Abstract
Iron oxide magnetic nanoparticles have been extensively employed in biomedical applications due to their biocompatibility, small size, ability to surface functionalization, superparamagnetism behavior, and targeting properties. Upon the application of external magnetic field , iron oxide nanoparticles can be guided to the target site of application, minimizing possible side effects to nontarget tissues. Recently, several papers describe the combination of iron oxide magnetic nanoparticles with photosensitizer (PS) molecules for photodynamic therapy (PDT). PDT is a clinical treatment based on the administration of a photosensitizer to the tumor site, which under the irradiation with visible-near-infrared light generates reactive oxygen species (ROS ) able to cause deleterious effects to the treated tumor site. The main disadvantage of PDT is the lack of selectivity; therefore, the combination of magnetic iron oxide nanoparticles with photosensitizer is a new and promising approach in PDT. In this direction, this chapter discusses the recent advantages in the design and applications of magnetic iron oxide nanoparticles in conjugation with photosensitizer in PDT to combat cancer .
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Iron oxide nanoparticles
- Photodynamic therapy
- Cytotoxicity
- Magnetic nanoparticles
- Singlet oxygen
- Fe3O4 nanoparticles
1 Introduction
Photodynamic therapy (PDT) is a clinical treatment that involves the administration of a photosensitizer (e.g., photofrin) in the tumor site (Bechet et al. 2008; Banerjee et al. 2017). Once at the tumor tissue, appropriated light irradiation (visible or near-infrared wavelengths) yields excited photosensitizer. Upon light activation, excited triplet photosensitizer in the presence of molecular oxygen (naturally available triplet-oxygen (3O2) produces highly reactive singlet oxygen (1O2), a well-known mediator of cell death (Allison et al. 2008; Chatterjee et al. 2008; Bhattacharyya et al. 2011; Smith et al. 2015). The efficiency of PDT depends on singlet oxygen formation, which is highly reactive and able to readily diffuse through the biological membranes (Bechet et al. 2008). Besides the generation of singlet oxygen, various free radicals are generated. All those reactive species might induce cell death via apoptosis, necrosis, and cell membrane damages with release of contents (Allison et al. 2008; Kim et al. 2016a; Lee et al. 2017). Indeed, singlet oxygen reacts with nucleic acids, lipids, amino acids, and proteins in the tumor tissue preventing angiogenesis in solid tumors (Smith et al. 2015). The generated oxygen-based cytotoxicity is expected to occur upon light irradiation, since in dark conditions, the photosensitizers are harmless. Therefore, in PDT light is used as a tool to trigger and modulate the selective destruction of malignant tissues/organs (Bechet et al. 2008). It should be noted that in PDT, the wavelength of light irradiation is a very important parameter. Irradiation in the near-infrared (NIR) region (700–1,000 nm) is the most appropriated wavelength to be employed. Hemoglobin is the major protein in the blood, which absorbs light up to 600 nm; therefore, tissues/organs must be irradiated at higher wavelengths to allow a suitable light penetration (Bechet et al. 2008; Huang et al. 2012; Chen et al. 2015a).
The clinical uses of PDT started in 1933, although it has been studied for over a century (Smith et al. 2015). Nowadays, there are several photosensitizers approved by the Food and Drug Administration (FDA) (Smith et al. 2015). The major clinical use of PDT is in cancer treatment (Bhattacharyya et al. 2011), although noncancerous applications have also been applied. Against cancer, PDT has been employed in the treatment of superficial tumors, such as melanoma, and tumors in the esophagus and bladder (Bechet et al. 2008). The noncancerous applications of PDT are mainly in the skin to treat diseases such as psoriasis and actinic keratosis, in the eyes in particular to treat macular degeneration, as well as at localized sites of inflammations including rheumatoid arthritis and dental infections (periodontitis) (Chatterjee et al. 2008). For example, a methylene blue (photosensitizer )-containing gel is applied to the infected gum pocket, and upon light irradiation via an optical fiber, singlet oxygen is locally generated in the infected pocket leading to cytotoxic effects (Chatterjee et al. 2008).
The advantages of PDT over traditional therapies are (i) relatively high cure rates, (ii) cost-effectiveness, (iii) localized treatment, (iv) no cumulative toxicity upon repetition of the therapy, and (v) induction of immunity (Chatterjee et al. 2008). In contrast, the disadvantages of PDT are the long in vivo half-life of the photosensitizers, consequently, their nonspecific distribution in vivo, and the limitation to reach deeper tumors in the body of the patient (Smith et al. 2015).
2 Why Use Superparamagnetic Iron Oxide Nanoparticles in PDT?
Although there are promising clinical uses of PDT, some drawbacks need to be overcome. For instance, the selective targeting and accumulation of the photosensitizers in the disease organ/tissue are necessary to minimize toxicity to normal cells (Bechet et al. 2008). Moreover, photosensitizers have poor water solubility and tend to aggregate in the biological medium, decreasing their photo-efficiency (Paszko et al. 2011).
The combination of photosensitizer and nanomaterials may overcome these issues. In this context, the combination of nanoparticles as carrier of photosensitizers is a promising approach in PDT (Bechet et al. 2008). The advantages of nanoparticles as nanocarriers of photosensitizers in PDT are:
(i) Ability to carry and to deliver therapeutic amounts of the photosensitizers in deep-seated tumors
(ii) Due to the high surface area/volume ratio, the nanoparticle surface can be used as multifunctional vehicle upon its functionalization with other therapeutic molecules, such as chemotherapeutical agents and/or tumor-seeking molecules
(iii) Enhanced solubility of hydrophobic photosensitizers with proper size to accumulate in the tumor tissues via enhanced permeability and retention effect (EPR effect) (Wang et al. 2004; Paszko et al. 2011; Gangopadhyay et al. 2015)
One of the major advantages of using nanoparticles in PDT is the EPR effect, which is the passive accumulation of nanoparticles in tumor sites (Kim et al. 2016a). This effect can be explained by considering the altered anatomy of tumor tissues characterized by an excessive angiogenesis and leaky blood vessels with impaired lymphatic drainage system. Therefore, nanoparticles can extravasate from blood pool and spontaneously accumulate into tumor sites. Once accumulated, the nanoparticles are retained in tumor tissues due to the compromised lymphatic drainage (Kelkar and Reineke 2011; Kim et al. 2016a, b). Interestingly, therapeutic amounts of photosensitizer -containing nanoparticles are accumulated in solid tumors due to EPR effect (Mbakidi et al. 2013), making nanoparticles promising vehicles for singlet oxygen generators in PDT.
