Abstract
Acute promyelocytic leukemia (APL) uncommonly occurs following exposure to cytotoxic drugs or ionizing radiation as a therapy-related myeloid neoplasm (t-MN), classified as therapy-related APL (t-APL). However, the clinical and pathologic features of t-APL closely resemble those of de novo APL, and t-APL is associated with a similarly favorable prognosis. Investigation into the molecular pathogenesis of t-APL has revealed novel mechanisms of leukemogenesis and consequently has provided insights into de novo APL development. This chapter will cover disease features, pathogenesis, treatment options, and outcomes for t-APL.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute promyelocytic leukemia
- Therapy-related myeloid neoplasms
- All-trans retinoic acid
- Arsenic trioxide
- Topoisomerase II inhibitors
- Radiation therapy
Introduction
Exposure to DNA-damaging agents, either by certain cytotoxic drugs or by radiation therapy, has been shown to predispose to later development of myeloid malignancies including myelodysplastic syndrome (MDS), myeloproliferative neoplasms (MPN), and acute myeloid leukemia (AML), which together constitute the World Health Organization category of therapy-related myeloid neoplasms (t-MN) [1]. t-MN currently accounts for about 10–20% of AML and MDS cases and exhibits characteristic chromosomal abnormalities and latency periods as well as poor prognoses in most cases [2]. t-MN after exposure to alkylating agents or radiation typically develops 5–7 years after initial therapy and is most often associated with a complex karyotype or abnormalities of chromosomes 5 or 7. There is often an antecedent myelodysplastic phase [3, 4]. t-MN after exposure to topoisomerase II inhibitors develops more quickly, generally within 1–3 years, and often involves rearrangements at chromosome bands11q23 or 21q22 [5, 6].
Less commonly, t-MN will present with a t(15;17)(q22;q21) and clinical features of acute promyelocytic leukemia (APL). These cases of therapy-related acute promyelocytic leukemia (t-APL) most commonly arise after exposure to topoisomerase II inhibitors but have also been observed after alkylating agents, antimitotic agents, and radiation therapy. t-APL represents a distinct subset of t-MN with clinical features, treatment options, and prognosis similar to those now seen in de novo APL.
Several rich sources of clinical information on t-APL are available in the literature and will be discussed throughout this chapter (see Table 19.1). In the largest series of t-APL cases to date, Beaumont et al. examined in detail 106 cases of t-APL diagnosed at 45 medical centers in three European countries between 1982 and 2001 [7]. In the same article, that group reviewed 77 pooled case reports from the literature up to that point [8]. In 2000, the International Workshop on the relationship of prior therapy to balanced chromosome aberrations in therapy-related myelodysplastic syndromes and acute leukemia was held in Chicago and described 511 cases of t-MNs, including 41 cases of t-APL [9]. In addition, Pulsoni et al. reported on the Italian cooperative group Gruppo Italiano Malattie EMatologiche dell’Adulto (GIMEMA) experience between 1984 and 1998 comparing 51 cases of t-APL to 641 cases of de novo APL [10]. Together, these reports help form the basis of clinical knowledge of t-APL.
Epidemiology
t-APL is an uncommon disease that accounts for a small proportion of all APL and t-MN cases. Earlier studies in particular highlighted the infrequency of t-APL diagnoses. Detourmignies et al. examined 284 cases of APL that were diagnosed between 1982 and 1991 at 7 European medical centers and found that only 16 cases (5.6%) were related to prior cytotoxic therapy [8]. Among the GIMEMA APL cohort, t-APL accounted for 4.8% of the 51 cases studied [10]. Kantarjian et al. reported on 112 patients with t-MNs seen at the MD Anderson Cancer Center between 1973 and1985 and found that only two cases (1.8%) had a t(15;17) [11]. Among 63 patients with t-MNs seen at the University of Chicago prior to 1985, 2 (3%) had a t(15;17) and clinical characteristics of APL [12]. The 2000 International Workshop in Chicago identified 8% of t-MN with balanced chromosome aberrations as t-APL [9].
While still rare, the incidence of t-APL appears to be on the rise although this may be the result of greater recognition for this striking disease. Beaumont et al. reported on 106 patients with t-APL diagnosed between 1982 and 2001 in France, Spain, and Belgium and found that 26 of those patients were diagnosed with t-APL in the first 10-year period, compared to 80 who were diagnosed in the second 10-year period [7]. Other centers have noted an apparent increase in the number of cases of t-APL as well, even after retrospectively examining all prior APL diagnoses to determine whether prior cytotoxic exposure had been overlooked and the therapy-related cases had been misclassified in earlier years. At the University Hospital of Lille, France, the proportion of APL cases that occurred after prior cytotoxic therapy rose considerably from 5% in the 1984–1993 period to 22% between 1994 and 2000 [7, 13]. A similar trend was noted at the MD Anderson Cancer Center, where 2% of all APL cases were therapy-related in 1986, compared to 12% in 1996 [11, 14]. Therefore, there may be a true increase in the incidence of t-APL as opposed to increased recognition of t-APL as an entity. This rise largely parallels the rising incidence of t-MN overall over the past few decades and may reflect increased use of specific leukemogenic therapies as well as improved survivorship from primary malignancies [15, 16].
Disease Presentation
Clinical Features
In general, clinical characteristics seen in t-APL parallel those of de novo APL. t-APL is seen across all adult age groups, with median age at diagnosis between 49 and 57 years [7,8,9,10]. Hematologic parameters are comparable between therapy-related and de novo groups [7, 9, 10]. Female predominance of t-APL has been demonstrated in multiple studies, most likely reflecting the frequency of topoisomerase II inhibitor use and radiation therapy for the treatment of breast and gynecologic malignancies [7, 9, 10, 14]. This differs from de novo APL, which exhibits no predisposition by sex. The GIMEMA group noted several other differences in those with t-APL compared to de novo disease in their study [10]. They found that those with t-APL presented with a worse performance status (P < 0.005) and older age (P < 0.05). Those with therapy-related disease also had higher fibrinogen levels and few hemorrhagic complications than their de novo counterparts. Elliott et al. found a slightly lower BMI in patients with therapy-related disease, but other clinical features were similar [17]. Overall, these few small differences in clinical features do not translate to differences in clinical outcome, as will be discussed below.
