Abstract
According to the Centers for Disease Control and Prevention (CDC), 2015 marked the record for drug overdoses in the United States as more than 33,000 individuals died from an overdose of heroin or synthetic opioids, with nearly half of these deaths attributed to prescription opioids. CDC estimates indicate that 60% of all drug overdose deaths involve opioids. Since 1999, opioid overdose has nearly quadrupled with more than half a million deaths documented between 2000 and 2015. Current estimates suggest that 91 citizens perish daily from opioid overdose (CDC, 2016).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Addiction
- Substance abuse
- Opiates
- Evolved vulnerability
- Darwinian medicine
- Evolution
- Mental disorders
- Psychopathology
According to the Centers for Disease Control and Prevention (CDC), 2015 marked the record for drug overdoses in the United States as more than 33,000 individuals died from an overdose of heroin or synthetic opioids, with nearly half of these deaths attributed to prescription opioids. CDC estimates indicate that 60% of all drug overdose deaths involve opioids. Since 1999, opioid overdose has nearly quadrupled with more than half a million deaths documented between 2000 and 2015. Current estimates suggest that 91 citizens perish daily from opioid overdose (CDC, 2016).
Increased availability of both licit and illicit forms of opioids has been attributed to the escalation in both use and deaths (Friedman, 2014). The prescribing of and misuse of opioid drugs has increased significantly in the United States. For example, 174.1 million prescription opioids were prescribed in 2002; this number increased to 256.9 million by 2009. In 2014, 4.5 million people in the United States aged 12 and older indicated that they used a prescription pain medication for a nonmedical issue in the past month, and 289 thousand people indicated they used heroin in the last month (SAMHSA, 2014). As the cost of procuring nonmedical prescription drugs has increased, the availability of less expensive street heroin has increased, thus expanding numbers of addicted users and potential overdoses (Center for Substance Abuse Treatment [CSAT], 2005). To combat the dangers of prescription opioids and overdose the Food and Drug Administration (FDA, 2016) now requires “boxed-warnings” emphasizing risks for accidental overdose and addiction potential when taking opioids and benzodiazepines.
These efforts by the FDA to combat the dangers of prescription opioids and the risk of overdose promise to be effective eventually, and new intervention and treatment methods are promising. However, risk remains high. This state of affairs places significant emphasis on the importance of available treatments to save lives and prevention initiatives to reduce the significant demand for opioids in the population.
Given the current demand for opioids and risks of addiction, it is imperative to understand the etiology of addiction and psychopharmacological function of opiates. A broad perspective may enable better understanding and eventually lead to better treatment and prevention approaches. We need to marshal all areas of knowledge about addiction from all possible sources in order to help understand and intervene. This chapter takes an evolutionary approach to augment traditional perspectives.
An evolutionary perspective could add to our understanding of addiction, but it must be stated that addiction has no adaptive value; rather, humans have evolved processes and mechanisms for other purposes, which allow vulnerability to addiction (Nesse & Berridge, 1997). An evolutionary perspective helps explain how we are neurologically and behaviorally susceptible to addiction. Brain substrates for normal motivation and emotion use chemical neurotransmitters, which enable other nonnatural chemicals to engage these pathways. Nesse (2016) summarizes:
Vulnerability to substance abuse results from our novel environment. The reliable availability of pure chemicals and clever new routes of administration increase the rate of drug taking. Tobacco administered via the technological advance of cigarettes is the most widespread and harmful addiction, with alcohol a close second. The so-called hard drugs of abuse, such as amphetamines and cocaine, act even more directly on ascending dopamine tracts to establish addiction. Substance abuse is a universal human vulnerability to drugs that hijack reward mechanisms. (p. 1017).
Here we take an evolutionary perspective to understand the current epidemic of opiate addiction. Understanding opiate addiction involves understanding many aspects of motivation, emotion, brain pathways, and neurotransmitters, which will be described. One area of research that has led to greater understanding of opiate addiction is research on the neuroscience of distress calls of neonatal rodents. When rodent pups are separated from the home nest, they emit ultrasonic distress calls. These are above 35 kHz (Branchi, Santucci, & Alleva, 2001), not audible to human ears. Upon hearing these calls, a mother rat or mouse will investigate the sound location, pick up the pup in her mouth, and retrieve it to the nest (Noirot, 1972; Sewell, 1970). Rodent pups reliably make these calls when they become cold (Okon, 1970). They cannot thermoregulate until about 2 weeks old and thus depend upon warmth from the mother and littermates in the nest. Separation from the nest can be fatal quickly. These calls are labeled “separation distress calls .” Understanding the neuroscience of distress calls of rodents and other animals has led to a greater understanding of opiate addiction in humans (Panksepp, 1998). The common link is the endogenous opioid system in the mammalian brain, which subserves response to pain and also motivates distress calls. The evolution of these brain systems is critical to survival, but the system is vulnerable to drugs of addiction that mimic natural opioids and provide stronger relief of both physical and emotional pain than endogenous opioid activity.
This chapter will propose that the involvement of the opioid system in social attachment and physical pain contributes to the current prevalence of addiction to opiate drugs. The process and course of addiction will be described. Then we will briefly review the brain systems involved in opiate addiction and note the common opioid drugs of abuse. Next, we will describe factors that may explain why opiate addiction has become such a problem today. An evolutionary perspective is helpful in understanding addiction (Nesse & Berridge, 1997), as this perspective led to the current understanding that physical and social pain use the same brain pathways (Panksepp, 1998). We will present recent evidence for the role of opioid brain systems in social and physical pain. These vulnerabilities are shared by all human beings. However, research has shown that individual differences exist in the opioid systems in the brain that contribute to both types of pain. Some of the most important research will be reviewed. Lastly, we will describe promising avenues of treatment, intervention, and prevention of opiate addiction.
What Is Addiction?
Addiction is considered to be a medical disease involving changes in brain pathways once addiction has taken hold (the “hijacked brain”). Considered a treatable medical disorder, drug use disorder is considered a brain disease instead of a moral failing or lack of willpower (CSAT, 2005).
Substance Use Disorders
According to the American Psychiatric Association (APA), Substance Use Disorders (formerly referred to as addictions) are disorders related to an individual continuing to use a specific substance despite experiencing significant problems related to this substance (APA, 2013). These problems fit into four areas: impaired control, social impairment, risky use, and pharmacological criteria. The severity of a given Substance Use Disorder is rated either mild, moderate, or severe based on the number of symptoms the individual is experiencing. Impaired control refers to the influence that the substance exerts on an individual’s life. Examples include: time devoted to activities related to obtaining, using, and recovering from the substance; more substance being used than the individual intended; or the individual’s inability to stop or reduce the amount of the substance despite efforts to do so. Social impairment refers to negative changes in behavior that are related to substance use. This includes the individual failing to meet obligations at work, home, or school; the individual withdrawing from activities that were previously important or pleasurable for the individual; or the individual continuing to use the substance despite use continually resulting in interpersonal problems. Risky use refers to the use of the substance in dangerous situations (e.g., driving while intoxicated), or the individual continuing to use the substance despite having knowledge that the substance will have a negative effect on their physical or psychological problems. Finally, the area of Physiological criteria refers to the individual experiencing tolerance (i.e., needing to consume more of the substance to have the same physiological effect) and/or withdrawal (i.e., symptoms related to a reduction in the concentration of the substance in the individual’s body). Substance Use Disorder cannot be diagnosed based on physiological criteria alone if the substance is being used appropriately to treat a diagnosed medical condition and the individual has a valid prescription for the substance. However, if an individual being treated for a medical condition begins to meet other criteria for Substance Use Disorder, then they will meet the diagnostic criteria despite having a valid prescription for the substance (APA, 2013).
Opioid Use Disorder (OUD)
Considered a treatable medical disorder, OUD is considered a brain disease instead of a moral failing or lack of willpower (CSAT, 2005). By virtue of opioids’ pharmacodynamic and pharmacokinetic properties , opioids are extraordinarily reinforcing (i.e., addictive) both psychologically and physiologically over a relatively short period of regular use. The initial “rush” following opioid ingestion is experienced by the user as an intense euphoria and, therefore, becomes promptly positively reinforced. Typically, abused street and nonmedical prescription drugs are short acting (i.e., 4–6 h) and lead to increasing levels of discomfort as they are metabolized and diminish, characteristic of opioids’ withdrawal syndrome. Withdrawal severity is moderated by tolerance and frequency of administration of the drug. Opioids become rapidly negatively reinforced through a conditioned avoidance of withdrawal as use progresses. Opioid use is further complicated by a simultaneous increasing tolerance to the initial euphoric effects of the drug. In combination, these factors make intentional behavior change (i.e., cessation) of opioids considerably more difficult when compared to other Substance Use Disorders (SUDs).
OUD is distinctively characterized from other SUDs in several respects. Opioids are available as licit substances in the form of prescription analgesics (e.g., oxycodone, hydrocodone, Percocet) or illicitly (e.g., heroin). In addition, nonmedical use of prescription drugs, especially for purposes of abuse, is deemed illegal. Opioids, unlike other commonly abused substances (e.g., alcohol, tobacco, cannabis, and cocaine), can be consumed through multiple routes of administration (e.g., intranasal, inhalation, rectal [mucosal], subcutaneous, transdermal, intravenous). Changes in routes of administration often indicate an intensification of addiction, for example, when intranasal use is substituted by methods of inhalation or intravenous administration.
