s weekly recommendations of moderate-to-vigorous physical activity (>150 min) [37]. Furthermore, when specifically looking at male cancer survivors, prostate cancer survivors were 35% more likely than colorectal cancer survivors to meet the same guidelines [37]; while this may partially be due to limitations in physical activity among colorectal cancer survivors [38, 39], it is also possible that prostate cancer survivors experiencing impotency or other treatment side-effects view physical activity as one way to maintain or enhance their masculinity. Interventions should therefore consider highlighting the masculine benefits of physical activity when developing energy balance messages for prostate cancer survivors.
Framing behavior change specifically in relation to one’s cancer prognosis may not, however, always be the most impactful messaging strategy for men with a prostate cancer history. Age and life stage are also relevant considerations for messaging design. As people age, the meaning of a cancer diagnosis (and the associated impetus for behavior change to reduce likelihood of recurrence) is often different than it would have been earlier in life [40]. For some prostate cancer survivors, it may be more effective to promote the benefits of energy balance outside the purview of cancer, and instead focus on health in general or other chronic conditions. Co-morbidities are very prevalent among prostate cancer survivors in the U.S. [41]: data from the 2009 Behavioral Risk Factor Surveillance System survey indicate that 72% of men with a history of prostate cancer are overweight or obese, 20.1% had heart disease, 58.3% had hypertension, 53.9% had high cholesterol, and 23.7% had diabetes [37]. Studies have found that cancer often does not play a leading role in prostate cancer survivors’ dietary habits; if there is a health consideration in how men eat, it is often related to another chronic condition such as heart disease [20, 42]. Research also notes that prostate cancer survivors are more likely to die of a co-morbid disease than of prostate cancer [41, 43, 44], which provides further support for the importance of a health promotional focus that does not consider prostate cancer in isolation, but rather gives explicit consideration to the entire health of the individual—and specifically to chronic co-morbidities.
As outlined, given the prevalence of co-morbidities, it may also be more effective for energy balance messages to focus on how diet and exercise can improve the life span of survivors in general, rather than specifically prioritizing implications for cancer. More diffuse “healthy lifestyle” messaging may also be particularly important for men with a prostate cancer history who do not identify with the term “cancer survivor,” or those who have been cancer-free for a long time [45]. To these men, their experience with prostate cancer may no longer be salient; hence, energy balance messages that are focused on other benefits to diet and exercise may be more likely to be impactful.
Sexual function is also an important issue to prostate cancer survivors, with short and long-term effects of treatment including erectile dysfunction, testicular atrophy, loss of libido, penile shortening and an altered orgasm experience [46,47,48]. These effects have been noted to impact notions of masculinity, further impacting distress caused by sexual dysfunction [49]. While sexual dysfunction has been acknowledged as important to prostate cancer survivors in general [48], younger prostate cancer survivors have been reported to be more concerned about treatment impact on their sexuality [50]. Although interventions exploring the benefits of exercise on sexual function among prostate cancer survivors are scarce, a recent randomized controlled trial among prostate cancer patients undergoing androgen deprivation therapy reported men participating in 12 weeks of bi-weekly sessions of moderate to high intensity resistance and aerobic exercise maintained their sexual activity levels, while those in the control group experienced decreased libido [51]. Researchers suggested the effect of exercise on sexual activity was mediated by improved quality of life. As such, highlighting emerging findings of the benefits exercise may have on sexual function may be another way to deliver energy balance messages to prostate cancer survivors (particularly younger ones) that motivates them to increase physical activity levels [48].
The benefits of physical activity may also appeal to prostate cancer survivors who are more concerned about their current quality of life, rather than balancing energy intake as a distal goal. Studies report that cancer survivors engaging in physical activity have higher quality of life than those not meeting recommended levels [7, 52]. Quality of life was also statistically significantly higher among prostate cancer survivors receiving androgen deprivation therapy who were randomized to a 12-week resistance exercise training intervention compared to controls [5]. Meanwhile, findings from the ENGAGE study suggest that cancer-specific quality of life factors (such as role functioning, sexual activity, hormonal symptoms and education level) may predict adherence to physical activity programs for prostate cancer survivors [19]. Messages emphasizing the benefits of exercise on quality of life outcomes may thus posit themselves as more salient for a broad range of survivors desiring to improve their quality of life post treatment.
