Abstract
Swelling and pain in the groin are a common presentation for the abdominal surgeon. Nevertheless, diagnosis of a problem in the groin can still, in some cases, be a difficult clinical dilemma. It is fair to say that the diagnosis of an obvious swelling in the groin is usually straightforward, in terms of a hernia being present or not. However, the traditional inguinoscrotal hernia, where the hernial sac passes down into the scrotum, is a relatively uncommon event. Coupled with the increasing body mass index of the population, it is increasingly common for even a large groin hernia not to result in an obvious groin swelling. In some cases, where there is diagnostic doubt, thinking about several key questions may focus the investigation pathway:
-
Groin symptoms but no swelling, is there a hernia?
-
Groin swelling, but is it a hernia?
-
Hernia, but is it causing the symptoms?
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Inguinal Hernia: The Adolescent and the Adult
The younger the patient, the more likely the hernia is to be indirect. An indirect hernia is where the hernial sac follows and is closely associated with the spermatic cord. It thus starts at the deep inguinal ring, passing medially and inferiorly down the inguinal canal, where with time it will emerge from the superficial inguinal ring. As the hernia continues to enlarge and follow the spermatic cord into the scrotum, it is then named an inguinoscrotal hernia. In contrast, a direct inguinal hernia exploits a weakness in the transversalis fascia, in the region of the superficial inguinal ring. The hernial sac in this case is less adherent to the spermatic cord.
The majority of inguinal hernias are diagnosed by the patients when they see or feel a lump in their groin. The shower room seems to be a common theme to the place of diagnosis, for obvious reasons. Sometimes pain or discomfort draws the patient’s attention to the groin, but this is rarely a significant element in the patient’s symptoms to begin with. As the hernia enlarges, symptoms in the groin, particularly a dragging sensation, but at times quite marked pain, can be reported. This swelling, discomfort, or pain rapidly settles on lying down but returns as the patient becomes ambulant again. It is not unusual for the patient to report episodes of discomfort in the groin on exercise for months or even a few years prior to the appearance of a swelling in the groin. The natural history of hernia development is very variable, with some patients’ hernia remaining small in size for years, while in others, there is rapid progression of a small lump to a large hernia. Symptoms from an inguinal hernia are also very variable, ranging from no symptoms at all apart from the swelling to pain that significantly interferes with work and recreation of the patient. Patients with a chronic cough, or who have to strain to micturate or defecate, may complain of symptoms while performing these maneuvers. Inguinal hernias in women are more likely to present with pain. It is postulated that the closed inguinal canal in the adult female means that a small indirect hernia in women causes more stretching of the tissues and hence more pain.
As the length of time that the patient has had the hernia increases, the cumulative probability of pain increases to almost 90% at 10 years, and the probability of irreducibility increases from 6.5% at 12 months to 30% at 10 years [1]. Patients who have an asymptomatic hernia may not progress to irreducibility of the hernia as quickly. A recent randomized trial of surgery vs. watchful waiting management of an asymptomatic inguinal hernia reported 72% in the watchful waiting group crossed over to surgery by 7.5 years, with increase in hernia pain being the most common reason offered [2]. Of these 80 men assigned to watchful waiting, only two had incarceration of their hernia during the follow-up period.
Inguinal hernias are more common in adult males than in adult females in a ratio of 10:1. However, it must not be forgotten that indirect inguinal hernias in women are as common as femoral hernias in women.
A number of patients will present with bilateral inguinal hernia, although one side is usually significantly larger than the other. Sometimes this can indicate a connective tissue disorder such as Ehlers-Danlos syndrome, although such diseases are rare. Patients with ascites, such as heart or liver failure, are more prone to bilateral hernias, as are patients on continuous ambulatory peritoneal dialysis (CAPD). It is not clear whether the incidence in such groups is higher or whether the fluid in the abdominal cavity results in more symptoms so that such patients present sooner.
Another area that can cause some diagnostic difficulty is recurrent inguinal hernia. Pain tends to be a more prominent feature. The mechanism for this is unclear, although recurrent inguinal hernias often have a tighter neck, perhaps due to fibrosis from the previous mesh or suture repair limiting dilatation of the neck or constriction of the hernial sac contents. However, such patients often give a good history, and the giveaway line is the comment that the symptoms feel similar to when the patient had the hernia previously.
An interesting element to modern hernia practice is the so-called work-related hernia or hernia following a single strenuous event. The patient is aware of sudden pain in the groin while lifting, pulling, or straining at a task. At the same time, or shortly afterward, a swelling in the region of the groin is evident. There has been a debate as to whether this strenuous event causes the hernia or simply brings a preexisting asymptomatic hernia to the attention of the patient. Current opinion is more of the latter. The strenuous event precipitates identification of the hernia, which would have become evident in a few months’ to years’ time anyway, had the strenuous event not taken place. Several studies have reported on this. In one study [3], 129 patients with 145 hernias presenting with an inguinal hernia pursing a negligence claim, only in nine (7%) did the patient have a “convincing history suggestive” of an associated strenuous event. However, the time from this event to diagnosis of the hernia was up to 4 years. In another study [4], 133 consecutive patients presenting with a hernia (the majority of which were inguinal) were examined. Fourteen (11%) reported a sudden development of the hernia, but on detailed questioning of these patients, there was no good evidence to point to a single strenuous event as the cause. A further similar study [5] reported 108 patients who alleged that their hernia was the result of an accident, clearly a subset of the hernia patient population. While 51% did have an alleged identifiable strenuous event, of the remaining 49%, no hernia was detectable in 23%; there was no single event in 19%; and the hernia was documented present before the alleged accident in 6%. Nevertheless, work-related hernia has been and continues to be a source of work-related litigation for compensation. The following guidelines have been suggested when considering such a claim [3]:
-
1.