Recently, iron oxide magnetic nanoparticles have been successfully employed as drug carriers for photosensitizers and also for chemotherapeutic agents. Magnetic nanoparticles such as magnetite (Fe3O4 ) have interesting properties that make them suitable nanocarriers in several biomedical applications. These properties can be summarized as: ability to reach the desired site of treatment upon application of an external magnetic field (magnetic targeting), high surface area, small size, biocompatibility, chemical stability, relatively low-cost production, and several different synthetic routes including chemical, physical, and biogenic synthesis (Seabra et al. 2013, 2014; Seabra and Duran 2015, Cheng et al. 2016). Therefore, iron oxide magnetic nanoparticles have been widely employed in several biomedical applications of targeted drug delivery system, magnetic resonance imaging, biosensing, immunoassay, and magnetic hyperthermia (Cheng et al. 2016). Magnetic hyperthermia can be allied to PDT to significantly enhance the cytotoxicity toward cancer tissues. Upon the appropriate targeting of superparamagnetic iron oxide nanoparticles using a magnetic targeting, an alternative magnetic field is applied for a certain period of time, leading to a local increase in the tissue temperature (42–45 °C), which targets cancer cell death by apoptosis (Kandasamy and Maity 2015). Therefore, hyperthermia therapy can be employed to enhance the efficacy of various cancer treatments.
Magnetite is the mostly used for synthesis of iron oxide magnetic nanoparticles due to its superparamagnetism, which allows rapid nanoparticle magnetization upon the influence of a magnetic field ; however, once this field is turned off, there is no permanent magnetization. In particular, superparamagnetic iron oxide nanoparticles have been employed in cancer therapy and diagnosis by magnetic targeting (Kandasamy and Maity 2015).
In this scenario, the use of magnetic iron oxide nanoparticles with PDT is based on the combination of a chromophore that is a photosensitizer and a phototrigger, and the ability to target the photosensitizer to the desired site of application, with minimum side effects to healthy cells/tissues (Kandasamy and Maity 2015). In this direction, the next section presents and discusses the recent advantages on the design and uses of superparamagnetic iron oxide nanoparticles as nanocarrier of photosensitizers in PDT.
3 Iron Oxide Magnetic Nanoparticles in PDT Applications
Recently, the photosensitizer protoporphyrin IX (PpIX), a metal-free porphyrin, was loaded in magnetoliposomes (MLs), which are comprised by liposomes and Fe3O4 magnetic nanoparticles (Basoglu et al. 2016). PpIX-containing MLs have a hydrodynamic size of 221 nm and displayed phototoxicity against human breast cancer cells (MCF-7). Cell irradiation was performed by using a LED (light-emitting diode) downlight white light (visible light irradiation in the range of 400–700 nm, at 20 W). MCF-7 viability was reduced to 65% upon cell incubation with 350 nM of PpIX-containing MLs under dark condition; however, upon 5 min of light irradiation, a significant cell death was observed at nanoparticle concentration of 250 nM. This result demonstrated the effective phototoxicity of PpIX-loaded magnetoliposomes (MLs) at nanomolar concentrations (Basoglu et al. 2016).
As stated before, near infrared (NIR) is a suitable wavelength range for PDT applications . In this direction, gold nanopopcorns containing self-assembled iron oxide cluster were synthesized for magnetic field targeting in PDT applications (Bhana et al. 2015). The nanoparticle surface was coated with the photosensitizer silicon 2,3-naphthalocyanine dihydroxide, followed by stabilization with polyethylene glycol (PEG) linked with 11-mercaptoundecanoic acid. The hybrid nanomaterial demonstrated superparamagnetic behavior and 61% of photothermal conversion efficiency under NIR irradiation . Upon the application of a gradient magnetic field, the hybrid nanomaterial demonstrated superior release of the photosensitizer and cellular uptake. The nanomaterial showed enhanced ability to carry therapeutic molecules deep into tumor tissue through magnetic manipulation and combat tumors locally by PDT (NIR light irradiation of 0.55 W/cm2) and by photothermal effect (Bhana et al. 2015). NIR and photothermal effect are expected to efficiently eradicate tumors, due to the delivery of high and therapeutic concentrations of photosensitizer-containing magnetic nanocarriers in deep tumors via applying a magnetic field on tumor surface.
The design of hybrid nanocarriers in PDT is a promising strategy. In this context, multifunctional silica-based magnetic nanoparticles were prepared (Chen et al. 2009). The nanoparticles are composed by Fe3O4 magnetic nanoparticles coated with 2,7,12,18-tetramethyl-3,8-di(1-propoxyethyl)-12,17-bis-(3-hydroxypropyl) porphyrin, shorted as PHPP, employed as photosensitizer (encapsulation efficiency of PHPP, 20.8%). Magnetic Fe3O4 nanoparticles and PHPP were incorporated into silica nanoparticles by sol-gel and microemulsion techniques; the final nanoparticles have a spherical shape and a diameter of 20–30 nm. The magnetic nanoparticles demonstrated good compatibility in dark conditions and ability to generate toxic singlet oxygen upon irradiation with λ = 488 nm (argon-ion laser) with energy density of 4.35 J/cm2 during 10 min toward SW480 carcinoma cells (Chen et al. 2009). Therefore, the nanoparticles displayed remarkable antitumor effects under irradiation .
A hybrid nanomaterial composed of reduced graphene oxide (rGO), magnetic iron oxide, and gold nanoparticles was designed. rGO-Fe2O3 @Au core-shell nanoparticle-graphene nanocomposite was prepared for magnetic targeting in cancer treatment via PDT and photothermal synergist effect and bioimaging agent (Chen et al. 2015b). The presence of Fe2O3 is responsible for magnetic field-assisted singlet oxygen generation and chemophotothermal effect direct to the cancer tissue. The hybrid nanomaterial was found to be superparamagnetic at room temperature, demonstrated high capacity to load the chemotherapeutic doxorubicin (DOX, 1.0 mg mg−1), and had considerable photothermal conversion efficiency under 808 nm (NIR) laser irradiation (2 W cm−2). The authors demonstrated that NIR irradiation triggers doxorubicin (DOX) release with an initial burst of the release of the therapeutic molecule. The in vitro cytotoxicity of DOX-rGO-Fe2O3@Au NPs (DOX-loaded hybrid nanomaterial) was evaluated against human cervical cancer cell line (HeLa) upon 5 min irradiation with NIR laser. Cancer cells significantly uptake DOX-containing nanoparticles within 4 h of incubation. Moreover, magnetic field -guided chemophotothermal synergistic therapy might find important applications in cancer treatment (Chen et al. 2015b).
