Abstract
Background: Distraction of the C1–C2 joint and maintenance thereof by introduction of spacers into the articular cavity can successfully and durably reduce basilar invagination (BI). Thus, with the adjunct of instrumented fusion and decompression, BI-induced myelopathy can be efficiently treated with a one-stage posterior approach. This intervention is technically challenging, and in this paper we describe a procedural variation to facilitate the approach.
Methods and Results: Through a description of a case of BI, the main anatomopathological alteration underlying and perpetrating the condition of BI is elucidated. A technique of realignment of BI is then described in which this alteration is specifically targeted and neutralized. The result is a single-stage posterior-only approach with decompression, C1–C2 distraction and introduction of poly(methyl methacrylate) (PMMA) into the joint cavity. Instrumented occipitocervical fusion completes the procedure.
Conclusion: C1–C2 joint distraction is a technically demanding procedure. By providing a modification of the original technique and a detailed description of the crucial steps necessary to successfully and safely carry it out, we hope to make this excellent procedure more approachable.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Atlantoaxial joint distraction and direct lateral mass fixation to treat basilar invagination (BI), as described by Goel in 2004 [1], has represented a true paradigm shift in the approach to a complex structural problem. In symptomatic BI, a condition in which myelopathy is essentially caused by an odontoid process that encroaches upward and posteriorly on the spinal cord, that same odontoid process has classically—and quite rightly—been seen as the main culprit [2, 3]. If the odontoid process was extending too far into the foramen magnum and impinging on the spinal cord, it was in a place where it was not supposed to be, and it was therefore ‘at fault’, so to speak.
As a consequence the transoral approach was adopted and subsequently refined to efficiently eliminate the culprit by excising the odontoid process and thus relieving pressure on the cord [4,5,6,7,8,9,10].
While this technique definitely remains valid and is still the procedure most widely used for symptomatic BI today, Goel’s discovery was truly revolutionary, as it ‘saved the messenger’. According to this vision of things, the odontoid process was no longer the culprit, even though it effectively impinged on the cord; rather, it was ‘the messenger carrying the bad news’ of an aberrant process that resided somewhere else. As a matter of fact, in BI it is not the dens that is malformed; rather, it is its adjoining structures that put it in the wrong place.
BI generally entails a varying combination of platybasia, assimilation of the atlas, atlantoaxial dislocation (AAD) and/or anterocaudal inclination of the C1–C2 articular surfaces, leading to the atlanto-occipital complex ‘sliding’ anteroinferiorly with respect to the axis and thus, in turn, causing the axis and dens to migrate upward and backward.
It is the identification and definition of these corollary—or, rather, causative—features that has led over the last two decades to a refined classification of BI that draws attention away from the odontoid impinging on the cord as the end product of the pathological process and, instead, elucidates the fundamental role of C1–C2 facet conformation and disposition as the root cause of the problem and therefore also the essential aim of reparative intervention [11].
While a detailed explanation of the classification of C1–C2 facetal anomalies clearly transcends the purpose of this paper, we attempt to outline the basic principles of the anomaly and its direct repair with the help of the following case description.
Case Report and Technical Note
A 56-year-old woman with an uneventful past medical history was referred to our department for worsening myelopathy and pain in the nape of the neck. On neurological examination she scored IIIA on the Ranawat scale for myelopathy [5].
She underwent cervical magnetic resonance imaging (MRI), which showed that the spinal cord was severely compressed at the level of the craniovertebral junction. Furthermore, the cord showed signs of hyperintensity on T2-weighted images and initial cavitation (Fig. 1). To better identify the nature of the compression, a computed tomography (CT) scan was done, which showed assimilation of the atlas (AA) with BI and AAD. As a result, the odontoid peg was protruding into the foramen magnum (Fig. 2a, c).
