Abstract
This chapter will review management of ear carcinomas with an emphasis on radiotherapy technique and published data.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Pearls
-
The external ear consists of the pinna (auricle), external auditory canal (EAC), tympanic membrane.
-
The middle ear contains the auditory ossicles and communicates with the pharynx via the Eustachian tube.
-
The inner ear is in the petrous portion of the temporal bone and consists of the bony and membranous labyrinth.
-
The University of Florida published a contouring atlas of the middle and inner ear (Pacholke, Am J Clin Oncol 2005).
-
Primary middle ear and temporal bone tumors are rare, but external ear cutaneous malignancies may involve these structures.
-
BCC >> SCC for malignancies of the external ear, but SCC accounts for 85% of EAC, middle ear, and mastoid tumors.
-
Nodal metastases occur in <15% with lymphatic drainage to parotid > cervical > postauricular nodes.
Workup
-
H&P with otoscopy and careful LN exam. CBC, chemistries, BUN/Cr. CT, MRI. Biopsy.
-
Audiologic testing includes measuring pure tone threshold with both air and bone conduction, speech reception threshold, word discrimination score, and impedance audiometry.
Treatment Recommendations
-
Tumors of the external ear may be treated with surgery or RT (either EBRT or IS brachytherapy). Surgery is used if the lesion has invaded the cartilage or extends medially into the auditory canal. Advanced lesions or close/+ margins require post-op RT. Treatment of the lymphatics may be indicated for tumors >4 cm or for cartilage invasion.
-
Tumors of the middle ear or temporal bone may be treated with surgery or RT. Facial nerve paralysis at presentation is considered a negative prognostic feature. Surgery may require mastoidectomy or subtotal or total temporal bone resection. Lateral temporal bone resection is often indicated for T1–2 cases and en bloc subtotal or total temporal bone resection for T3–4 tumors. Post-op RT is generally required for close/+ margin or T2–4 disease to increase LRC.
-
LC depends on the extent of disease, and ranges from 40 to 100% across multiple small published case series (owing to rarity of condition).
-
Preoperative RT or chemo-RT has also been advocated as an alternative to post-op RT for selected cases (Nakagawa, Otol Neurotol 2006).
Studies
-
Madsen (Head Neck 2008): 68 primary cancers of EAC and middle ear in Denmark. Five years LRC rates for surgery, RT, or surgery + RT were 55.6%, 47.4%, and 45.3%, respectively. Of 28 recurrences, 24 were purely local.
-
Pfreundner (IJROBP 1999): 27 primary carcinomas of EAC and middle ear. Five-year OS 61%. Five-year LC 50%. Five-year OS by stage: T1–T2 86%, T3 50%, T4 41%. Complete resection and clear margins were prognostic. All patients with dural invasion died.
-
Ogawa (IJROBP 2007). 87 pts with EAC SCC, 61% treated with surgery and post-op RT, 39% with RT alone. 5-yr DFS with surgery and post-op RT: T1 75%, T2 75%, T3 46%. 5-yr DFS with RT alone: T1 83%, T2 45%, T3 0%. T-stage and margins prognostic.
-
Yin (Auris Nasus Larynx 2006). 95 SCC cases of middle ear and EAC. 14% had regional LN metastasis. 5-yr OS: stage I/II 100%, stage III 67%, stage IV 30%. Stage, completeness of resection with negative margin, recurrence, and metastasis influence survival.
-
Clark (J Plastic Reconstr Aesthet Surg 2008): Meta-analysis of LN metastases from auricular SCC. Metastatic rate is 11.2%, commonly to parotid and upper cervical chain. Usually develops within 12 months and half will die.
Radiation Techniques
Simulation and Field Design
-
Definitive RT (usually considered for early-stage or inoperable advanced-stage pts).
-
Superficial tumors of the pinna may be treated with electrons or orthovoltage photons. For small tumors, 1 cm margins are adequate, but for larger lesions, 2–3 cm margins are required (see Chap. 1).
-
Advanced or unresectable EAC or middle ear tumors may be treated definitively with high energy electrons (energy appropriate for tumor depth) alone or mixed with photons, or with 3DCRT/IMRT if coverage of nodal volumes is desired.
-
GTV: clinical and radiographic gross disease.
-
CTV1: GTV + 0.3–0.5 cm margin; 66–70 Gy at 2.0 Gy per fraction.
-
CTV2: CTV1 + 0.5–0.7 cm margin, including ipsilateral preauricular and postauricular nodes, and upper level II nodes, and parotid gland (if involved); 63 Gy at 1.8 Gy per fraction.
-
CTV3 (considered for more advanced and aggressive tumors): ipsilateral level III and IV, contralateral level II; 56 Gy at 1.6 Gy per fraction.
-
PTV: CTV + 0.3–0.5 cm margin.
-
-
-
Postoperative treatment.
-
CTV1: original tumor, surgical bed, soft-tissue invasion, areas with possible residual disease; 60–66 Gy at 2 Gy per fraction (62–70 Gy at 2–2.2 Gy per fraction for gross residual disease).
-
CTV2: CTV1 + 0.5–0.7 cm margin, depending on anatomy include ipsilateral level II and parotid; 54–60 Gy at 1.8 Gy per fraction.
