Abstract
Cardiovascular disease, is a well known complication of radiation therapy. This is especially seen in Hogdkin’s lymphoma survivors, who have received mediastinal therapy.
In this chapter, we present some of the common conditions associated with radiation induced heart disease.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keyword
Improvement in cancer therapy has led to an increasing number of survivors of childhood malignancy. In the United States alone, nearly 14.5 million children and adults with a history of cancer were alive on January 1, 2014 and it is estimated that by 2024, the population of cancer survivors will increase to almost 19 million [1]. Some of these cancer survivors are afflicted with long term side effects of therapy. One well recognized late secondary effect in patients receiving mediastinal and chest wall radiation is cardiovascular disease (CVD) [2].
The data for possible causal association of radiation and heart disease mainly comes from studies of Hodgkin’s lymphoma (HL) and breast cancer patients undergoing radiation therapy (RT).
Amongst long term survivors of HL, previously treated with radiation, CVD is one of the most common cause of death [3]. Patients with HL treated with mediastinal radiation, have a 3.0 times higher relative risk of death from myocardial infarction [4]. Patients previously treated with mediastinal radiation are at increased risk for the development of coronary artery disease (CAD), valvular heart disease, congestive heart failure (CHF), pericardial and conduction system disease [1, 5]. The incidence of cardiac events increases with time, can affect younger adults and is related to the radiation dose to the heart [5, 6].
A meta-analysis of eight randomized trials of patients with breast cancer found a 62% increase in cardiac deaths among women who were treated with RT [7]. The curve for development of cardiac diseases and subsequent cardiac procedures rises steeply after 10 years of RT [8].
The basic mechanism behind radiation induced vascular damage is endothelial dysfunction, with activation of inflammatory mechanism, release of cytokines and growth factors with cellular infiltration, fibrin leak into the tissues promoting collagen deposition, which may eventually lead to fibrosis [9].
This chapter illustrates some common CVD encountered in patients with history of previous RT.
RT can affect the pericardium, myocardium, coronary vessel, valves and the conduction system. Pericardium is most frequently involved (Table 7.1).
Acute Pericarditis
Patients with acute pericarditis during RT, frequently present with chest pain, low grade fever and non- specific ECG changes. Sometimes classic ECG finding is seen, as illustrated in the case (Fig. 7.1).
Patients are treated with conventional therapy which includes non-steroidal anti-inflammtory drugs (NSAID), cochicine and steroids (in resistant cases). Treatment of underlying malignancy is usually continued. Echocardiogram may or may not show minimal to small pericardial effusion. Cases with pericardial effusion should be followed up by a limited echocardiogram in 4–6 weeks. In most cases the effusion resolves with medical therapy. Patients who develop pericardial effusion after radiation, even if minimal should be followed up by periodic echocardiogram, as rarely it may lead to chronic pericardial effusion.
Chronic Pericardial Effusion
Chronic pericardial effusion can develop months or years after completion of radiation therapy. The development of chronic pericardial effusion is usually discovered by the incidental finding of enlarged cardiac silhouette on chest–X-ray or development of pericardial effusion on CT scan, which is done routinely for follow up purposes (Figs. 7.2 and 7.3). Some of these patients may develop symptoms of fatigue, dyspnea on exertion and leg edema.
Following case illustrates the development of chronic pericardial effusion due to RT.
A 49 year old man, stage 3 lung carcinoma, who had received a total of 70 Gy radiation to the chest, completed in Jan 2006. When seen in the clinic on 3rd Dec 2007, he was well and walking 5 miles/day with minimal shortness of breath. A chest-X-ray showed enlarging cardiac silhouette (Fig. 7.2). Review of CT scans showed a slowly increasing pericardial effusion (Fig. 7.3)
CT scans shows development of chronic pericardial effusion. A CT scan on 6th Mar 2006 showed no pericardial effusion. Subsequent CT scan on 30th May 2006 shows small pericardial effusion, which progressively increases to become large in Dec 2007, necessitating a pericardial drainage. CT scan on 9th Jan 2012, shows no re-accumulation of pericardial fluid. The red arrow points to the large pericardial effusion
This led to an echocardiogram showing a large pericardial effusion, with tamponade physiology, for which he underwent successful pericardiocentesis. The pericardial fluid showed only inflammatory cells with no malignant pathology. Subsequent follow up echocardiograms shows no re-accumulation of the fluid. When seen last in clinic in 2014, he was asymptomatic and doing well.