Unlike alcohol and other common drugs of abuse, tolerance effects for opioids typically occur rapidly necessitating ever-increasing amounts of the substance. This is naturally followed by a characteristic withdrawal syndrome with severity predicated upon frequency and quantity of opioids used. The characteristic withdrawal syndrome includes three or more of the following: dysphoria, nausea, tearing, runny nose, sweating, gooseflesh, dilated pupils, diarrhea, yawning, fever, and insomnia (APA, 2013). It is common for tolerant users avoiding withdrawal to experience financial problems maintaining a steady supply, in addition to engaging in protracted drug-seeking behavior.
The characteristics of opiate addiction are illuminated by understanding the brain pathways that are involved in this type of addiction. Brain pathways that are hijacked by opiate drugs are normally responsible for inhibiting pain.
Opioid System in the Brain
Addiction involves multiple pathways and brain areas. The dopaminergic mesolimbic reward pathway is best known and is implicated in most addictions. It travels from the midbrain ventral tegmental area (VTA) to the nucleus accumbens (NAcc). Stimulant drugs directly affect this pathway, while other drugs of abuse such as opiates increase dopaminergic transmission in this pathway more indirectly (reviewed in Nestler, Hyman, & Malenka, 2009). Here we focus on opioid systems and their interconnections with other systems. In one conceptualization, the DA reward pathway mediates approach to rewards (appetitive motivation), while consumption (which would terminate approach) is mediated by opioid pathways (Berridge, 1996; Robinson & Berridge, 1993). Stimulation of the DA reward pathway/median forebrain bundle is intrinsically reinforcing, as demonstrated by studies of rodents taught to bar press for brain stimulation (Olds 1977). Consumption of a reward (e.g., food or sex) never occurs, but rather compulsive self-administration is never-ending (as described by Panksepp, Knutson, & Burgdorf, 2002).
A major job of the opioid system in the brain is to inhibit pain (Meyer & Quenzer, 2013). At the spinal cord level, when pain occurs small inhibitory spinal interneurons release endorphins that reduce the likelihood of the pain signal being sent up to the brain by spinal projection neurons (Meyer & Quenzer, 2013). Pain is also regulated by descending modulatory pathways that are predominately found in the periaqueductal gray (PAG) area in the brain. Through these pathways, pain can be regulated in three different ways: (1) by inhibiting the spinal projection neuron, (2) by inhibiting excitatory interneurons that synapse on the spinal projection neuron, and (3) by exciting the small inhibitory spinal interneurons that inhibit the spinal projection neuron (Meyer & Quenzer, 2013). Pain can further be modulated by higher brain structures, including the cerebral cortex, medial thalamus, and the hypothalamus, which send neuronal projections to the PAG (Apkarian, Bushnell, Treede, & Zubieta, 2005; Meyer & Quenzer, 2013). Specific regions of the cerebral cortex that are considered to be part of the perception of acute pain include: primary and secondary somatosensory, insular, anterior cingulate, and prefrontal cortices (Apkarian et al., 2005). Thus, one of the functions of the opiate system is to lessen or stop pain signals transmitted to those areas.
Secondary pain affect is a term for how an individual imagines prolonged pain will interfere with his or her life (Price, 2000, 2002). It involves planning for how the pain will affect an individual’s life, but may lead to rumination. Thus, individuals with particular personality disorders have been found to have greater secondary pain affect (Price, 2002). The anterior cingulate cortex (ACC) is believed to be the brain area where there is coordination between the immediate threat of pain in the parietal cortex with secondary pain affect in the prefrontal cortex (PFC; Price, 2002).
However, when it comes to opioids, pain is not where the story ends because opioids also promote feelings of euphoria and well-being (Meyer & Quenzer, 2013). These euphoric effects explain why individuals take opioids recreationally (Mestek, Chen, & Yu, 1996). Another issue with opioids is that their use is highly reinforced, which easily leads to the development of Opioid Use Disorders , even in individuals who are prescribed an opioid for a valid medical reason who originally only intend to take the drug as prescribed. The reward and reinforcement pathway in the brain was mentioned earlier, the dopaminergic mesolimbic pathway (Meyer & Quenzer, 2013). Evidence supports that opioids achieve reinforcement in this pathway by inhibiting neurons that prevent/reduce the firing of the VTA neurons (Meyer & Quenzer, 2013). Thus, by inhibiting the neurons that inhibit the VTA neurons, the VTA neurons that project to the NAcc are able to fire more often, and release more dopamine on the receptors of neurons in the NAcc, which results in positive reinforcement (Meyer & Quenzer, 2013).
Thus, opiate drugs affect the same reward pathways as other addictive drugs, but opiates have other effects that add to the addiction potential of these drugs. These effects will be described further below. First, the main types of opioid receptors will be described.
Opioid Receptors
Four opioid receptors have been discovered. These include the mu (μ), delta (δ), kappa (κ), and nociceptin/orphanin FQ (NOP-R) opioid receptors (Meyer & Quenzer, 2013). These receptors evolved to respond to different classes of ligands that the body makes: endomorphins, endorphins, enkephalin, dynorphins, and nociceptin/orphanin FQ (Meyer & Quenzer, 2013). Each of the opioid receptors has a class of ligands that binds to it more strongly than it does to the other opioid receptors, but there is overlap between which ligands activate each receptor (Goldstein, 1987). For example, the μ-opioid receptor has the highest binding affinity for endomorphins and endorphins, but studies have found that enkephalins and dynorphins can also activate these receptors at physiological levels, each of which more strongly binds to delta opioid receptors and kappa opioid receptors, respectively (Mestek et al., 1996; Meyer & Quenzer, 2013). However, despite strong genetic similarity between the NOP-R receptor and the other opioid receptors, NOP-R neither binds traditional opioid ligands, nor does its ligand, nociceptin/orphanin FQ, bind to the three other opioid receptors, suggesting a unique role for this receptor and its ligand (Meyer & Quenzer, 2013). Of the receptors, the μ-opioid receptor has been studied the most in connection with opioid use disorders, as it has the strongest affinity for opioid drugs (Mestek et al., 1996). However, it is important to keep in mind that the opioid system as a whole is affected by use of opioids.
Based on receptor distribution in the brain and genetic knockout studies, evidence suggests that μ-opioid receptors have many different roles, such as in analgesia, respiratory/cardiovascular depression, nausea/vomiting, and sensorimotor integration (Meyer & Quenzer, 2013). Additionally, μ-opioid receptors have a complicated role in mood regulation, as the activation of μ-opioid receptors is associated with euphoria and relief from depression, whereas loss of these receptors in rodents is associated with reduced anxious and depressive symptoms (Filliol et al., 2000; Lutz & Kieffer, 2013a; Yoo, Lee, Loh, Ho, & Jang, 2004). Similar to μ-opioid receptors, δ-opioid receptors are associated with analgesia and positive reinforcement, but δ receptors are also found in higher brain structures and have additional roles in olfaction and cognition (Meyer & Quenzer, 2013). κ-Opioid receptors have distinctive roles from μ and δ receptors, as they regulate homeostatic mechanisms, such as eating, drinking, temperature control, and also produce hallucinations and dysphoria (Meyer & Quenzer, 2013). Studies suggest that the reinforcing properties of opioids are caused by μ- and δ-opioid receptors, whereas κ-opioid receptors were found to not be reinforcing, and to be possibly aversive (Shippenberg, 1993).
Drugs that Are Opioid Agonists
The endogenous ligands of the opiate system include: β-endorphin, enkephalins, and dynorphins (Lutz & Kieffer, 2013b). However, there are many natural and synthetic drugs that have been discovered or created to activate this system, which cause an array of different desired effects and symptoms. These effects include: analgesia, slowing of the gastrointestinal system, cardiovascular depression, nausea/vomiting, euphoria, calming, anti-depressant functions, suppressing coughing, dysregulation of homeostatic mechanisms, and reduced sex drive (Lutz & Kieffer, 2013b; Meyer & Quenzer, 2013). Opium was the first opiate used for medicinal, recreational, and ceremonial purposes. Natural components found in opium have been extracted and purified to be used as drugs that have more potent analgesic properties and/or fewer side effects than opium. The naturally derived opiates include morphine and codeine, of which codeine is less effective at reducing pain, but has fewer side effects than morphine (Meyer & Quenzer, 2013). Synthetic modification of the components in opium , as well as the synthetic production of molecules that bear structural similarity to these compounds, has given rise to a whole host of different medically available opioids that have an even greater number of street names (Table 1). Additionally, opioid partial agonists and opioid antagonists have been developed as less potent drugs and used in opioid replacement therapy for Opioid Use Disorder (buprenorphine and methadone), and to reverse the effects of opioid overdoses (e.g., naloxone) in order to save lives, respectively (Meyer & Quenzer, 2013).
Why Are Opiates an Epidemic Problem Currently?
