Abstract
Although recent decades have seen proliferation of tension-free mesh techniques, the tissue-based inguinal hernia repair remains a critical element of every general surgeon’s arsenal. Proficiency in tissue-based repair is crucial in circumstances where synthetic mesh placement is contraindicated, undesirable, or unavailable. In this chapter, we describe the indications and techniques for performing the four modern tissue-based repairs: Bassini, Shouldice, McVay, and Desarda procedures. With appropriate patient selection, sound understanding of inguinal anatomy, and meticulous attention to operative technique, these repairs can achieve favorable outcomes.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Placement of mesh is now favored in both open and laparoscopic repairs of uncomplicated adult hernias. Techniques that rely on tissue-based repair are typically reserved for exceptional circumstances due to an elevated risk of recurrence. Impaired collagen synthesis has been shown to contribute to hernia formation, and the tissues in the presence of a hernia may be regarded as intrinsically abnormal. Suture lines secure tissue under tension which is known to be associated with recurrence. Synthetic mesh materials have been developed to be strong, lightweight, and inert. Mesh-based repairs have been demonstrated in several randomized controlled trials to carry lower rates of recurrence [1,2,3]. Nevertheless, tissue-based repairs are preferred in certain circumstances where mesh usage is contraindicated, undesirable, or unavailable. In the setting of contamination or infection, implantation of synthetic material is contraindicated. Consideration of mesh-related pain and complications is important and should factor into the shared patient and surgeon decision regarding repair technique. Adolescents and young adults as well as female patients with small indirect hernias may also be better suited for a tissue-based repair when chronic pain and foreign body sensation are taken into account. In underserved settings, where inguinal hernias are more likely to present with strangulation or mesh may simply not be immediately available, tissue-based repair remains the standard of care.
The surgical literature includes references to more than 70 different tissue-based repairs. The most common techniques in modern use include the Bassini, Shouldice, McVay, and Desarda repairs. The latest data from the national hernia registry in Sweden indicated that tissue repairs were used in 0.8% of inguinal operations in 2015 [4]. In this chapter, we will describe these procedures with an emphasis on the details of neuroanatomy and intraoperative technique.
Preoperative Considerations
Preoperative considerations for tissue-based repairs are similar to standard inguinal hernia repairs. Patients presenting with an inguinal hernia regardless of symptoms are appropriate for operative repair barring medical contraindications. Those with elevated cardiac or pulmonary risk can be considered for feasibility of repair under local anesthesia with or without sedation. Patient with prohibitive medical risk may be offered expectant management with the use of a truss for comfort unless severity of symptoms, incarceration, or strangulation necessitate an urgent nonelective operation. The most relevant preoperative consideration is whether the patient is indeed an appropriate candidate for tissue-based repair. Larger hernias and patients with intrinsic hernia-related risk factors should, in general, undergo mesh repair. Since mesh repairs are associated with lower rates of recurrence and pain, prosthetic repairs are generally favored unless contraindicated. Smaller hernias in a patient without increased hernia-related risk factors, adolescents or young adults with a likely small indirect hernia, female patients with a small hernia, and patients that have an aversion or contraindication to mesh should be considered for a tissue repair. Potential contamination of the operative field and prosthetic due to necrotic bowel, active infection, strangulation, or sepsis are considered indications for tissue-based repair. In resource-limited settings where mesh and training in mesh-based techniques are not readily available, tissue repairs remain the standard treatment option for the burden of inguinal hernia disease.
Patient Positioning and Theater Setup
The patient is placed in the supine position. In most cases, tissue-based repair can be performed under local anesthesia alone. Our preferred technique of infiltration of a mixture of a short- and long-acting local anesthetic into the intradermal, subdermal, deep dermal, and subaponeurotic spaces has been described in detail for Lichtenstein repairs—the same technique works well for inguinal tissue-based repairs [5].
Incision and Access
Each inguinal tissue-based repair begins with a 5–6 cm incision along the Langer line extending laterally from the pubic tubercle. The external oblique aponeurosis is incised sharply with care to preserve the ilioinguinal nerve. On the medial side, the avascular plane between the external and internal oblique aponeuroses is bluntly dissected to reveal and preserve the iliohypogastric nerve. The genital nerve is identified along the lateral aspect of the cord at the lateral crus of the internal ring running parallel and adjacent to the external spermatic vein within the cremasteric bundle. The spermatic cord and hernia sac are each identified and isolated. A direct defect is identified along the floor of the canal medial to the inferior epigastric vessels. The femoral canal may be explored either through the hernia sac in the case of an indirect hernia or through the opened transversalis fascia with a direct hernia.