Constrictive Pericarditis
Pericardial constriction can develop many years after completion of radiation therapy. Patients usually present with fatigue, dyspnea and signs of heart failure.
Figure 7.4 illustrates the case of a young man who completed his radiation therapy 40 Gy to mediastinum and neck for HL in 1984. He presented with complete heart block in 2005 for which a permanent pacemaker was implanted. In March 2007 he presented with a pericardial effusion for which he underwent pericardiocentesis and a pericardial window. His symptoms persisted and further evaluation confirmed a pericardial constriction for which he underwent a pericardial stripping in April 2007. The coronary angiogram also showed a 50% LAD. Figure 7.5 shows hemodynamic findings of constrictive pericarditis.
Constrictive pericarditis: Hemodynamics showing venticular discordance (interdependence) with an increase in right venticular (RV) pressure and a simultaneous decrease in left venticular (LV) pressure during inspiration in a patient with constrictive pericarditis due to previous thoracic surgery (The red arrow points to the RV and the black arrow points to the LV)
Coronary Artery Disease (CAD)
CAD may manifest many after completion of RT. Proximal vessels which are in the field of RT are frequently affected. However radiation is also known to affect the small vessels. Asymptomatic cardiac perfusion defects are seen in about 50% of breast cancer patients treated with RT and can occur as early as early as 6 months after radiotherapy [10].
Following cases illustrates the development of symptomatic and asymptomatic radiation induced CAD (Figs. 7.6 and 7.7).
A 34 year female with history of diabetes mellitus and no other risk factors. She completed RT for HL in Nov 2005. In Jan 2014 she presented with a Non ST elevation myocardial infarction (NSTEMI). A coronary angiogram showed a significant proximal right coronary artery (RCA) disease for which she underwent successful percutaneous intervention. The red arrow points to the proximal RCA lesion (Image courtesy of Dr. C. Iliescu)
Coronary artery disease: A 50 year old man with previous history of mesothelioma and radiation in the cardiac field, fully asymptomatic. A routing pre-op tress test shows severe ischemia in the inferior wall (in the region of previous radiation). (a) A nuclear scan showing inferior wall ischemia. (b) A coronary angiogram shows significant RCA disease. (c) Following successful coronary intervention and stenting
Patients with radiation induced CAD are treated as per ACC/AHA guidelines, with aggressive medical therapy for stable disease and per-cutaneous intervention for unstable disease. Surgical intervention can sometimes be challenging due to significant mediastinal fibrosis and involvement of the internal mammary arteries.
Valvular Heart Disease
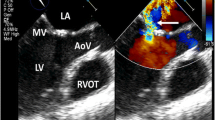
There is a high prevalence of asymptomatic valvular disease (particularly aortic), following mediastinal irradiation [11]. Most of the lesions are regurgitant and mild [11]. Rarely severe valvular disease may occur. Fig. 7.8 illustrates the case of radiation induced valvular disease.
Illustrates the case of a 46 year asymptomatic female, who had completed 30 Gy radiation to the mediastinum and neck for HL in 1976. Following echocardiogram in 2005 (29 years after completion of radiation therapy) was obtained for routine follow up. The echocardiogram shows mild regurgitation of all valves with moderate aortic stenosis
Vascular Calcification and Stenosis
Following cases illustrates the development of calcification and stenosis in major vessels (Figs. 7.9, 7.10 and 7.11).
Shows complete occlusion of the left subclavian artery (radial approach) in a 66 year old man with history of radiation in the region of subclavian artery for a hypopharyxngeal tumor. He had a previous history of CABG in 2000. The coronary angiogram was done in Nov 2008 for an abnormal stress test obtained for a pre-operative evaluation. The patient was otherwise asymptomatic, with finding of absent left radial and a barely palpable left brachial pulse. Image shows complete occlusion of the left subclavian artery (red arrow) (left brachial artery approach). Left Internal mammary artery (LIMA) is visible. In addition there is about 50% stenosis at the origin of the left vertebral artery. Slide courtesy of Dr. Iliescu
The following image shows carotid atherosclerosis/stenosis in a patient who has received radiation for nasopharyngeal carcinoma more than 25 years ago. This 77 year old man was physically active, with no neurological symptoms and had no history of other vascular disease. A carotid Doppler showed calcified plaques in the right and left bulbs with secondary 50–69% stenosis of the left internal carotid artery segment and <50% stenosis of the right internal carotid artery segment. Normal forward flow was present in the right and left vertebral arteries
Cardiomyopathy
Cardiomyopathy is also a known complication, and myocardial strain imaging is a novel method to detect myocardial abnormality in patients with RT [12] (Fig. 7.12).