Effective Communication Modalities
In addition to identifying how to best tailor messages that promote energy balance among prostate cancer survivors, it is crucial to select appropriate modalities to communicate these messages. The communication modality will shape how information is received: When is a message conveyed? Where? And, in what form? The conveyance modality will also shape the potential influence of any delivered message, as engagement with messages is influenced by both message source and substance [53, 54].
In-person communication via healthcare providers continues to be a useful modality to reach and influence cancer survivors, particularly as not all populations have equal access to or engagement with messages conveyed via mass media [55]. Literature supporting the role of healthcare provider communication in behavior change among cancer survivors highlights providers’ abilities to influence changes in physical activity levels and dietary behaviors, given their direct contact with prostate cancer survivors throughout treatment and the care continuum [56]. Especially important is the immediate post-diagnostic period, often referenced as the “teachable moment”, when cancer survivors may be more motivated to change health behaviors due to the salience of their diagnosis [6, 42]. Healthcare providers and other practitioners may thus capitalize on this short timeframe to intervene with tailored energy balance messages.
It is important to note that as yet, energy balance interventions are not a routine part of survivorship care (in general, not just for prostate cancer survivors); the literature indicates that the doctor-patient interaction is often a missed interventional opportunity regarding physical activity as a part of healthy survivorship [1, 2, 57, 58]. A survey conducted at a Canadian cancer center highlights that 70% of cancer survivors reported not receiving exercise counseling throughout their cancer care continuum—although 90% stated a desire to participate in an exercise program post-diagnosis [58]. These findings may be indicative of the time constraints providers face during patient encounters. The 2007 Institute of Medicine (IOM) report on implementing survivorship care planning called for the inclusion of lifestyle recommendations within documentation that is intended to create the foundation for healthy survivorship beyond acute treatment [59]. To the extent that survivorship care plans become a routine part of care coordination for all cancer patients, so this may be an important mechanism by which to provide both information regarding the reasons why energy balance is key to healthy survivorship, as well as demonstrated effective mechanisms to achieve meaningful change.
Recent literature has suggested a central role for healthcare professionals beyond just physicians in communication about energy balance [60, 61]. For example, researchers in the Australian ENGAGE study assessed the efficacy of clinician referrals to a supervised exercise program for prostate cancer survivors [60]. The program used postgraduate clinical exercise physiology students (supervised by accredited exercise physiologists) to delivery two supervised, 50-min sessions per week at local gym and advised participants on a weekly home-based session. Among participants enrolled in the experimental arm of the study, 80% indicated the clinician’s referral to the exercise program influenced their decision to participate. Another way to assist patient-provider communication regarding energy balance is by leveraging the efforts of nurses and other care team members. Webb, Foster and Poulter [61] describe the development of a training intervention designed to improve nurses’ capability, opportunity and motivation in delivering very brief advice on physical activity to cancer survivors. This program is based on the Behaviour Change Wheel, a theoretical model describing eight steps to designing behavior change interventions [62]. The program teaches nurses to ‘Ask, Advise and Act’: ask patients about physical activity levels and whether they are aware of the health benefits; advise on the benefits of physical activity, based on the patient’s needs; and act by providing support and referring to local services or other resources. Although this study is still ongoing, nurses’ promotion of physical activity through brief advice may successfully influence cancer survivors, given their regular interaction through treatment and follow-up visits [63].
When we consider behavioral modifications for men as a path to achieving energy balance, it is also important to adopt a socio-ecological approach and consider the individual within a familial, cultural and structural context. Partners have been reported to be very influential in decision making that affects patient care [20, 50, 64]. Davison and colleagues [50] discussed decision-making among prostate cancer survivors and partners at the time of diagnosis, reporting that the majority of both groups preferred collaborative roles in making medical decisions. Communication strategies may thus be more successful if tailored to the dyad or the broader familial context, rather than men alone. There is also strong reason to focus on female spouses beyond medical decision-making in order to understand and impact men’s dietary behaviors. While familial norms have changed significantly over the past 30 years, women still tend to take primary responsibility for daily food preparation [65]. Prior research has found that wives of men with a prostate cancer history play a key role in shaping the diets of their husbands [20], with the majority of men relying on their spouses to prepare their meals [35]. It may sometimes be most efficacious to direct dietary messaging for prostate cancer survivorship towards both spouses and the men themselves, given histories and structures for food preparation within households.