Opiate addiction and overdose are an epidemic and increasing problem for several reasons. First, medical prescriptions lead to nonmedical use, which leads to use of illicit drugs. Secondly, opiates are strongly addictive due to sensitization of the brain pathway subserving natural reward. Third, and less well known, is that opiates impact our brain systems related to social attachment in addition to impacting the brain reward system common to most addictive substances. It is the many effects on social attachment that may give opiate drugs a special appeal that is difficult to replace.
Addiction to substances involves progressively stronger craving of them, in addition to the phenomenon of tolerance and withdrawal symptoms . Systems that respond to addictive drugs appear to become sensitized after repeated exposure, where the desire for a drug increases rather than decreases (Robinson & Berridge, 1993). The mechanism involves repeated activation of the mesolimbic pathway, which causes a process of long-term potentiation of glutamine synapses on VTA dopamine neurons (Nestler et al., 2009). Sensitization appears to make drugs and associated stimuli more attractive, a state that can persist for a long time and contribute to relapse after a period of abstinence.
As noted earlier, there is widespread exposure to opiates through prescription painkillers; as prescriptions become unavailable or too expensive individuals often begin to use heroin. The director of the National Institute of Health recently asserted several reasons for the growing epidemic of opioid use—the number of prescriptions being written by doctors has increased dramatically over the past two decades, the increasing acceptability of using substances recreationally in the United States, and aggressive marketing by pharmaceutical companies (Volkow, 2014).
A recent survey of American high school seniors in the Monitoring the Future study 2009–2013 found that the frequency of nonmedical opioid use in this sample was estimated to be 12.4% (Palomar, Shearston, Dawson, Mateu-Gelabert, & Ompad, 2016). Similar lifetime prevalence was reported (13.5%) for a European Union sample aged 12–49 (Novak et al., 2016). It has been suggested that opioid misuse results from unused pain medications being stored in the family home, thus giving access of these drugs to young people who live there (Dodrill, Helmer, & Kosten, 2011). In a study by Green, Black, Serrano, Budman, and Butler (2011), 45.8% of people who developed Opioid Use Disorder had been given a prescription for a valid medical reason.
The recent increase in heroin use is related to the surge in prescription opioid use. In the 1960s, 80% of heroin users were not exposed to prescription opiates first, but in the past 20 years, 75% of heroin users were first exposed to prescription opioids (Cicero, Ellis, Surratt, & Kurtz, 2014). A recent survey of American high school seniors, mentioned above, found that recent nonmedical use of opioids strongly increased the risk of heroin use (Palomar et al., 2016). Additionally, the demographic characteristics of heroin users have changed. Over the past 20 years, the people who have begun using heroin have been older (mid-twenties), predominantly white, and living in less urban areas than previous generations of heroin users (Cicero et al., 2014). Proposed reasons for this shift are that heroin is cheaper to obtain on the street and easier to obtain than prescription opioids, despite the facts that heroin is more likely to lead to an overdose and be less pure than prescription opioids (Cicero et al., 2014).
Wright et al. (2014) conducted a study to find what county-level features drive opioid prescription misuse. They found that access to healthcare, in particular dentists and pharmacists, increased access to prescription opioids (Wright et al., 2014). Other studies have listed systemic problems in the healthcare system as helping to fuel this national health epidemic, in that prescribers were not coordinating care for painful conditions and thus unknowingly overprescribing opiates to the same individuals (Dodrill et al., 2011). A recent analysis of data from the Veterans Health Administration determined that risk of overdose death increases in a dose–response fashion as prescription doses of opioids go from 0 to >100 mg per day or higher of morphine equivalent medication (Bohnert et al., 2011). Maximum daily dose over 50 mg was associated with elevated risk compared to dosage below 20 mg.
Third, and less well known, is that opiates impact our brain systems related to social attachment in addition to impacting the brain reward system common to most addictive substances. It is the effects on social attachment that may give opiate drugs a special appeal that is difficult to replace. We will focus on this aspect next.
Brain Pathways for Social Pain Overlap with Those for Physical Pain
The proposition that animal separation distress calls helps to understand human emotion, specifically social pain, may seem to be a stretch. Extrapolating animal research to humans requires the assumption that the neural pathways underlying behaviors are homologous in animals and humans. Experts in brain evolution have concluded that older brain structures have been modified and integrated with new structures, as more complex brains evolved. Interested readers are referred to a recent series of papers by O’Connell and Hoffman (O’Connell & Hofmann, 2011a, 2011b) that describe two ancient brain circuits present in vertebrates, the mesolimbic reward system and the social behavior network. These two circuits form part of a large social-decision-making network that is homologous among vertebrates (mammals, birds, reptiles, amphibians, and teleost fish; O’Connell and Hoffman, O’Connell & Hofmann, 2011a, O’Connell & Hofmann, 2011b).
Panksepp (1998) analyzed the brain substrates of separation distress , providing evidence that the emotion of separation distress uses the same brain substrates as physical pain, involving the opioid receptor system. Animal research supporting this conclusion dates to an early study by Panksepp, Herman, Conner, Bishop, and Scott (1978) showing that low doses of morphine reduced separation distress vocalizations in 6–8 week old puppies in a dose-dependent fashion.
Panksepp (1998) describes four primary emotion systems, one of which is called “ PANIC .” This basic emotion is associated with social loss and separation, subserved by neural pathways originally processing thermoregulation and pain. Nelson and Panksepp (1998) proposed that social pain messages are sent via pathways for physical pain, a neurological arrangement that facilitated social responses important for survival, such as making distress calls when separated from one’s mother. Panksepp (1998) proposed that the PANIC system arises from the midbrain PAG, close to the area where electrical stimulation results in physical pain (p. 267). Separation distress calls can be obtained by stimulation of the PAG, and in the ventral septal area, the dorsal preoptic area, the dorsomedial thalamus, the bed nucleus of the stria terminalis, and the anterior cingulate cortex (Panksepp, 1998, 2003). There is evidence from a variety of species that morphine reduces distress calls and naloxone increases these (from chicks [Panksepp, Bean, Bishop, Vilberg, & Sahley, 1980] to sheep [Shayit, Nowak, Keller, & Weller, 2003]). Other neurochemicals are also involved in social bonds. Panksepp (1998) states that, in addition to opioid systems, the prime substrates of social bonds in mammals are oxytocin and AVP (p. 259). The brain pathways important for physical pain and social attachment will now be described.
Research on social pain in humans has been conducted, complementing research with animal separation distress vocalizations. Figure 1 shows the brain pathways relevant to pain, with three types of cross-hatching to distinguish those areas that are considered to process physical pain, pain affect, and social pain. This diagram is adapted with permission from Apkarian et al. (2005) and Price (2000).
Diagram of brain with pain-processing pathways indicated. Three types of shading indicate pathways related to physical pain (diagonal hatching), the affective dimension of physical pain (stippling), and social pain (dashed hatching). Names of brain structures are abbreviated: PAG periaqueductal gray area, PB parabrachial nuclei, HT hypothalamus, AMYG amygdala, ACC anterior cingulate cortex, PCC posterior cingulate cortex, PPC posterior parietal cortex, S1 somatosensory area, S2 secondary somatosensory area, M1 motor cortex, SMA supplementary motor area, PF prefrontal cortex. Redrawn with permission from Apkarian et al. (2005) and Price (2000)
Areas that subserve physical pain include the PAG , the somatosensory cortex (S1), the thalamus (medial), and the hypothalamus, along with spinal neurons (Price, 2002). As stated earlier, pain pathways involving the PAG can be modulated by higher brain structures, including the cerebral cortex, medial thalamus, and the hypothalamus, through neuronal projections to the PAG (Apkarian et al., 2005; Meyer & Quenzer, 2013).
The affective dimension of pain was described by Price (2000) as being processed in the amygdala, the anterior cingulate cortex (ACC), and the insula. These areas are shown with a different type of shading in Fig. 1. Intense physical pain that causes distress activates areas in the brain associated with pain, as well as the areas associated with the affective dimension of pain. Price (2002) viewed the ACC as associated with pain unpleasantness, as it receives multiple inputs and has connections with the prefrontal cortex, enabling cognitive evaluation of pain and related emotion.
The proposition that animal separation distress will help us understand human emotion requires evidence that human social bonding and attachment is similar to that of animals, and the assumption that separation distress/social pain in adult humans can be induced and measured in a laboratory setting. The third type of shading in Fig. 1 shows areas related to social pain, assessed in the laboratory as pain from social rejection.
Researchers have recently begun studying social pain in laboratory experiments with humans (reviewed by Eisenberger, 2012, 2015). In the first study of its kind, Eisenberger, Lieberman, and Williams (2003) used fMRI to determine that the brain regions activated by social pain are similar to those activated by physical pain. Heightened activity in the ACC was shown when participants were exposed to social rejection (exclusion during a video game), and the amount of activity correlated strongly with self-reported distress (r = .88). In this study, participants initially thought they were playing the internet computer game with two others, but then the others stopped throwing them the ball. Eisenberger (2012) contends that social pain uses the same brain pathways as does the affective component of physical pain. Recent research in this and other laboratories have found similar results using various manipulations to induce social pain, such as reliving a romantic rejection (Kross, Berman, Mischel, Smith, & Wager, 2011). Indeed, with this type of intense social pain, neural substrates for the sensory component of pain were also activated (Kross et al., 2011). These authors concluded that: “brain systems that underlie social rejection developed by co-opting brain circuits that support the affective component of physical pain” (p. 6273; Kross et al., 2011).
