Abstract
Essential thrombocythemia (ET) is a myeloproliferative neoplasm characterized by elevated peripheral blood platelet count and bone marrow megakaryocyte hyperplasia. Three driver mutations in JAK2, CALR, and MPL have been identified and result in these clinical findings via activation of the JAK/STAT pathway. These mutations are included in the diagnostic criteria for ET. Here, we not only focus on the molecular aspects of ET but also discuss the morphological, immunophenotypic, and clinical features of this disease.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Essential thrombocythemia (ET) is classified as a chronic myeloproliferative neoplasm (MPN ) involving the megakaryocytic lineage [1]. It was first described by Austrian pathologists, Epstein and Goedel, in 1934 [2], and the definition has evolved over the years. By the most recent diagnostic criteria (Table 7.1), ET is characterized by thrombocytosis ≥450 × 109/L in the peripheral blood; a bone marrow showing increased numbers of enlarged, mature megakaryocytes with hyperlobulated nuclei; no fibrosis or rare grade 1 reticulin fibrosis; exclusion of other myeloid neoplasms; and the presence of mutations involving Janus kinase 2 (JAK2), calreticulin (CALR), or thrombopoietin receptor, also known as myeloproliferative leukemia virus oncogene (MPL) [3].
Epidemiology
The overall age-adjusted incidence rate for ET is 9.6 per one million persons per year. Differences are seen in incidence rates for Blacks (11.5), Caucasians (9.7), and Hispanics (6.4). The median age at diagnosis is 68 years. ET is rarely seen in children, and incidence rates increase exponentially with increasing age. There is a female predilection, with a M:F ratio of 0.8:1, most prominent in women <60 years of age [4].
Clinical Features
Up to 50% of patients can be asymptomatic at time of diagnosis, while others may present with vasomotor symptoms, thrombosis, or hemorrhage. Common patient complaints include difficulty sleeping, abdominal discomfort, dizziness/vertigo/lightheadedness, sweats, numbness/tingling in hands/feet and less commonly pruritus, bruising, and fatigue [5].
Morphology
The 2016 World Health Organization (WHO) diagnostic criteria for ET have been updated to include the mutation status of CALR and MPL (in addition to JAK2, included in the 2008 classification), while the morphological criteria have remained essentially the same.
While morphology has always been an indispensable component of the diagnoses of MPNs, the new criteria emphasize the importance of distinguishing prefibrotic/early primary myelofibrosis (pre-PMF) from ET. Absence of fibrosis or only minimal fibrosis (grade 1) is acceptable for a diagnosis of ET. Although this was implied by the 2008 exclusion criteria for PMF and stated in the footnote, the degree of allowable fibrosis is now directly stated under the major criteria heading of the 2016 classification [3]. This distinction is important clinically, as true patients with ET can survive up to 7 years longer than those with pre-PMF [6]. Pre-PMF has a significantly worse prognosis than ET [6,7,8]. Compared with pre-PMF, patients with true ET have a lower risk of progression to acute leukemia and high-grade fibrosis, superior overall survival, and higher risk of bleeding complications [7].
Peripheral Blood
The major finding in the peripheral blood is marked thrombocytosis. Platelets can vary in size and shape with occasional bizarre forms. The white blood cell count and differential are typically within normal limits, although they may be borderline high. Red blood cells are typically normochromic, normocytic [1].
Bone Marrow
The bone marrow biopsy is normocellular or shows only a slight increase in age-matched cellularity (Fig. 7.1). Only the megakaryocytic lineage shows increased proliferation. Megakaryocytes are enlarged and increased in number, with mature morphology and hyperlobulated nuclei (staghorn appearance) (Fig. 7.2). Neutrophil granulopoiesis and erythropoiesis are not significantly increased or left shifted. Reticulin fibrosis is absent, or very rarely there is minor (grade 1) increase in reticulin fibers [3, 6, 9] (Fig. 7.3). When differentiating ET from pre-PMF, it is important to note that ET lacks marrow hypercellularity, granulocytic proliferation, significant megakaryocyte clustering, and cloud-like or hyperchromatic megakaryocytes (Fig. 7.4).