Pathologic Features
Pathologic features of t-APL, including cytologic, cytogenetic, and molecular abnormalities, have been shown to be similar to those seen in de novo APL. Duffield et al. compared bone marrow specimen from nine patients with t-APL to those with de novo disease and found no differences in morphology or immunophenotype between the two groups [18]. In contrast to non-promyelocytic t-MN where an antecedent myelodysplastic phase is common, cases of t-APL lack such a phase and present with overt leukemia [7, 19].
In addition to t(15;17), other chromosomal abnormalities occasionally occur in APL. The incidence and types of additional abnormalities found in t-APL are similar to those also seen in de novo APL. While the prognostic impact of additional chromosomal abnormalities in APL has been a matter of debate in the past, in the current era of therapy, they do not seem to confer adverse risk [20,21,22,23]. Overall in APL, 26–33% of cases harbor additional chromosomal abnormalities, the most common being trisomy 8 (12%), followed by abnormalities in chromosomes 9 (2%), 7 (2%), 21 (2%), and 17 (1%) [20]. Beaumont et al. reported a similar incidence of additional chromosomal abnormalities in t-APL, with a slightly different distribution. Within this group, trisomy 8 was seen in only 5% of cases, and the remaining abnormalities predominantly involved chromosomes 5, 7, or 17 [7]. Among the 41 cases analyzed through the International Workshop, 41% of cases included additional abnormalities, most frequently trisomy 8 in 12%. There was no association between additional chromosomal abnormalities and either age or type of previous therapy in this series. While occasional variant translocations involving RARA that confer resistance to standard therapy have been reported in de novo APL, they are rare, and such cytogenetic variants have not been reported in t-APL.
Molecular profiling has been reported for a small number of patients with t-APL. FMS-like tyrosine kinase-3 receptor (FLT3) gene mutations are commonly seen in de novo APL. However, they do not appear to connote the same negative prognosis that is seen in non-promyelocytic AML. Several groups have compared the frequency of FLT3 mutations between therapy-related and de novo APL cases and reported somewhat discordant results. Yin et al. found a high incidence of FLT3 mutations (42% of 12 t-APL cases studied) [24]. Ottone et al. found a similar incidence, 30% in t-APL compared to 44% in de novo APL (P = 0.50) [25]. Duffield et al. found that all five t-APL cases studied had a FLT3 mutation compared to 59% of de novo cases (P = 0.41) [18]. This variation may be due to the small numbers in each series and to differences in the patient population studied. One study focused on patients with prior malignancies, while another focused on patients with multiple sclerosis (MS). Ottone et al. also tested for mutations in several other genes associated with myeloid malignancies, including tet oncogene family member 2 (TET2) , isocitrate dehydrogenases 1 and 2 (IDH1 and IDH2), and DNA methyltransferase 3A (DNMT3A) [25]. They found a DNMT3A pathogenic mutation in one t-APL case but none in the de novo APL group. They reported one IDH1 mutation in a de novo case. TET2 polymorphisms were common in both groups. Further evaluation with larger cohort sizes and more extensive mutation panels will clarify the mutational profiles of these two disorders.
Prior Diagnosis and Exposures
t-APL has been reported following a variety of therapies used for several different malignant and nonmalignant disorders (see Table 19.2). The most commonly implicated antecedent therapies are topoisomerase II-targeting agents such as mitoxantrone, etoposide, and anthracyclines (particularly epirubicin) [7, 9, 10]. The mechanism by which topoisomerase II inhibitors initiate development of t-APL has been described in detail by Grimwade and colleagues and will be discussed below (see Pathogenesis). However, t-APL has also been described after treatment with other DNA-damaging therapies such as alkylating agents, antimetabolites, external beam radiation, and radioactive iodine. The leukemogenic risk may be dose-dependent for some agents such as etoposide, but not for others such as mitoxantrone [26,27,28]. While t-APL typically develops rapidly with a median latency of 25–32 months, cases have been reported as early as 4 months after first exposure and as late as 276 months after therapy [7, 9, 28, 29]. Thus, the latency period, both at median and the range, is similar to what is observed in cases of non-promyelocytic t-MN that develops after topoisomerase II inhibitors.
The majority of t-APL cases have arisen after treatment for solid malignancies. In the Beaumont series of 106 t-APL cases, the most common primary disorder was breast cancer (60%) followed by non-Hodgkin lymphoma (15%), Hodgkin lymphoma (2%), uterine cancer (4%), lung cancer (1%), other solid tumors (19%), and, rarely, nonmalignant disorders (2%). Treatments for these primary tumors included chemotherapy alone (28%), radiation alone (26%), or both (46%). Most patients received an alkylating agent or a topoisomerase II inhibitor, in 64% and 57%, respectively [7]. Findings were similar in the 41 patients included in the International Workshop, where breast cancer was again the most common primary diagnosis (44%), followed by non-Hodgkin lymphoma (17%), Hodgkin lymphoma (10%), other solid tumors (27%), and nonmalignant conditions (2%). Most had received both chemotherapy and radiation (54%), though in this series, fewer received chemotherapy alone (17%) and more received radiation alone (29%) [9].