The brain areas recruited for processing social pain are shown in Fig. 1: Secondary somatosensory cortex (S2), prefrontal cortex (PF), and BG (Basal ganglia, ventral striatum). During the experience of social pain, these areas are activated in addition to the areas responsive to pain affect (ACC, insula, and thalamus). Eisenberger (2012) described the two types of pain well:
Physical pain is a deeply psychological phenomenon that can be altered by expectation, mood, and attention. Likewise, social pain is a deeply biological phenomenon that has been built into our brains and bodies over millions of years of mammalian evolution because of the crucial part it plays in our survival (p. 431–432).
Social Pain Pathways Involve Opioids
Brain pathways and areas responsive to pain utilize opioid neurotransmitters. Panksepp (1998) proposed that endogenous brain opioid systems regulate distress associated with separation and the pleasure that comes with social connection. Eisenberger (2012) hypothesized that brain areas related to the affective component of physical pain were coopted to “warn against and prevent the dangers of social harm” (p. 423).
The information about pain pathways and μ-opioid receptor distribution comes from various lines of research. One line of research employs brain scans to measure changes during laboratory manipulation of pain. Other research has used indirect methods, such as testing pain thresholds . Early studies measured opioid receptor distribution anatomically. Table 2 shows distribution of three receptor types in the brain areas depicted in Fig. 1. This table is based upon in situ hybridization histochemistry using 33P–labeled RNA probes in postmortem human brains (Peckys & Landwehrmeyer, 1999). Additional information is included for rat brain from Mansour et al. (1994) where human studies are lacking. It is clear that opioid receptors are widely distributed in the brain. The areas with highest concentration of μ and κ receptors appear to be the thalamus and amygdala. The δ receptor appears to be highly prevalent in many areas, including the parietal cortex, cingulate cortex, insula, and amygdala. It is beyond the scope of this chapter to describe the pain pathways and their neurochemistry in fine detail; rather we focus on the basic areas where there is a consensus about their involvement. For example, the diagram shows the ACC as one area, but we do not separate the dorsal ACC from other anterior cingulate areas, nor do we separate the lateral from the medial pain system. Research about the various sections of the ACC continues. In another example, the ACC was reported to show presence of μ-opioid receptors (MOR) at a low level with in situ hybridization (Table 2), rather than a highly dense concentration. Despite not being the highest in MOR distribution in anatomical studies (Table 2), the ACC has high opioid receptor binding potential (Baumgärtner et al., 2006). Baumgärtner et al. (2006) measured binding potential with the subtype unselective radio-ligand [18F]flouroethyl-diprenorphine (which binds with MOR, KOR, and DOR with equal affinity). The fMRI studies reviewed by Eisenberger (2012) detected activity in these areas, blood-oxygenation level-dependent (BOLD) responses. Further research needs to integrate BOLD studies with those employing PET scanning methods.
Several experiments have investigated real-time changes in opioid receptor binding using PET scans in regard to emotional/social pain. Zubieta et al. (2003) conducted a study looking at changes in μ-opioid receptor binding in various brain regions when subjects were recalling a personal story that was sad versus when subjects were in a “neutral” state where they were merely asked to be aware of their physical sensations. This study found that in the sadness state there was a significant reduction of μ-opioid receptor binding compared to the neutral state in: the rostral anterior cingulate, ventral pallidum, amygdala, and inferior temporal cortex (Zubieta et al., 2003). In a similarly designed study, women with Major Depressive Disorder (MDD) and age and educational level matched control women were asked to think of a sad story during one scan, and be in a “neutral” state during another PET scan (Kennedy, Koeppe, Young, & Zubieta, 2006). This study demonstrated that women with MDD had significantly less endogenous μ-opioid receptor binding in the neutral state, and also had significantly less μ-opioid receptor binding in the left inferior temporal cortex. Matched control women had significantly more binding in the rostral ACC (Kennedy et al., 2006). More recently, a study demonstrated that social touch decreased endogenous μ-opioid receptor binding in the thalamus, striatum, cingulate cortex, insular cortex, and frontal cortex in men (Nummenmaa et al., 2016). The PET studies presented here provide a few examples of the burgeoning research investigating emotional aspects of pain. For more information on imaging and opioid receptors, see Henriksen and Willoch (2008).
Another laboratory has examined human response to social rejection while visualizing brain activity using PET scanning with [11C]carfentanil, a ligand that has high affinity for μ-opioid receptors (MOR; Hsu et al., 2013). The rejection manipulation was false feedback on personal dating profiles being considered for possible intimate relationships. Fake feedback given during the PET scan about his or her own profile was designed to generate rejection or acceptance. There were areas of the brain that were significantly activated during rejection compared to baseline, specifically the left and right amygdala, right ventral striatum in the area of the nucleus accumbens, midline thalamus, and PAG. The authors note that this pattern is similar to the response to physical pain. During the social acceptance phase, compared to baseline, higher activation was seen in the amygdala and anterior insula, and lower MOR activation in the midline thalamus and subgenual anterior cingulate cortex. There was higher activation during rejection blocks compared to acceptance blocks in the right ventral striatum, bilateral amygdala, midline thalamus in the area of the nucleus accumbens, subgenual ACC, and dorsal ACC. Hsu et al. (2013) caution against interpreting MOR and BOLD studies together because the relationship between MOR activation has not been precisely correlated with BOLD signal in fMRI studies.
To reiterate, sufficient research supports the involvement of opioid systems in social pain, not just physical pain. Controversies remain because of differing methods and interpretations among numerous studies. In addressing these controversies, Eisenberger (2015) concludes that the dACC may function as a type of neural alarm system, with its role in pain unpleasantness being primary (as a role in responding to threatening situations) and with a role in discrepancy detection/conflict monitoring being more recently developed evolutionarily. Further research with various paradigms is necessary to delineate pathways that are active during different emotional states. However, enough evidence has accumulated to reveal the potential impact of opiate drugs on the brain pathways subserving social attachment that it is not surprising that the addiction potential of such drugs is so strong. The social attachment system is important for humans and other primates.
Social Attachment in Primates
A new theory has been proposed about the importance of opioid transmission in social attachment in primates , including humans. Machin and Dunbar (2011) review comparative work on primate social grooming and mother–infant behavior. Studies with naloxone discovered that it increased grooming behavior in monkeys (Fabre-Nys, Meller, & Keverne, 1982; Meller, Keverne, & Herbert, 1980). Naloxone also led to an increase in distress calls in nonhuman primate infants (Kalin, Shelton, & Barksdale, 1988; Martel, Nevison, Simpson, & Keverne, 1995). These findings led Dunbar (2010) to theorize that social touch stimulates opioid release for anthropoid primates, including humans. Social touch has been shown to increase serum beta-endorphin in dogs—which are highly social—and people (Odendaal & Meintjes, 2003). Dunbar (2010) suggests that touch and group activities such as music, dancing, storytelling, and laughter may increase social bonding via endorphin release. Dunbar et al. (2016) refer to social activities in large groups as “grooming at a distance” (p. 10). The critical importance of social bonds to human survival (and reproduction) creates vulnerability to addiction when drugs mimic the natural neurotransmitters involved in brain pathways.
Could Humans Evolve a Brain that Is Less Prone to Opiate Addiction?
It is clear that the physical and social pain systems are essential for survival, and thus could never be eliminated by natural selection against addiction. The survival value of the physical pain system is obvious, but it is also clear that evolution could not act to remove our brain pathways related to reward and social attachment, the pathways that are hijacked by addictive substances. O’Connell and Hoffman (O’Connell & Hofmann, 2011a, 2011b) describe two ancient brain circuits present in vertebrates, the mesolimbic reward system and the social behavior network . These two circuits form part of a large social-decision-making network that is homologous among vertebrates (mammals, birds, reptiles, amphibians, and teleost fish; O’Connell & Hoffman, O’Connell & Hofmann, 2011b). These circuits subserve naturally rewarding behaviors such as sexual activity (O’Connell & Hofmann, 2011a). MacLean (1985) suggested that the evolution of vocalizations that maintain contact between mothers and offspring may be a key development in the evolution of mammals and that this capability may depend on pathways connecting the thalamus and the cingulate cortex.
Anthropoid primates, including humans, have extended long-term bonds beyond monogamous mating situations (Schultz & Dunbar, 2007). Social attachment has a unique role in human evolution in that social groups include nonrelatives with whom long-term cooperative reciprocal relationships are maintained (Machin & Dunbar, 2011). Because of this unique social system, Machin and Dunbar (2011) asserted that the “opioid system may play a more central role in sociality in primates (including humans) than in other mammalian taxa” (p. 985). They suggest that endogenous opioids are involved in maintaining stable long-term relationships (while relationship onset may be subserved by dopamine, serotonin, oxytocin, and vasopressin). Thus, our human complex social bonds are “emancipated” from hormonal control and are rather supported by higher cognitive abilities and may be maintained by brain opioid systems (reviewed by Machin & Dunbar, 2011). As stated by Machin and Dunbar (2011),
… the evidence seems to suggest that while non-primate mammals may utilize the endorphin system to maintain infant/mother and sexual pair bonds, primates (and hence humans) may rely to a much greater extent on this system to maintain the complex, diverse and enduring social networks that are uniquely characteristic of this order (p. 1014).