Targeting partners as part of an energy balance communication modality may also be effective, particularly when combined with strategies targeting quality of life issues. For example, Song and colleagues [66] developed a web-based educational intervention targeting quality of life among prostate cancer survivors and their partner. The interactive website included seven modules for couples to review, among which was a mandatory module focusing on working as a team. In addition to reporting that the website was informative and easy to use, participants also stated that the program provided couples with new ways to work together and strengthen their relationship during a time of hardship. While this intervention was developed to assist with quality of life issues, these communication skills can be transferred to messages educating couples about the benefits of exercise in improving both quality of life and disease prognosis.
Another communication modality that may assist in delivering energy balance messages is the utilization of peer groups. Peer support groups have been used for some time as a way to improve depression and self-efficacy, including among prostate cancer survivors who had recently undergone a radical prostatectomy [67]. Weber et al.’s study [67] demonstrated that men who participated in an eight-week peer support intervention had higher self-efficacy and lower depression over time than those not partnered with a peer mentor. This provides some support for the idea that utilizing peer support groups may be a beneficial mechanism for promoting energy balance activities among prostate cancer survivors, especially given findings that suggest group-based exercise is better at improving prostate cancer survivors’ physical fitness and quality of life than home-based exercise programs [2].
It may not always be feasible to communicate with prostate cancer survivors about energy balance strategies in person. In such scenarios, telephone and/or mail may be a useful strategy to communicate with men to maintain healthy physical activity levels and dietary behaviors. Parsons and colleagues [31] used the Social Cognitive Theory and motivational interviewing techniques to develop a 6-month telephone-based dietary counseling program tailored to prostate cancer survivors aged 50 to 80. At the end of the intervention, vegetable consumption and carotenoid concentrations had increased in the intervention arm [31]. Another telephone-based intervention designed using the Social Cognitive Theory was the Reach out to Enhance Wellness (RENEW) trial , a 12-month home-based telephone counseling program with mailed materials developed to promote physical activity and diet quality among long-term breast, prostate and colorectal cancer survivors aged 65 years or older [68]. Results indicate statistically significant changes in physical activity levels and dietary behaviors between intervention and control groups, with intervention participants reporting a mean weight loss more than double that reported by controls. It is important to note that, compared to individuals not recruited for this study, participants were younger, female (breast cancer survivors), and had a more proximal cancer diagnosis [68]. Given in-person dialogue has been reported to be preferred among older audiences [69, 70], the RENEW trial’s findings may suggest that in-person communication modalities may be more effective than telephone and/or mail communication among some older men. Nonetheless, these communication modalities have the capacity of reaching a large number of prostate cancer survivors in cost-effective ways, as do newer technologies (such as social media and texting), which are further discussed below.
Moving Forward
As outlined in other chapters in this volume, the evidence base regarding energy balance and prostate cancer survivorship is complex, yet clearly pertinent for effective health promotion in this population. The following section provides recommendations for future energy balance interventions for men with a history of prostate cancer. One of the challenges regarding messaging for such interventions is that much of the evidence of the impact of weight loss on cancer survival is focused on women with breast cancer [9]. There is a need for greater specificity of efficacy of interventions (weight loss as well as physical activity) for specific survivor subgroups [9]. There is also a need for a more robust evidence base on the benefits of physical activity for prostate cancer survivors by intensity, duration and frequency, as well as studies that consider the nature of treatment undergone [2].
Our review of the literature did not reveal much in the way of cultural tailoring of energy balance messaging for subpopulations of men with a history of prostate cancer. There is also a gap in the evidence base regarding the extent to which behavior change messaging is more efficacious if it is targeted by gender and cultural factors . Cultural awareness has been shown to be key to developing and implementing impactful screening programs for underserved populations [71] and it might be assumed that such tailoring would also be beneficial for sustainable and impactful energy balance interventions during survivorship. This is particularly important among minority groups with a higher burden of obesity and other co-morbid conditions that may result from poor energy balance. For example, a recent study assessing racial and ethnic differences in health behaviors among prostate cancer survivors highlights that African American men had higher prevalence of obesity and diabetes than White and Hispanic survivors [72]. However, the study did not have sufficient power to detect differences between groups other than African Americans and Whites, further highlighting the importance of exploring factors impacting energy balance among other prostate cancer survivor subpopulations.