Diagnostic criteria of distinctive value regarding WHO-defined ET (left) versus early-prefibrotic stage of PMF (right), including standardized morphological features (see Table 7.1 for more details), allowing the generation of characteristic histological bone marrow patterns (Used with permission from Thiele et al. [6])
Molecular Features
Research efforts in the last 10 years have resulted in a much better understanding of the molecular pathogenesis of ET and other BCR/ABL1-negative MPNs. Cytogenetic abnormalities occur in less than 5% of ET, and no specific recurrent abnormalities have been documented. In contrast, approximately 90% of ET cases carry driver mutations in one of three genes.
Three main driver mutations have now been well characterized in terms of their incidence and clinical effects. JAK2 is the most commonly mutated gene in MPNs , followed by CALR and MPL. These driver mutations ultimately result in overproduction of one or more cell lineages. All three driver mutations activate the Janus kinase 2/signal transducer and activator of transcription (JAK/STAT) signaling pathway. In the case of JAK2 and MPL mutations , the mechanisms of action involve constitutive activation of their mutated counterparts, while mutated CALR has been shown to activate the thrombopoietin receptor, MPL [10]. JAK2 mutation status was included in the 2008 WHO criteria for a diagnosis. In addition to JAK2, the 2016 classification includes mutation status of MPL and CALR. The clinical features of ET are influenced by which gene is mutated, as discussed further below (Table 7.2).
The first recurrent mutation identified in all three BCR/ABL-negative MPNs was JAK2 V617F, discovered in 2005 by four groups [11,12,13,14]. About 50–60% of ET cases harbor a JAK2 V617F mutation [15]. JAK2 is a protein tyrosine kinase. In normal megakaryocytes , binding of thrombopoietin to the thrombopoietin receptor results in JAK2 autophosphorylation, recruitment of STAT, and phosphorylation of STAT. The phosphorylated STAT dimerizes and moves to the nucleus, where it activates transcription of genes resulting in proliferation of platelets. The JAK2 V617F mutation deactivates the repressor pseudokinase domain of JAK2, resulting in activation of JAK2 and downstream signaling pathways in the absence of the appropriate activating ligand.
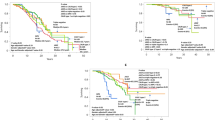
The percentage of cells with the JAK2 V617F mutation , or allele burden , affects the clinical features of the disease. Cells homozygous for JAK2 V617F mutation also contribute to a higher allele burden. Low JAK2 V617F allele burden is typically seen in ET and pre-PMF, with intermediate levels in polycythemia vera (PV), high levels in fibrotic PMF, and very high levels seen in post-PV MF. The percentage ofJAK2 V617F homozygous granulocytes is also higher in PV and PMF than in ET [16]. Some MPN experts suggest that ET and PV may be different stages of the same disease, with ET representing early, low allelic burden disease, and PV and PMF representing a higher allelic burden later in the disease course (Fig. 7.5) [17]. Recent studies suggest a diagnosis of true ET is unusual in patients with a JAK2 V617F allele burden over 50% [18]. Increased JAK2 V617F allele burden in ET is associated with increased splenomegaly, microvessel disease, higher leukocyte count, and history of thrombosis [19, 20]. Although less than 5% of patients with ET are homozygous for JAK2 V617F, homozygosity also shows correlation with clinical features. Patients with ET homozygous for JAK2 V617F are more likely than heterozygotes to have splenomegaly (73% vs 28%), cardiovascular events (43% vs 12%), and progression to myelofibrosis (14% vs 5%) [21].