Operative Steps
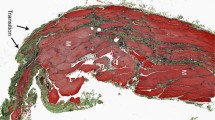
Bassini Repair
The Bassini repair involves extensive dissection of the spermatic cord with high ligation of the hernia sac and inguinal floor reconstruction. Once the spermatic cord dissection is completed and indirect hernia sac excised, the inguinal floor is exposed. In a proper Bassini repair, the transversalis fascia is then incised from pubic tubercle to the internal inguinal ring, although this step is often excluded from modern adaptations of the Bassini repair. A triple-layer tissue repair is then performed with fixation of the transversalis fascia, transversus abdominis, and internal oblique aponeurosis to the shelving edge of the inguinal ligament with six to eight nonabsorbable interrupted sutures (see Fig. 14.1). A relaxing incision may be made along the falx inguinalis if required to minimize tension [6].
Bassini repair. (Reproduced from [7])
The transversalis fascia is opened widely to permit a complete three-layer closure. Medially, the sutures catch the falx inguinalis and transversalis fascia. Laterally, the sutures catch the transversalis fascia and the shelving edge of the inguinal ligament:
-
1.
Aponeurosis of the external oblique
-
2.
Internal oblique
-
3.
Inguinal ligament
-
4.
Relaxing incision of the falx inguinalis
-
5.
Transversalis fascia
-
6.
Repair with nonabsorbable suture
-
7.
Subperitoneal fat
-
8.
Closure of the external oblique aponeurosis anterior to the conjoint tendon
Shouldice Repair
In the Shouldice repair , the surgeon similarly divides the transversalis fascia between the pubic tubercle and internal ring. Medial and lateral fascial flaps are then mobilized by bluntly dissecting the underlying preperitoneal tissue. The layers are then reapproximated using a running, nonabsorbable monofilament suture from the lateral edge of the rectus sheath to the iliopubic tract starting at the pubic tubercle. At the internal ring, this suture includes the lateral cremaster remnant and reverses back toward the pubic tubercle. The medial transversalis fascia flap is approximated to the shelving edge of the inguinal ligament. The suture is tied down at the pubic tubercle. A new running stitch starts at the internal ring and approximates the conjoint tendon to the inguinal ligament (Fig. 14.2c). At the tubercle, the stitch again reverses to progress laterally through the same structures and the lower end of the external oblique aponeurosis until it is tied down at the internal ring (Fig. 14.2d). The external oblique aponeurosis is then closed. An additional feature of the Shouldice repair is the routine division of the genital branch of the genitofemoral nerve during cord dissection.
Shouldice repair. (Reproduced from [8])
McVay Repair
The McVay repair is primarily notable for addressing both the inguinal and femoral defects. Once isolation of the spermatic cord is achieved, the transversalis fascia is opened to access the preperitoneal space. Cooper’s ligament is then exposed using gentle blunt dissection. A relaxing incision is then made in the anterior rectus sheath at the pubic tubercle (Fig. 14.3a). The medial flap of the transversalis fascia is sutured to Cooper’s ligament and runs laterally to occlude the femoral ring. A transition stitch approximates the transversalis fascia to the femoral sheath and inguinal ligament lateral to the femoral ring. A relaxing incision of the ipsilateral anterior rectus sheath reduces tension on the reapproximated external oblique aponeurosis and is considered a critical step of the McVay repair (Fig. 14.3d).
McVay repair. (Reproduced from [7])
Desarda Repair
The Desarda repair , a modern variant of the historic Halstead repair, entails reinforcement of the inguinal floor with a laterally based pedicled strip of external oblique aponeurosis [8]. An undetached portion of external oblique aponeurosis is mobilized to the posterior wall of the inguinal canal with interrupted stitches securing it to the internal oblique muscle superiorly and inguinal ligament inferiorly (Fig. 14.4).
Desarda repair (Reproduced from [9]). (1) internal oblique aponeurosis; (2) upper strip of the medial leaf of external oblique aponeurosis sutured to internal oblique aponeurosis; (3) medial leaf of external oblique aponeurosis that is sutured to inguinal ligament
Closure
Each of these tissue repairs is completed with restoration of the spermatic cord to its anatomic position followed by reapproximation of the external oblique aponeurosis. Scarpa’s fascia and the skin can then be closed with running or interrupted sutures according to the surgeon’s preference. Drain placement is not typically required or advised.
Postoperative Management
Postoperative management following tissue repair is similar to open mesh-based techniques. If tissue repair was selected in patients with infection, strangulated bowel, or other complicating factors, patients are typically observed in the hospital to assure appropriate return of bowel function and resolution of infection. In elective tissue-based repairs, patients may be discharged from the ambulatory setting once they have recovered from anesthesia. Postoperative activity is typically restricted for 3–4 weeks given that the strength of the repair is based upon tissue scarring and wound healing properties rather than mesh strength. In the longer term, surgeon-driven follow-up regarding recurrence and chronic pain is encouraged to help define the appropriate role for tissue repair and allow for tailoring of ideal technique for different patient cohorts.