Understanding the cultural and historical context of care provision is also key to designing efficacious messaging and interventions. Prior research with African American men with a history of prostate cancer illustrated an initial level of mistrust with the healthcare system and a desire for providers to address them with respect and as knowledgeable participants in their care [73]. Meanwhile, a study of coping strategies of low-income, immigrant Mexican men with a prostate cancer diagnosis highlighted the importance of relying on God and doctors as sources of support for many men with this shared cultural heritage [74]. Studies such as these are illustrative of the importance of seeking to understand the specific facets that may be important for underserved groups in making meaningful behavior change. Cultural understanding can form the foundation for appropriate program design and message tailoring that will assist not only in recruiting participants in energy balance clinical trials, but also in creating and sustaining interventions that embed energy balance messaging into issues important to these communities.
Interventions focusing on the effects of exercise on masculinity and sexual functioning are also needed. As highlighted by Cormie and colleagues [48], exercise as a way to lessen the effects of prostate cancer treatment on sexual dysfunction has both strong theoretical rationale and budding empirical support [51]. This is an issue of importance to not only prostate cancer survivors, but also their partners. A recent study by Wootten et al. [64] focusing on prostate cancer highlighted the role that partners have in helping with influencing how the survivor adapts to and copes with a prostate cancer diagnosis. Partners stated the importance of supporting men who feel a loss in masculinity, particularly as they face challenges with communication constrains. Researchers suggest psychosocial interventions could focus on dyadic communication, sexuality and intimacy issues, support and communication pertaining loss of masculinity, social support and coping strategies (including discussions about thoughts and emotions). As such, future research should consider developing exercise interventions both assessing the impact of exercise on improving sexual function and notions of masculinity, while also integrating partners as a means of support.
The utilization of technology to promote energy balance is another important area for further research [9, 75]. As technology continues to advance and the digital divide shrinks, mobile apps, text messaging, social media and other mHealth platforms may help facilitate behavioral change interventions that reach multiple audiences that are difficult to access. Such interventions have already been used to promote weight loss among overweight and obese men [76], improve quality of life among couples with a prostate cancer survivor [66], and, more recently, assess the feasibility of text messaging to increase prostate cancer screening awareness among African American men [77]. These technologies present as areas of opportunity to engage hard-to-reach prostate cancer survivors, such as those living in rural areas with limited transportation, as well as men from racial/ethnic minorities or other underserved groups. However, technology-driven interventions may not be appropriate for all: results from a recent survey assessing men’s needs and interests for a technology-driven weight loss intervention reported that while the Internet (88%) and email (91%) were commonly used among men over the age of 60, text messaging (49%) and smartphone app utilization (22%) was substantially lower [35]. Future research exploring mHealth avenues must therefore assess the readiness of its intended audiences in adopting new technologies prior to delivery of energy balance messages.
References
Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93.
Keogh JW, MacLeod RD. Body composition, physical fitness, functional performance, quality of life and fatigue benefits of exercise for prostate cancer patients: a systematic review. J Pain Symptom Manage. 2012;43(1):96–110.
Ligibel JA, Alfano CM, Courneya KS, Demark-Wahnefried W, Burger RA, Chlebowski RT, et al. American Society of Clinical Oncology position statement on obesity and cancer. J Clin Oncol. 2014;32(31):3568–74.
Cao Y, Ma J. Body mass index, prostate cancer–specific mortality, and biochemical recurrence: a systematic review and meta-analysis. Cancer Prev Res. 2011;4(4):486–501.
Segal RJ, Reid RD, Courneya KS, Malone SC, Parliament MB, Scott CG, et al. Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. J Clin Oncol. 2003;21(9):1653–9.
Demark-Wahnefried W, Peterson B, McBride C, Lipkus I, Clipp E. Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer. 2000;88(3):674–84.
Blanchard CM, Courneya KS, Stein K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol. 2008;26(13):2198–204.
Kwon S, Hou N, Wang M. Comparison of physical activity levels between cancer survivors and non-cancer participants in the 2009 BRFSS. J Cancer Surviv. 2012;6(1):54–62.
Alfano CM, Molfino A, Muscaritoli M. Interventions to promote energy balance and cancer survivorship. Cancer. 2013;119(S11):2143–50.