Schematic representation of JAK2 (V617F) allele burden (middle panel) and its relationship with clinical phenotype (bottom panel), and disease complications (top panel). At low levels of mutant allele, the clinical phenotype is dominated by thrombocytosis, at intermediate levels by erythrocytosis, and at higher levels by leukocytosis. Among complications, current evidence indicates a relationship between allele burden and evolution into myelofibrosis (Used with permission from Passamonti et al. [17])
The second most commonly mutated gene in ET is calreticulin ( CALR ) . In 2013, two groups discovered CALR mutations in the majority of patients with JAK2-negative ET [22, 23]. About 20–25% of ET cases have CALR mutations [15]. CALR normally acts as a protein chaperone that helps newly synthesized proteins fold properly in the endoplasmic reticulum (ER) . CALR is also a calcium ion (Ca2+) transporter that regulates Ca2+ levels between the ER and the cytoplasm of cells. The carboxy end of CALR is enriched in negatively charged amino acids that promote binding of Ca2+. The carboxy terminal also has a four amino acid sequence – lysine, aspartic acid, glutamic acid, leucine (KDEL) – that acts as a signal for CALR to be retained in the ER. CALR mutations include more than 50 different insertions and deletions (indels). These indels result in altered charge of the carboxy end of the CALR protein, which is the primary calcium-binding domain. The two most common CALR mutations are classified as type 1 (a 52 base pair deletion in exon 19) and type 2 (a 5 base pair insertion in exon 19). Type 1 CALR mutation is seen in approximately 50% of CALR-mutated ET cases, while type 2 is seen in approximately 30%. Type 1-like mutations result in a loss of the majority of the negatively charged amino acids in the calcium-binding region of CALR, and type 2-like mutations result in loss of approximately half the positively charged amino acids in this region. A third group, seen in approximately 10% of cases, includes indels that are typically classified as type 1-like and type 2-like based on the expected change in charge of the mutated CALR carboxy terminus [24].
Compared with JAK2 V617F-positive ET, CALR-mutated patients with ET present at a younger age and have a lower risk of thrombosis and higher platelet counts [25]. Within the group of CALR-mutated cases, type 1 mutations are more frequently associated with features of PMF at presentation than type 2 mutated cases. ET type 1 mutated cases have a higher risk of progression to post-ET MF than type 2 mutated cases. In contrast, patients with type 2 CALR mutations more frequently have features of ET at presentation as well as very high platelet counts and lower risk for thrombosis [24]. Increased CALR mutant allele burden has been demonstrated in post-ET MF [26].
Approximately 3–5% of ET cases have MPL mutations involving exon 515. These include W515L, W515K, W515A, W515S, and W515R [27]. These mutations result in constitutive activation of the JAK-STAT pathway via the thrombopoietin receptor encoded by MPL, as well as increased sensitivity of the receptor to thrombopoietin. MPL-mutated patients with ET tend to be older and have a higher rate of progression to fibrosis and acute myeloid leukemia (AML) .
Approximately 10% of MPNs have none of the three main driver mutations and are referred to as triple-negative MPNs. A small subset of these “triple-negative” cases has been shown to have novel mutations in JAK2 or MPL. The remaining cases have as yet unidentified abnormalities or rare mutations. Whole exome sequencing of triple-negative ET cases in one study uncovered the following mutations : JAK2 G571S (germline), ITGAV R333H, WBSCR28 A201T, and loss of chromosome 4q [27]. Lymphocyte-specific adapter protein (LNK) also known as src homology 2B3SH2B adapter protein 3 (SH2B3) is mutated in rare cases of ET [28].
In addition to driver mutations, many patients with ET harbor mutations in other genes involved in epigenetic modification, RNA splicing, and cell signaling pathways (Table 7.3). Data regarding the frequency of these nondriver mutations in ET specifically are difficult to extract from the literature due to the inclusion of mixed cases of MPNs and small numbers of cases in most series; however, in one study including 69 patients with ET, 62% had only a single driver mutation, 22% had one additional mutation, and 3% had two additional mutations. The most commonly mutated nondriver genes in ET were DNMT3A, TET2, and TP53 [29]. TET2 was reported to occur in approximately 5% of ET in one study [30]. In another study, 15% of patients with ET had TET2 mutations, 12.5% had ASXL1 mutations, and less than 1% of patients had mutations in SRSF2, SF3B1, IDH1, IDH2 or GATA1 [31]. Single ET cases had mutations involving each of the following genes: ASXL1, EXH2, CUX1, PIK3R2, SH2B3, and del7q [29].