In a similar approach, magnetofluorescence nanoparticles composed of Fe3O4 @SiO2@APTES@glutaryl-PPa (MF NPs) were synthesized (Cheng et al. 2016), where APTES is (3-aminopropyl)triethoxysilane. The obtained nanoparticles have a mean diameter of 50 nm and can be used for PDT and fluorescence imaging in medical applications. The surface of core-shell Fe3O4@SiO2@APTES NPs was functionalized with the photosensitizer chlorine pyropheophorbide-a (PPa) for PDT application. The cytotoxicity of the nanoparticles was evaluated toward HeLa cells, and the results indicated that the nanoparticles were able to quickly permeate the tumor cells due to their lipo-hydro partition coefficient, leading to cell apoptosis and death. Indeed, due to their small size, the nanoparticles were absorbed on the cancer cell membrane, followed by cell internalization via endocytosis vesicle formation by deformation of cell membrane, which led to the dispersion of the nanoparticles into the cytoplasm of HeLa cells. In addition, the nanoparticles demonstrated light-dependent cytotoxicity to the cancer cells (irradiation with visible light for 10 min at dosage of 25 Jcm−2). As expected, reactive oxygen species (ROS ) generated in HeLa cells (Cheng et al. 2016). Hence, these results highlight the promising therapeutic uses of these nanoparticles in PDT treatment with good magnetic targeting to site-specific toxicity.
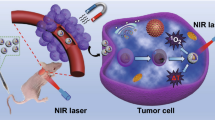
In an interesting paper, iron oxide magnetic nanoparticles (Fe3O4 ) were synthesized and coated with carboxyl-terminated poly(ethylene glycol)-phospholipid to increase nanoparticle dispersion in water (Chu et al. 2013). The phototoxicity of the nanoparticles was evaluated toward esophageal cancer cells upon irradiation with NIR (λ = 808 nm, power density of 0.25 W/cm2 for 20 min) light exposition. Figure 1.1 shows the schematic representation of the light-trigged toxicity of Fe3O4-based nanoparticles toward cancer cell. The application of magnetic nanoparticle and NIR laser irradiation is responsible to decrease esophageal cancer cell viability and to inhibit mouse esophageal tumor growth, leading to tumor reduction (Chu et al. 2013).
Schematic representation of cancer cell death by treating with Fe3O4 -based nanoparticles upon NIR laser light irradiation (Reproduced from reference Chu et al. 2013 with permission from Elsevier)
In a promising strategy, magnetic photosensitive liposomes were synthesized by loading aqueous core iron oxide nanoparticles with lipid bilayer containing therapeutic amounts of photosensitizer payload (Corato et al. 2015). Under laser excitation, the obtained nanoparticles were able to generate toxic singlet oxygen and heat upon alternating magnetic field stimulation, for hyperthermia application. Figure 1.2 shows the schematic representation of the biomedical application of magnetic photosensitive liposome nanoparticles (Corato et al. 2015).
Schematic representation of the treatment of magnetic photosensitive liposome nanoparticles on tumor-bearing mice: (a) therapeutic strategy sketch, liposomes were injected intratumorally, and mice were subsequently subjected to combined treatment with magnetic hyperthermia and laser irradiation . (b) Increased local temperature during magnetic hyperthermia treatment was monitored with an infrared thermocamera. The maximum temperature was reached about 5 min after field application and maintained for the entire treatment cycle (30 min) (Modified from reference Corato et al. 2015 with permission of American Chemical Society)
In a further example, magnetic nanoclusters (MNCs) are composed of Fe3O4 nanoparticles and poly(acrylic acid-co-propargyl acrylate) on the surface for multimodal imaging probes (Daniele et al. 2013). The NRI photosensitizer azide-modified indocyanine green was inserted on the surface of the MNCs. In biological medium, the photosensitizer complexed with bovine serum albumin leading to an extended coating of serum on the MNCs, which induce turn-on of NRI emission for PDT applications (Daniele et al. 2013). Recently, SPIO@SiO2-Re@PEG magnetic nanoparticles for optical probes and PDT sensitizers were obtained and characterized (Galli et al. 2016). Firstly, superparamagnetic iron oxide (SPIO) nanoparticles with an average size distribution of 10 nm were synthesized by thermal decomposition of iron oleate, followed by nanoparticle coating with silica shell by reverse microemulsion technique. Upon pyridine ligand via triethoxysilane moiety, the surface of the nanoparticles was functionalized with luminescent [Re(phen)(CO)3(py)]CF3SO3 complexes anchored to the silica layer. To increase the stability and dispersion of the nanoparticles in physiological conditions, the nanoparticle surface was further covered with PEG layer leading to the formation of SPIO@SiO2-Re@PEG nanoparticles. PEG also increases the nanoparticle circulation in vivo by avoiding nanoparticle uptake and clearance by macrophage. The final nanocomposite had an average size of 40 nm and demonstrated satisfactory efficiency to generate singlet oxygen . The toxicity of the nanoparticles was evaluated toward human lung adenocarcinoma A549 cells. The confocal microscopy demonstrated that after 4 h of cell incubation with the nanoparticles, the latter were efficiently internalized and accumulated in the perinuclear region of the cancer cells. Moreover, increased cytotoxicity was revealed upon irradiation with visible light (by using a 150 W/NDL lamp, 390 nm cut off filters, 142 mW/cm−2). No significant cytotoxicity was observed in the dark condition, indicating the promising uses of this nanoparticle in PDT applications (Galli et al. 2016). Guo et al. (2016) described the preparation of monodisperse Fe3O4 nanoparticles with sizes in the range of 60–310 nm. The authors observed that smaller Fe3O4 nanoparticles displayed enhanced cell internalization and, hence, deeper penetration into multicellular spheroids, which make them suitable for PDT applications. Larger Fe3O4 nanoparticles tended to accumulate in tumors increasing tumor growth inhibition (Guo et al. 2016).