While the largest series of t-APL cases have primarily identified those that develop after treatment of primary cancers, the literature is ripe with smaller series and case reports describing t-APL after treatment for nonmalignant disorders. Multiple reports describe an association between APL and psoriasis, particularly after treatment with the antimitotic drugs, bimolane and razoxane. Both of these drugs function through inhibition of topoisomerase II and were previously used in China to treat both neoplastic disorders and psoriasis [30, 31]. Ge et al. reported on 17 cases of APL in patients with psoriasis diagnosed over 10 years at the First Affiliated Hospital at Harbin Medical University, China [32]. These cases represented 8.3% of all APL diagnoses at that center during that time period. Only four patients had received prior therapy with bimolane, suggesting that there could be additional risk conferred by the underlying psoriasis itself. Another report by Wang et al. examined 100 cases of acute leukemia that developed in patients with psoriasis [33]. In their series, APL was by far the most common leukemia subtype, present in 53 of the cases. Of those, 40% had been treated with bimolane or related analogues, 42% had been treated with agents other than bimolane, and 18% had not been treated. Various theories have been proposed to explain the increased leukemia susceptibility among patients with psoriasis even in the absence of treatment, including antigenic stimulation, and the presence of chromosomal fragile sites [34, 35]. Interestingly, downregulation of the retinoic acid receptor alpha (RARA) in the epidermis leads to abnormal keratinocyte proliferation that is responsive to retinoic acid therapy, suggesting some biologic similarity between APL and psoriasis. These authors speculate that additional predisposition to APL may exist in these psoriasis patients even prior to DNA-damaging agents [36, 37].
Children treated for Langerhans cell histiocytosis (LCH) with etoposide have also been found to have increased risk for t-APL. In an analysis of 77 case reports of t-APL, 12 of those cases were found to have occurred in children with LCH. All 12 had been treated with etoposide, and 9 of the 12 had received cumulative doses >4500 mg/m2 [7, 26, 27]. However, in another series of 348 patients with LCH treated at several European medical centers with etoposide, no cases of t-APL were reported. In this series, all patients received total etoposide doses of <2000 mg/m2, suggesting a dose-dependent leukemogenic effect of this agent [26].
Similarly, patients with multiple sclerosis (MS) treated with the topoisomerase II inhibitor mitoxantrone have developed t-APL. Ammatuna et al. reported on 33 patients at various European medical centers who had MS and were subsequently diagnosed with t-APL [28]. Among those patients, 30/33 had received mitoxantrone . Their median cumulative dose of mitoxantrone was 112 mg and ranged from only 14 mg in one patient up to 242 mg, suggesting an idiosyncratic relationship and the lack of a dose-response risk in this situation. The three patients who had not received mitoxantrone had been treated with steroids alone, interferon beta with sequential steroids, and interferon beta plus azathioprine. Many additional case reports of t-APL after mitoxantrone for MS can be found in the literature [38,39,40,41,42,43,44,45,46]. Other leukemogenic risk factors may be present in some patients with MS, such as genetic variants involving DNA repair (BRCA2 and XRCC5) that could predispose to translocation events or variants affecting the metabolism of chemotherapeutics (such as CYP3A4) that could result in increased cellular exposure to drugs such as mitoxantrone [47].
Several cases of APL after immunosuppressive treatment alone for nonmalignant conditions have been reported, but it is controversial whether these cases should be considered therapy-related. In Japanese centers, two children developed APL after receiving living donor partial orthotopic liver transplantation. The first was 12 years old and received a liver transplant for ornithine transcarbamylase deficiency, followed by tacrolimus and azathioprine immunosuppression posttransplant. Azathioprine has been associated with t-MN after solid organ transplantation [48]. The second, a 4-year-old girl, received a liver transplant for congenital biliary atresia and received tacrolimus after transplant. APL developed after latencies of 21 months and 46 months, respectively. Both were treated with all-trans retinoic acid (ATRA, tretinoin) and chemotherapy, and both attained complete remissions (CR), which were ongoing at the time of publication [49]. One case of APL in a patient with Crohn’s disease treated with the anti-TNF alpha monoclonal antibody infliximab has been reported in the literature [50]. It would be difficult to infer causality from this single case report alone. Treatment with TNF antagonists and the presence of inflammatory bowel disease have both been associated with increased risk of developing lymphoid neoplasms, but a causal link to myeloid neoplasms remains unclear [51,52,53,54].
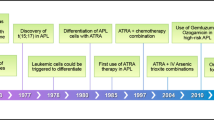
Pathogenesis
In virtually all cases of APL, a balanced translocation between the long arms of chromosomes 15 and 17 results in juxtaposition of the promyelocytic leukemia (PML) gene with the retinoic acid receptor alpha (RARA) gene [55, 56]. The resulting PML-RARA fusion protein functions as an aberrant retinoid receptor that resists physiologic retinoid-induced differentiation of myeloid cells [57]. In cases of de novo APL, the inciting factors that lead to this translocation event are largely unknown. In contrast, in t-APL, the molecular mechanisms underlying the cleavage of DNA strands and subsequent translocation are well described. This is particularly true after treatment with topoisomerase II inhibitors, which represents the most common setting for development of t-APL.
Topoisomerases are enzymes that regulate the DNA topology through the introduction of single- or double-stranded DNA breaks at specific breakpoints. In the case of topoisomerase II, the enzyme generates transient double-stranded breaks through the formation of a covalent cleavage complex, thus allowing for modulation of DNA supercoiling and release of knots or tangles. DNA repair mechanisms subsequently religate the cleaved DNA strands. Modern pharmacology has been successful in exploiting these mechanisms for therapeutic purposes, and today topoisomerase II is a crucial target for a number of chemotherapeutic agents. Chemotherapeutics that affect topoisomerase II can be divided into two categories. The first includes compounds that decrease the overall activity of the enzyme, such as anthracyclines (i.e., epirubicin, daunorubicin, and doxorubicin). The second group increases transition levels of the topoisomerase II-DNA cleavage complexes, leading to inhibition of cell replication and transcription. Drugs in this category are referred to as topoisomerase II poisons and include etoposide and mitoxantrone [58, 59].