The order of acquisition of gene mutations also affects the clinical features of disease. Calreticulin mutations generally occur before other mutations. JAK2-positive cases may have mutations in TET2 and/or DNMT3A that generally occur before JAK2 V617F [29].
Cases in which TET2 or DNMT3A mutations occur before JAK2 mutations are more frequently associated with clinical features of ET, while cases carrying one of these mutations with JAK2 mutated first are reportedly more frequently associated with features of PV [25].
Finally, host factors may also predispose patients to ET. Several single nucleotide polymorphisms (SNPs) have been shown to be associated with increased risk of developing MPNs. Compared with other SNPs, the 46/1 haplotype of JAK2, found in approximately 50% of healthy Caucasians, carries three to four times the risk of developing a MPN, not only mutated JAK2 but also wild-type JAK2 [32, 33]. The risk of ET in first-order relatives of 46/1 JAK2 patients with ET is increased 12 times [33]. Other less common JAK2 SNPs have also been associated with increased risk for ET [34]. Additional genes with SNPs associated with increased risk of ET and other Ph-negative MPNs include telomerase reverse transcriptase (TERT), TET2, and SH2B adapter protein 3 (SH2B3), also known as LNK, HBS1L/MYB, and MECOM [35, 36].
Prognosis and Therapy
Prognosis in ET is determined by multiple clinical factors, including patient’s age, hematologic parameters, mutation status, and type of previous therapy. The international prognostic score for essential thrombocythemia (IPSET-thrombosis) is the current standard for risk stratification in patients with ET and is based on age, history of thrombosis, and JAK2 V617F mutation status [37–39]. In this model, patients’ risk of thrombosis is stratified as follows: very low = age ≤ 60, JAK2-negative, no prior thrombosis; low = age ≤ 60, JAK2-positive, no prior thrombosis; intermediate = age > 60, JAK2-negative, no prior thrombosis; and high = prior thrombosis or age > 60 and JAK2-positive. The model predicts the risk of vascular events in patients with ET, ranging from very low risk, 0.44% patients per year, to high risk, 4.17% patients per year.
The rates of overall survival and disease progression vary in different studies, most likely due to data collected in studies including a mixed population of patients diagnosed as ET that include pre-PMF patients. When taken as a pure population, patients with ET have rates of progression to post-ET MF of less than 1% at 5 and 10 years and approximately 9% at 15 years. The rate of progression of ET to AML is less than 1% at 5 and 10 years and approximately 2% at 20 years. Death rates are approximately 3% at 5 years, 5% at 10 years, and 25% at 15 years [11].
Risk factors for progression of ET to MF include older age, anemia, and absence of JAK2 V6178F. Risk factors for progression of ET to AML include history of thrombosis and extreme thrombocytosis. Risk factors for death include older age, leukocytosis greater than 11 × 109/L, hemoglobin less than 12 g/dL, and history of thrombosis [11].
As described above, there are differences in the clinical features of ET based on the driver mutation causing the disease. Some molecular features have also been found to be correlated with prognosis . Overall survival is similar in JAK2-mutated and CALR-mutated cases, but is inferior in patients with MPL mutations and better in triple-negative cases [39]. However, patients with MPL mutations are older at presentation, accounting for the poor survival in that group [39]. Of the common nondriver mutations, SRSF2 is associated with inferior survival in post-ET MF, whereas EZH2, ASXL1, IDH1, an IDH2 mutations had no effect on survival [26]. Mutations in TP53 are often seen at the time of leukemic transformation [40].