Similarly, multifunctional magnetic nanoparticles with average size of 108 nm were synthesized for tumor treatment and diagnosis (Kim et al. 2016b). The magnetic nanoparticle core (MNP) is composed of Fe3O4 , and the nanoparticle surface was conjugated with hyaluronic acid (AHP), leading to the formation of AHP@MNPs. The cytotoxicity of AHP@MNPs was evaluated toward mouse embryonic fibroblast (NIH3T3) cells, via heat generation properties of the nanoparticles and generation of singlet oxygen , upon magnetic and laser irradiation conditions. The nanoparticle concentration was fixed at 12 g/mL, and NIH3T3 cells were exposed to PDT (4 Jcm−2) and magnetic heat treatment alone or in combination. Cell viability decreased to 30% with PDT treatment. Live/dead staining experiments revealed that the nanoparticles displayed controllable cell death via targeting CD44 receptor-mediated endocytosis (Kim et al. 2016b). Lee et al. (2016) reported the synthesis of caffeic acid-polyethylene glycol-folic acid; FA-PEG-CA, caffeic acid-polyethylene glycol-pheophorbide-a; and pheoA-PEG-CA-coated Fe3O4 nanoparticles for PDT targeting. The presence of caffeic acid on the surface of iron oxide nanoparticles increased the nanoparticle dispersion in aqueous environment, while folate is responsible for mediation of tumor targeting. The cytotoxicity of the nanoparticles was evaluated toward human breast carcinoma cell line (MDA-MB-231). The cell was incubated with the nanoparticles, and light irradiation was performed by using 670 nm laser source (5 mW/cm2) for 200 s. The irradiation increased twofold the cytotoxicity. Furthermore, due to the presence of folate on the surface of the nanoparticle, the nanoparticles were internalized into tumor cells , which over express folic acid receptors (Lee et al. 2016).
In another study, a widely employed photosensitizer in PDT applications, i.e., chlorin e6 (Ce6), was loaded on PEG-functionalized iron oxide nanoclusters (IONCs), leading to the formation of IONC-PEG-Ce6 nanoparticles (Li et al. 2013). The absorbance and excitation peaks of the IONC-PEG-Ce6 were found to be located in the NIR (~700 nm), making the nanoparticles suitable for PDT due to improved tissue penetration. The in vivo efficacy of IONC-PEG-Ce6 was performed based on magnetic tumor targeting by using the 4T1 tumor modal on Balb/c mice. The results revealed a significant delay in tumor growth upon a single nanoparticle injection and the application of a magnetic field -enhanced PDT treatment. The light source for PDT application was 704 nm light at 5 mW/cm2 for 1.5 h (27 J/cm2). Under dark conditions, tumors of mice that received IONC-PEG-Ce6 injection showed the same growth trend compared to the untreated groups. This result suggests that IONC-PEG-Ce6 is not toxic under dark condition. However, significant inhibition of tumor growth was observed upon light irradiation after IONC-PEG-Ce6 injection. Indeed, littler tumor growth was observed over a course of 16 days post-PDT application, revealing the post-effect of the treatment in the combat to cancer . These nanoparticles have desirable properties for cancer treatment, such as no cytotoxicity under dark condition, high generation of singlet oxygen upon NIR illumination, tumor targeting upon application of externa magnetic field, and high cancer cell uptake (Li et al. 2013).
The same photosensitizer , Ce6, was combined with magnetic nanoparticles for PDT (Ling et al. 2014). The authors reported an elegantly pH-dependent PDT to selectively kill cancer cells. Tumor tissues are acidic with pH range of 6.8 which can also reach lower values (5.0–5.5) in endo-/lysosomes. Therefore, the changes in the pH environment from healthy tissues to tumor sites can be used to trigger the release of therapeutic agents on the surface of nanocarriers. In this context, self-assembled extremely small iron oxide nanoparticles (ESIONs) , average size of 3 nm, were prepared and coated with polymeric ligands, leading to the formation of pH-sensitive magnetic nanogrenades (PMNs). PMNs can be activated under low pH values found in tumors for combating resistant heterogeneous tumors in vivo and also as bimodal imaging agent, as represented in Fig. 1.3. According to Fig. 1.3a, the ESIONs were functionalized via catechol-anchored ligand A. Figure 1.3b shows the schematic representation of self-assembly ESIONs into colloidal magnetic core-shell nanomaterial . In this structure, the ESIONs are the hydrophobic core, which is coated with hydrophobic blocks of the tumor-sensing polymeric ligands. The obtained nanoparticles had hydrodynamic diameter of 70 nm, which is suitable for tumor treatments due to the EPR effect. Moreover, the nanoparticle surface allows a pH activation resulting in surface charge reversal in tumor periphery that increases cell adsorption and permeation and endo-/lysosomal pH-dependent theranostic effect of the nanoparticles. Interestingly, the PMN photoactivity (generation of oxygen singlet) was quenched at physiological pH (7.4) due to fluorescence resonance energy transfer. In contrast, at lower pH value found in tumor environment (pH <6), the photoactivity of the PMNs significantly increased due to the disassembly, in a similar manner observed for other self-assembled polymeric ligands. Therefore, pH controls the fluorescence intensity and NIR generation of toxic singlet oxygen . The cytotoxicity of PMNs was demonstrated toward human colorectal carcinoma (HCT116) cells under irradiation and compared to dark conditions. As expected, PMNs had no toxicity in the dark and significant toxicity under irradiation. In vivo studies were also performed by using HCT116 tumor-bearing mice injected with PMNs, followed by irradiation. A significant tumor regression of treated groups was observed, in comparison with control groups. The nanomaterial was designed to be toxic only at the tumor site, since the photosensitizer on the nanoparticle can be self-quenched in the normal tissues, until it reaches the target tumor site. In the tumor, the low pH value suppresses the self-quenched effect, particularly, the intracellular pH stimulus, resulting to a high specific toxic effect to the target region. One week post-PMN injection, the tumors were completely destroyed, and only a remaining scar tissue was observed in the animals (Ling et al. 2014). Taken together, these results demonstrated the efficacy of tumor-targeting iron oxide nanoparticles for PDT and tumor diagnosis.
Schematic representation of the design and mechanism of pH-sensitive magnetic nanogrenades (PMNs) for tumor pH activation: (a) Schematic representation of pH-responsive, ligand-assisted self-assembly of extremely small iron oxide nanoparticles (ESIONs), (b) schematic representation of tumor pH-recognizable treatment strategy using PMNs (Reproduced from reference Ling et al. 2014 with permission from American Chemical Society)
In a similar interesting strategy, hydrophilic chlorin-conjugated magnetic nanoparticles were designed for PDT in the combat of melanoma (Mbakidi et al. 2013).The nanomaterial is comprised of an iron oxide magnetic core covered with water-stable and biocompatible dextran shell bearing polyaminated chlorin p6 (the photosensitizer ). The toxicity of the nanomaterial was assayed toward variants of B16 mouse melanoma cell line (B16F10 and B16G4F, with and without melanin, respectively). The in vitro results demonstrated that the nanoparticles had no cytotoxicity in the dark between 0.1 and 1 μM, while 1 μM of the nanoparticles had strong phototoxicity toward B16F10 cell line (Mbakidi et al. 2013).