The incident of muscular strain must be reported officially to the patient’s line manager.
-
2.
There must be severe groin pain at the time of the strain.
-
3.
A diagnosis of a hernia must be made by a doctor within 30 days and preferably within 3 days.
-
4.
There should be no previous history of a hernia.
While there is little evidence to support the detail of these guidelines, they remain a useful, pragmatic approach to the problem. The compensation level is minimal, as causation is a problem; the strenuous event did not cause the hernia, but simply speeded up the patients being aware that they were developing a hernia anyway.
Femoral Hernia
A femoral hernia accounts for approximately 5–10% of all groin hernias in the adult [6]. In an analysis of 379 patients with groin hernia presenting electively at a university department of surgery, 16 patients had a femoral hernia. The correct diagnosis of femoral hernia was made in only three cases by general practitioners and in only six cases by surgical staff of all grades indicating the difficulty in diagnosis.
Most femoral hernias occur in women over 50 years. The incidence of femoral hernias, male to female, is around 1:4 (remember, inguinal hernias are much commoner in men, so femoral hernias in men represent just 1% of groin hernias but 27% in women). The different pelvic shape and additional preperitoneal fat in women are postulated to increase their risk compared to men. Women with femoral hernias are usually multiparous—multiple pregnancies are said to predispose to femoral herniation. Indeed, femoral hernias are as common in men as nulliparous women.
Forty percent of femoral hernias present as an emergency with incarcerated or strangulated hernia sac contents. It is a diagnosis that is often missed, with the patient vomiting for several days, often with plain films of the abdomen supporting small bowel dilatation. The patient or the nursing staff (if the patient is confined) then detects the red, painful groin swelling during bathing duties, which prompt calls for a surgeon. It is believed that femoral hernias are more likely to strangulate because of the relatively small neck to the sac, which also makes them less likely to be reduced in the emergency setting [7]. Ischemic bowel appears to be the major risk factor for death in the emergency setting [8], and thus patients, who are fit for surgery, should have femoral hernias repaired in a timely manner, and a watch-and-wait policy is not recommended. A study reported 111 patients undergoing femoral hernia repair in the Netherlands [9]. In the elective group, 10% of whom had significant comorbidity; there was no mortality and no bowel resection. Of the 33 patients treated as an emergency of which 20% had significant comorbid disease, there were 9 bowel resections and 3 deaths. The remainder of patients with a femoral hernia, who presented electively, complained of a groin lump and/or groin pain. About half of femoral hernias are irreducible at elective presentation.
The accuracy of diagnosis of femoral hernias in the community varies. In a retrospective review [6], letters of referral were traceable in 88% of elective patients with an operative diagnosis of femoral hernia. The correct diagnosis was arrived at by the referring general practitioner in less than 40% of cases, and the diagnostic rate was only improved by 20% in the hands of the surgical staff.
Differential Diagnoses of Groin Bulges
Hydrocele
The presence of a hydrocele in the adult will most commonly be associated with an inguinal hernia. In general, this does not present a diagnostic dilemma. However, there are situations in which either the hernia or the hydrocele is so large that the diagnosis is difficult to ascertain despite all the physical examination maneuvers that are employed. The use of diagnostic ultrasound will easily determine the diagnosis, as the use of transillumination in this circumstance is not always reliable.
Vascular Disease
Arterial—aneurysms of the iliac and femoral vessels: these may be complicated by distal embolization or vascular insufficiency, which will make the diagnosis more straightforward. A recent history of cardiac catheterization or transluminal angioplasty should raise awareness of a possible aneurysm.
Venous—a saphenovarix can be confused with a femoral hernia. Its anatomical site is the same, but its soft feel, fluid thrill, and disappearance when the patient lies down are characteristics. In a thin patient, the swelling may be a blue color. Varicose veins of the leg also support such a diagnosis, although varicose veins and groin hernias are associated with a common etiology of collagen disease. Venous bulging in the groin area during pregnancy is also well recognized and does not require surgery!
Inguinal venous dilation secondary to portosystemic shunting can result in a painful inguinal bulge. Again, there is a dramatic change on lying the patient flat. A Doppler ultrasound will confirm this with ease [10].
Lymphadenopathy
Chronic painless lymphadenopathy may occur in lymphoma and a spectrum of infective diseases. Acute painful lymphadenitis can be confused with a strangulated femoral hernia. A lesion in the watershed area, the lower abdomen, inguinoscrotal area, perineal region, anal canal, or the ipsilateral lower limb will often suggest this. Ultrasonic examination is very helpful to distinguish this pathology.
Tumors
Lipomas are very common tumors . The common “lipoma of the cord,” which in reality is an extension of preperitoneal fat, is frequently associated with an indirect or direct inguinal hernia. A study reported 140 inguinal hernias in 129 patients [11]. A fatty swelling was deemed significant if it was possible to separate it from the fat accompanying the testicular vessels. The fatty swelling was designated as being a lipoma if there was no connection with extraperitoneal fat and was designated as being a preperitoneal protrusion if it was continuous through the deep ring with extraperitoneal fat. Protrusions of extraperitoneal fat were found in 33% of patients and occurred in association with all varieties of hernia. There was a true lipoma of the cord in only one patient. It was concluded that the mechanisms causing the hernia were also responsible for causing protrusion of extraperitoneal fat. Read has commented that occasionally extraperitoneal protrusions of fat may be the only herniation, and therefore inguinal hernia classifications need to include not only fatty hernias but sac-less, fatty protrusions [12]. Indeed, in the laparoscopic approach, it is our impression that a lipoma of the cord may be more common than suggested above. Lipomas can also occur in the subcutaneous fat of the groin and upper thigh. A lipoma is rarely tender; it is soft with lobulated or scalloped edges, is not fixed to the skin, and does not have a cough impulse. A number of rare tumors have also been described, some arising in the pelvis and growing down the inguinal canal such as giant aggressive angiomyxoma [13] and tumors of the spermatic cord [14].