Treatment is primarily directed toward lowering the platelet count and decreasing the risk of thrombosis and bleeding complications. Treatment is tailored to each patient’s risk profile. Patients are classified as high risk or low risk based on age and history of thrombosis. High-risk patients are those 60 years of age and older and/or those with a history of thrombosis. Low-risk patients are those under 60 with no history thrombosis. Secondary risk factors that may also be considered when selecting a treatment regimen are JAK2 V617 status and the presence or absence of cardiovascular risk factors (diabetes, hypertension, and smoking history). The presence of either or both of these risk factors is associated with increased risk of thrombosis and may indicate a need for more aggressive therapy [41].
First-line therapy for all patients with ET is once-daily, low-dose aspirin unless contraindicated. In addition, cytoreductive treatment is recommended for patients 60 years and older and for patients with a history of arterial thrombosis with JAK2 V617 positivity and/or the presence of cardiovascular risk factors. Patients with a history of venous thrombosis may receive systemic anticoagulation in addition to cytoreductive therapy and aspirin.
Cytoreductive agents frequently used to treat ET include hydroxyurea (HU), anagrelide, and pegylated interferon alpha-2a (PEG-IFNα-2a). HU is the frontline cytoreductive drug most often used. HU treatment has been shown to decrease platelet counts and risk of thrombosis.
PEG-IFNα-2a or anagrelide may be used in patients who do not tolerate HU. Long-term IFNα treatment has been shown to induce complete hematologic remission in 77% of patients with ET and complete molecular remission in 17% of patients with ET. In one study, the efficacy of PEG-IFNα-2a to achieve a complete molecular response was found to be influenced by the presence of somatic mutations in addition to JAK2 (CALR status was unknown at the time of the study). In particular, patients with TET2 mutations showed a smaller decrease in JAK2 allele burden with treatment and a lower rate of complete molecular response [42]. PEG-IFNα-2a may also be effective in treating CALR-positive ET. Complete long-term hematologic remission was documented in two patients with CALR-positive ET. At the time of the report, these patients had been in remission for 18 months and over 5 years, respectively, after discontinuation IFNα [43].
Anagrelide, a drug that inhibits maturation of megakaryocytes into platelets, has also been used as a cytoreductive treatment in patients with ET who cannot tolerate or are resistant to HU. This drug has been associated with a greater incidence of thrombotic events and a higher incidence of transformation to acute leukemia compared with HU in one study [44], but with no adverse effects relative to HU in another study [45].
Although the Janus kinase inhibitors including ruxolitinib have been used to treat PV and PMF, there are few studies documenting Janus kinase inhibitor treatment in ET. In one study, ruxolitinib decreased platelet and leukocyte counts, reduced spleen size, and improved disease-related symptoms in patients with ET [46].
Conclusion
While morphological criteria for the diagnosis of ET have changed little, our understanding of the molecular underpinnings of this disease have progressed greatly in recent years. The updated 2016 WHO morphological diagnostic criteria remain similar to the 2008 classification, with emphasis on the distinction of ET from pre-PMF based on morphological and laboratory values [3].
In contrast, the molecular diagnostic WHO criteria now incorporate mutation status of CALR and MPL, in addition to the previously known driver mutations in JAK2. Clinical features including age at presentation, cell counts, propensity for thrombosis, and risk of progression to more aggressive disease are influenced by molecular features, including which gene is mutated, the structure of the mutated protein, and in some cases by the mutant allele burden. Furthermore, nondriver mutations and the order in which they are acquired relative to driver mutations also have clinical correlates.
With greater understanding of these molecular features, the future holds great potential for expanding targeted therapy for ET and other MPNs beyond Janus kinase inhibitors.
References
Thiel J, Kvasnicka HM, Orazi A, et al. Essential thrombocythaemia. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC; 2008. p. 48–50.
Epstein E, Goedel A. Hamorrhagischethrombo-zythamiebeivascularerschrumpfmilz (hemorrhagic thrombocythemia with a vascular, sclerotic spleen). Virchows Arch A Pathol Anat Histopathol. 1934;293:233–48.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. doi:10.1182/blood-2016-03-643544.
