Abstract
Atrial Fibrillation (AF)
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Name and Synonyms
Atrial Fibrillation (AF)
Incidence/Epidemiology
-
The most common cardiac arrhythmia
-
Affects 4 % of individuals older than 60 years and 8 % of those older than 80 years.
-
-
It is more prevalent in men, and prevalence increases with age.
-
In developed countries, hypertension and coronary artery disease are the most common underlying disorders.
-
Rheumatic heart disease is associated with a higher incidence of AF, but this is much less common than in the past. Other causes of mitral valve disease also may lead to AF.
-
Classified as follows:
-
Paroxysmal AF: terminates spontaneously or with intervention within 7 days of onset.
-
Persistent AF: does not terminate within 7 days.
-
Permanent AF: persists for a year or longer.
-
“Lone” AF: does not occur with any other clinical or echocardiographic cardiac problems; usually occurs in patients younger than 50.
-
Differential Diagnosis
-
Atrial flutter
-
Multifocal atrial tachycardia
-
Supraventricular tachycardia
Pathophysiology and Etiology
-
Instead of being coordinated, atrial contractions are irregular, disorganized, chaotic, and very rapid.
-
This electrical malfunction may result in:
-
Tachypalpitations, often described by patients as a “fluttering” or “butterflies” in the chest.
-
Inadequate “topping off” of the ventricular volume prior to ventricular systole, which may result in fatigue, dizziness, or heart failure.
-
-
Because the cardiac cycle of atrial systole followed by ventricular systole is disrupted by the lack of regularity of impulses through the atrioventricular node, the ventricles beat irregularly and often beat faster than normal.
-
This “irregularly irregular” rhythm is classified as showing a “controlled” ventricular response (rate <100 bpm) or “rapid” ventricular response (rate ≥100 bpm).
-
-
The precise mechanism that causes AF is not completely understood, but AF often is seen concomitantly with other heart and metabolic diseases, including:
-
Congestive heart failure
-
Coronary artery disease
-
Valvular heart disease
-
Hypertension
-
Hyperthyroidism
-
-
Acute alcohol abuse, especially in binges, may cause AF (“holiday heart”).

Focal atrial premature complexes usually originating from pulmonary veins can initiate AF. Ablation of these arrhythmogenic focal triggers can restore rhythm. This finding opens an exciting era in electrophysiology with the possibility of curing AF by ablation. [Grogin HR. Supraventricular tachycardia. In: Scheinman M, editor. Arrhythmias: electrophysiologic principles. Philadelphia: Current Medicine; 1996. Chapter 5 (Braunwald E, editor. Atlas of heart diseases; vol. 9).] Caption adapted from original

Causes of Atrial Fibrillation. [From article: Reversible atrial fibrillation secondary to a mega-oesophagus. BMC Ear Nose Throat Disord. 2006 Dec 13;6(1):15. https://doi.org/10.1186/1472-6815-6-15, at http://springerlink.bibliotecabuap.elogim.com/article/10.1186/1472-6815-6-15; by Tahwinder Upile, Waseem Jerjes, Mohammed El Maaytah, Sandeep Singh, Colin Hopper, Jaspal Mahil, © Upile et al; licensee BioMed Central Ltd. 2006; licensed under Creative Commons Attribution License BY 2.0 http://creativecommons.org/licenses/by/2.0] Caption from original

Atrial fibrillation is a multifactorial condition resulting from an interaction between cardiovascular disease effects, aging, genetics, and environmental factors. CAD coronary artery disease, COPD chronic obstructive pulmonary disease, EtOH alcohol use, HF heart failure, HTN hypertension, OSA obstructive sleep apnea, VHD valvular heart disease [Eleid MF, Cha Y-M, Shen W-K. Atrial fibrillation and heart failure: rate versus rhythm control. In: Bartunek J, Vanderheyden M, editors. Translational approach to heart failure [Internet]. New York: Springer; 2013 [cited 2015 Aug 13]. p. 129–44. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/978-1-4614-7345-9_6] Caption from original
Presentation
Typical/“Classic”
-
Not all patients with AF have symptoms, but the risk of thromboembolic complications is the same, regardless.