Secondary Tumors
A lymph node enlarged with metastatic tumor usually lies in a more superficial layer than a femoral hernia. Such lymph nodes are more mobile in every direction than a femoral hernia and are often multiple. A metastatic deposit of a tumor arising from the abdominal cavity such as adenocarcinoma can present as a rock-hard immobile mass that can be confused as either a primary incarcerated inguinal hernia [15] or a postoperative fibrotic reaction following inguinal hernia repair.
Genital Anomalies
Ectopic testis in the male—there is no testicle in the scrotum on the same side. Torsion of an ectopic testicle can be confused with a strangulated hernia.
Cyst of the canal of Nuck—these cysts extend toward or into the labia majora. They can be transilluminable [16].
Inguinal endometriosis can also mimic a hernia, although the cyclical nature of the swelling when present is the diagnostic giveaway [17].
Obturator Hernia
An obturator hernia , especially in the female, lies in the thigh lateral to the adductor longus muscle. Vaginal examination may sometimes help with the diagnosis. This hernia is nearly always detected as an emergency, with the patient presenting with bowel obstruction with a Richter’s-type hernia.
Rarities
A cystic hygroma is a rare swelling; it is loculated and very soft. Usually the fluid can be pressed from one part of it to another.
A psoas abscess is a soft swelling frequently associated with backache. It loses its tension if the patient is laid flat. It is classically lateral to the femoral artery. This will frequently be associated with elevation of the white blood cell count and a fever.
A hydrocele of the femoral canal is a rarity reported from West Africa. In reality it is the end stage of an untreated strangulated femoral epiplocele. The strangulated portion of omentum is slowly reabsorbed, the neck of the femoral sac remains occluded by viable omentum, while the distal sac becomes progressively more and more distended by a protein-rich transudate.
Clinical Examination of a Swelling in the Groin
Traditional surgical teaching is that the patients should be undressed and the entire abdomen and lower limbs examined. When the diagnosis of a hernia is suspected from the history and examination reveals an obvious hernia, then this pursuit of excellence is not necessary, and the patient is not expecting such exposure. However, if a hernia is not evident, then such exposure to allow adequate examination is necessary.
In the male, the first step is to observe where the testicles are. Knowledge of testicle position prevents all the confusions of undescended testicles, etc. If there is a significant scrotal swelling, the key question to differentiate between an inguinoscrotal hernia and a scrotal swelling is “can I get above the swelling and palpate a relatively normal cord,” which excludes an inguinoscrotal hernia. A lack of a cough impulse is additional support that the scrotal swelling is not a hernia. If the swelling is confined to the scrotum, the next key question is whether a testicle is palpable or, if not, a hydrocele is present. If a testicle is palpable, the next question is “is it normal?” If the testicle is diffusely enlarged and painful, then think infection, either bacterial or viral. If eccentrically enlarged, then a tumor is likely. If the swelling is separate from the testicle, but appears to be applied to one side of the testicle, then an epididymocele is likely. If the swelling is separate from the testicle but along the cord, then a spermatocele is likely.
The groin should be examined with the patient standing erect and again with the patient lying flat. Hernias are sometimes only apparent when the patients are standing or when they strain or cough. The majority of moderate and large hernias, especially in the nonobese, are evident on inspection of the groin in a standing patient with asymmetry evident between the two sides of the groin (Fig. 11.1). This swelling is then gently palpated, the patient is asked to cough, and a cough impulse will confirm the presence of a hernia. Sometimes the swelling will visibly increase in size, again consistent with a hernia. In small groin hernias or in the obese, visual inspection may not show a hernia so obviously. In this case, palpate the groin in both the anatomical positions of an inguinal or femoral hernia and also over the area where the patient feels pain.
If a cough impulse is not obvious, lie the patient down. Again palpate the groin before and during a cough. As the hernia is likely to have reduced by lying down, the cough impulse is often more prominent when lying down, and indeed the cough thrill of hernial sac contents passing under the examination fingers may be palpated.
As already discussed, the need to differentiate direct from indirect inguinal hernias and, to a lesser degree, inguinal from femoral hernias is largely a hangover from a far from perfect art from the past. The operative approach to groin hernias allows whichever groin hernia is encountered at surgery to be corrected. This is especially true of the laparoscopic approach to groin hernia repair. The key is to be able to make a diagnosis of a hernia and modify the surgical strategy depending on the hernia type found during surgery.
Previous surgery may add to the difficulty of hernia diagnosis. Femoral hernias may present as “recurrences” after repair of an inguinal hernia at open surgery [18]. In these circumstances, they are often indistinguishable from inguinal hernias. The diagnostic difficulty is increased by the fact that as a femoral hernia emerges through the cribriform fascia at the fossa ovalis, the fundus comes forward and then turns upward to lie over and anterior to the inguinal ligament. If the external ring and the cord can be palpated, the diagnosis is more easily made. The difficulty is in the female. If the hernia can be reduced, careful palpation of the hernial aperture should enable the examiner to orientate it relative to the inguinal ligament. If the hernia emerges above the inguinal ligament when the patient coughs, the hernia is inguinal: if below the ligament, it is femoral.