Nam et al. (2016) reported the PDT activity of hematoporphyrin-conjugated Fe3O4 nanoparticles. The Fe3O4 nanoparticles were conjugated with hematoporphyrin (HP) leading to the formation of Fe3O4@HPs. The phototoxicity of the Fe3O4@HPs was evaluated toward human prostate cancer (PC-3) and breast cancer (MDA-MB-231) cell lines. The authors used a LED, with an electrical power of 3 W at 505 nm maximum wavelength and a power density of up to 7 mW/cm2. A significant phototoxicity of Fe3O4@HPs was found toward both cancer cell lines, which was dependent on the amount of HP on the nanoparticle surface. In addition, the results demonstrated a cell membrane translocation and nuclear fragmentation of cancer cells due to apoptosis (Nam et al. 2016).
The photosensitizer pheophorbide-a (pheoA), which produces fluorescent emission in the range of 660–670 nm, was conjugated with iron oxide nanoparticles for PDT and magnetic resonance imaging (Nafiujjaman et al. 2015). The synthesis of the nanohybrid material was performed by the conjugation of pheoA with heparin (pheoA-Hep), which was further bound with APTES-coated Fe3O4 nanoparticles. The final material, spherical pheoA-Hep-Fe3O4 nanoparticles (average hydrodynamic size of 90 nm), had improved biocompatibility and can easily penetrate the cell surface via ERP effect. The phototoxicity of pheoA-Hep-Fe3O4 nanoparticles was demonstrated toward epithelial cancer (KB) cells, at nanoparticle concentration of 50 μg mL−1 and 24 h of incubation. The irradiation was performed by using a laser source 670 nm (4 mW/cm−2) for 10 min. The results showed that pheoA-Hep-Fe3O4 nanoparticles caused 80% cell death , under irradiation, while in the dark, no toxicity was observed. Moreover, a high degree of nanoparticle internalization was reported (Nafiujjaman et al. 2015).
Oleic acid (OA) -coated magnetic iron oxide nanoparticles were synthesized by coprecipitation technique, followed by addition of Mn2+-doped NaYF4:Yb/Er luminescent shell (Qin et al. 2016). The obtained monodispersed Fe3O4 @Mn2+-doped NaYF4Yb/Er core-shell nanoparticles were able to emit luminescence under NIR excitation indicating their potential uses for PDT (Qin et al. 2016). Similarly, core-shell nanoparticles (size of 99 nm) composed by magnetite/silica/titania were obtained by sol-gel technique (Sakr et al. 2016). The photosensitizer ruthenium polypyridyl dye was added to the surface of the synthesized nanoparticles. The cytotoxicity of the nanoparticles was demonstrated toward lung cancer cells (A549) under a laser source at 532 nm (5 mW/cm2). Indeed, upon irradiation , the ROS generation increased fivefold compared to bare NPs, which caused cell death (the half maximal inhibitory concentration, IC50, was found to be 3 μg/mL1). The mechanisms of cell death are under investigation (Sakr et al. 2016).
The photosensitizer porphyrin was added on the surface of superparamagnetic iron oxide nanoparticles (SPION-TPP) through click chemistry (Thandu et al. 2014). Phototoxicity of the obtained nanomaterial was demonstrated toward murine amelanotic melanoma B78-H1 cells, upon cell irradiation at NIR region (14 Jcm−2, 30 min). Cell internalization of the nanoparticles was improved by the conjugation of the nanoparticles with TAT peptide (a cell-penetrating peptide) (Thandu et al. 2014). Unterweger et al. (2015) reported the synthesis of hypericin-linked-containing dextran coating on the surface of superparamagnetic iron oxide nanoparticles with 55–85 nm of hydrodynamic size. Dextran was used as stabilizing agent for the nanoparticles, and hypericin is a PS. The phototoxicity of the obtained nanoparticles was demonstrated toward human T-cell leukemia cells (Jurkat) upon white irradiation (40 Wm−2) up to 15 min. The results showed a time-dependent and concentration-dependent cytotoxicity due to ROS generation (Unterweger et al. 2015).
A versatile nanomaterial was synthesized for multifunctional anticancer treatment and diagnosis (Wan et al. 2015). The nanomaterial, Fe3O4 -NS-C3N4@mSiO2-PEG-RGD, is composed of C3N4 (PS, a graphitic carbon nitride), mSiO2 (mesoporous silica to enhance the stability of the nanomaterial and the ability of drug loading), and RGD (integrin-binding cell adhesive peptide, which is a tumor biomarker). The versatile nanomaterial allied PDT and low pH-triggered anticancer properties. The phototoxicity of the nanomaterial was evaluated toward A549 and HeLa cancer cells, upon visible light irradiation (450 nm, 40 mW/cm−2 for 10 min). Figure 1.4 shows images, obtained by confocal laser scanning microscopy, of the cells after incubation with the nanomaterial and PDT treatment, compared with control groups. As can be observed, a significant green fluorescence was emitted from the cells that were irradiated, in comparison with a less intensive green fluorescence light emission from the cells in the dark (no irradiated). This result illustrates the ability of the nanoparticles to generate ROS under irradiation with visible light. Interestingly, the confined beam of light source employed in this experiment caused a desired site-targeted cytotoxic effect on the treated cells, which might be able to decrease potential side effects toward noncancer cells (Fig. 1.4) (Wan et al. 2015).
Detection of intracellular ROS in A549 cancer cells treated with Fe3O4 -NS-C3N4@mSiO2-PEG-RGD either (c) under visible light irradiation or (a) not; (e) site-targeted PDT. Parts b, d, and f correspond to the optical images of a, c, and e (Reproduced from reference Wan et al. 2015 with permission from American Chemical Society)
Core-shell nanomaterial was obtained by coating hollow magnetic nanospheres (HMNSs) with silica (SiO2) shells followed by conjugation with carboxylated graphene quantum dots (GQDs) leading to HMNS/SiO2/GQDs (Wo et al. 2016). The anticancer drug DOX was added to the nanomaterial, which was further stabilized with liposomes. The phototoxicity of the multimodal nanoparticle was proved toward human esophageal squamous carcinoma (Eca-109) cells upon NIR laser irradiation (671 nm or 808 nm for 20 min). The authors demonstrated that liposome-stabilized nanomaterial was adsorbed by the tested cancer cells, which led to membrane and nuclei damages. As expected, by DOX loading on the nanoparticle, the cytotoxicity toward cancer cells was significantly increased (Wo et al. 2016).