Ballard-Barbash R, Siddiqi SM, Berrigan DA, Ross SA, Nebeling LC, Dowling EC. Trends in research on energy balance supported by the National Cancer Institute. Am J Prev Med. 2013;44(4):416–23.
Demark-Wahnefried W, Rogers LQ, Alfano CM, Thomson CA, Courneya KS, Meyerhardt JA, et al. Practical clinical interventions for diet, physical activity, and weight control in cancer survivors. CA Cancer J Clin. 2015;65(3):167–89.
Segar M, Jayaratne T, Hanlon J, Richardson CR. Fitting fitness into women’s lives: effects of a gender-tailored physical activity intervention. Womens Health Issues. 2002;12(6):338–47.
Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131(6):856.
Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133(4):673.
Gjerset GM, Fosså SD, Courneya KS, Skovlund E, Thorsen L. Exercise behavior in cancer survivors and associated factors. J Cancer Surviv. 2011;5(1):35–43.
American Cancer Society. Key statistics for prostate cancer. 2016. Retrieved from http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-key-statistics.
Lewis S, Thomas SL, Hyde J, Castle DJ, Komesaroff PA. A qualitative investigation of obese men’s experiences with their weight. Am J Health Behav. 2011;35(4):458–69.
Barker R, Cooke B. Diet, obesity and being overweight: a qualitative research study. Health Educ J. 1992;51(3):117–21.
Craike M, Gaskin CJ, Courneya KS, Fraser SF, Salmon J, Owen PJ, et al. Predictors of adherence to a 12-week exercise program among men treated for prostate cancer: ENGAGE study. Cancer Med. 2016;5(5):787–94.
Coa KI, Smith KC, Klassen AC, Thorpe RJ, Caulfield LE. Exploring important influences on the healthfulness of prostate cancer survivors’ diets. Qual Health Res. 2015;25(6):857–70.
Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass; 2008.
Bluethmann SM, Bartholomew LK, Murphy CC, Vernon SW. Use of theory in behavior change interventions: an analysis of programs to increase physical activity in posttreatment breast cancer survivors. Health Educ Behav. 2016;44(2):245–53. doi:10.1177/1090198116647712.
Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv. 2015;9(2):305–38.
Green HJ, Steinnagel G, Morris C, Laakso EL. Health behaviour models and patient preferences regarding nutrition and physical activity after breast or prostate cancer diagnosis. Eur J Cancer Care. 2014;23(5):640–52.
Husebø AML, Dyrstad SM, Søreide JA, Bru E. Predicting exercise adherence in cancer patients and survivors: a systematic review and meta-analysis of motivational and behavioural factors. J Clin Nurs. 2013;22(1-2):4–21.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986.
Courneya KS, Segal RJ, Reid RD, Jones LW, Malone SC, Venner PM, et al. Three independent factors predicted adherence in a randomized controlled trial of resistance exercise training among prostate cancer survivors. J Clin Epidemiol. 2004;57(6):571–9.
Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37(2):122–47.
Parsons JK, Newman VA, Mohler JL, Pierce JP, Flatt S, Marshall J. Dietary modification in patients with prostate cancer on active surveillance: a randomized, multicentre feasibility study. BJU Int. 2008;101(10):1227–31.
Livingston PM, Salmon J, Courneya KS, Gaskin CJ, Craike M, Botti M, et al. Efficacy of a referral and physical activity program for survivors of prostate cancer [ENGAGE]: rationale and design for a cluster randomised controlled trial. BMC Cancer. 2011;11(1):1.
Mróz LW, Chapman GE, Oliffe JL, Bottorff JL. Men, food, and prostate cancer: gender influences on men’s diets. Am J Mens Health. 2011;5(2):177–87.
Mandair D, Rossi RE, Pericleous M, Whyand T, Caplin ME. Prostate cancer and the influence of dietary factors and supplements: a systematic review. Nutr Metab. 2014;11(1):1.
Schleper A, Sullivan DK, Thrasher JB, Holzbeierlein JM, Klemp J, Befort C, Hamilton-Reeves JM. Weight management to reduce prostate cancer risk: a survey of men’s needs and interests. Cancer Clin Oncol. 2016;5(1):43.
Befort CA, Austin H, Klemp JR. Weight control needs and experiences among rural breast cancer survivors. Psychooncology. 2011;20(10):1069–75.