The above image is of a 35 year old man with mediastinal lymphoma, ex-smoker, Chol = 234, LDL = 150, who had received a total of 39.6 Gy radiation between Sep and Oct 2010. The initial global strain (GLPSAvg) (24th Sep 2010) was −18.5, which decreased to −15.7 (19th Jan 2011) with RT, indicating abnormal myocardial strain due to RT(normal myocardial strain is >−18.5)
Conduction System Disorder
Heart block can occur many years after completion of the RTand is due to fibrosis of the conduction system (Fig. 7.13).
Shows the ECG of a patient who presented with complete heart block 29 years after completion of RT. The patient presented underwent RT for HL (when aged 16 years) in 1978. In 1998 she was found to have moderate aortic regurgitation. In 2001 she under Aortic Valve replacement (AVR) with coronary artery bypass grafting (CABG). In 2009 (aged 47 years), she presented with syncope and was found to be in complete heart block for which she underwent a permanent pacemaker placement
Discussion
As illustrated by cases above, radiation causes pericardial, valvular, vascular, myocardial and conduction system disease.
Effort should be made to prevent the development of these complications. With advancement in radiation and decreasing dose the incidence may decrease over a period of time, but globally still many patients will be afflicted with these cardiovascular side effects of RT.
For patients undergoing mediastinal radiation, at baseline evaluation clinical risk factors like smoking, hyperlipidemia, diabetes mellitus and hypertension should be identified and treated according to existing guidelines. At baseline a lipid profile, thyroid function, 12 lead ECG and an echocardiogram should also be obtained.
The prevalence and development of radiation associated valve disease (RAVD) is related to the time following RT e.g. in one study the prevalence of moderate to severe aortic regurgitation was 1.1% amongst those who had undergone RT 2–10 years earlier, which increased to 15% amongst the group receiving RT > 20 years ago [11]. Hence a follow up echocardiogram should be done at least at a minimum of 10 year interval after radiation therapy.
Likely due to tumor location, radiation related CAD primarily has been described to involve the proximal vessels, the coronary ostia and left main artery [13, 14]. Patients with radiation induced CAD commonly present with angina, myocardial infarction or syncope related to complete heart block [14]. Rarely, sudden death may be the initial presentation in these patients [14]. Myocardial perfusion defects, in irradiated portion of left ventricle in asymptomatic patients also suggest small vessel damage due to RT [15]. In one study, which included patients who had received more than 35 gray of RT, about 8.4% of patients had some sort of perfusion defect on their stress test. Of these only 5% had received RT within 2–10 years of being enrolled in this study, compared to 20% who had received radiation therapy >20 years ago [16]. In this study, in the group that had received RT within 5–10 years of being enrolled in the study only 1.7% of the total patients enrolled underwent coronary angiogram based on the result of the stress test [16].A functional non-invasive stress test is recommended 5–10 years after completion of RT, in high risk asymptomatic patients. (patients who have undergone anterior or left sided chest radiation with >1 risk factors for radiation induced heart disease) [17].Carotid stenosis, is recognosed complication of radiation therapy to the neck. Long segement of the carotid artery may be affected. In one study in which patients received a mean cumulative radiation dose of 6420 cGy (range 5500–7680), with a mean duration of 10.2 years since their last radiation treatment, 16 patients (40%) had significant carotid artery stenosis [18]. Based on little data, a firm conclusion cannot be made for Doppler screening in these patients, but it is not unreasonable to have a screening Doppler of the carotid arteries, at >10 years after completion of radiation, or earlier if any clinical finding of bruit.
Key Points
-
Hodgkin’s lymphoma and breast cancer survivors treated with radiation therapy are at increased risk of development of cardiovascular disease.
-
Radiation related damage to the heart affects the pericardium, myocardium, valves, and coronary vessels, with pericardium being most frequently involved.
-
Asymptomatic cardiac perfusion defect are seen in about 50% of breast cancer patients treated with radiation therapy and can occur as early as early as six months after radiotherapy.
-
Due to improvement in radiation techniques, the risk of cardiovascular complications in relation to radiation may have declined over time, but the risk of death from myocardial infarction in patients with HL remains increased even amongst those treated after 1985. Recently, population based case-control study of major coronary events in women who received radiation therapy for invasive breast cancer between 1958 and 2001, reported that the subsequent rate of ischemic heart disease was proportional to the mean dose to the heart, with the relative risk increasing by 7.4% per Gray (Gy) [19].