Other multifunctional iron oxide-based nanoparticles were synthesized and applied in PDT. Firstly, Fe3O4 @NaYF4:Yb/Er core-shell nanomaterial was synthesized, followed by addition of tetrasulfonic phthalocyanine aluminum (AIPcS4), as the photosensitizer and PEG coating (Zeng et al. 2013). The phototoxicity of the nanomaterial was shown toward MCF-7 cells, upon irradiation with 980 nm laser source (20 mW/cm2) for 3 min. The authors reported a decrease of 70% of cancer cell viability upon this treatment. Moreover, the nanoparticles were found to accumulate on the MCF-7 surfaces. The toxicity to cancer cells was attributed to the ability of AIPcS4 to generate singlet oxygen (Zeng et al. 2013).
The nanocomposite Fe3O4 @NaYF4:Yb-E conjugated with folic acid (FA) was synthesized and applied as PDT agent (under NIR irradiation ) toward in vitro and in vivo (MCF-7 tumor-bearing nude mice) evaluations (Zeng et al. 2015). In vitro studies demonstrated that the viabilities of HeLa and MCF-7 cells decreased to 18% and 31%, upon incubation with the nanocomposite and 980 nm laser irradiation. Moreover, in vivo studies revealed 95% of MCF-7 tumors in bearing nude mice, indicating the promising application of this nanomaterial to combat cancer (Zeng et al. 2015). A DNA damage caused by Fe3O4 nanoparticles in PDT application was reported (Zhang and Chai 2012). Magnetite-silica core-shell nanomaterial was synthesized by sol-gel technique to promote DNA damage by a photoactive platinum-diimine complex under red light (Zhang and Chai 2012).
Zhao et al. (2014) reported the incorporation of the photosensitizer methylene blue (MB) into folate-conjugated Fe3O4 /mesoporous silica core-shell nanoparticles. The toxicity of the nanoparticles was demonstrated toward different cell lines: HeLa cells, mouse fibroblast cells (NIH3T3 cells), mouse sarcoma cells (S-180 cells), and human ovarian cancer cells (SK-OV-3 cells). Folic acid (FA) was used to target the nanoparticles to the cancer cells, since cancer cells are known to overexpress folate receptors. The cell irradiation was performed by using a 650 nm laser beam (70 mW/cm2 for 4 min). The results demonstrated a significant decrease in cell viability (reduction of 80% of viable cells compared to control group) by incubating SK-OV-3 cells with 200 μg/mL1 of the nanoparticle. Moreover, the nanoparticles were found to internalize to cancer cells. In vivo experiments were performed with S-180 tumor-bearing mice treated with the nanoparticles and laser irradiation at 650 nm. The results demonstrated the potential anticancer activity of the nanoparticles by suppressing tumor growth (Zhao et al. 2014).
Finally, the photosensitizer indocyanine green (IR820) was conjugated with chitosan quaternary ammonium (CSQ) magnetic iron oxide nanoparticles, leading to the formation of IR820-CSQ-Fe nanoparticles (Zhou et al. 2016). The phototoxicity of the nanoparticles (808 laser source, 8 Wcm−2, 7 min) was demonstrated with breast cancer cell line (MDA-MB-231 cells) (Zhou et al. 2016). Taking together, several important and recent publications described successfully the synthesis of magnetic iron oxide-based nanoparticles as targeting nanocarriers in PDT to combat cancer.
4 Conclusions
The recent advantages in the design of iron oxide magnetic nanoparticles as nanocarriers of photosensitizers are able to generate therapeutic amounts of singlet oxygen directly in the target site of application. The targeting therapy can be achieved upon the application of an external magnetic field due to the superparamagnetic grapheme of iron oxide nanoparticles. It is clear from the reviewed literature that there is a great interest on the preparation of hybrid nanomaterials with multifunctions (e.g., cancer treatment and cancer diagnosis).
It should be noted that although tremendous progress has been made in this promising field, still more studies are required to translate the research to the clinical settings. In this direction, the ideal nanocarrier needs to meet the following requirements: (i) biocompatibility, (ii) biodegradability, (iii) small size and high loading capacity of the photosensitizer , (iv) minimum side effects, (v) prolonged body circulation with minimum tendency to aggregation, (vi) enhanced ERP effect, and (vii) ability to generate therapeutic amounts of singlet oxygen directed to the desired site and no dark toxicity.
Although PDT has been used in oncology for several years, some challenges need to be overcome, for instance, (i) minimization of systemic toxicity, (ii) adequate generation and permeation of singlet oxygen , and (iii) no dark toxicity.
Finally, it can be concluded that the combination of magnetic iron oxide nanoparticles as nanocarriers of photosensitizers in PDT is a promising field in cancer treatment. However, more studies are necessary in this area of nanomedicine.
Abbreviations
- 1O2 :
-
Singlet oxygen
- 3O2 :
-
Triplet oxygen
- AHP:
-
Hyaluronic acid
- AIPcS4:
-
Tetrasulfonic phthalocyanine aluminum
- Ce6:
-
Chlorin e6
- CSQ:
-
Chitosan quaternary ammonium
- DOX:
-
Doxorubicin
- Eca-109:
-
Esophageal squamous carcinoma
- EPR:
-
Enhanced permeability and retention
- ESIONs:
-
Extremely small iron oxide nanoparticles
- FDA:
-
Food and Drug Administration
- Fe3O4 :
-
Magnetite
- HeLa:
-
Human cervical cancer cell line
- HMNSs:
-
Hollow magnetic nanospheres
- HP:
-
Hematoporphyrin
- IC50 :
-
Maximal inhibitory concentration
- IONCs:
-
Iron oxide nanoclusters
- IR820:
-
Indocyanine green
- Jurkat:
-
Human T-cell leukemia cells
- LED:
-
Light-emitting diode
- MCF-7:
-
Human breast cancer cells
- MDA-MB-231:
-
Breast cancer
- MLs:
-
Magnetoliposomes
- MNCs:
-
Magnetic nanoclusters
- mSiO2 :
-
Mesoporous silica
- NIH3T3:
-
Mouse embryonic fibroblast
- NRI:
-
Near infrared
- OA:
-
Oleic acid
- PC-3:
-
Human prostate cancer
- PDT:
-
Photodynamic therapy
- PEG:
-
Polyethylene glycol
- pheoA:
-
Pheophorbide A
- PHPP:
-
2,7,12,18-Tetramethyl-3,8-di(1-propoxyethyl)-12,17-bis-(3-hydroxypropyl) porphyrin
- PMNs:
-
Magnetic nanogrenades
- PpIX:
-
Protoporphyrin IX
- PS:
-
Photosensitizer
- RGD:
-
Integrin-binding cell adhesive peptide
- rGO:
-
Reduced graphene oxide
- ROS :
-
Reactive oxygen species
- S-180:
-
Sarcoma cells
- SK-OV-3:
-
Ovarian cancer cells
- SPIO:
-
Superparamagnetic iron oxide
References
Allison RR, Mota HC, Bagnato VS, Sibata CH. Bio-nanotechnology and photodynamic therapy—–State of the art review. Photodiagn Photodyn Ther. 2008;5:19–28.