LeMasters TJ, Madhavan SS, Sambamoorthi U, Kurian S. Health behaviors among breast, prostate, and colorectal cancer survivors: a US population-based case-control study, with comparisons by cancer type and gender. J Cancer Surviv. 2014;8(3):336–48.
Jansen L, Herrmann A, Stegmaier C, Singer S, Brenner H, Arndt V. Health-related quality of life during the 10 years after diagnosis of colorectal cancer: a population-based study. J Clin Oncol. 2011;29(24):3263–9.
Krouse RS, Herrinton LJ, Grant M, Wendel CS, Green SB, Mohler MJ, et al. Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. J Clin Oncol. 2009;27(28):4664–70.
Hannum SM, Clegg Smith K, Coa K, Klassen AC. Identity reconstruction among older cancer survivors: age and meaning in the context of a life-altering illness. J Psychosoc Oncol. 2016:1–16.
Bradley CJ, Dahman B, Anscher M. Prostate cancer treatment and survival: evidence for men with prevalent comorbid conditions. Med Care. 2014;52(6):482.
Demark-Wahnefried W, Aziz NM, Rowland JH, Pinto BM. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol. 2005;23(24):5814–30.
Chamie K, Daskivich TJ, Kwan L, Labo J, Dash A, Greenfield S, Litwin MS. Comorbidities, treatment and ensuing survival in men with prostate cancer. J Gen Intern Med. 2012;27(5):492–9.
Lund L, Borre M, Jacobsen J, Sørensen HT, Nørgaard M. Impact of comorbidity on survival of Danish prostate cancer patients, 1995–2006: a population-based cohort study. Urology. 2008;72(6):1258–62.
Smith KC, Klassen AC, Coa KI, Hannum SM. The salience of cancer and the “survivor” identity for people who have completed acute cancer treatment: a qualitative study. J Cancer Surviv. 2016;10(3):457–66.
Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, Incrocci L. Cancer and sexual problems. J Sex Med. 2010;7(1pt2):349–73.
Bober SL, Varela VS. Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol. 2012;30(30):3712–9.
Cormie P, Newton RU, Taaffe DR, Spry N, Galvão DA. Exercise therapy for sexual dysfunction after prostate cancer. Nat Rev Urol. 2013;10(12):731–6.
Zaider T, Manne S, Nelson C, Mulhall J, Kissane D. Loss of masculine identity, marital affection, and sexual bother in men with localized prostate cancer. J Sex Med. 2012;9(10):2724–32.
Davison BJ, Gleave ME, Goldenberg SL, Degner LF, Hoffart D, Berkowitz J. Assessing information and decision preferences of men with prostate cancer and their partners. Cancer Nurs. 2002;25(1):42–9.
Cormie P, Newton RU, Taaffe DR, Spry N, Joseph D, Hamid MA, Galvao DA. Exercise maintains sexual activity in men undergoing androgen suppression for prostate cancer: a randomized controlled trial. Prostate Cancer Prostatic Dis. 2013;16(2):170–5.
Courneya KS. Exercise in cancer survivors: an overview of research. Med Sci Sports Exerc. 2003;35(11):1846–52.
Silk KJ, Atkin CK, Salmon CT. Developing effective media campaigns for health promotion. In: Thompson TL, Parrott R, Nussbaum JF, editors. The Routledge handbook of health communication. New York: Routledge; 2011. p. 203–20.
Atkin CK, Rice RE. Theory and principles of public communication campaigns. In: Rice RE, Atkin CK, editors. Public communication campaigns. London: Sage; 2013. p. 3–19.
Clayman ML, Manganello JA, Viswanath K, Hesse BW, Arora NK. Providing health messages to Hispanics/Latinos: understanding the importance of language, trust in health information sources, and media use. J Health Commun. 2010;15(suppl 3):252–63.
Jones LW, Courneya KS, Fairey AS, Mackey JR. Effects of an oncologist’s recommendation to exercise on self-reported exercise behavior in newly diagnosed breast cancer survivors: a single-blind, randomized controlled trial. Ann Behav Med. 2004;28(2):105–13.
Roberts CS, Baker F, Hann D, Runfola J, Witt C, McDonald J, et al. Patient-physician communication regarding use of complementary therapies during cancer treatment. J Psychosoc Oncol. 2006;23(4):35–60.