The association between myeloid neoplasms and topoisomerase II-damaging agents has been recognized for quite some time, but only more recently have the molecular mechanisms underlying this relationship come to light. Mistry et al. examined differences in the genomic breakpoint regions between three groups of patients: those with t-APL that developed after exposure to mitoxantrone , those with t-APL that developed after other exposures (e.g., radiation therapy or epirubicin), and those with de novo APL [60]. They found that the breakpoints in cases of t-APL arising after mitoxantrone treatment were clustered in an eight base pair region in intron 6 within the PML gene. This breakpoint region corresponded to a site that was preferentially cleaved by mitoxantrone at nine times the frequency that was seen in the absence of the drug. While breakpoints in RARA were more dispersed, they similarly corresponded to preferential sites of DNA cleavage by mitoxantrone. Short, homologous sequences in PML and RARA were observed, suggesting that DNA repair occurred by nonhomologous end joining. One of their patients had only received 15 mg of mitoxantrone, supporting previous observations for an absence of dose-response effect with mitoxantrone. A subsequent series of 12 patients with t-APL that developed after treatment with mitoxantrone for MS demonstrated that the PML breakpoint fell within the previously identified breakage “hotspot” in 42% of cases [41]. An extension of this study included 23 patients with t-APL and demonstrated DNA breakpoints within the PML “hotspot” in 39% of t-APL cases overall, compared to none of the de novo cases (P = 0.007) [61]. In addition, breakpoints in RARA were found to cluster in a region of intron 2 in 65% of t-APL cases compared to 28% of de novo cases.
Patients who developed t-APL after treatment with epirubicin have also been found to share breakpoints that cluster within specific hotspots. Mays et al. examined genomic features in six patients who developed t-APL after treatment with epirubicin for breast cancer and observed specific breakpoint clustering within both PML and RARA loci [62]. Within PML, three of the six patients were found to have breakpoints in intron 6 that occurred at close approximation to one another, which was unlikely to occur by chance (P = 0.014). These intron 6 breakpoints occurred outside of the hotspot region that had previously been identified for mitoxantrone-induced APL cases. Other PML breakpoints were found in intron 3 and exon 7. The RARA breakpoints occurred within intron 2 in all six cases. In two of those cases, the breakpoints occurred within four nucleotides of each other, which was unlikely to occur by chance (P = 0.017). In all cases, the breakpoints in both chromosomes were found to occur at preferential sites for epirubicin-induced DNA cleavage by topoisomerase II.
From these observations, models have been generated by Grimwade and coworkers to depict the formation of the leukemogenic balanced translocation of chromosomes 15 and 17 after exposure to a topoisomerase II inhibitor (see Fig. 19.1) [62]. In this model, topoisomerase II induces 4 base pair nicks in double-stranded DNA at preferential sites within PML and RARA genes on chromosomes 15 and 17, respectively, and on other genes. Exonucleolytic processing occurs, followed by nonhomologous end joining. Gaps are filled by template-directed DNA polymerization and mismatch repair mechanisms, and strands are ligated. If this results in translocation between chromosomes 15 and 17, the PML-RARA fusion gene may be generated. The discovery of susceptible breakage sites and creation of this model for translocation formation have illuminated the likely molecular mechanisms for t-APL development and perhaps represent a step toward discovering mechanisms for the pathogenesis of de novo APL.
Model for the mechanism of PML-RARA translocation in topoisomerase II inhibitor-induced t-APL. (1) Topoisomerase II induces 4-bp nicks in double-stranded DNA at preferential sites within PML and RARA genes. (2) Exonucleases digest bases from 5′ overhang (indicated by black box). (3) Nonhomologous end joining occurs (indicated by black box), followed by template-directed DNA polymerization (indicated by gray text) and strand ligation, resulting in the formation of a PML-RARA fusion gene (Reproduced with permission) [62]
Treatment Approaches
While most t-MN confer a significantly worse prognosis compared to their cytogenetically matched de novo counterparts, those with APL seem to do similarly well regardless of whether the disease is related to prior cytotoxic therapy [2, 7, 10, 63, 64]. A report from the GIMEMA retrospectively identified 51 patients with APL after a prior cancer diagnosis and compared the outcomes of these patients to those with de novo APL [10]. The majority of t-APL patients (31 out of 51) were treated with a standard regimen of ATRA plus idarubicin. Despite older age and worse performance status among the t-APL patients in this series, outcomes were equally good between the two groups. CR rates were 97% and 93% in the t-APL group and de novo APL group, respectively, and 4-year overall survival (OS) was 85% and 78%, respectively. Other case series similarly show encouraging long-term survival for patients with t-APL treated with ATRA plus chemotherapy [7, 9, 65].
In the era of arsenic trioxide (ATO) therapy, these favorable and comparable outcomes between de novo and t-APL have held up. Dayyani et al. conducted a retrospective analysis of 29 patients with t-APL treated at the MD Anderson Cancer Center and compared outcomes of patients treated with ATRA/ATO (n = 19) to those treated with ATRA/anthracycline-based chemotherapy (n = 10) [66]. Remission rates were similar between the two groups, with CRs in 89% and 70%, respectively (P = 0.35). Median OS was not reached at last follow-up for the ATRA/ATO group, compared to 161 weeks for the ATRA/chemotherapy group (P = 0.79). Similarly, Ge et al. examined 17 patients with psoriasis-associated t-APL treated with ATO-based induction and post-remission therapy and reported an 88% CR rate and estimated a 3-year OS rate of 77% ± 12% [32]. Given this overall favorable response profile, patients with t-APL should be treated according to conventional APL treatment algorithms, and one can expect favorable outcomes quite similar to those with de novo disease. In contrast to other t-MN, intensification of therapy based on therapy-related status, such as inclusion of allogeneic stem cell transplantation, is typically not necessary in t-APL to achieve cure.
Although primary chemotherapy resistance is common in other t-MN subtypes, drug resistance is rare in t-APL. In de novo APL, acquired mutations in PML or RARA have been shown to confer resistance to ATRA or ATO infrequently [67,68,69,70,71]. One such case of ATO resistance in a patient with t-APL has been analyzed and reported on by Iaccarino et al. [72]. The patient was found to have a point mutation in PML in both the rearranged and unrearranged alleles, as well as two mutations in the rearranged RARA gene, none of which were present prior to ATO treatment. Madan et al. characterized the molecular signature of relapsed APL and found that mutations in PML or RARA were commonly acquired at the time of relapse [73]. Further study is needed to determine whether patients with APL may benefit from screening for these or similar mutations to identify those at risk for developing relapse or resistance.