Reducing the hernia and then using one finger to hold it while the patient coughs is a useful test, which will enable the inguinal canal or the femoral ring to be identified, almost with certainty. This test becomes less reliable the fatter the patient becomes, as accurate location of landmarks becomes more difficult. Invagination of the scrotal skin into the inguinal canal, a time-hallowed test, is uncomfortable for the patient and does not provide useful information, except perhaps in small indirect inguinal hernias.
Remember, once you have thought about a lump or swelling in terms of any changes in the skin overlying the lump; the position, size, shape, and consistency of the lump; any fixation to the skin or deep tissues; disappearance of the lump when contracting the muscles in the area; fluctuation or pulsation of the lump; and in the scrotum, transillumination, the diagnosis of the swelling is usually evident. Further investigations may be necessary, not to confirm the type of lump or swelling but to investigate the cause of the lump, especially if malignancy is expected, but this is out with the remit of this chapter.
Inguinoscrotal Pain
Inguinoscrotal pain may arise in the groin and radiate to the ipsilateral hemiscrotum, thigh, flank, or hypogastrium. Such pain may be neuralgic in type and accentuated by physical exertion. If the cause is a hernia or preperitoneal fat forcing its way out through the deep inguinal ring, it is postulated that these structures are stretched and pain fibers are stimulated. This is thought to cause a local reflex increase of tone in the internal oblique and transversus muscles coupled with neuralgic pain from stretching of the ilioinguinal nerve. The pain due to increase in tone is intermittent, whereas the neuralgic pain leading to hyperalgesia can be constant. This pain can resolve following hernia repair but sometimes can persist following surgery. It is imperative that this fact be made known to the patient preoperatively.
Numerous other conditions can give rise to acute or chronic pain in the inguinoscrotal and neighboring anatomical regions (Table 11.1). These include gynecological and urological pathology and a variety of musculoskeletal syndromes. An important entity increasingly being characterized is the syndrome of Gilmore’s groin or the sportsman’s hernia. Thus, patients presenting with pain, as opposed to a painless, reducible swelling in the groin, require a careful history and examination for urological, gynecological, and musculoskeletal disorders.
In many patients presenting with chronic groin pain, a urological disorder is the initial working diagnosis. Chronic prostatitis or seminal vesiculitis is commonly suspected, and many patients may have been treated with multiple courses of antibiotics.
When pain is the main presentation, it is useful to ask patients to shade in pain areas on an anatomical diagram, to identify areas in which the pain occurs and is developing (Fig. 11.2). Sometimes patients will point to an area of spot tenderness with one finger, but a more diffuse area of pain is more typical.
Clinical Examination of Patients with Groin Pain
Examination will have begun as you observe the patient walking into your office. However, it is useful to ask the patient to walk and observe their gait. Exposure from the abdomen to the toes is necessary while preserving their modesty as best as possible. Palpate the spine. Test for movement of the lumbar spine in forward, backward, and lateral flexion and rotation. Ask the patient to hop on one and then the other foot. Pain elicited over the pubic symphysis while hopping points to instability or osteitis pubis. Perform bilateral femoral nerve stretch tests. Examine the patient standing as described above for a possible hernia in the groin. Then lay the patient flat and perform full active and passive movements of the hip, comparing one side with the other. Sportsmen, especially those with well-developed quadriceps muscles (hockey players), load their hip joint in an abnormal way, and early arthritis can be picked up by subtle reduction in the range of movement on the affected side. Perform bilateral sciatic nerve stretch tests. Palpate carefully the whole of the groin and upper thigh area, although the area of palpation will at times be focused if the patient reports pain in one spot. Enthesopathy—tennis elbow of the groin (inflammation of the insertion, enthesis, of a ligament or tendon) [19]—typically produces point tenderness at the affected site, in particular at the adductor longus insertion, inguinal ligament insertion, rectus abdominis insertion, or along the inguinal ligament at sites where the transversalis and internal oblique muscles insert. Such symptoms may respond to local injection of long-acting local anesthetic and steroid. If no point tenderness is evident, then examine the pectineus muscle, adductor muscles (magnus, brevis, and longus), and gracilis muscle by palpation, passive abduction, and adduction against resistance and hip flexion. The rectus abdominis muscle should be examined by active contraction with both legs elevated and by palpation of its origins. Examine the bony pelvis by palpation of the pubic arches, the crests and tubercles, and the pubic symphysis by compression and direct pressure. Depending on the patient’s symptoms, a full neurological examination of the lower limb and affected groin, with particular reference to ilioinguinal or genitofemoral nerve neuralgias, may be appropriate.
In sportsmen’s hernia, the clinical findings following a period of rest may be minimal. However, following a period of training or sporting activity, the whole inguinoscrotal region may be tender. While examination is important to rule out other pathology, it is my feeling that the sequence of events in the history is more important in reaching a diagnosis than the examination findings, as there is no single finding or test that easily supports the diagnosis. Palpation of the external ring by invagination of the scrotal skin is an uncomfortable maneuver, but it is typically much more painful on the affected side, which is made worse by coughing, and a more prominent cough impulse may be detected. If the diagnosis is still in doubt, ask the patient to adopt a half sit-up and cough while the margins of the superficial ring and the posterior inguinal wall palpated. An enlarged tender ring and posterior pain as compared to the other side are evidence of inguinal canal disruption [20].