-
Endothelial damage is an early sign of radiotherapy induced vascular injury.
-
Radiation induced fibrosis seems to be the result of multicellular interactions mediated by inflammatory cytokines, vascular inflammation and endothelial cell dysfunction.
-
Prevention of radiation induced heart disease should be the main goal of all clinicians involved in the care of these patients.
-
Risk factors like smoking, hypertension, diabetes mellitus, and hyperlipidemia should be aggressively targeted and treated as per current guidelines.
-
Echocardiogram should be done at 5–10 years follow up, or earlier if clinically indicated.
-
A functional non-invasive stress test is recommended 5–10 years after completion of radiation, in high-risk patients.
References
American Cancer Society. Cancer treatment and survivorship facts & figures 2014–2015. 2014. http://www.cancer.org/
Yusuf SW, Sami S, Daher IN. Radiation-induced heart disease: a clinical update. Cardiol Res Pract. 2011;2011:317659. doi:10.4061/2011/317659.
Ng AK, Bernardo MP, Weller E, et al. Long-term survival and competing causes of death in patients with early-stage Hodgkin’s disease treated at age 50 or younger. J Clin Oncol. 2002;20(8):2101–8.
Hancock SL, Tucker MA, Hoppe RT. Factors affecting late mortality from heart disease after treatment of Hodgkin’s disease. JAMA. 1993;270(16):1949–55.
Mulroney DA, Easel MW, Kawashima T, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the childhood cancer survivor study cohort. BMJ. 2009;339:b4606.
Swerdlow AJ, Higgins CD, Smith P, et al. Myocardial infarction mortality risk after treatment for Hodgkin disease: a collaborative British cohort study. J Natl Cancer Inst. 2007;99(3):206–14.
Cuzick J, Stewart H, Rutqvist L, et al. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol. 1994;12(3):447–53.
Galper SL, Yu JB, Mauch PM, et al. Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation. Blood. 2011;17(2):412–8.
Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol. 2003;4:529–3.
Hardenberg PH, Munley MT, Bentel GC, et al. Cardiac perfusion changes in patients treated for breast cancer with radiation therapy and doxorubicin; preliminary results. Int J Radiation Oncol Biol Phys. 2001;49(4):1023–8.
Heidenreich PA, Hancock SL, Lee BK, Mariscal CS, Schnittger I. Asymptomatic cardiac disease following mediastinal irradiation. J Am Coll Cardiol. 2003;42(4):743–9.
Thavendiranathan P, Poulin F, Lim KD, et al. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014;63(25 Pt A):2751–68. doi:10.1016/j.jacc.2014.01.073. Epub 2014 Apr 2
Brosius FC 3rd, Waller BF, Roberts WC. Radiation heart disease. Analysis of 16 young (aged 15 to 33 years) necropsy patients who received over 3,500 rads to the heart. Am J Med. 1981;70(3):519–30.
Orzan F, Brusca A, Conte MR, Presbitero P, Figliomeni MC. Severe coronary artery disease after radiation therapy of the chest and mediastinum: clinical presentation and treatment. Br Heart J. 1993;69(6):496–500.
Gyenes G, Fornander T, Carlens P, Glas U, Rutqvist LE. Myocardial damage in breast cancer patients treated with adjuvant radiotherapy: a prospective study. Int J Radiat Oncol Biol Phys. 1996;36(4):899–905.
Heidenreich PA, Schnittger I, Strauss HW, et al. Screening for coronary artery disease after mediastinal irradiation for Hodgkin’s disease. J Clin Oncol. 2007;25(12):43–9.
Lancellotti P, Nkomo VT, Badano LP, BerglerKlein J, Bogaert J, Davin L, et al. Expert consensus for multi-modality imaging evaluationof cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26(9):1013–32.
Steele SR, Martin MJ, Mullenix PS, et al. Focused high-risk population screening for carotid arterial stenosis after radiation therapy for head and neck cancer. Am J Surg. 2004;187:594–8.
Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368:987–98.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Yusuf, S.W. (2018). Radiation Related Cardiovascular Disease. In: Yusuf, S., Banchs, J. (eds) Cancer and Cardiovascular Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-62088-6_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-62088-6_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62086-2
Online ISBN: 978-3-319-62088-6
eBook Packages: MedicineMedicine (R0)