-
CTV3: ipsilateral level III and IV ± contralateral level II; 50–54 Gy at 1.6 Gy per fraction.
-
PTV: CTV + 0.3–0.5 cm margin.
-
Care should be taken to cover the glenoid fossa of the TMJ and periauricular soft tissue as marginal misses have been identified in these locations with IMRT (Chen, IJROBP 2012).
-
-
Immobilization with a thermoplastic mask is necessary.
-
Use wax bolus to fill EAC and surrounding concha for pinna tumors to decrease complications and improve homogeneity and superficial dose delivery.
-
In carefully selected pts at experienced centers, post-op intracavitary brachy boost may be considered (Badakh, J Cancer Res Ther 2014).
Dose Prescriptions
-
Tumors of the pinna may be treated with 1.8–2 Gy per fraction to 50 Gy for small, thin lesions <1.5 cm, 55 Gy for larger tumors, 60 Gy for minimal or suspected cartilage or bone invasion, or 65 Gy for large lesions with bone or cartilage invasion.
-
Tumors of the auditory canal or temporal bone: postoperative, 54–66 Gy; definitive, 66–70 Gy, and may consider chemo-RT.
Dose Limitations
-
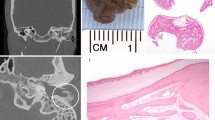
Limit temporal bone to ≤70 Gy to minimize risk of osteoradionecrosis (∼10% for doses >65 Gy) (Fig 4.1).
Complications
-
Cartilage necrosis of the pinna and/or temporal bone necrosis is possible if careful planning is not used.
-
Neurosensory: hearing compromise or loss.
-
Chronic otitis media.
-
Xerostomia.
Follow-Up
-
Frequent H&P with otoscopy every 3–4 months for 1–2 years, then every 6 months for 1–2 years, then annually.
References
Badakh DK, Grover AH. To analyze the impact of intracavitary brachytherapy as boost radiation after external beam radiotherapy in carcinoma of the external auditory canal and middle ear: A retrospective analysis. J Cancer Res Ther. 2014;10(2):342.
Chen WY, Kuo SH, Chen YH, et al. Postoperative intensity-modulated radiotherapy for squamous cell carcinoma of the external auditory canal and middle ear: treatment outcomes, marginal misses, and perspective on target delineation. Int J Radiat Oncol Biol Phys. 2012;82(4):1485–93.
Clark RR, Soutar DS. Lymph node metastases from auricular squamous cell carcinoma. A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg. 2008;61(10):1140–7.
Gal T, Futran N, Bartels L, et al. Auricular carcinoma with temporal bone invasion: outcome analysis. Otolaryngol Head Neck Surg. 1999;121:62–5.
Hirsch BE. Staging system revision. Arch Otolaryngol Head Neck Surg. 2002;128:93–4.
Jereczek-Fossa B, Zarowski A, Milani F, et al. Radiotherapy-induced ear toxicity. Cancer Treat Rev. 2003;29:417–30.
Lin R, Hug E, Schaefer R, et al. Conformal proton radiation therapy of the posterior fossa: a study comparing protons with three-dimensional planned photons in limiting dose to auditory structures. IJROBP. 2000;48:1219–26.
Osborne R, Shaw T, Zandifar H, et al. Elective parotidectomy in the management of advanced auricular malignancies. Laryngoscope. 2008;118:2139–45.
Madsen A, Gundgaard M, Hoff C, et al. Cancer of the external auditory canal and middle ear in Denmark from 1992 to 2001. Head Neck. 2008;30:1332–8.
Nakagawa T, Kumamoto Y, Natori Y, et al. Squamous cell carcinoma of the external auditory canal and middle ear: an operation combined with preoperative chemoradiotherapy and a free surgical margin. Otol Neurotol. 2006;27:242–8.
Ogawa K, Nakamura K, Hatano K, et al. Treatment and prognosis of squamous cell carcinoma of the external auditory canal and middle ear: a multi-institutional retrospective review of 87 patients. Int J Radiat Oncol Biol Phys. 2007;68(5):1326–34.
Pacholke HD, Amdur RJ, Schmalfuss IM, et al. Contouring the middle and inner ear on radiotherapy planning scans. Am J Clin Oncol. 2005;28(2):143–7.
Pfreundner L, Schwager K, Willner J, et al. Carcinoma of the external auditory canal and middle ear. Int J Radiat Oncol Biol Phys. 1999;44:777–88.
Wang TJC, Chao KSC. Ear. In: Perez CA, Wazer DE, Brady LW, Halperin EC, et al., editors. Principles and practice of radiation oncology. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2013. p. 711–7.
Yin M, Ishikawa K, Honda K, et al. Analysis of 95 cases of squamous cell carcinoma of the external and middle ear. Auris Nasus Larynx. 2006;33(3):251–7.
Acknowledgment
We thank Fred Y. Wu MD, PhD, and Eric K. Hansen MD for their work on the prior edition of this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Chan, J., Yom, S.S. (2018). Cancer of the Ear. In: Hansen, E., Roach III, M. (eds) Handbook of Evidence-Based Radiation Oncology. Springer, Cham. https://doi.org/10.1007/978-3-319-62642-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-62642-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62641-3
Online ISBN: 978-3-319-62642-0
eBook Packages: MedicineMedicine (R0)