Srour SA, Devesa SS, Morton LM, et al. Incidence and patient survival of myeloproliferative neoplasms and myelodysplastic/myeloproliferative neoplasms in the united states, 2001–12. Br J Haematol. 2016;174(3):382–96. doi:10.1111/bjh.14061.
Mesa RA, Miller CB, Thyne M, et al. Differences in treatment goals and perception of symptom burden between patients with myeloproliferative neoplasms (MPNs) and hematologists/oncologists in the United States: findings from the MPN landmark survey. Cancer. 2016. doi:10.1002/cncr.30325.
Thiele J, Kvasnicka HM, Mullauer L, et al. Essential thrombocythemia versus early primary myelofibrosis: a multicenter study to validate the WHO classification. Blood. 2011;117(21):5710–8. doi:10.1182/blood-2010-07-293761.
Barbui T, Thiele J, Passamonti F, et al. Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: an international study. J Clin Oncol. 2011;29(23):3179–84. doi:10.1200/JCO.2010.34.5298.
Gisslinger H, Jeryczynski G, Gisslinger B, et al. Clinical impact of bone marrow morphology for the diagnosis of essential thrombocythemia: comparison between the BCSH and the WHO criteria. Leukemia. 2016;30(5):1126–32. doi:10.1038/leu.2015.360.
Gianelli U, Vener C, Bossi A, et al. The European consensus on grading of bone marrow fibrosis allows a better prognostication of patients with primary myelofibrosis. Mod Pathol Off J US Can Acad Pathol Inc. 2012;25(9):1193–202. doi:10.1038/modpathol.2012.87.
Chachoua I, Pecquet C, El-Khoury M, et al. Thrombopoietin receptor activation by myeloproliferative neoplasm associated calreticulin mutants. Blood. 2016;127:1325–35. doi:10.1182/blood-2015-11-681932.
Baxter EJ, Scott LM, Campbell PJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054–61. doi:10.1016/S0140-6736(05)71142-9.
James C, Ugo V, Le Couedic J-P, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144–8. doi:10.1038/nature03546.
Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352(17):1779–90. doi:10.1056/NEJMoa051113.
Levine RL, Wadleigh M, Cools J, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;4:387–97. doi:10.1016/j.ccr.2005.03.023.
Barbui T, Thiele J, Vannucchi AM, et al. Rationale for revision and proposed changes of the WHO diagnostic criteria for polycythemia vera, essential thrombocythemia and primary myelofibrosis. Blood Cancer J. 2015;5(8):e337. doi:10.1038/bcj.2015.64.
Scott LM, Scott MA, Campbell PJ, et al. Progenitors homozygous for the V617F mutation occur in most patients with polycythemia vera, but not essential thrombocythemia. Blood. 2006;108:2435–7. doi:10.1182/blood-2006-04-018259.
Passamonti F, Rumi E, Daniela P, et al. Relation between JAK2 (V617F) mutation status, granulocyte activation, and constitutive mobilization of CD34+ cells into peripheral blood in myeloproliferative disorders. Blood. 2006;107:3676–82. doi:10.1182/blood-2005-09-3826.
Hussein K, Bock O, Theophile K, von Neuhoff N, et al. JAK2(V617F) allele burden discriminates essential thrombocythemia from a subset of prefibrotic-stage primary myelofibrosis. Exp Hematol. 2009;37(10):1186–1193.e7. doi:10.1016/j.exphem.2009.07.005.
Antonioli E, Guglielmelli P, Poli G, et al. Influence of JAK2V617F allele burden on phenotype in essential thrombocythemia. Haematologica. 2008;93(1):41–8. doi:10.3324/haematol.11653.
Tefferi A, Strand JJ, Lasho TL, et al. Bone marrow JAK2V617F allele burden and clinical correlates in polycythemia vera. Leukemia. 2007;21(9):2074–5.