-
Typical symptoms include palpitations, tachycardia, fatigue, weakness, dizziness, lightheadedness, reduced exercise capacity, and dyspnea.
Atypical
-
The first presentation of AF may be a thromboembolic complication, such as stroke or mesenteric ischemia.
-
AF may present as anginal pain.
-
Some patients, particularly those who are elderly, may not notice the palpitations (particularly if the ventricular rate is less than 100 bpm) and may present with completely unrelated complaints.
Primary Differential Considerations
-
Atrial flutter
-
Multifocal atrial tachycardia
-
Supraventricular tachycardia
-
Premature atrial contractions
-
Premature ventricular contractions
History and Physical Exam
Findings That Confirm Diagnosis
-
Although an “irregularly irregular” pulse is suggestive of AF, this also may be associated with other arrhythmias, and an ECG is required to differentiate among them.
Factors That Suggest Diagnosis
-
Irregularly irregular pulse on examination
-
Palpitations plus dyspnea
-
Palpitations plus syncope or near-syncope
-
Palpitations and generalized weakness
-
Palpitations and hypotension
-
Unexplained dyspnea, syncope, generalized weakness, or hypotension
-
Acute ischemic stroke
Factors That Exclude Diagnosis
-
ECG showing a normal sinus rhythm excludes AF “in the moment,” but does not exclude paroxysmal AF.
Ancillary Studies
Laboratory
-
Often obtained in search for underlying disorders or other associated disorders:
-
B-type natriuretic peptide (BNP)
-
Troponin
-
Electrolytes
-
Blood glucose
-
Thyroid-stimulating hormone (TSH)
-
Toxicology
-
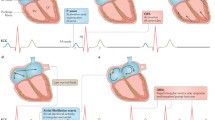
Electrocardiography
-
ECG is necessary to make the diagnosis.
-
Irregular rate with an atrial rate greater than 300 bpm
-
Ventricular rate may be slow, normal, or fast.
-
Absent or erratic P waves are noted.
-
PR interval is absent.
-
QRS may be normal but may be widened if conduction delay is present.

Atrial fibrillation. Atrial fibrillation is characterized by the absence of P waves, which are replaced by irregular f waves or no sign of atrial activity. The QRS complexes may be normal or irregular and varying in amplitude. The 12‐lead ECG shown here demonstrates atrial fibrillation with moderate ventricular response rate. [Leung J. Electrocardiographic monitoring. In: Lichtor JL, editor. Preoperative preparation and intraoperative monitoring. Philadelphia: Current Medicine; 1997. Chapter 7. (Miller RD, editor. Atlas of anesthesia; vol. 3).] Caption from original

Atrial fibrillation (AF) 12-lead surface electrocardiogram. AF is the most common sustained arrhythmia and is particularly prevalent in the elderly. Characteristic of AF is an irregular ventricular response and rapid irregular oscillations or fibrillatory waves that vary in shape, amplitude, and timing. [Epstein L, Stevenson W, Steven D, Seiler J, Roberts-Thomson K, See V. Arrhythmias. In: Libby P, editor. Essential atlas of cardiovascular disease. 4th ed. Philadelphia: Current Medicine; 2009. Chapter 7.] Caption from original
Imaging
-
Transthoracic echocardiography may be performed to evaluate the size of the right and left atria and size and function of the right and left ventricles; this also can detect valvular heart disease.
-
Transesophageal echocardiography is used to identify thrombi in the left atrium or left atrial appendage.
Special Populations
Age
-
Incidence of AF increases with advancing age.
-
“Lone AF” more common below age 50.
Co-morbidities
-
As under “Pathophysiology and Etiology,” a host of other cardiac and metabolic disorders are frequent co-morbidities in patients with AF.