Clinical examination of the scrotum may be necessary if the diagnosis is still not clear or there are symptoms in the scrotum. A small hernia protruding at the deep ring may stimulate the genital branch of the genitofemoral nerve to give scrotal pain in the male or labial pain in the female as its feature. If the patient presents acutely complaining of pain in the groin associated with a lump, the differential examination should look for hernias, torsion of the testicle or testicular appendage, spasm of the cremaster, and trauma to the testicle or cord.
Other rare causes of inguinoscrotal pain include abdominal aneurysms, degenerative disease of the lower thoracic and lumbar spines, and degenerative disease of the hip joint. The genital pelvic viscera, prostate, seminal vesicles, and proximal vasa have an autonomic supply from T12 to L2 and from S2 to S4. Referred pain from these organs may radiate via the genital branch of the genitofemoral nerve L1 and posterior scrotal nerves S2 and S3 to the groin and external genitalia.
Investigations in Occult Hernia and Groin Pain
In the majority of cases, a good history and examination is all that is required to establish the likely diagnosis and initiate management. However, there are occasions where help from a radiologist or a laparoscopy may help with the management. The tests will be discussed in turn and then use such investigations to answer the three questions laid out in the introduction of this chapter summarized.
Herniography
Herniography is still popular with some hernia surgeons, although I have not requested this investigation in 10 years! In those patients referred to me who have had a herniogram demonstrating a symptomatic hernia, I would have been happy to offer hernia surgery on the basis of the history and clinical examination alone. Nevertheless, herniography is used by many surgeons and is a sensitive tool, capable of demonstrating hernias in the groin, especially when clinical examination is negative [21]. One study reported lateral protrusion of the urinary bladder (“bladder ears”) into the deep inguinal ring in 9% of 406 patients undergoing intravenous urography and cystograms [22].
Direct herniography was first performed in experimental animals [23] and subsequently performed in children [24]. Herniography with fluoroscopy and peritoneography, performed by puncture of the abdominal wall and injection of nonionic contrast medium, is now the preferred method of investigation [25]. Indications are principal symptoms indicative of a hernia but no palpable lump, obscure groin pain (other diagnoses having been excluded by appropriate investigation), and evaluation of patients who remain symptomatic following primary hernia repair.
Technique is important. The patients must be placed on a tilt table with fluoroscopy, enabling tangential views of the pelvic floor and groin. The bladder should be empty at the time of the examination to avoid inadvertent puncture. A needle puncture is performed using a 22-G spinal needle or occasionally a 21-G Chiba needle at the border of the lateral rectus muscle below the level of the umbilicus on the opposite side to the patient’s symptoms. This site of puncture is chosen to minimize the risk of injury to the inferior epigastric vessels. Typically three pops are felt as the needle traverses the anterior rectus sheath, posterior rectus sheath, and transversalis fascia to enter the peritoneal cavity. Correct needle placement within the peritoneal cavity is confirmed by injection of a small volume of nonionic contrast under fluoroscopic guidance, which should freely run away from the needle tip. Approximately 60–80 mL of contrast is then injected with the head of the table elevated 30° to encourage the contrast to pool in the various fossae and hernial orifices. After the contrast has been injected, the patient is turned prone with the head elevated 20°, and PA and oblique views are taken. The patient is then instructed to exercise for 15–20 min, and repeat radiographs are taken with additional views obtained with the patient straining and coughing or during any other maneuver, which precipitates the symptoms.
A thorough examination of the entire surgical anatomy of the pelvic and inguinal floor should be performed for exact verification of all potential hernia orifices. Figure 11.3 demonstrates a normal herniogram.
The different types of hernia can be diagnosed from their shape, relation to the pelvic peritoneal folds, and the resulting pelvic fossae. Five pelvic peritoneal folds in the pelvis and groin (lateral umbilical, medial umbilical, and median umbilical) divide the pelvic cavity into five fossae: the supravesical, the left and right medial umbilical, and left and right lateral umbilical fossae. An indirect hernia protrudes lateral to the lateral fold through the lateral (inguinal) fossa. A direct inguinal hernia protrudes lateral to the median fold through the medial (inguinal) fossa, whereas a femoral hernia protrudes through the median umbilical fossa in a lateral direction through the femoral canal. Figure 11.4 demonstrates herniograms depicting bilateral indirect hernias in a patient suspected clinically of having a unilateral left-sided hernia.
Herniography can be used in the postoperative evaluation of patients with persistent symptoms in whom clinically detectable hernias are not evident on physical examination. One study [26] performed herniograms in 46 patients with 54 symptomatic sites. Ten recurrent hernias were found, although only two were symptomatic. In addition, 14 hernias were found in the contralateral, asymptomatic groin, and the herniogram was negative in one patient with a clinical hernia. Although herniography can demonstrate a hernia, 22 of the hernias detected in this study had no clinical significance, and the reason for performing the study in the patient with a clinically evident hernia is unclear.
Inguinal and femoral hernias are most easily detected by herniography. Anterior wall defects such as ventral, Spigelian, and obturator hernias are less well demonstrated [27] and are more eloquently demonstrated by CT or MRI.
Complications of herniography occur in around 6% of patients. Fortunately the majority of these are minor, including hematoma of the anterior abdominal wall, adverse reaction to the contrast, and extraperitoneal extravasation of contrast medium. More serious, infrequent complications include bowel perforation, mesenteric hematoma formation, and pelvic peritonitis.
In short, herniography can detect occult hernias and aid in the diagnosis of obscure groin pain, and series of patients said to benefit from the investigation continue to be reported [28]. It is performed under local anesthesia on an outpatient basis with minimal complications [29]. Visceral perforation is a rare hazard that does not usually require significant intervention [30]. However, herniography use is no longer in widespread use.