Vannucchi AM, Antonioli E, Guglielmelli P, et al. Clinical profile of homozygous JAK2 617V>F mutation in patients with polycythemia vera or essential thrombocythemia. Blood. 2007;110(3):840–6. doi:10.1182/blood-2006-12-064287.
Nangalia J, Massie CE, Baxter EJ, et al. Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. NEJM. 2013;369(25):2391–405. doi:10.1056/NEJMoa1312542.
Klampfl T, Gisslinger H, Harutyunyan AS, et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013;369(25):2379–90. doi:10.1056/NEJMoa1311347.
Pietra D, Rumi E, Ferretti VV, Di Buduo CA, et al. Differential clinical effects of different mutations subtypes in CALR-mutant myeloproliferative neoplasms. Leukemia. 2016;30(2):431–8. doi:10.1038/leu.2015.277.
Palandri F, Latagliata R, Polverelli N, et al. Mutations and long-term outcome of 217 young patients with essential thrombocythemia or early primary myelofibrosis. Leukemia. 2015;29(6):1344–9. doi:10.1038/leu.2015.87.
Rotunno G, Pacilli A, Artusi V, et al. Epidemiology and clinical relevance of mutations in postpolycythemia vera and postessential thrombocythemia myelofibrosis: a study on 359 patients of the AGIMM group. Am J Hematol. 2016;91(7):681–6. doi:10.1002/ajh.24377.
Milosevic Feenstra JD, Nivarthi H, Gisslinger H, et al. Whole-exome sequencing identifies novel MPL and JAK2 mutations in triple-negative myeloproliferative neoplasms. Blood. 2016;127(3):325–32. doi:10.1182/blood-2015-07-661835.
ST O, Simonds EF, Jones C, et al. Novel mutations in the inhibitory adaptor protein LNK drive JAK-STAT signaling in patients with myeloproliferative neoplasms. Blood. 2010;116:988–92. doi:10.1182/blood-2010-02-270108.
Lundberg P, Karow A, Nienhold R, et al. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood. 2014;123(14):2220–8. doi:10.1182/blood-2013-11-537167.
Tefferi A, Pardanani A, Lim KH, et al. TET2 mutations and their clinical correlates in polycythemia vera, essential thrombocythemia and myelofibrosis. Leukemia. 2009;23(5):905–11. doi:10.1038/leu.2009.47.
Delic S, Rose D, Kern W, et al. Application of an NGS-based 28-gene panel in myeloproliferative neoplasms reveals distinct mutation patterns in essential thrombocythaemia, primary myelofibrosis and polycythaemia vera. Br J Haematol. 2016. doi:10.1111/bjh.14269.
Landgren O, Goldin L, Kristinsson S, et al. Increased risks of polycythemia vera, essential thrombocythemia, and myelofibrosis among 24,577 first-degree relatives of 11,039 patients with myeloproliferative neoplasms in Sweden. Blood. 2008;112:2199–204. doi:10.1182/blood-2008-03-143602.
Olcaydu D, Harutyunyan A, Jager R, et al. A common JAK2 haplotype confers susceptibility to myeloproliferative neoplasms. Nat Genet. 2009;41:450–4. doi:10.1038/ng.341.
Pardanani A, Fridley BL, Lasho TL, et al. Host genetic variation contributes to phenotypic diversity in myeloproliferative disorders. Blood. 2008;111:2785–9. doi:10.1182/blood-2007-06-095703.
Hinds DA, Barnholt KE, Mesa RA, et al. Germ line variants predispose to both JAK2 V617F clonal hematopoiesis and myeloproliferative neoplasms. Blood. 2016;128:1121–8. doi:10.1182/blood-2015-06-652941.
Tapper W, Jones AV, Kralovics R, et al. Genetic variation at MECOM, TERT, JAK2 and HBS1L-MYB predisposes to myeloproliferative neoplasms. Nat Commun. 2015;6:6691. doi:10.1038/ncomms7691.