-
Binge alcohol consumption predisposes to “holiday heart.”
Pitfalls in Diagnosis
Critical Steps Not to Miss
-
Complications such as blood clot formation, strokes, and heart failure may arise, but rhythm conversion reduces the chances that such complications will develop.
Mimics
-
Atrial flutter
-
Multifocal atrial tachycardia
-
Supraventricular tachycardia
Time-Dependent Interventions
-
Patients may have potentially life-threatening symptoms that need immediate intervention with electrical cardioversion, including decompensated congestive heart failure, hypotension, angina, or cardiac ischemia.
Overall Principles of Treatment
-
The initial focus of AF management is rate control to minimize any perfusion stress on the ventricles.
-
The usual approach is with titrated doses of calcium channel blockers or beta-blockers.
-
-
Once rate is controlled (or if patient presents with a controlled ventricular rate), consideration is given to converting the rhythm out of AF back into a sinus rhythm.
-
This may be approached pharmacologically with a variety of potential drugs, such as ibutilide or procainamide, or electrically via synchronized cardioversion.
-
-
If the patient has been in AF for 24 to 48 hours or longer, anticoagulation therapy should be provided before attempting cardioversion, as clots that may have formed in the fibrillating atria or atrial appendage may dislodge and embolize when normal atrial electrical activity is restored. Therapy may be provided acutely with parenteral agents such as unfractionated or low-molecular weight heparin or with fast-acting non-warfarin oral anticoagulants (dabigatran, rivaroxaban, apixaban, edoxaban)
-
Alternatively, cardioversion may be attempted after transesophageal echocardiography that excludes atrial clots
-
Likelihood of stroke or systemic embolization may be assessed with CHA2DS2-VASc score
-

CHADS2VASC score points for prediction of stroke in atrial fibrillation. (Data from Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of Clinical Classification Schemes for Predicting Stroke: Results From the National Registry of Atrial Fibrillation. JAMA.2001;285(22):2864-2870. https://doi.org/10.1001/jama.285.22.2864.) [Table from Verheugt FWA. The new oral anticoagulants. Netherlands Heart Journal. 2010 Jun;18(6):314–8.] Caption adapted from original
-
Patients whose AF is resistant to cardioversion or recurs after initially successful cardioversion may be referred to electrophysiology, where the possibility of catheter ablation of the electrical source of the AF can be addressed definitively and specifically.
-
Success rates usually exceed 65–75 %
-
Disease Course
-
The most feared complication of AF is thromboembolism to a critical vascular bed—especially stroke.
-
The palpitations of AF may have a very adverse effect on quality of life. They may be symptomatic even in patients with controlled ventricular response.
-
Patients with diminished pump function are particularly sensitive to the absence of consistent ventricular filling (the missing “atrial kick”) and may experience persistent easy fatigability and even angina.
-
Longstanding AF increases mortality.