Ultrasonography
Ultrasound examination of the abdominal wall and inguinal region is being used increasingly in the diagnosis of occult hernia and groin pain. This has the advantage of avoiding the use of ionizing radiation, but the quality and accuracy of the study depend on the skill and experience of the sonographer and the body habitus of the patient. The technique is performed using a medium- to high-frequency linear array probe (7–13.5 MHz) depending on the patient’s body habitus. The patient is initially examined in the supine position before and during the Valsalva maneuver and with coughing with the transducer placed parallel to the inguinal ligament with the inferior epigastric vessels used as a landmark in an attempt to distinguish between indirect and direct inguinal hernias. Using the same transducer orientation, the femoral canal is then examined to assess for a femoral hernia. Both sides are examined and the procedure should be repeated with the patient in the erect position if the supine examination is negative despite a strong clinical suspicion of an occult hernia.
Although the procedure is operator dependent, in experienced hands, ultrasonography has a reported sensitivity and specificity approaching 100% in determining the nature of groin hernia [31]. When used for the assessment of equivocal groin signs and groin pain, the accuracy of ultrasound is not so good [32]. False interpretation is said to be more likely to occur in cases of femoral hernia, although a recent study reported an accuracy of 37% in detecting clinically occult femoral hernias [33]. The typical findings and interpretation of a femoral hernia are shown in Fig. 11.5.
The antenatal diagnosis of abdominal wall defects is now a successful part of obstetric/pediatric practice. Patients born with significant abdominal wall herniation can be detected prenatally and thus delivered in a unit with the appropriate pediatric surgical expertise.
The use of ultrasound to diagnose hernias in small children is less successful. One study reported ultrasound assessment of the contralateral groin accurately diagnoses a patent processus vaginalis in only 15 of 23 infants, with four false-positive and four false-negative cases [34]. Thus ultrasound alone should be used with caution to plan management of the contralateral groin in infants. An interesting study reported that inguinal hernias could be accurately diagnosed using the parent’s digital photographs when the physical examination is not diagnostic [35].
In boys, where there is doubt about the diagnosis, ultrasound is a noninvasive and highly accurate diagnostic tool [36]. Using 4 mm as the upper limit of the normal diameter of the internal ring, occult inguinal hernias can be diagnosed with 98% accuracy.
A small study in 19 patients with clinically diagnosed groin hernias assessed the ability of color Doppler sonography to distinguish between different types of groin hernia in adults [37]. The inferior epigastric artery was used as a landmark to differentiate different types of hernia sac but was only visualized in 55% of cases making this examination an unreliable method for differentiating hernia types. However, a more recent study has reported a much higher accuracy of 96% in differentiating hernia types [38]. The use of a protocol-driven approach for ultrasound evaluation of the groin is suggested to ensure an accurate and comprehensive evaluation of the groin region [39].
Computed Tomography
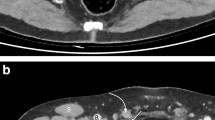
Cross-sectional imaging by CT scanning can accurately evaluate disorders of the abdominal wall, including hernias. In the elective setting, CT scanning of a lump in the groin is indicated when the lump is not considered on clinical grounds to be a hernia. CT scanning will delineate tumors of the anterior abdominal wall, lymph node masses, and tumors of the abdominal cavity enlarging though hernial orifices. Inflammatory conditions and abscesses within the abdomen and pelvic can also be detected. Sometimes such tumors and other conditions can be the causes of groin pain (Fig. 11.6). Several studies describe the use of CT scanning to differentiate clinically evident hernias of the groin into inguinal or femoral [40, 41] (Fig. 11.7) and between direct and indirect hernias (Fig. 11.8) [42]. The multiplanar high-resolution reconstructions obtained from multidetector CT scans clearly depict the inferior epigastric vessels to allow differentiation of indirect from direct hernias. The femoral canal can also be directly visualized (using the inguinal ligament, femoral vein, and adductor longus as landmarks), thus allowing the diagnosis of femoral hernias.
To laparoscopic groin surgeons, and I expect to most open groin hernia surgeons also, this is seen as a waste of resource and unnecessary radiation risk to the patient with the usual type of groin hernia.
The real role of CT scanning is in the assessment of a patient with difficult to diagnosis multiply recurrent herniation or with obstruction of the bowel. Femoral and obturator hernias, with a Richter’s-type hernia, can be difficult to detect clinically until infarction and perforation of the bowel have occurred. CT scan eloquently demonstrates these otherwise occult hernias to be the cause of the underlying bowel obstruction (Fig. 11.9). It is also useful to rule out other sources of lower abdominal or groin pathology as the source of pain. However, the detection of a clinically occult hernia on CT in a patient with groin pain needs careful consideration that the hernia is truly the cause of the pain [43].
Magnetic Resonance Imaging
MRI of the abdomen and pelvis is also increasing in use for the assessment of groin pain and groin swellings not thought to be a hernia (Fig. 11.10). MRI provides superb soft tissue resolution with multiplanar anatomical depiction and avoids the use of ionizing radiation. It is a useful “screening” tool to detect foci of inflammation that may explain the patient’s symptoms, especially in athletes. Osteitic changes particularly in the pubis are detected as areas and low signal intensity on T1-weighted images of high and homogenous signal intensity on T2-weighted scans [44] (Fig. 11.11). Abnormalities in myotendinous structures are also well documented by this technique as is involvement of the sacroiliac joints [45]. Groin hernias can be detected on MRI, which allows direct visualization of the hernial sac within the inguinal or femoral canal (Fig. 11.12). More rapid sequence times also allow the scan to be performed with a Valsalva technique [46].