Banerjee SM, MacRobert AJ, Mosse CA, Periera B, Bown SG, Keshtgar MRS. Photodynamic therapy: inception to application in breast cancer. Breast. 2017;31:105–13.
Basoglu H, Bilgin MD, Demir MM. Protoporphyrin IX-loaded magnetoliposomes as a potential drug delivery system for photodynamic therapy: fabrication, characterization and in vitro study. Photodiagn Photodyn Ther. 2016;13:81–90.
Bechet D, Couleaud P, Frochot C, Viriot ML, Guillemin F, Barberi-Heyob M. Nanoparticles as vehicles for delivery of photodynamic therapy agents. Trends Biotechnol. 2008;26:612–21.
Bhana S, Lin G, Wang L, Starring H, Mishra SR, Liu G, Huang X. Near-infrared-absorbing gold nanopopcorns with iron oxide cluster core for magnetically amplified photothermal and photodynamic cancer therapy. ACS Appl Mater Interfaces. 2015;7:11637–47.
Bhattacharyya S, Kudgus RA, Bhattacharya R, Mukherjee P. Inorganic nanoparticles in cancer therapy. Pharm Res. 2011;28:237–59.
Chatterjee DV, Fong LS, Zhang Y. Nanoparticles in photodynamic therapy: an emerging paradigm. Adv Drug Deliv Rev. 2008;60:1627–3.
Chen ZL, Sun Y, Huang P, Yang XX, Zhou XP. Studies on preparation of photosensitizer loaded magnetic silica nanoparticles and their anti-tumor effects for targeting photodynamic therapy. Nanoscale Res Lett. 2009;4:400–8.
Chen G, Agren H, Ohulchanskyy TY, Prasad PN. Light upconverting core–shell nanostructures: nanophotonic control for emerging applications. Chem Soc Rev. 2015a;44:1680–713.
Chen H, Liu F, Lei Z, Ma L, Wang Z. Fe2O3@Au core@shell nanoparticle–graphene nanocomposites as theranostic agents for bioimaging and chemo-photothermal synergistic therapy. RSC Adv. 2015b;5:84980–7.
Cheng J, Tan G, Li W, Li J, Wang Z, Jin Y. Preparation, characterization and in vitro photodynamic therapy of a pyropheophorbide-a-conjugated Fe3O4 multifunctional magnetofluorescence photosensitizer. RSC Adv. 2016;6:37610–20.
Chu M, Shao Y, Peng J, Dai X, Li H, Wu Q, Shi D. Near-infrared laser light mediated cancer therapy by photothermal effect of Fe3O4 magnetic nanoparticles. Biomaterials. 2013;34:4078–88.
Corato DR, Béalle G, Kolosnjaj-Tabi J, Espinosa A, Clément O, Silva AK, Ménager C, Wilhelm C. Combining magnetic hyperthermia and photodynamic therapy for tumor ablation with photoresponsive magnetic liposomes. ACS Nano. 2015;9:2904–16.
Daniele MA, Shaughnessy ML, Roeder R, Childress A, Bandera YP, Foulger S. Magnetic nanoclusters exhibiting protein-activated near-infrared fluorescence. ACS Nano. 2013;7:203–13.
Galli M, Moschini E, Dozzi MV, Arosio P, Panigati M, D’Alfonso L, D’Alfonso L, Mantecca P, Lascialfari A, D’Alfonso G, Maggioni D. SPIO@SiO2–Re@PEG nanoparticles as magneto-optical dual probes and sensitizers for photodynamic therapy. RSC Adv. 2016;6:38521–32.
Gangopadhyay M, Mukhopadhyay SK, Karthik S, Barmana S, Pradeep Singh ND. Targeted photoresponsive TiO2–coumarin nanoconjugate for efficient combination therapy in MDA-MB-231 breast cancer cells: synergic effect of photodynamic therapy (PDT) and anticancer drug chlorambucil. Med Chem Commun. 2015;6:769–77.
Guo X, Wu Z, Li W, Wang Z, Li Q, Kong F, Zhang H, Zhu X, Du YP, Jin Y, Du Y, You J. Appropriate size of magnetic nanoparticles for various bioapplications in cancer diagnostics and therapy. ACS Appl Mater Interfaces. 2016;8:3092–106.
Huang Y, He S, Cao W, Cai K, Liang X-J. Biomedical nanomaterials for imaging-guided cancer therapy. Nanoscale. 2012;4:6135–49.
Kandasamy G, Maity D. Recent advances in superparamagnetic iron oxide nanoparticles (SPIONs) for in vitro and in vivo cancer nanotheranostics. Int J Pharm. 2015;496:191–218.
Kelkar SS, Reineke TM. Theranostics: combining imaging and therapy. Bioconjug Chem. 2011;22:1879–903.
Kim H, Chung K, Lee S, Kim DH, Lee H. Near-infrared light-responsive nanomaterials for cancer theranostics. WIREs Nanomedicine Nanobiotechnol. 2016a;8:23–45.
Kim KS, Kim J, Lee JY, Matsuda S, Hideshima S, Mori Y, Osaka T, Na K. Stimuli-responsive magnetic nanoparticles for tumor-targeted bimodal imaging and photodynamic/hyperthermia combination therapy. Nanoscale. 2016b;8:11625–34.
Lee J, Kim KS, Na K. Caffeic acid-coated multifunctional magnetic nanoparticles for the treatment and bimodal imaging of tumours. J Photochem Photobiol B. 2016;160:210–6.
Lee HH, Choi MG, Hasan T. Application of photodynamic therapy in gastrointestinal disorders: an outdated or re-emerging technique? Korean J Intern Med. 2017;32:1–10.