(a) Sagittal T2 magnetic resonance imaging (MRI) scan showing the craniocervical region with basilar invagination (BI), severe compression of the spinal cord, intramedullary changes of oedema and initial syrinx formation. (b) Sagittal computed tomography (CT) scan showing BI with atlantoaxial dislocation (AAD) and clear upward migration of the odontoid process. Note the position of the dens traversing Chamberlain’s line (white). (Reprinted from Cacciola et al. [12], with permission)
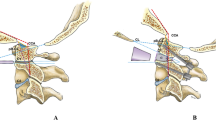
(a) Prone position of the patient with the head in traction and resting on a horseshoe headholder. (Reprinted from Goel and Laheri, with permission.) (b) Positioning of a laminar spreader between the occiput and the C2 lamina with ensuing opening of the C1–C2 joint space. (c) Introduction of small poly(methyl methacrylate) (PMMA) spheres into the opened joint space with a dissector. (Reprinted from Cacciola et al. [12], with permission)
The patient was thus scheduled for posterior-only surgery in the prone position. Transcranial traction of 16 pounds was applied with the head supported by a horseshoe headrest and the table inclined to roughly 30° anti-Trendelenburg (Fig. 3a).
(a) Sagittal computed tomography (CT) scan centred on the C1–C2 joint postoperatively. Note the oblique inclination of the joint and the filling of the distracted joint with hyperdense material [poly(methyl methacrylate) (PMMA)] to an opening of 5 mm. (b) Coronal CT scan through the C1–C2 joints bilaterally. Note the distracted joints and PMMA in the cavities. (c) Lateral cervical radiograph showing the instrumented fusion. (Reprinted from Cacciola et al. [12], with permission)
After a vertical incision was made, centring on C1–C2, the posterior arch of the atlas and the laminae and spinous process of C2 were exposed. Subsequent dissection was carried out laterally to identify and section both C2 ganglions to provide good exposure of both C1–C2 joints. During this stage the perivertebral venous plexus can often bleed significantly, and this can be made even worse by small emissaries of the vertebral artery. The surgeon should be prepared for this and, through sound knowledge of the anatomy, not be withheld by such bleeding, as this can sometimes be so copious as to lead to the misbelief that the vertebral artery itself may have been injured.
Once the joints were exposed, a small osteotome was introduced into the joint spaces and rotated to achieve some distraction and mobilization of the joint complex. Subsequently, a cervical laminar spreader was inserted between the occiput and the superior rim of the C2 laminae to distract the joint space in a controlled fashion and keep it distracted at first on the right side (Fig. 3b).
Once the joint was distracted, poly(methyl methacrylate) (PMMA) was made in a standard fashion and stirred until it reached a semi-solid state, just enough to allow for the making of small pea-sized spheres. These were then introduced into the joint with a dissector until the cavity was felt to be sufficiently filled with cement (Fig. 3c). Once the cement had turned solid, the laminar spreader was taken off and put into place on the contralateral joint, and the operation was performed in the same fashion on the left side. Following that, the foramen magnum was decompressed in a standard fashion, and instrumented C0–C3 fusion was performed with integration of an autologous tricortical bone graft harvested from the posterior iliac crest, which was placed under compression between the occiput and the superior border of the C2 spinolaminar complex.
The patient was discharged with a hard collar and, at 1-month follow-up, showed a neurological improvement of one grade (to II) on the Ranawat scale.
At that stage a CT scan was done, which showed a clear realignment of the odontoid process moving below Wackenheim’s line, thus normalizing and essentially reversing the condition of BI (Fig. 2b). The AAD showed marked reduction as well.
Follow-up at 6 months confirmed maintenance of the clinical improvement, and imaging studies showed persistence of the realignment.
Discussion
Goel’s posterior-only C1–C2 distraction and fusion technique has revolutionized the treatment of BI, with the potential to relegate the need for a transoral approach to a more restricted selection of cases. The rationale for this technique lies in the fact that the origin of the problem, or the ‘culprit’, is the conformation of the atlantoaxial joints. Being generally inclined in an oblique direction, mostly in the anteroinferior direction (Fig. 3b), the occipitoatlantal complex slides forward, thus causing AAD and BI. Therefore, careful attention should always be given to the joint complex when facing a case of BI as, if these findings are present, the whole pathology can be corrected with a posterior-only distraction operation, as depicted in our case.