Future Directions
While much has been learned about t-APL over the past 15 years, additional questions remain. Further clarification is needed regarding the apparent rise in incidence of t-APL in recent years. Preventive strategies such as minimizing exposure to topoisomerase II inhibitors and radiation therapy whenever possible may be helpful in mitigating this upturn. Whether adjunctive therapy with hematopoietic growth factors such as filgrastim facilitates the leukemogenic effects of intensive chemotherapy remains to be determined. Further evaluation of screening strategies for early detection of t-APL in the most high-risk situations, prior to the development of complications such as bleeding, is also warranted. A genetic predisposition to t-APL may exist in a proportion of patients, as is the case in other t-MNs; however, this requires further investigation [74]. In addition, molecular characterization of t-APL by high-throughput methods may identify those at higher risk for drug resistance or relapse. Lastly, models for the pathogenesis of t-APL may help elucidate mechanisms of de novo disease development.
Conclusions
Treatment with certain agents, particularly topoisomerase II inhibitors, can result in DNA damage within specific hotspots that predispose to development of balanced translocations in chromosomes 15 and 17. Radiation therapy is also implicated in these chromosomal rearrangements. t-APL is associated with a short latency period and typically develops within 2–3 years after the causative exposure. While the breakpoints in t-APL differ from those found in de novo APL, the phenotype that results is largely identical. Clinical and pathologic features of t-APL closely reflect those of de novo disease. Outcomes are similar to de novo APL, and same treatment algorithms should be employed.
Abbreviations
- AML:
-
Acute myeloid leukemia
- APL:
-
Acute promyelocytic leukemia
- ATO:
-
Arsenic trioxide
- ATRA:
-
All-trans retinoic acid (tretinoin)
- CR:
-
Complete remission
- DNMT3A:
-
DNA methyltransferase 3A
- FLT3:
-
FMS-like tyrosine kinase-3 receptor
- GIMEMA:
-
Gruppo Italiano Malattie EMatologiche dell’Adulto
- IDH1/2:
-
Isocitrate dehydrogenase 1 and 2
- LCH:
-
Langerhans cell histiocytosis
- MDS:
-
Myelodysplastic syndrome
- MS:
-
Multiple sclerosis
- OS:
-
Overall survival
- PML:
-
Promyelocytic leukemia
- RARA:
-
Retinoic acid receptor alpha
- RT:
-
Radiation therapy
- t-APL:
-
Therapy-related acute promyelocytic leukemia
- TET2:
-
Tet oncogene family member 2 isocitrate
- t-MN:
-
Therapy-related myeloid neoplasm
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. PubMed PMID: 27069254.
Granfeldt Ostgard LS, Medeiros BC, Sengelov H, Norgaard M, Andersen MK, Dufva IH, et al. Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: a National Population-Based Cohort Study. J Clin Oncol. 2015;33(31):3641–9. PubMed PMID: 26304885.
Rowley JD, Golomb HM, Vardiman JW. Nonrandom chromosome abnormalities in acute leukemia and dysmyelopoietic syndromes in patients with previously treated malignant disease. Blood. 1981;58(4):759–67. PubMed PMID: 7272506.
Traweek ST, Slovak ML, Nademanee AP, Brynes RK, Niland JC, Forman SJ. Clonal karyotypic hematopoietic cell abnormalities occurring after autologous bone marrow transplantation for Hodgkin’s disease and non-Hodgkin’s lymphoma. Blood. 1994;84(3):957–63. PubMed PMID: 8043877.
Pedersen-Bjergaard J, Rowley JD. The balanced and the unbalanced chromosome aberrations of acute myeloid leukemia may develop in different ways and may contribute differently to malignant transformation. Blood. 1994;83(10):2780–6. PubMed PMID: 8180374.
Ratain MJ, Rowley JD. Therapy-related acute myeloid leukemia secondary to inhibitors of topoisomerase II: from the bedside to the target genes. Ann Oncol. 1992;3(2):107–11. PubMed PMID: 1318741.
Beaumont M, Sanz M, Carli PM, Maloisel F, Thomas X, Detourmignies L, et al. Therapy-related acute promyelocytic leukemia. J Clin Oncol. 2003;21(11):2123–37. PubMed PMID: 12775738.
Detourmignies L, Castaigne S, Stoppa AM, Harousseau JL, Sadoun A, Janvier M, et al. Therapy-related acute promyelocytic leukemia: a report on 16 cases. J Clin Oncol. 1992;10(9):1430–5. PubMed PMID: 1517786.
Andersen MK, Larson RA, Mauritzson N, Schnittger S, Jhanwar SC, Pedersen-Bjergaard J. Balanced chromosome abnormalities inv(16) and t(15;17) in therapy-related myelodysplastic syndromes and acute leukemia: report from an international workshop. Genes Chromosomes Cancer. 2002;33(4):395–400. PubMed PMID: 11921273.
Pulsoni A, Pagano L, Lo Coco F, Avvisati G, Mele L, Di Bona E, et al. Clinicobiological features and outcome of acute promyelocytic leukemia occurring as a second tumor: the GIMEMA experience. Blood. 2002;100(6):1972–6. PubMed PMID: 12200354.
Kantarjian HM, Keating MJ, Walters RS, Beran M, McLaughlin P, McCredie KB, et al. The association of specific “favorable” cytogenetic abnormalities with secondary leukemia. Cancer. 1986;58(4):924–7. PubMed PMID: 3719557.
Le Beau MM, Albain KS, Larson RA, Vardiman JW, Davis EM, Blough RR, et al. Clinical and cytogenetic correlations in 63 patients with therapy-related myelodysplastic syndromes and acute nonlymphocytic leukemia: further evidence for characteristic abnormalities of chromosomes no. 5 and 7. J Clin Oncol. 1986;4(3):325–45. PubMed PMID: 3950675.
Beaumont, M, JL Lai, E Simonnet, C Preudhomme, I Plantier, B Quesnel, F Bauters, and P Fenaux. Therapy related acute promyelocytic leukemia (tAPL): increasing incidence, especially after nonHodgkin’s lymphoma (NHL) treated intensively? Blood. 2000;96(11):321a.