Related Evidence
Papers of particular importance have been highlighted as:
** Of key importance
Practice Guideline
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014 Dec 2;64(21):e1-76. https://doi.org/10.1016/j.jacc.2014.03.022. PMID: 24685669. http://www.ncbi.nlm.nih.gov/pubmed/24685669 **
Verma A, Cairns JA, Mitchell LB, Macle L, Stiell IG, Gladstone D, McMurtry MS, Connolly S, Cox JL, Dorian P, Ivers N, Leblanc K, Nattel S, Healey JS; CCS Atrial Fibrillation Guidelines Committee. 2014 focused update of the Canadian Cardiovascular Society Guidelines for the management of atrial fibrillation. Can J Cardiol. 2014 Oct;30(10):1114-30. https://doi.org/10.1016/j.cjca.2014.08.001. PMID: 25262857. http://www.ncbi.nlm.nih.gov/pubmed/25262857 **
Steinberg BA, Beckley PD, Deering TF, Clark CL, Amin AN, Bauer KA, Cryer B, Mansour M, Scheiman JM, Zenati MA, Newby LK, Peacock WF, Bhatt DL; Society of Cardiovascular Patient Care. Evaluation and management of the atrial fibrillation patient: a report from the Society of Cardiovascular Patient Care. Crit Pathw Cardiol. 2013 Sep;12(3):107-15. https://doi.org/10.1097/HPC.0b013e31829834ed. PMID: 23892939. http://www.ncbi.nlm.nih.gov/pubmed/23892939 **
Frendl G, Sodickson AC, Chung MK, Waldo AL, Gersh BJ, Tisdale JE, Calkins H, Aranki S, Kaneko T, Cassivi S, Smith SC Jr, Darbar D, Wee JO, Waddell TK, Amar D, Adler D; American Association for Thoracic Surgery. 2014 AATS guidelines for the prevention and management of perioperative atrial fibrillation and flutter for thoracic surgical procedures. J Thorac Cardiovasc Surg. 2014 Sep;148(3):e153-93. https://doi.org/10.1016/j.jtcvs.2014.06.036. PMID: 25129609. http://www.ncbi.nlm.nih.gov/pubmed/25129609**
Review
Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol. 2014 Jun 16;6:213-20. https://doi.org/10.2147/CLEP.S47385. PMID: 24966695. http://www.ncbi.nlm.nih.gov/pubmed/24966695**
Ball J, Carrington MJ, McMurray JJ, Stewart S. Atrial fibrillation: profile and burden of an evolving epidemic in the 21st century. Int J Cardiol. 2013 Sep 1;167(5):1807-24. https://doi.org/10.1016/j.ijcard.2012.12.093. PMID: 23380698. http://www.ncbi.nlm.nih.gov/pubmed/23380698
Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015 Jan 27. https://doi.org/10.1038/nrcardio.2015.2. PMID: 25622848. http://www.ncbi.nlm.nih.gov/pubmed/25622848**
Mohmand-Borkowski A, Tang WH. Atrial fibrillation as manifestation and consequence of underlying cardiomyopathies: from common conditions to genetic diseases. Heart Fail Rev. 2014 May;19(3):295-304. https://doi.org/10.1007/s10741-014-9424-0. PMID: 24531802. http://www.ncbi.nlm.nih.gov/pubmed/24531802**
Longobardo L, Todaro MC, Zito C, Piccione MC, Di Bella G, Oreto L, Khandheria BK, Carerj S. Role of imaging in assessment of atrial fibrosis in patients with atrial fibrillation: state-of-the-art review. Eur Heart J Cardiovasc Imaging. 2014 Jan;15(1):1-5. https://doi.org/10.1093/ehjci/jet116. PMID: 23798579. http://www.ncbi.nlm.nih.gov/pubmed/23798579**
Chapa DW, Akintade B, Thomas SA, Friedmann E. Gender differences in stroke, mortality, and hospitalization among patients with atrial fibrillation: A systematic review. Heart Lung. 2015 Feb 19. pii: S0147-9563(15)00009-6. https://doi.org/10.1016/j.hrtlng.2015.01.008. PMID: 25703992. http://www.ncbi.nlm.nih.gov/pubmed/25703992**
Vergara P, Della Bella P. Management of atrial fibrillation. F1000Prime Rep. 2014 Apr 1;6:22. https://doi.org/10.12703/P6-22. PMID: 24765527. http://www.ncbi.nlm.nih.gov/pubmed/24765527**
Use PubMed Clinical Queries to find the most recent evidence. Use this search strategy:
“Atrial Fibrillation”[Mesh] OR “Atrial Fibrillation”
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Pollack Jr., C.V., Platt, M., Riese, V.G. (2019). Atrial Fibrillation. In: Pollack Jr., C. (eds) Differential Diagnosis of Cardiopulmonary Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-63895-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-63895-9_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63894-2
Online ISBN: 978-3-319-63895-9
eBook Packages: MedicineMedicine (R0)