The human brain has an evolved vulnerability to addiction. The dopaminergic reward system and the social and physical pain pathways are essential for survival. Because these pathways operate using neurotransmitters, vulnerability to the effects of external chemicals is inherent. These susceptibilities are shared by all human beings. However, research has shown individual differences in risk for addiction. Some of the most important individual differences in risk to addiction will be reviewed.
Individual Differences in Vulnerability to Addiction
An evolutionary approach typically focuses on characteristics that are common to human beings as a species, Homo sapiens. However, an evolutionary perspective can also help illuminate some differences among humans. For example, demographic differences in patterns of alcohol problems follow similar gender and age patterns as do many risky behaviors (reviewed by Hill & Chow, 2002). Alcohol problems are most common for young men, whose rates of alcohol disorders are 3–4 times as high as for women. Onset of alcohol problems peaks during the ages 15–29. Hill and Chow (2002) examined risky drinking patterns using life-history theory, which is a subset of evolutionary theory. Life-history theory explains higher risk-taking propensity of young males as based in more intense competition for mates, where success in competition requires taking risks (Wilson & Daly, 1985).
Individual differences in risk-taking would have many sources. The risky behavior involved in alcohol intoxication or use of illegal substances is complex, and the motivational basis is multidimensional. Various areas of addiction research have used psychological concepts such as impulsivity and future orientation. Impulsivity has been separated statistically into two main components, cognitive and behavioral impulsivity (White et al., 1994).
Future discounting would correlate with risk-taking because of the way present versus future benefits and costs of a risky act are evaluated. When the future is devalued, both benefits and costs are given lesser weight when delayed, in an unconscious calculation underlying behavior. The present benefits and costs have more weight in a decision. This construct of future discounting fits into cognitive impulsivity or decision-making impulsivity noted above. Life history acceleration has been used to help explain health-related risk-taking versus health-promoting behaviors, a relationship that persists even after accounting for demographic factors (Kruger & Kruger, 2016).
Future discounting has been measured using monetary choices after delays. According to this assessment, steeper discounting of the future has been found among people with a history of addiction (e.g., Kirby, Petry, & Bickel, 1999; Vuchinich & Simpson, 1998). A lucid description of the methods and results of monetary discounting measurement is given in Kirby et al. (1999). Recently, researchers have proposed that delayed-reward discounting is a central feature of addiction (Bickel & Johnson, 2003; MacKillop et al., 2011). One prominent symptom of addictive behavior is the use of drugs (immediate temporary benefit) despite future costs due to such use and the loss of potential future benefits gained by remaining free of addiction. MacKillop et al. (2011) conducted a meta-analysis of 46 published studies with the purpose of comparing groups with addictive behavior to those without. They found a medium effect size (d = .58) for this comparison, which indicates that groups with addiction differ from those without addiction by about a half of a standard deviation in delay-discounting.
Specific to the topic of this chapter, Kirby and Petry (2004) compared individuals with addictions who were abstinent to those who were actively using substances. Lower discount rate was shown by a group previously addicted to heroin but currently abstinent, compared to current users. This study included only seven people in the abstinent group, however. This finding was replicated in a recent study wherein individuals in treatment for opiate addiction were tested for delay-discounting at baseline and 12 weeks later at the end of treatment (Landes, Christensen, & Bickel, 2012). The patients’ average delay-discounting became less steep over the course of treatment (which was buprenorphine).
A recent study with a sample of patients suffering from chronic pain assessed impulsivity as a risk factor for prescription opioid misuse (Vest, Reynolds, & Tragesser, 2016). They reported that two aspects of impulsivity did correlate with opioid misuse, which were the dimensions of urgency and sensation-seeking (but not lack of premeditation or lack of perseverance). Only urgency was a significant risk factor for future misuse (Vest et al., 2016). More research on urgency is warranted, because many existing studies focused on other aspects of impulsivity.
Individual differences may also occur through geographic variation in human populations. For some substance use disorders , such as Alcohol Use Disorder, differences in vulnerability have been found to exist based on the genetic predisposition of specific ethnic groups. An example of this is found in individuals of East Asian descent, where protective gene variants that affect alcohol metabolism cause flushing in response to alcohol consumption, and thus prevent binge drinking (Edenberg, 2007). Another example is found in specific Native American populations who have an increased prevalence of Alcohol Use Disorder, which is associated with unique gene variants that are also involved in alcohol metabolism (Mulligan et al., 2003). However, ethnicity-based vulnerabilities or protective effects have yet to be demonstrated in regard to Opiate Use Disorder. This is despite the fact that the use of opium-containing substances has been long standing in some parts of the world and relatively new in other parts of the world.
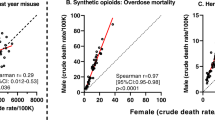
Opium is thought to have been originally used in cultural practices in the Middle East beginning between 3000–2000 B.C. (Brownstein, 1993). In contrast, it was not brought to China and India until around 700 A.D., and not to Europe until around 900–1200 A.D. (Brownstein, 1993). This geographic variation presents the possibility that populations that have used opiate derivatives for a long period of time could have evolved traits that are protective against addiction and/or other complications of opiate use, such as overdose death. An article on global epidemiology (Degenhardt et al., 2014) suggests that there are geographic differences in the consequences related to opioid use. Most startling are the years of life lost due to opioid use disorder. Of those regions that had a rate of years of life lost that was greater than 75 years per 100,000 people, the following had the highest, in order: South Sub-Saharan Africa, North America, Eastern Europe, and Australia (Degenhardt et al., 2014). This is in contrast to predominately Asian regions, where there were still high rates of disability due to Opioid Use Disorder, but years of life lost per 100,000 people was under 10 (Degenhardt et al., 2014). This pattern generally suggests that regions with large populations of Caucasians had more death due to opioid use. It would be interesting in future work to see if there are different ethnic vulnerabilities to mortality from opioids.
Geographic and ethnic variation in substance use point to potential genetic differences. It is beyond the scope of the current article to review genetic susceptibility to opiate addiction, however. Research is being conducted on a polymorphism in the μ-opioid receptor gene, OPRM1. One allele (G) has been associated with beta-endorphin sensitivity (Bond et al., 1998). Individuals with this allele showed high levels of rejection sensitivity in a laboratory social exclusion experiment, with greater dACC and AI activation (Way, Taylor, & Eisenberger, 2009). Recent studies indicate possible associations of opioid addiction with OPRMI and also markers related to the δ-opioid receptor (OPRD1), galanin (GAL), and one related to ATP (ABCB1) (reviewed in Beer et al., 2013). Nevertheless, there is as yet no consensus on various candidate genes in vulnerability to addiction, due to inconsistent results between studies (Beer et al., 2013).
Based upon our previous discussion of the importance to survival of the brain pathways relevant to opiate addiction, human vulnerability to addiction cannot be eliminated by evolution nor by human invention. The impact of substance use on sufferers and society could be reduced. Efforts to stem the flood of prescription opioids were mentioned earlier. Effective approaches to treating addiction have been developed. Current treatment approaches combine medication with psychotherapy. It appears that successful treatment is associated with changes in future discounting, described above as a risk factor and correlate of substance use. A brief review of current treatment approaches will be given next.
Current Treatment Approaches for Opioid Use Disorder
Although human vulnerability to addiction cannot be eliminated, its impact could be reduced. Current treatment approaches combine medication with psychotherapy. Medication-Assisted Treatment replacement therapies are demonstrated as more efficacious than psychotherapy alone when treating OUD (e.g., Mattick, Breen, Kimber, & Davoli, 2009; Mattick et al., 2013).
OUD treatment options include methods of harm reduction (Seiger, 2014), tapered withdrawal, and medication-assisted treatment (MAT; CSAT, 2005). Optimal treatment options are established based upon a thorough biopsychosocial assessment of multiple patient-specific factors: (a) one’s readiness for change (DiClemente, 2003); (b) medical issues (e.g., HIV status, hepatitis A, B, or C, and liver cirrhosis); (c) other substance use disorders; (d) psychological factors (e.g., co-occurring and/or substance induced disorders) characteristically depressive, anxiety, and personality disorders; (e) vocational status (i.e., employment history and educational status); (e) legal status (e.g., incarcerated, probation, or parole); and (f) status of family (e.g., child custody) and other significant relationships (e.g., living with others with OUD; CSAT, 2005).
Harm Reduction
Harm reduction (HR) is a treatment approach that recognizes a number of individuals with OUD have no desire to stop, are ambivalent, or view themselves as incapable of discontinuing use (DiClemente, 2003). HR approaches seek to minimize harm to the opioid user and the community at large. Examples of HR include needle exchange programs, healthcare outreach, education about cleaning used needles with bleach, strategies to avoid a drug overdose, and access and knowledge about naloxone (Narcan) and its ability to reverse acute opioid overdose (CSAT, 2005). The philosophy is to meet patients where “they’re at” with the long-term goal of providing treatment when patients are ready to change their drug-using behavior (Seiger, 2014).