Pollicardo N, O’Brien S, Estey EH, al-Bitar M, Pierce S, Keating M, et al. Secondary acute promyelocytic leukemia. Characteristics and prognosis of 14 patients from a single institution. Leukemia. 1996;10(1):27–31. PubMed PMID: 8558933.
Allan JM, Travis LB. Mechanisms of therapy-related carcinogenesis. Nat Rev Cancer. 2005;5(12):943–55. PubMed PMID: 16294218.
Seedhouse C, Russell N. Advances in the understanding of susceptibility to treatment-related acute myeloid leukaemia. Br J Haematol. 2007;137(6):513–29. PubMed PMID: 17539774.
Elliott MA, Letendre L, Tefferi A, Hogan WJ, Hook C, Kaufmann SH, et al. Therapy-related acute promyelocytic leukemia: observations relating to APL pathogenesis and therapy. Eur J Haematol. 2012;88(3):237–43. PubMed PMID: 22023492.
Duffield AS, Aoki J, Levis M, Cowan K, Gocke CD, Burns KH, et al. Clinical and pathologic features of secondary acute promyelocytic leukemia. Am J Clin Pathol. 2012;137(3):395–402. PubMed PMID: 22338051. Pubmed Central PMCID: 3578661.
Pedersen-Bjergaard J, Christiansen DH, Desta F, Andersen MK. Alternative genetic pathways and cooperating genetic abnormalities in the pathogenesis of therapy-related myelodysplasia and acute myeloid leukemia. Leukemia. 2006;20(11):1943–9. PubMed PMID: 16990778.
De Botton S, Chevret S, Sanz M, Dombret H, Thomas X, Guerci A, et al. Additional chromosomal abnormalities in patients with acute promyelocytic leukaemia (APL) do not confer poor prognosis: results of APL 93 trial. Br J Haematol. 2000;111(3):801–6. PubMed PMID: 11122141.
Cervera J, Montesinos P, Hernandez-Rivas JM, Calasanz MJ, Aventin A, Ferro MT, et al. Additional chromosome abnormalities in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and chemotherapy. Haematologica. 2010;95(3):424–31. PubMed PMID: 19903674. Pubmed Central PMCID: 2833072.
Ono T, Takeshita A, Iwanaga M, Asou N, Naoe T, Ohno R, et al. Impact of additional chromosomal abnormalities in patients with acute promyelocytic leukemia: 10-year results of the Japan Adult Leukemia Study Group APL97 study. Haematologica. 2011;96(1):174–6. PubMed PMID: 20884714. Pubmed Central PMCID: 3012784.
Hernandez JM, Martin G, Gutierrez NC, Cervera J, Ferro MT, Calasanz MJ, et al. Additional cytogenetic changes do not influence the outcome of patients with newly diagnosed acute promyelocytic leukemia treated with an ATRA plus anthracyclin based protocol. A report of the Spanish group PETHEMA. Haematologica. 2001;86(8):807–13. PubMed PMID: 11522536.
Yin CC, Glassman AB, Lin P, Valbuena JR, Jones D, Luthra R, et al. Morphologic, cytogenetic, and molecular abnormalities in therapy-related acute promyelocytic leukemia. Am J Clin Pathol. 2005;123(6):840–8. PubMed PMID: 15899774.
Ottone T, Cicconi L, Hasan SK, Lavorgna S, Divona M, Voso MT, et al. Comparative molecular analysis of therapy-related and de novo acute promyelocytic leukemia. Leuk Res. 2012;36(4):474–8. PubMed PMID: 22071137.
Haupt R, Fears TR, Heise A, Gadner H, Loiacono G, De Terlizzi M, et al. Risk of secondary leukemia after treatment with etoposide (VP-16) for Langerhans’ cell histiocytosis in Italian and Austrian-German populations. Int J Cancer. 1997;71(1):9–13. PubMed PMID: 9096658.
Group TFLCHS. A multicentre retrospective survey of Langerhans’ cell histiocytosis: 348 cases observed between 1983 and 1993. The French Langerhans’ Cell Histiocytosis Study Group. Arch Dis Child. 1996;75(1):17–24. PubMed PMID: 8813865. Pubmed Central PMCID: 1511663.
Ammatuna E, Montesinos P, Hasan SK, Ramadan SM, Esteve J, Hubmann M, et al. Presenting features and treatment outcome of acute promyelocytic leukemia arising after multiple sclerosis. Haematologica. 2011;96(4):621–5. PubMed PMID: 21193421. Pubmed Central PMCID: 3069242.
Rowley JD, Olney HJ. International workshop on the relationship of prior therapy to balanced chromosome aberrations in therapy-related myelodysplastic syndromes and acute leukemia: overview report. Genes Chromosomes Cancer. 2002;33(4):331–45. PubMed PMID: 11921269.
Frantz CE, Smith H, Eades DM, Grosovsky AJ, Eastmond DA. Bimolane: in vitro inhibitor of human topoisomerase II. Cancer Lett. 1997;120(2):135–40. PubMed PMID: 9461029.
Xue Y, Lu D, Guo Y, Lin B. Specific chromosomal translocations and therapy-related leukemia induced by bimolane therapy for psoriasis. Leuk Res. 1992;16(11):1113–23. PubMed PMID: 1434747.
Ge F, Zhang Y, Cao F, Li J, Hou J, Wang P, et al. Arsenic trioxide-based therapy is suitable for patients with psoriasis-associated acute promyelocytic leukemia—a retrospective clinical study. Hematology. 2016;21(5):287–94. PubMed PMID: 26871996.
Wang Y, Mi Y, Li D, Xue Y, Bian S, Wang J. Acute leukemia association with psoriasis: a report on 100 patients from a single center in China. Am J Hematol. 2010;85(5):378–9. PubMed PMID: 20425800.
Soderberg KC, Jonsson F, Winqvist O, Hagmar L, Feychting M. Autoimmune diseases, asthma and risk of haematological malignancies: a nationwide case-control study in Sweden. Eur J Cancer. 2006;42(17):3028–33. PubMed PMID: 16945522.