Tips and Pitfalls
Nerve identification : As with all open anterior repairs, identification of nerves is crucial to minimize the risk of chronic pain. Since each tissue-based repair includes placement of numerous sutures, care must be taken to avoid nerve entrapment. Rarely, pragmatic nerve ligation may be considered if injury to one of the nerves is recognized intraoperatively or if the course of the nerve predisposes it to injury. In these cases, resection of the inguinal segment of the nerve with proximal intramuscular reimplantation of the upstream segment into the internal oblique is recommended. Prophylactic neurectomy of the inguinal nerves is not typically recommended as it may lead to unnecessary sensory disturbance and the rates of chronic pain are not decreased versus a “nerve-mindfulness” approach.
Inspection for femoral hernia : In the proper Bassini and Shouldice procedures, incising the transversalis fascia at the floor of the canal permits inspection for a femoral hernia. If a femoral hernia is present, a McVay repair is indicated. The Desarda repair does not require opening the canal floor, and thus the surgeon could fail to identify a femoral hernia. We suggest routinely creating a small opening in the floor of the canal to expose the space of Bogros and evaluate for the presence of a femoral hernia or interrogating the femoral orifice through the hernia sac.
Selecting a Tissue-Based Repair
Selection of a particular technique for tissue-based repair depends on surgeon familiarity and comfort with each approach. In experienced hands, the Shouldice repair is associated with recurrence rates that approach mesh repairs and is considered the optimal tissue-based technique. Both European Hernia Society and HerniaSurge guidelines recommend the Shouldice procedure for non-mesh repairs although rates of recurrence are noted to be considerably higher when performed by nonexpert surgeons [10, 11]. Evidence is lacking regarding the specific learning curves of the various tissue-based repairs; however, the Shouldice technique is considered notably challenging to master. Indeed, the Shouldice Hospital is reported to require 300 operations prior to considering a surgeon qualified [4]. Thus, it is reasonable to select a particular technique for tissue-based repair according to a combination of guidelines and individual surgeon comfort and training.
References
McGillicuddy JE. Prospective randomized comparison of the Shouldice and Lichtenstein hernia repair procedures. Arch Surg. 1998;133(9):974–8.
Danielsson P, Isacson S, Hansen MV. Randomised study of Lichtenstein compared with Shouldice inguinal hernia repair by surgeons in training. Eur J Surg. 1999;165(1):49–53. https://doi.org/10.1080/110241599750007504.
Nordin P, Bartelmess P, Jansson C, Svensson C, Edlund G. Randomized trial of Lichtenstein versus Shouldice hernia repair in general surgical practice. Br J Surg. 2002;89(1):45–9. https://doi.org/10.1046/j.0007-1323.2001.01960.x.
Evolution of Groin Hernia Surgery. World Guidelines for Groin Hernia Management: The HerniaSurge Group; 2016.
Amid PK, Shulman AG, Lichtenstein IL. Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg. 1994;220(6):735–7.
Read RC, McLeod PC Jr. Influence of a relaxing incision on suture tension in Bassini’s and McVay’s repairs. Arch Surg. 1981;116(4):440–5.
Stoppa R. Hernia of the abdominal wall. In: Chevrel J, editor. Hernias and surgery of the abdominal wall. 2nd ed. Berlin: Springer; 1997.
Bendavid R. The shouldice operation. In: Chevrel J, editor. Hernias and surgery of the abdominal wall. 2nd ed. Berlin: Springer; 1997.
Szopinski J, Dabrowiecki S, Pierscinski S, Jackowski M, Jaworski M, Szuflet Z. Desarda versus Lichtenstein technique for primary inguinal hernia treatment: 3-year results of a randomized clinical trial. World J Surg. 2012;36(5):984–92. https://doi.org/10.1007/s00268-012-1508-1.
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343–403. https://doi.org/10.1007/s10029-009-0529-7.
Simons MP, Kleijnen J, van Geldere D, Hoitsma HF, Obertop H. Role of the Shouldice technique in inguinal hernia repair: a systematic review of controlled trials and a meta-analysis. Br J Surg. 1996;83(6):734–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Carter, N.H., Chen, D.C. (2018). Tissue Repairs for Inguinal Hernia. In: LeBlanc, K., Kingsnorth, A., Sanders, D. (eds) Management of Abdominal Hernias. Springer, Cham. https://doi.org/10.1007/978-3-319-63251-3_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-63251-3_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63250-6
Online ISBN: 978-3-319-63251-3
eBook Packages: MedicineMedicine (R0)