Li Z, Wang C, Cheng L, Gong H, Yin S, Gong Q, Yonggang L, Zhuang L. PEG-functionalized iron oxide nanoclusters loaded with chlorin e6 for targeted, NIR light induced, photodynamic therapy. Biomaterials. 2013;34:9160–70.
Ling D, Park W, Park SJ, Lu Y, Kim KS, Hackett MJ, Kim BH, Yim H, Jeon YS, Na K, Hyeon T. Multifunctional tumor pH-sensitive self-assembled nanoparticles for bimodal imaging and treatment of resistant heterogeneous tumors. J Am Chem Soc. 2014;136:5647–5.
Mbakidi JP, Drogat N, Granet R, Ouk TS, Ratinaud MH, Rivière E, Verdier M, Sol V. Hydrophilic chlorin-conjugated magnetic nanoparticles-potential anticancer agent for the treatment of melanoma by PDT. Bioorg Med Chem Lett. 2013;23:2486–90.
Nafiujjaman M, Revuri V, Nurunnabi M, Cho KJ, Lee YK. Photosensitizer conjugated iron oxide nanoparticles for simultaneous in vitro magneto-fluorescent imaging guided photodynamic therapy. Chem Commun. 2015;51:5687–90.
Nam KC, Choi KH, Lee KD, Kim JH, Jung JS, Park BJ. Particle size dependent photodynamic anticancer activity of hematoporphyrin-conjugated Fe3O4 particles. J Nanomater. 2016;2016:1278393.
Paszko E, Ehrhardt C, Senge MO, Kelleher DP, Reynolds JV. Nanodrug applications in photodynamic therapy. Photodiagn Photodyn Ther. 2011;8:14–29.
Qin Z, Du S, Luo Y, Liao Z, Zuo F, Luo J. Hydrothermal synthesis of superparamagnetic and red luminescent bifunctional Fe3O4@Mn2+-doped NaYF4:Yb/Er core@shell monodisperse nanoparticles and their subsequent ligand exchange in water. Appl Surf Sci. 2016;378:174–80.
Sakr MH, Halabi MN, Kalash LN, Al-Ghadban SI, Rammah MK, Sabban MEE, Bouhadir KH, Ghaddar TH. Synthesis and in vitro cytotoxicity evaluation of ruthenium polypyridyl-sensitized paramagnetic titania nanoparticles for photodynamic therapy. RSC Adv. 2016;6:47520–9.
Seabra AB, Duran N. Nanotoxicology of metal oxide nanoparticles. Metals. 2015;5:934–75.
Seabra AB, Haddad PS, Duran N. Biogenic synthesis of nanostructured iron compounds: applications and perspectives. IET Nanobiotechnol. 2013;7:90–9.
Seabra AB, Pasquôto T, Ferrarini AC, Santos Mda C, Haddad PS, de Lima R. Preparation, characterization, cytotoxicity, and genotoxicity evaluations of thiolated- and S-nitrosated superparamagnetic iron oxide nanoparticles: implications for cancer treatment. Chem Res Toxicol. 2014;27:1207–18.
Smith BE, Roder PB, Hanson JL, Manandhar S, Devaraj A, Perea DE. Singlet-oxygen generation from individual semiconducting and metallic nanostructures during near-infrared laser trapping. ACS Photon. 2015;2(4):559–64.
Thandu M, Rapozzi V, Xodo L, Albericio F, Comuzzi C, Cavalli S. “Clicking” porphyrins to magnetic nanoparticles for photodynamic therapy. Chem Plus Chem. 2014;79:90–8.
Unterweger H, Subatzus D, Tietze R, Janko C, Poettler M, Stiegelschmitt A, Schuster M, Maake C, Boccaccini AR, Alexiou C. Hypericin-bearing magnetic iron oxide nanoparticles for selective drug delivery in photodynamic therapy. Int J Nanomedicine. 2015;10:6985–96.
Wan H, Zhang Y, Zhang W, Zou H. Robust two-photon visualized nanocarrier with dual targeting ability for controlled chemo-photodynamic synergistic treatment of cancer. ACS Appl Mater Interfaces. 2015;7:9608–18.
Wang S, Gao R, Zhou F, Selke M. Nanomaterials and singlet oxygen photosensitizers: potential applications in photodynamic therapy. J Mater Chem. 2004;14:487–93.
Wo F, Xu R, Shao Y, Zhang Z, Chu M, Shi D, Liu S. A multimodal system with synergistic effects of magneto-mechanical, photothermal, photodynamic and chemo therapies of cancer in Grapheme-quantum dot-coated hollow magnetic nanospheres. Theranostics. 2016;6:485–500.
Zeng L, Xiang L, Ren W, Zheng J, Li T, Chen B. Multifunctional photosensitizer-conjugated core–shell Fe3O4@NaYF4:Yb/Er nanocomplexes and their applications in T2-weighted magnetic resonance/upconversion luminescence imaging and photodynamic therapy of cancer cells. RSC Adv. 2013;3:13915–25.
Zeng L, Luo L, Pan Y, Luo S, Lu G, Wu A. In vivo targeted magnetic resonance imaging and visualized photodynamic therapy in deep-tissue cancers using folic acid-functionalized superparamagnetic-upconversion nanocomposites. Nanoscale. 2015;7:8946–54.
Zhang Z, Chai A. Core-shell magnetite-silica composite nanoparticles enhancing DNA damage induced by a photoactive platinum-diimine complex in red light. J Inorg Biochem. 2012;117:71–6.
Zhao X, Chen Z, Zhao H, Zhang D, Tao L, Lan M. Multifunctional magnetic nanoparticles for simultaneous cancer near-infrared imaging and targeting photodynamic therapy. RSC Adv. 2014;4:62153–9.
Zhou H, Hou X, Liu Y, Zhao T, Shang Q, Tang J, Liu J, Wang Y, Wu Q, Luo Z, Wang H, Chen C. Superstable magnetic nanoparticles in conjugation with near-infrared dye as a multimodal theranostic platform. ACS Appl Mater Interfaces. 2016;8:4424–33.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Seabra, A.B. (2017). Iron Oxide Magnetic Nanoparticles in Photodynamic Therapy: A Promising Approach Against Tumor Cells. In: Rai, Ph.D, M., Shegokar, Ph.D, R. (eds) Metal Nanoparticles in Pharma. Springer, Cham. https://doi.org/10.1007/978-3-319-63790-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-63790-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63789-1
Online ISBN: 978-3-319-63790-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)