In the original technical description, intraoperative distraction of the joint (besides the head traction) is achieved by insertion of small osteotomes inside the joint and rotation of the same so as to open the joint. Titanium spacers are then impacted into the joint. The spacers have a bullet-shaped nose, and that edge is abutted at the entrance of the joint cavity. Then, with the help of a mallet and an impactor, they are made to advance into the joint cavity, similarly to the insertion of a cage into the lumbar disc space during posterior lateral interbody fusion (PLIF). As these manoeuvres might appear challenging to the first-time user of this technique, given both unfamiliarity with the anatomical region and the proximity of the vertebral artery on one side and the spinal cord on the other, we have introduced a variation into these two steps. With the use of a laminar spreader, the joint spaces are distracted gradually and in a controlled fashion. Then, once the joint cavity is open, the small spheres of semi-cured PMMA can be inserted into the cavity with the help of a dissector, without the need to exert any force on the structures. Once the PMMA has reached the solid state inside the joint cavity, the spreaders are taken off and the distraction is thus maintained.
Conclusion
C1–C2 distraction has proven to be a reliable technique in the treatment of basilar invagination. Considering the relatively low overall incidence of this pathology, many surgeons lack sufficient exposure to gain experience in the transoral approach, which is classically the mainstay of treatment for this condition. Even though it is still technically demanding, the joint distraction technique could prove to be more approachable by a spinal surgeon who is mainly confident with posterior approaches, and our technical modification might further facilitate the endeavour.
References
Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1(3):281–6.
Chamberlain WE. Basilar impression (platybasia): a bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med. 1939;11:487–96.
von Torklus D, Gehle W. The upper cervical spine: regional anatomy, pathology and traumatology. In: A systematic radiological atlas and textbook. New York: Grune & Stratton; 1972. p. 1–98.
Balasingam V, Anderson GJ, Gross ND, Cheng CM, Noguchi A, Dogan A, McMenomey SO, Delashaw JB Jr, Andersen PE. Anatomical analysis of transoral surgical approaches to the clivus. J Neurosurg. 2006;105:301–8.
Choi D, Crockard HA. Evolution of transoral surgery: three decades of change in patients, pathologies, and indications. Neurosurgery. 2013;73:296–304.
Crockard HA, Johnston F. Development of transoral approaches to lesions of the skull base and craniocervical junction. Neurosurg Q. 1993;3(2):61–82.
Dickman CA, Locantro J, Fessler RG. The influence of odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992;77:525–30.
Di Lorenzo N, Fortuna A, Guidetti B. Craniovertebral junction malformations. Clinicoradiological findings, long-term results and surgical indications in 63 cases. J Neurosurg. 1982;57:603–8.
Di Lorenzo N. Transoral approach to extradural lesions of the lower clivus and upper cervical spine: an experience of 19 cases. Neurosurgery. 1989;24:37–42.
Di Lorenzo N. Craniocervical junction malformation treated by transoral approach. A survey of 25 cases with emphasis on postoperative instability and outcome. Acta Neurochir. 1992;118:112–6.
Goel A. Craniovertebral junction instability: a review of facts about facets. Asian Spine J. 2015;9:636–44.
Cacciola F, Patel V, Boszczyk BM. Novel use of bone cement to aid atlanto-axial distraction in the treatment of basilar invagination: a case report and technical note. Clin Neurol Neurosurg. 2013;115:787–9.
Competing Interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Ethics declarations
No financial support was received for this work.
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Cacciola, F., Boszczyk, B., Perrini, P., Gallina, P., Di Lorenzo, N. (2019). Realignment of Basilar Invagination by C1–C2 Joint Distraction: A Modified Approach to a Paradigm Shift. In: Visocchi, M. (eds) New Trends in Craniovertebral Junction Surgery. Acta Neurochirurgica Supplement, vol 125. Springer, Cham. https://doi.org/10.1007/978-3-319-62515-7_39
Download citation
DOI: https://doi.org/10.1007/978-3-319-62515-7_39
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62514-0
Online ISBN: 978-3-319-62515-7
eBook Packages: MedicineMedicine (R0)