Medically Supervised Withdrawal
Those not eligible for MAT (e.g., OUD < 1 year; a minor i.e., <17 years old) or who prefer remaining medication free can opt for medically assisted withdrawal , which detoxifies the patient gradually with a process referred to as “ tapering” (CSAT, 2005). Tapering is performed with either methadone (an opioid agonist) or buprenorphine (an opioid partial-agonist) short-term (i.e., ≤30 days) or long-term (i.e., ≤180 days). Federal regulations stipulate that two unsuccessful detoxification attempts in 1 year necessitate consideration of an alternative treatment option (CSAT, 2005).
Tapering
Tapering is a process whereby a gradual reduction in the dosage of methadone. Patients are informed about the salience and effects of individual differences and other variables in the tapering process, such as body weight, drug absorption, and individual metabolism and acquired opioid tolerance, which can affect their course of treatment (CSAT, 2005). Methadone doses are typically reduced in 5–10% increments every 1–2 weeks. Patients tapering from methadone typically experience reduction of opioid withdrawal symptoms; however, the final stages of tapering require an inevitable experience of discomfort. This may increase patient risk for opioid relapse and/or use of other drugs such as benzodiazepines, alcohol, and cocaine to ameliorate their remaining symptoms. Given that 80% of tapered patients return to opioid abuse, it is imperative that patients develop robust relapse prevention skills in addition to extensive sober and social supports (CSAT, 2005).
Outpatient Treatment Programs (OTPs)
OTPs provide a range of treatment options for a diverse range of individuals with OUD onsite and in collaboration with other community agencies. Patients deemed appropriate for OTPs should meet Federal and State requirements for opioid treatment and in addition, have previously failed a medically supervised withdrawal; or participate in a residential treatment setting; or require a long-term MAT stabilization. Hospital-based OTPs typically provide access to both medical and psychosocial services, which increase the prospects of patient compliance and successful treatment outcome (CSAT, 2005).
Residential Programs
MAT residential programs are recommended for patients who can benefit from structured stabilization and robust sober supports that address both their physical and psychological well-being (CSAT, 2005).
Community Self-Help
Self-help fellowships otherwise known as 12-step programs provide community-wide support for individuals with OUD. Narcotics Anonymous (NA) was fashioned after Alcoholics Anonymous in the late 1940s (NA, 2016) and supported individuals with alcohol and other drug problems. However, Bulletin 29# (NA, 2016) published in 1996 established that individuals on replacement therapy (i.e., MAT) were welcome to attend NA meetings but not to actively participate. Methadone Anonymous is a reported alternative that supports individuals in attempting or in sustained remission for OUD through MAT or maintenance (CSAT, 2005).
Therapeutic Communities
Historically, therapeutic communities (TC) such as Synanon in California were long-term residential treatment centers facilitated by staff typically in recovery from OUD themselves. The aim of TCs is to return individuals to successful drug free lifestyles that lead either to an effective return to the outside community or a transition within the Synanon community (Friedman, 2014).
Medication-Assisted Treatment (MAT)
OUD treatment is a dynamic, intentional, time-dependent process with characteristic fits and starts punctuated by substantial levels of patient ambivalence. This is the norm. It is often difficult for outsiders (i.e., those non-addicted) to appreciate, especially when a patient’s life is in total shambles, that there is any reluctance at all in escaping the grip of OUD. Although an in-depth discussion of recovery is beyond the scope of this chapter, we provide a brief overview of the phases of Medication-Assisted Treatment (MAT) to give the reader a sense of the complexity of both the physiological and psychological aspects of OUD experienced by individuals in search of OUD recovery. Federal and state regulations must be followed in the United States to offer MAT, which inopportunely limit the number of opioid treatment programs (OTP) and qualified physicians available to prescribe methadone and buprenorphine for medication replacement purposes (see CSAT, 2005).
Stages of Comprehensive Medication-Assisted Treatment (MAT)
Successful MAT (i.e., with methadone or buprenorphine) is blended with evidence-based therapies, such as cognitive behavioral therapy (Beck, Wright, Newman, & Liese, 1993), motivational interviewing (Miller & Rollnick, 2002), and the transtheoretical model (i.e., stages of change; DiClemente, 2003) in combination with social supports (e.g., community self-help, family, church), which afford individuals the optimal success in cessation of OUD.
Clinicians recognize six phases of MAT—acute, rehabilitative, supportive-care, medical maintenance, tapering and readjustment, and continuing care (CSAT, 2005). The acute phase can range from several days to months, and entails the cessation of all opioid use, including any other drugs abused by the patient. Therapeutic maintenance medication (i.e., methadone or buprenorphine) is initiated to suppress patient symptoms of the withdrawal syndrome and incessant drug craving.
In the rehabilitative phase referrals are made to appropriate supportive services determined at assessment to enhance and address unsuccessful functioning in patients’ other major life areas (e.g., co-occurring disorders, activities of daily living, medical, social, employment, legal, family). This phase is essential to reducing patient anxiety, depression, and other salient impediments that allow establishing a firm footing in early recovery. Furthermore, the rehabilitative phase advances opportunities to engage patients in community-based recovery (e.g., 12-step programs) and faith-based organizations. In conjunction with formal treatment, these organizations can provide social support, teach patients to identify personal high-risk situations and emotional states, and develop a manner of daily living that promotes substance free living (CSAT, 2005).
Supportive care and medical maintenance phases involve progressively longer periods where patients may take medication at home rather than at a clinical site, progressing to a 30-day supply of medication. Progression in treatment is verified with routine drug tests (CSAT, 2005). The tapering and readjustment phase involves reducing one’s medication dosage over time with the goal of forgoing medication altogether. Tapering and continued medication maintenance are both considered appropriate treatment goals; however, the risk for relapse increases significantly for those who cease medication (CSAT, 2005). The continuing care phase follows a patient’s successful tapering and readjustment to living medication free. Ongoing treatment is highly recommended owing to the chronicity of OUD and perpetual risk of relapse for some patients.
Given the evidence that physical and emotional pain share brain substrates, it is logical to assume that successful OUD treatment necessarily consists of medication, psychological, and social supportive interventions. Unfortunately, a disproportionate focus is placed on medication to the exclusion of other psychological and social services. Emotional stress is a well-known and documented relapse trigger in nearly all SUDs, and research on opioids and social pain suggests that attention to treatment of emotional cues be as important, if not more important, especially for those whose treatment goal is eventual tapering to a non-medicated recovery state.
Conclusion
Panksepp et al. (2002) noted that social interactions and drug addictions utilize common brain pathways. They suggested that drugs trick animals into associating stimulation of the social brain pathways with drug stimuli. Understanding the social pain aspect can help us understand why opiates are so addicting. Reducing social pain as well as physical pain feels better than pain patients might expect. Treatment programs need to replace the reinforcing good feelings given by the drug, mimicking social connection. The stereotypical idea is that opiates are for physical pain, but we now know that much of the power of opiate addiction is about emotional pain.
Only recently have researchers started to understand the common basis of social and physical pain as a risk factor for drug addiction (LeBlanc, McGinn, Itoga, & Edwards, 2015). LeBlanc et al. (2015) proposed that pain pathway sensitization by stress may create greater risk for addiction through increasing pain unpleasantness (i.e., the affective dimension of pain). In one study of former opioid-dependent individuals who had attained abstinence, variation in sensitivity to physical pain correlated with the level of craving they reported to opioid cues (Ren, Shi, Epstein, & Wang, 2009). Pain-induced distress was the critical factor, not simply level of pain (Ren et al., 2009). Edwards et al. (2011) found that individual differences in pain sensitivity predicted opioid misuse among chronic pain patients. LeBlanc et al. (2015) reviewed preclinical animal studies showing pain-induced sensitization in the ACC and the central amygdala, which they speculate might underlie addiction liability to pain relief medication. More research is needed on affective dimensions of pain and pain relief.
Treatment programs need to focus more on ameliorating social pain during recovery from opiate addiction. Social attachment is a human universal. Heilig, Epstein, Nader, and Shaham (2016) acknowledge that neuroscience research on addiction has had insufficient impact on clinical treatment. Social integration has rarely been included as a measured or manipulated variable in animal studies of addiction neurobiology. Social stressors that trigger relapse for people are difficult to model in laboratory settings, such as family conflicts or social ostracism (Heilig et al., 2016). Heilig et al. (2016) discuss the role of social exclusion in addiction and recovery, “Improving the social integration of drug users through opportunities for housing, jobs and meaningful relationships is therefore not merely a nonspecific intervention but rather a neurobiologically specific and critically important way to decrease drug use” (p. 4).