Lu HL, Li WD, Wen HQ, et al. Chromosome aberration rate of lymphocytes in peripheral blood and fragile site of psoriasis patients. Chin J Dermatol. 1998;11:112.
van de Kerkhof PC. Update on retinoid therapy of psoriasis in: an update on the use of retinoids in dermatology. Dermatol Ther. 2006;19(5):252–63. PubMed PMID: 17014480.
Feng S, Lin L, Wu Q, Zhou W, Shao C. Study on the expression of RXRalpha in patients with psoriasis vulgaris. Eur J Dermatol. 2006;16(1):33–8. PubMed PMID: 16436339.
Ellis R, Boggild M. Therapy-related acute leukaemia with mitoxantrone: what is the risk and can we minimise it? Mult Scler. 2009;15(4):505–8. PubMed PMID: 19251838.
Colovic N, Suvajdzic N, Kraguljac Kurtovic N, Djordjevic V, Dencic Fekete M, Drulovic J, et al. Therapy-related acute leukemia in two patients with multiple sclerosis treated with Mitoxantrone. Biomed Pharmacother. 2012;66(3):173–4. PubMed PMID: 22440894.
Bosca I, Pascual AM, Casanova B, Coret F, Sanz MA. Four new cases of therapy-related acute promyelocytic leukemia after mitoxantrone. Neurology. 2008;71(6):457–8. PubMed PMID: 18678830.
Hasan SK, Mays AN, Ottone T, Ledda A, La Nasa G, Cattaneo C, et al. Molecular analysis of t(15;17) genomic breakpoints in secondary acute promyelocytic leukemia arising after treatment of multiple sclerosis. Blood. 2008;112(8):3383–90. PubMed PMID: 18650449. Pubmed Central PMCID: 2954750.
Ramkumar B, Chadha MK, Barcos M, Sait SN, Heyman MR, Baer MR. Acute promyelocytic leukemia after mitoxantrone therapy for multiple sclerosis. Cancer Genet Cytogenet. 2008;182(2):126–9. PubMed PMID: 18406875.
Ledda A, Caocci G, Spinicci G, Cocco E, Mamusa E, La Nasa G. Two new cases of acute promyelocytic leukemia following mitoxantrone treatment in patients with multiple sclerosis. Leukemia. 2006;20(12):2217–8. PubMed PMID: 17051242.
Nollet S, Berger E, Deconinck E, Baldauf E, Rumbach L. Acute leukaemia in two multiple sclerosis patients treated with mitoxantrone. Rev Neurol. 2006;162(2):195–9. PubMed PMID: 16518259. Leucemies aigues chez deux patients atteints de sclerose en plaques et traites par mitoxantrone.
Ghalie RG, Mauch E, Edan G, Hartung HP, Gonsette RE, Eisenmann S, et al. A study of therapy-related acute leukaemia after mitoxantrone therapy for multiple sclerosis. Mult Scler. 2002;8(5):441–5. PubMed PMID: 12356214.
Vicari AM, Ciceri F, Folli F, Lanzi R, Colombo B, Comi G, et al. Acute promyelocytic leukemia following mitoxantrone as single agent for the treatment of multiple sclerosis. Leukemia. 1998;12(3):441–2. PubMed PMID: 9529141.
Hasan SK, Buttari F, Ottone T, Voso MT, Hohaus S, Marasco E, et al. Risk of acute promyelocytic leukemia in multiple sclerosis: coding variants of DNA repair genes. Neurology. 2011;76(12):1059–65. PubMed PMID: 21346221.
Offman J, Opelz G, Doehler B, Cummins D, Halil O, Banner NR, et al. Defective DNA mismatch repair in acute myeloid leukemia/myelodysplastic syndrome after organ transplantation. Blood. 2004;104(3):822–8. PubMed PMID: 15090454.
Sato T, Kobayashi R, Iguchi A, Nakajima M, Koizumi S, Furukawa H, et al. Acute promyelocytic leukemia after living donor partial orthotopic liver transplantation in two Japanese girls. Leuk Lymphoma. 2005;46(7):1057–60. PubMed PMID: 16019558.
Mohammad F, Vivekanandarajah A, Haddad H, Shutty CM, Hurford MT, Dai Q. Acute promyelocytic leukaemia (APL) in a patient with Crohn’s disease and exposure to infliximab: a rare clinical presentation and review of the literature. BMJ Case Rep. 2014;2014. PubMed PMID: 24842356. Pubmed Central PMCID: 4039892.
Mir Madjlessi SH, Farmer RG, Weick JK. Inflammatory bowel disease and leukemia. A report of seven cases of leukemia in ulcerative colitis and Crohn’s disease and review of the literature. Dig Dis Sci. 1986;31(10):1025–31. PubMed PMID: 3463495.
Anderson LA, Pfeiffer RM, Landgren O, Gadalla S, Berndt SI, Engels EA. Risks of myeloid malignancies in patients with autoimmune conditions. Br J Cancer. 2009;100(5):822–8. PubMed PMID: 19259097. Pubmed Central PMCID: 2653768.
Askling J, Brandt L, Lapidus A, Karlen P, Bjorkholm M, Lofberg R, et al. Risk of haematopoietic cancer in patients with inflammatory bowel disease. Gut. 2005;54(5):617–22. PubMed PMID: 15831904. Pubmed Central PMCID: 1774486.
Brown SL, Greene MH, Gershon SK, Edwards ET, Braun MM. Tumor necrosis factor antagonist therapy and lymphoma development: twenty-six cases reported to the Food and Drug Administration. Arthritis Rheum. 2002;46(12):3151–8. PubMed PMID: 12483718.
de The H, Lavau C, Marchio A, Chomienne C, Degos L, Dejean A. The PML-RAR alpha fusion mRNA generated by the t(15;17) translocation in acute promyelocytic leukemia encodes a functionally altered RAR. Cell. 1991;66(4):675–84. PubMed PMID: 1652369.