Laparoscopy
This investigation has merit as treatment can sometimes be undertaken at the same time. There have always been cases, where the history is suggestive of a hernia (including the so-called sportsman’s hernia), but the clinical findings are equivocal, yet the patient has symptoms that interfere with work or social activities. In such patients, I discuss investigation options vs. exploring their groin with a laparoscope. While traditional intraperitoneal laparoscopy is within the ability of most general and hernia surgeons, lipomas of the cord, obturator hernias, and small femoral hernias when there is little in the way of hernial sac can be missed by this approach. If a hernia is found by conventional laparoscopy, then the options would be to do a TAPP or convert to a traditional open operation or perhaps convert to a TEP depending on the surgeon’s experience. I still feel uncomfortable exploring the groin by open surgery, when the diagnosis is not clear, because of the small risk of severe chronic groin pain (in the region of 2–3%), while severe chronic pain following laparoscopic surgery is a more rare event but can still occur (see Chap. 23 on Pain).
Clinical Dilemmas
-
1.
Symptom but no swelling: is there a hernia?
The investigative options here are to consider an ultrasound scan first, perhaps a herniogram, but my preference unless significant anesthetic risk or contraindication is to proceed with laparoscopy and perform a TAPP repair.
-
2.
Swelling, but is it a hernia?
The investigative options here are to consider an ultrasound scan first, followed by an MRI or CT scan if the ultrasound is equivocal, or further evaluation of deeper aspects of the swelling is necessary.
-
3.
Hernia, but is it causing the symptoms?
The investigative options here are to consider an MRI scan first. If this is normal or fails to identify an alternate obvious cause for the symptoms, then proceed with laparoscopy (or open exploration) of the groin.
Conclusions
An effort should be made to distinguish inguinal from femoral hernias before surgery to help plan the surgical approach. However, with laparoscopic surgery, this is less important as all the hernial orifices in the groin can be easily exposed during the operation.
Careful identification of the pubic tubercle, the anterior superior iliac spine, and, between them, the inguinal ligament is the prerequisite. Inguinal hernias emerge from the fascia transversalis above this line and femoral hernias below it.
Femoral hernias never pass from the abdomen into the scrotum or labia majora as indirect inguinal hernias do.
The diagnosis of inguinoscrotal pain can be a challenging clinical problem. A diagnosis can often be achieved by taking a detailed history and examination, supported with appropriate radiological investigation [47, 48].
References
Hair A, Paterson C, Wright D, Baxter JN, O’Dwyer PJ. What effect does the duration of an inguinal hernia have on patient symptoms? J Am Coll Surg. 2001;193:125–9.
Chung L, Norrie J, O’Dwyer PJ. Long-term follow-up of patients with a painless inguinal hernia from a randomized trial. Br J Surg. 2011;98:596–9.
Smith GD, Crsoby DL, Lewis PA. Inguinal hernia and a single stressful event. Ann R Coll Surg Engl. 1996;78:367–8.
Pathak S, Poston GJ. It is highly unlikely that the development of an abdominal wall hernia can be attributable to a single strenuous event. Ann R Coll Surg Engl. 2006;88:168–71.
Schofield PF. Inguinal hernia: medicolegal implications. Ann R Coll Surg Engl. 2000;82:109–10.
Hair A, Paterson C, O’Dwyer PJ. Diagnosis of a femoral hernia in the elective setting. J R Coll Surg Edinb. 2001;46:117–8.
Harissis HV, Douitsis E, Fatouros M. Incarcerated hernia: to reduce or not to reduce. Hernia. 2009;13:263–6.
Derici H, Unalp HR, Bozdaq AD. Factors affecting morbidity and mortality in incarcerated abdominal wall hernia. Hernia. 2007;11:341–6.
Kemler MA, Oostvogel HJM. Femoral hernia: is a conservative policy justified? Eur J Surg. 1997;163:187–90.
Horn TW, Harris JA, Martindale R, Gadacz T. When a hernia is not a hernia: the evaluation of inguinal hernias in the cirrhotic patient. Am Surg. 2001;67:1093–5.
Fawcett AN, Rooney PS. Inguinal canal lipoma. Br J Surg. 1997;84:1169–70.
Read RC, White HJ. Lipoma of the spermatic cord, fatty herniation, liposarcoma. Hernia. 2000;4:149–54.
Sozutek A, Irkorucu O, Reyhan E, et al. A giant aggressive angiomyxoma of the pelvis misdiagnosed as incarcerated femoral hernia: a case report and review of the literature. Case Rep Surg. 2016;2016:1–6.
Valeshabad AK, et al. An important mimic of inguinal hernia. Urology. 2016;97:e11.
Buchs NC, Bloemendaal AL, Guy RJ. Localized peritoneal carcinomatosis mimicking an irreducible left inguinal hernia. Ann R Coll Surg Engl. 2016;98(3):e52–4.
Sarkar S, Panja S, Kumar S. Hydrocele of the canal of Nuck (female hydrocele): a rare differential for inguinal-labial swelling. J Clin Diagn Res. 2016;10(2):PD21–2.
Pandey D, Coondoo A, Shetty J, Mathew S. Jack in the box: inguinal endometriosis. BMJ Case Rep. 2015;2015. https://doi.org/10.1136/bcr-2014-207988.
Henriksen NA, Bisgaard Thorup J, Jorgensen LN. Unsuspected femoral hernia in patients with a prospective diagnosis of recurrent inguinal hernia. Hernia. 2012;16:381–5.