This review has mentioned research that indicates risk factors for addiction, and some of these are potential targets of future research. One is future discounting and impulsivity. Another is gender differences. There is evidence from brain imaging that there are gender differences in the opioid system of the brain, from a study with women tested twice at two menstrual phases and with a manipulation of estrogen level by an estrogen patch (Smith et al., 2006). During estrogen administration, mu-receptor binding increased 15–32% in the target brain regions. MRI results correlated with individual subjective ratings of pain (Smith et al., 2006). This finding calls for further research in gender differences in all subjective and physical aspects of pain.
Another potential source of individual differences in vulnerability is trauma. A study of military veterans who had experienced trauma detected changes in opioid receptor binding under PET scanning (Liberson et al., 2007). Those with post-traumatic stress disorder had lower binding specifically in the ACC (Liberson et al., 2007). Lower binding might indicate a lower or depleted ability to process social connection, which might enhance vulnerability to opiates. More research on social losses and vulnerability to addiction is needed.
Variations in sensitivity to loss and activity in the “PANIC” emotional system may be viable indicators of vulnerability to opiate addiction. Eisenberger (2012) describes various individual differences that correlate with increased propensity to feel social pain, all of which might be researchable risk factors for opiate addiction. These included low self-esteem, anxious attachment, and interpersonal sensitivity (reviewed by Eisenberger, 2012).
Panksepp et al. (2002) speculated that, “If adequate social bonds fail to develop, an individual may show an altered future tendency to engage emotional brain systems through other (e.g., pharmacological) means …” (p. 461). It would behoove social scientists to assess patterns in contemporary society that appear to reflect general weakening of social bonds (Putnam, 2001). Kinship and community networks are less tightly enveloping of people than in past decades, leading to fewer routine social gatherings, joint volunteering efforts, regular group meetings, or other activities that automatically reinforce social connection. Putnam (2001) referred to these experiences as building a person’s social capital, a storehouse of social resources. Instead, we now spend less time engaged in face-to-face socialization and communication, and more in long-distance internet communication. Virtual communities on the internet, while attractive to people, do not foster the same sense of community commitment and social support given by an in-person network of relatives and close friends (Song, 2009). If a progressive widespread weakening of social bonds continues, it will present an increasing risk for vulnerability to the psychological effects of opiates.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5 th edition): DSM-5. Arlington, VA: American Psychiatric Association.
Apkarian, A. V., Bushnell, M. C., Treede, R. D., & Zubieta, J. K. (2005). Human brain mechanisms of pain perception and regulation in health and disease. European Journal of Pain, 9(4), 463–463.
Baumgärtner, U., Buchholz, H. G., Bellosevich, A., Magerl, W., Siessmeier, T., Rolke, R., … Schreckenberger, M. (2006). High opiate receptor binding potential in the human lateral pain system. NeuroImage, 30(3), 692–699.
Beck, A. K., Wright, F. D., Newman, C. F., & Liese, B. S. (1993). Cognitive therapy of substance abuse. New York: Guilford Press.
Beer, B., Erb, R., Pavlic, M., Ulmer, H., Giacomuzzi, S., Riemer, Y., & Oberacher, H. (2013). Association of polymorhphisms in pahrmacogenetic candidate genes (OPRD1, GAL, ABCB1, OPRM1) with opioid dependence in European population: A case-control study. PloS One, 9(9), e75359.
Berridge, K. C. (1996). Food reward: Brain substrates of wanting and liking. Neuroscience and Biobehavioral Reviews, 20(1), 1–25.
Bickel, W. K., & Johnson, M. W. (2003). Delay discounting: A fundamental behavioral process of drug dependence. In G. Loewenstein, D. Read, & R. Baumeister (Eds.), Time and decision: Economic and psychological perspectives on intertemporal choice (pp. 419–440). New York, NY: Russell Sage.
Bohnert, A. S. B., Valenstein, M., Bair, M. J., Ganoczy, D., McCarthy, J. F., Ilgen, M. A., & Blow, F. C. (2011). Association between opioid prescribing patterns and opioid overdose-related deaths. Journal of the American Medical Association, 305, 1315–1321.
Bond, C., LaForge, K. S., Tian, M., Melia, D., Zhang, S., Borg, L., … Tischfield, J. A. (1998). Single-nucleotide polymorphism in the human mu opioid receptor gene alters beta-endorphin binding and activity: Possible implications for opiate addiction. Proceedings of the National Academy of Sciences, USA, 95, 9608–9613.
Branchi, I., Santucci, D., & Alleva, E. (2001). Ultrasonic vocalisation emitted by infant rodents: A tool for assessment of neurobehavioural development. Behavioural Brain Research, 125, 49–56.
Brownstein, M. J. (1993). A brief history of opiates, opioid peptides, and opioid receptors. Proceedings of the National Academy of Sciences, 90(12), 5391–5393.
Center for Substance Abuse Treatment (CSAT). (2005). Medication assisted treatment for opioid addiction in opioid addiction programs (treatment improvement protocols [TIP] series 43, [SMA] 05–4018). Rockville, MD: SAMHSA.
Centers for Disease Control and Prevention. (2016). Injury prevention & control: Opioid overdose. Retrieved December 20, 2016, from https://www.cdc.gov/drugoverdose/.
Cicero, T. J., Ellis, M. S., Surratt, H. L., & Kurtz, S. P. (2014). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry, 71(7), 821–826.
Degenhardt, L., Charlson, F., Mathers, B., Hall, W. D., Flaxman, A. D., Johns, N., & Vos, T. (2014). The global epidemiology and burden of opioid dependence: Results from the global burden of disease 2010 study. Addiction, 109(8), 1320–1333.
DiClemente, C. C. (2003). Addiction and change: How addictions develop and addicted people recover. New York: Guilford Press.
Dodrill, C. L., Helmer, D. A., & Kosten, T. R. (2011). Prescription pain medication dependence. American Journal of Psychiatry, 168(5), 466–471.
Dunbar, R. I. M. (2010). The social role of touch in humans and primates: Behavioral function and neurobiological mechanisms. Neuroscience and Biobehavioral Reviews, 34, 260–268.
Dunbar, R. I. M., Teasdale, B., Thompson, J., Budelmann, F., Duncan, S., van Emde Boas, E., & Maguire, L. (2016). Emotional arousal while watching drama increases pain threshold and social bonding. Royal Society Open Science, 3, 160288.
Edenberg, H. J. (2007). The genetics of alcohol metabolism: Role of alcohol dehydrogenase and aldehyde dehydrogenase variants. Alcohol Research & Health, 30(1), 5–14.
Edwards, R. R., Wasan, A. D., Michna, E., Greenbaum, S., Ross, E., & Jamison, R. N. (2011). Elevated pain sensitivity in chronic pain patients at risk for opioid misuse. The Journal of Pain, 12, 953–963.
Eisenberger, N. I. (2012). The pain of social disconnection: Examining the shared neural underpinnings of physical and social pain. Nature Reviews: Neuroscience, 13, 421–434.
Eisenberger, N. I. (2015). Social pain and the brain: Controversies, questions, and where to go from here. Annual Review of Psychology, 66, 601–629.
Eisenberger, N. I., Lieberman, M. D., & Williams, K. D. (2003). Does rejection hurt? An fMRI study of social exclusion. Science, 302, 290–292.
Fabre-Nys, C., Meller, R. E., & Keverne, E. B. (1982). Opiate antagonists stimulate affiliative behaviour in monkeys. Pharmacology, Biochemistry, and Behavior, 16(4), 653–659.
Filliol, D., Ghozland, S., Chluba, J., Martin, M., Matthes, H. W., Simonin, F., … Kieffer, B. L. (2000). Mice deficient for δ-and μ-opioid receptors exhibit opposing alterations of emotional responses. Nature Genetics, 25(2), 195–200.
Food & Drug Administration (FDA). (2016). FDA requires strong warnings for opioid analgesics, prescription opioid cough products, and benzodiazepine labeling related to serious risks and death from combined use. Retrieved December 20, 2016, from, http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm518697.htm.
Friedman, E. G. (2014). Assessment and treatment of individuals dependent on opioids. In S. L. Ashenberg Straussner (Ed.), Clinical work with substance-abusing clients (pp. 88–109). New York: Guilford Press.
Goldstein, A. (1987). Binding selectivity profiles for ligands of multiple receptor types: Focus on opioid receptors. Trends in Pharmacological Sciences, 8(12), 456–459.
Green, T. C., Black, R., Serrano, J. M. G., Budman, S. H., & Butler, S. F. (2011). Typologies of prescription opioid use in a large sample of adults assessed for substance abuse treatment. PloS One, 6(11), e27244.
Heilig, M., Epstein, D. H., Nader, M. A., & Shaham, Y. (2016). Time to connect: Bringing social context into addiction neuroscience. Nature Reviews: Neuroscience, 17(9), 592. doi:10.1038/nrn.2016.67.
Henriksen, G., & Willoch, F. (2008). Imaging of opioid receptors in the central nervous system. Brain, 131, 1171–1196.
Hill, E. M., & Chow, K. (2002). Life-history theory and risky drinking. Addiction, 97, 401–413.
Hsu, D. T., Sanford, B. J., Meyers, K. K., Love, T. M., Hazlett, K. E., Wang, H., … Zubieta, J.-K. (2013). Response of the μ-opioid system to social rejection and acceptance. Molecular Psychiatry, 18, 1211–1217.