Dorsay JP, Cheifetz O. Cancer and exercise: a survey of patients’ knowledge and preferences. Arch Phys Med Rehabil. 2008;89:e27.
Institute of Medicine. Implementing survivorship care planning. Washington, DC. 2007.
Livingston PM, Craike MJ, Salmon J, Courneya KS, Gaskin CJ, Fraser SF, et al. Effects of a clinician referral and exercise program for men who have completed active treatment for prostate cancer: a multicenter cluster randomized controlled trial (ENGAGE). Cancer. 2015;121(15):2646–54.
Webb J, Foster J, Poulter E. Increasing the frequency of physical activity very brief advice for cancer patients. Development of an intervention using the behaviour change wheel. Public Health. 2016;133:45–56.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):1.
Murphy JL, Girot EA. The importance of nutrition, diet and lifestyle advice for cancer survivors–the role of nursing staff and interprofessional workers. J Clin Nurs. 2013;22(11–12):1539–49.
Wootten AC, Abbott JM, Osborne D, Austin DW, Klein B, Costello AJ, Murphy DG. The impact of prostate cancer on partners: a qualitative exploration. Psychooncology. 2014;23(11):1252–8.
Allen P, Sachs C. Women and food chains: The gendered politics of food. Int J Sociol Food Agric. 2012;15(1):1–23.
Song L, Rini C, Deal AM, Nielsen ME, Chang H, Kinneer P, Palmer MH. Improving couples’ quality of life through a web-based prostate cancer education intervention. Oncol Nurs Forum. 2015, March;42(2):183–92.
Weber BA, Roberts BL, Resnick M, Deimling G, Zauszniewski JA, Musil C, Yarandi HN. The effect of dyadic intervention on self-efficacy, social support, and depression for men with prostate cancer. Psychooncology. 2004;13(1):47–60.
Morey MC, Snyder DC, Sloane R, Cohen HJ, Peterson B, Hartman TJ, et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA. 2009;301(18):1883–91.
Witham MD, McMurdo ME. How to get older people included in clinical studies. Drugs Aging. 2007;24(3):187–96.
Norton MC, Breitner J, Welsh KA, Wyse BW. Characteristics of nonresponders in a community survey of the elderly. J Am Geriatr Soc. 1994;42(12):1252–6.
Ashing-Giwa K. The recruitment of breast cancer survivors into cancer control studies: a focus on African-American women. J Natl Med Assoc. 1999;91(5):255.
Li J, Thompson TD, Richards TB, Steele CB. Peer reviewed: racial and ethnic differences in health behaviors and preventive health services among prostate cancer survivors in the United States. Prev Chronic Dis. 2016;13:E95.
Allen JD, Kennedy M, Wilson-Glover A, Gilligan TD. African-American men’s perceptions about prostate cancer: implications for designing educational interventions. Soc Sci Med. 2007;64(11):2189–200.
Maliski SL, Husain M, Connor SE, Litwin MS. Alliance of support for low-income Latino men with prostate cancer: god, doctor, and self. J Relig Health. 2012;51(3):752–62.
Alfano CM, Bluethmann SM, Tesauro G, Perna F, Agurs-Collins T, Elena JW, et al. NCI funding trends and priorities in physical activity and energy balance research among cancer survivors. J Natl Cancer Inst. 2016;108(1):djv285.
Patrick K, Calfas KJ, Norman GJ, Rosenberg D, Zabinski MF, Sallis JF, et al. Outcomes of a 12-month web-based intervention for overweight and obese men. Ann Behav Med. 2011;42(3):391–401.
Le D, Holt CL, Saunders DR, Wang MQ, Coriolan A, Savoy AD, et al. Feasibility and acceptability of SMS text messaging in a prostate cancer educational intervention for African American men. Health Informatics J. 2015;22(4):932–47.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Rivera, Y.M., Smith, K.C. (2018). Energy Balance-Based Strategies to Reduce Consequences of Prostate Cancer: How to Communicate with Men. In: Platz, E., Berger, N. (eds) Energy Balance and Prostate Cancer. Energy Balance and Cancer, vol 14. Springer, Cham. https://doi.org/10.1007/978-3-319-64940-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-64940-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-64939-9
Online ISBN: 978-3-319-64940-5
eBook Packages: MedicineMedicine (R0)