Barbui T, Vannucchi AM, Buxhofer-Ausch V, et al. Practice-relevant revision of IPSET-thrombosis based on 1019 patients with WHO-defined essential thrombocythemia. Blood Cancer J. 2015;5:e369. doi:10.1038/bcj.2015.94.
Haider M, Gangat N, Lasho T, et al. Validation of the revised international prognostic score of thrombosis for essential thrombocythemia (IPSET-thrombosis) in 585 mayo clinic patients. Am J Hematol. 2016;91(4):390–4. doi:10.1002/ajh.24293.
Tefferi A, Guglielmelli P, Larson DR, et al. Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood. 2014;124:2507–13. doi:10.1182/blood-2014-05-579136.
Cerquozzi S, Tefferi A. Blast transformation and fibrotic progression in polycythemia vera and essential thrombocythemia: a literature review of incidence and risk factors. Blood Cancer J. 2015;5:e366. doi:10.1038/bcj.2015.95.
Tefferi A, Barbui T. Polycythemia vera and essential thrombocythemia: 2015 update on diagnosis, risk-stratification and management. Am J Hematol. 2015;90(2):162–73. doi:10.1002/ajh.23895.
Quintás-Cardama A, Abdel-Wahab O, Manshouri T, et al. Molecular analysis of patients with polycythemia vera or essential thrombocythemia receiving pegylated interferon α-2a. Blood. 2013;122:893–901. doi:10.1182/blood-2012-07-44201.
Cassinat B, Verger E, Kiladjian JJ. Interferon alfa therapy in CALR-mutated essential thrombocythemia. N Engl J Med. 2014;371(2):188–9. doi:10.1056/NEJMc1401255.
Landolfi R, Marchioli R, Kutti J, et al. Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med. 2004;350(2):114–24. doi:10.1056/NEJMoa035572.
Gisslinger H, Gotic M, Holowiecki J, et al. Anagrelide compared with hydroxyurea in WHO-classified essential thrombocythemia: the ANAHYDRET Study, a randomized controlled trial. Blood. 2013;121(10):1720–8. doi:10.1182/blood-2012-07-443770.
Verstovsek S, Passamonti F, Rambaldi A, et al. Long-term results from a phase II open-label study of ruxolitinib in patients with essential thrombocythemia refractory to or intolerant of hydroxyurea. Blood. 2014;124:184.
Tefferi A, Wassie EA, Lasho TL, et al. Calreticulin mutations and long-term survival in essential thrombocythemia. Leukemia. 2014;(12):2300–3. doi:10.1038/leu.2014.148.
Jones AV, Cross NC. Inherited predisposition to myeloproliferative neoplasms. Ther Adv Hematol. 2013;4:237–53.
Recommended Reading
Milosevic JD, Kralovics R. Genetic and epigenetic alterations of myeloproliferative disorders. Int J Hematol. 2013;97(2):183–97. doi:10.1007/s12185-012-1235-2.
Reilly JT. Pathogenetic insight and prognostic information from standard and molecular cytogenetic studies in the BCR-ABL-negative myeloproliferative neoplasms (MPNs). Leukemia. 2008;22:1818–27. doi:10.1038/leu.2008.218.
Rumi E, Pietra D, Ferretti V, et al. JAK2 or CALR mutations status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood. 2014;123(10):1544–51. doi:10.1182/blood-2013-11-539098.
Tefferi A, Barbui T. Personalized management of essential thrombocythemia—application of recent evidence to clinical practice. Leukemia. 2013;27:1617–20. doi:10.1038/leu.2013.99.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Ewton, A.A., Donohue, R.E. (2018). Essential Thrombocythemia. In: Chang, CC., Ohgami, R. (eds) Precision Molecular Pathology of Myeloid Neoplasms. Molecular Pathology Library, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-319-62146-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-62146-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62144-9
Online ISBN: 978-3-319-62146-3
eBook Packages: MedicineMedicine (R0)