Kakizuka A, Miller WH Jr, Umesono K, Warrell RP Jr, Frankel SR, Murty VV, et al. Chromosomal translocation t(15;17) in human acute promyelocytic leukemia fuses RAR alpha with a novel putative transcription factor, PML. Cell. 1991;66(4):663–74. PubMed PMID: 1652368.
Grignani F, Ferrucci PF, Testa U, Talamo G, Fagioli M, Alcalay M, et al. The acute promyelocytic leukemia-specific PML-RAR alpha fusion protein inhibits differentiation and promotes survival of myeloid precursor cells. Cell. 1993;74(3):423–31. PubMed PMID: 8394219.
Deweese JE, Osheroff N. The DNA cleavage reaction of topoisomerase II: wolf in sheep’s clothing. Nucleic Acids Res. 2009;37(3):738–48. PubMed PMID: 19042970. Pubmed Central PMCID: 2647315.
Lo-Coco F, Hasan SK. Understanding the molecular pathogenesis of acute promyelocytic leukemia. Best Pract Res Clin Haematol. 2014;27(1):3–9. PubMed PMID: 24907012.
Mistry AR, Felix CA, Whitmarsh RJ, Mason A, Reiter A, Cassinat B, et al. DNA topoisomerase II in therapy-related acute promyelocytic leukemia. N Engl J Med. 2005;352(15):1529–38. PubMed PMID: 15829534.
Hasan SK, Ottone T, Schlenk RF, Xiao Y, Wiemels JL, Mitra ME, et al. Analysis of t(15;17) chromosomal breakpoint sequences in therapy-related versus de novo acute promyelocytic leukemia: association of DNA breaks with specific DNA motifs at PML and RARA loci. Genes Chromosomes Cancer. 2010;49(8):726–32. PubMed PMID: 20544846.
Mays AN, Osheroff N, Xiao Y, Wiemels JL, Felix CA, Byl JA, et al. Evidence for direct involvement of epirubicin in the formation of chromosomal translocations in t(15;17) therapy-related acute promyelocytic leukemia. Blood. 2010;115(2):326–30. PubMed PMID: 19884644. Pubmed Central PMCID: 2808156.
Borthakur G, Lin E, Jain N, Estey EE, Cortes JE, O’Brien S, et al. Survival is poorer in patients with secondary core-binding factor acute myelogenous leukemia compared with de novo core-binding factor leukemia. Cancer. 2009;115(14):3217–21. PubMed PMID: 19441109. Pubmed Central PMCID: 4184418.
Larson RA, Le Beau MM. Prognosis and therapy when acute promyelocytic leukemia and other “good risk” acute myeloid leukemias occur as a therapy-related myeloid neoplasm. Mediterr J Hematol Infect Dis. 2011;3(1):e2011032. PubMed PMID: 21869918. Pubmed Central PMCID: 3152454.
Jantunen E, Heinonen K, Mahlamaki E, Penttila K, Kuittinen T, Lehtonen P, et al. Secondary acute promyelocytic leukemia: an increasingly common entity. Leuk Lymphoma. 2007;48(1):190–1. PubMed PMID: 17325866.
Dayyani F, Kantarjian H, O’Brien S, Pierce S, Jones D, Faderl S, et al. Outcome of therapy-related acute promyelocytic leukemia with or without arsenic trioxide as a component of frontline therapy. Cancer. 2011;117(1):110–5. PubMed PMID: 20803607. Pubmed Central PMCID: 4287232.
Schachter-Tokarz E, Kelaidi C, Cassinat B, Chomienne C, Gardin C, Raffoux E, et al. PML-RARalpha ligand-binding domain deletion mutations associated with reduced disease control and outcome after first relapse of APL. Leukemia. 2010;24(2):473–6. PubMed PMID: 19865110.
Gallagher RE, Moser BK, Racevskis J, Poire X, Bloomfield CD, Carroll AJ, et al. Treatment-influenced associations of PML-RARalpha mutations, FLT3 mutations, and additional chromosome abnormalities in relapsed acute promyelocytic leukemia. Blood. 2012;120(10):2098–108. PubMed PMID: 22734072. Pubmed Central PMCID: 3437597.
Tomita A, Kiyoi H, Naoe T. Mechanisms of action and resistance to all-trans retinoic acid (ATRA) and arsenic trioxide (As2O 3) in acute promyelocytic leukemia. Int J Hematol. 2013;97(6):717–25. PubMed PMID: 23670176.
Zhu HH, Qin YZ, Huang XJ. Resistance to arsenic therapy in acute promyelocytic leukemia. N Engl J Med. 2014;370(19):1864–6. PubMed PMID: 24806185.
Lehmann-Che J, Bally C, de The H. Resistance to therapy in acute promyelocytic leukemia. N Engl J Med. 2014;371(12):1170–2. PubMed PMID: 25229938.
Iaccarino L, Ottone T, Divona M, Cicconi L, Cairoli R, Voso MT, et al. Mutations affecting both the rearranged and the unrearranged PML alleles in refractory acute promyelocytic leukaemia. Br J Haematol. 2016;172(6):909–13. PubMed PMID: 26728337.
Madan V, Shyamsunder P, Han L, Mayakonda A, Nagata Y, Sundaresan J, et al. Comprehensive mutational analysis of primary and relapse acute promyelocytic leukemia. Leukemia. 2016;30(8):1672–81. PubMed PMID: 27063598. Pubmed Central PMCID: 4972641.
Churpek JE, Marquez R, Neistadt B, Claussen K, Lee MK, Churpek MM, et al. Inherited mutations in cancer susceptibility genes are common among breast cancer survivors who develop therapy-related leukemia. Cancer. 2016;122(2):304–11. https://doi.org/10.1002/cncr.29615. Epub 7 Dec 2015. PMID: 26641009.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Pettit, K., Larson, R.A. (2018). Therapy-Related Acute Promyelocytic Leukemia. In: Abla, O., Lo Coco, F., Sanz, M. (eds) Acute Promyelocytic Leukemia . Springer, Cham. https://doi.org/10.1007/978-3-319-64257-4_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-64257-4_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-64256-7
Online ISBN: 978-3-319-64257-4
eBook Packages: MedicineMedicine (R0)