Ashby EC. Chronic obscure groin pain is commonly caused by enthesopathy: ‘tennis elbow’ of the groin. Br J Surg. 1994;81:1632–4.
Macleod DAD, Gibbon WW. The sportsman’s groin. Br J Surg. 1999;86:849–50.
Eames NWA, Deans GT, Lawson JT, Irwin ST. Herniography for occult hernia and groin pain. Br J Surg. 1994;81:1529–30.
Allen RP, Condon VR. Transitory extraperitoneal hernia of the bladder in infants (bladder ears). Radiology. 1961;77:979–83.
Sternhill B, Schwartz S. Effect of hypaque on mouse peritoneum. Radiology. 1960;75:81–4.
Ducharme JC, Bertrand R, Chacar R. Is it possible to diagnose inguinal hernia by x-ray? J Can Assoc Radiol. 1967;18:448.
Gullmo A. Herniography. World J Surg. 1989;13:560–8.
Hamlin JA, Kahn AM. Herniography in symptomatic patients following inguinal hernia repair. West J Med. 1995;162:28–31.
Harrison LA, Keesling CA, Martin NL, Lee KR, Wetzel LH. Abdominal wall hernias: review of herniography and correlation with cross-sectional imaging. Radiographics. 1995;15:315–32.
Hachem MI, Saunders MP, Rix TE, Anderson HJ. Herniography: a reliable investigation avoiding needless groin exploration—a retrospective study. Hernia. 2009;13:57–60.
MacArthur DC, Grieve DC, Thompson JD, Greig JD, Nixon SJ. Herniography for groin pain of uncertain origin. Br J Surg. 1997;84:684–5.
Heise CP, Sproat IA, Starling JR. Peritoneography (herniography) for detecting occult inguinal hernia in patients with inguinodynia. Ann Surg. 2002;235:140–4.
Djuric-Stefanovic A, Saranovic D, Ivanovic A, et al. The accuracy of ultrasonography in classification of groin hernias according to the criteria of the unified classification system. Hernia. 2008;12:395–400.
Depasquale R, Landes C, Doyle G. Audit of ultrasound and decision to operate in groin pain of unknown aetiology with ultrasound technique explained. Clin Radiol. 2009;64:608–14.
Gupta H, Subedi N, Robinson P. Effectiveness of sonography in detecting clinically occult femoral hernias. J Ultrasound Med. 2016;35:1675–9.
Lawrenz K, Hollman AS, Carachi R, Cacciagnerra S. Ultrasound assessment of the contralateral groin in infants with unilateral inguinal hernia. Clin Radiol. 1994;49:546–8.
Kawaguchi AL, Shaul DB. Inguinal hernias can be accurately diagnosed using the parent’s digital photographs when the physical examination is nondiagnostic. J Pediatr Surg. 2009;44:2327–9.
Chen KC, Chu CC, Chou TY, Wu CJ. Ultrasound for inguinal hernias in boys. J Pediatr Surg. 1999;34:1890–1.
Zhang GQ, Sugiyama M, Hagi H, Urata T, Shimamori N, Atomi Y. Groin hernias in adults; value of colour Doppler sonography in their classification. J Clin Ultrasound. 2001;29:429–34.
Lee RK, Griffith JF, Ng WH. High accuracy of ultrasound in diagnosing the presence and type of groin hernia. J Clin Ultrasound. 2015;43:538–47.
Jacobson JA, Khoury V, Brandon CJ. Ultrasound of the groin: techniques, pathology and pitfalls. Am J Roentgenol. 2015;205:513–23.
Cherian PT, Parnell AP. The diagnosis and classification of inguinal and femoral hernia on multisection spiral CT. Clin Radiol. 2008;63:184–92.
Kitami M, Takase K, Tsuboi M, et al. Differentiation of femoral and inguinal hernias on the basis of anteroposterior relationship to the inguinal ligament on multidimensional computed tomography. J Comput Assist Tomogr. 2009;33:678–81.
Hahn-Pederson J, Lund L, Hansen-Hojhus J, Bojsen-Muller F. Evaluation of direct and indirect inguinal hernia by computed tomography. Br J Surg. 1994;81:569–72.
Garvey JF. Computed tomography scan diagnosis of occult groin hernia. Hernia. 2012;16:307–14.
Omar IM, Zoga AC, Kavanagh EC, et al. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008;28:1415–38.
Barile A, Erriquez D, Cacchio A, DePaulis F, Di Cesare E, Masciocchi C. Groin pain in athletes: role of magnetic resonance. Radiol Med. 2000;100:216–22.
Leander P, Ekberg O, Sjoberg S, Kesek P. MR imaging following herniography in patients with unclear groin pain. Eur Radiol. 2000;10:1691–6.
Robinson A, Light D, Kasim A, Nice C. A systematic review and meta-analysis of the role of radiology in the diagnosis of occult inguinal hernia. Surg Endosc. 2013;27:11–8.
Miller J, Cho J, Michael MJ, Saouaf R, Towfigh S. Role of imaging in the diagnosis of occult hernias. JAMA Surg. 2014;149:1077–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
de Beaux, A.C., Patel, D. (2018). Diagnosis of a Lump in the Adult Groin. In: LeBlanc, K., Kingsnorth, A., Sanders, D. (eds) Management of Abdominal Hernias. Springer, Cham. https://doi.org/10.1007/978-3-319-63251-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-63251-3_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-63250-6
Online ISBN: 978-3-319-63251-3
eBook Packages: MedicineMedicine (R0)