Kalin, N. H., Shelton, S. E., & Barksdale, C. M. (1988). Opiate modulation of separation-induced distress in non-human primates. Brain Research, 440, 285–292.
Kennedy, S. E., Koeppe, R. A., Young, E. A., & Zubieta, J. K. (2006). Dysregulation of endogenous opioid emotion regulation circuitry in major depression in women. Archives of General Psychiatry, 63(11), 1199–1208.
Kirby, K. N., & Petry, N. M. (2004). Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction, 99, 461–471.
Kirby, K. N., Petry, N. M., & Bickel, W. K. (1999). Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General, 128, 78–87.
Kross, E., Berman, M. G., Mischel, W., Smith, E. E., & Wager, T. D. (2011). Social rejection shares somatosensory representations with physical pain. PNAS, 108(15), 6270–6275.
Kruger, D. J., & Kruger, J. S. (2016). Psychometric assessment of human life history predicts health related behaviors. Psychological Topics, 25, 19–28.
Landes, R. D., Christensen, D. R., & Bickel, W. K. (2012). Delay discounting decreases in those completing treatment for opioid dependence. Experimental and Clinical Psychopharmacology, 20(4), 302–309.
LeBlanc, D. M., McGinn, M. A., Itoga, C. A., & Edwards, S. (2015). The affective dimension of pain as a risk factor for drug and alcohol addiction. Alcohol, 49, 803–809.
Liberson, I., Taylor, S. F., Phan, K. L., Britton, J. C., Fig, L. M., Bueller, J. A., … Zubieta, J.-K. (2007). Altered central mu-opioid receptor binding after psychological trauma. Biological Psychiatry, 61, 1030–1038.
Lutz, P. E., & Kieffer, B. L. (2013a). Opioid receptors: Distinct roles in mood disorders. Trends in Neurosciences, 36(3), 195–206.
Lutz, P. E., & Kieffer, B. L. (2013b). The multiple facets of opioid receptor function: Implications for addiction. Current Opinion in Neurobiology, 23(4), 473–479.
Machin, A. J., & Dunbar, R. I. M. (2011). The brain opioid theory of social attachment: A review of the evidence. Behaviour, 148, 985–1025.
MacLean, P. D. (1985). Brain evolution relating to family, play, and the separation call. Archives of General Psychiatry, 42, 405–417.
MacKillop, J., Amlung, M. T., Few, L. R., Ray, L. A., Sweet, L. H., & Munafo, M. R. (2011). Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology, 216, 305–321.
Mansour, A., Fox, C. A., Burke, S., Meng, F., Thompson, R. C., Akil, H., & Watson, S. J. (1994). Mu, delta, and kappa opioid receptor mRNA expression in the rat CNS: An in situ hybridization study. Journal of Comparative Neurology, 350(3), 412–438.
Martel, F. L., Nevison, C. M., Simpson, M. J. A., & Keverne, E. B. (1995). Effects of opioid receptor blockade on the social behavior of rhesus monkeys living in large family groups. Developmental Psychobiology, 28, 71–84.
Mattick, R. P., Ali, R., White, J. M., O’Brien, S., Wolk, S., & Danz, C. (2013). Buprenorphine versus methadone maintenance therapy: A randomized double-blind trial with 405 opioid-dependent patients. Addiction, 98, 441–452.
Mattick, R. P., Breen, C., Kimber, J., & Davoli, M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database of Systematic Reviews Issue, 3. doi:10.1002/14651858.CD002209.pub2.
Meller, R. E., Keverne, E. B., & Herbert, J. (1980). Behavioural and endocrine effects of naltrexone in male talapoin monkeys. Pharmacology, Biochemistry, and Behavior, 13, 663–672.
Mestek, A., Chen, Y., & Yu, L. (1996). Mu opioid receptors: Cellular action and tolerance development. NIDA Research Monographs, 161, 104–126.
Meyer, J. S., & Quenzer, L. F. (2013). Psychopharmacology: Drugs, the brain, and behavior. Sunderland, NY: Sinauer.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people for change (2nd ed.). New York: Guilford Press.
Mulligan, C. J., Robin, R. W., Osier, M. V., Sambuughin, N., Goldfarb, L. G., Kittles, R. A., … Long, J. C. (2003). Allelic variation at alcohol metabolism genes (ADH1B, ADH1C, ALDH2) and alcohol dependence in an American Indian population. Human Genetics, 113(4), 325–336.
Narcotics Anonymous (NA) World Services. (2016). Bulletin #29: Regarding methadone and other drug replacement programs. Retrieved 20 December, from https://www.na.org/?ID=bulletins-bull29.
Nelson, E. E., & Panksepp, J. (1998). Brain substrates of infant-mother attachment: Contributions of opioids, oxytocin and norepinephrine. Neuroscience and Biobehavioral Reviews, 22, 437–452.
Nesse, R. M. (2016). Evolutionary psychology and mental health. In D. M. Buss (Ed.), The handbook of evolutionary psychology: Volume 2 integrations (2nd ed.pp. 1007–1026). New York, NY: Wiley.
Nesse, R. M., & Berridge, K. C. (1997). Psychoactive drug use in evolutionary perspective. Science, 278, 63–66.
Nestler, E. J., Hyman, S. E., & Malenka, R. C. (2009). Molecular neuropharmacology: A foundation for clinical neuroscience (2nd ed.). New York, NY: McGraw-Hill.
Noirot, E. (1972). Ultrasounds and maternal behavior in small rodents. Developmental Psychobiology, 5, 371–387.
Novak, S. P., Håkansson, A., Martinez-Raga, J., Reimer, J., Krotki, K., & Varughese, S. (2016). Nonmedical use of prescription drugs in the European Union. BMC Psychiatry, 16, 274. doi:10.1186/s12888-016-0909-3.
Nummenmaa, L., Tuominen, L., Dunbar, R., Hirvonen, J., Manninen, S., … Sams, M. (2016). Social touch modulates endogenous μ-opioid system activity in humans. NeuroImage, 138, 242–247.
O’Connell, L. A., & Hofmann, H. A. (2011a). Genes, hormones, and circuits: An integrative approach to study the evolution of social behavior. Frontiers in Neuroendocrinology, 32, 320–335.
O’Connell, L. A., & Hofmann, H. A. (2011b). The vertebrate mesolimbic reward system and social behavior network: A comparative synthesis. The Journal of Comparative Neurology, 519, 3599–3639.
Odendaal, J. S. J., & Meintjes, R. A. (2003). Neurophysiological correlates of affiliative behavior between humans and dogs. The Veterinary Journal, 165, 296–301.
Okon, E. E. (1970). The effect of environmental temperature on the production of ultrasounds by isolated non-handled albino mouse pups. Journal of Zoology. London, 162, 71–83.
Olds, J. (1977). Drives and reinforcements: Behavioral studies of hypothalamic functions. New York: Raven Press.
Palomar, J. J., Shearston, J. A., Dawson, E. W., Mateu-Gelabert, P., & Ompad, D. C. (2016). Nonmedical opioid use and heroin use in a nationally representative sample of high school seniors. Drug and Alcohol Dependence, 158, 132–138.
Panksepp, J. (1998). Affective neuroscience. New York, NY: Oxford University Press.
Panksepp, J. (2003). Feeling the pain of social loss. Science, 302, 237–239.
Panksepp, J., Bean, N. J., Bishop, P., Vilberg, T., & Sahley, T. L. (1980). Opioid blockade and social comfort in chicks. Pharmacology, Biochemistry and Behavior, 13, 673–683.
Panksepp, J., Herman, B. H., Conner, R., Bishop, P., & Scott, J. P. (1978). The biology of social attachments: Opiates relieve separation distress. Biological Psychiatry, 13, 607–613.
Panksepp, J., Knutson, B., & Burgdorf, J. (2002). The role of brain emotional systems in addictions: A neuro-evolutionary perspective and a new ‘self-report’ animal model. Addiction, 97, 459–469.
Peckys, D., & Landwehrmeyer, G. B. (1999). Expression of mu, kappa, and delta opioid receptor messenger RNA in the human CNS: A 33 P in situ hybridization study. Neuroscience, 88(4), 1093–1135.
Price, D. D. (2000). Psychological and neural mechanisms of the affective dimension of pain. Science, 288(5472), 1769–1772.
Price, D. D. (2002). Central neural mechanisms that interrelate sensory and affective dimensions of pain. Molecular Interventions, 2(6), 392.
Putnam, R. D. (2001). Bowling alone: The collapse and revival of American community. New York, NY: Simon and Schuster.
Ren, Z.-Y., Shi, J., Epstein, D. H., & Wang, J. (2009). Abnormal pain response in pain-sensitive opiate addicts after prolonged abstinence predicts increased drug craving. Psychopharmacology, 204, 423–429.
Robinson, T. E., & Berridge, K. C. (1993). The neural basis of drug craving: An incentive-sensitization view. Addiction, 95(Suppl. 2), S91–S117.
Schultz, S., & Dunbar, R. I. M. (2007). The evolution of the social brain: Anthropoid primates contrast with other vertebrates. Proceedings of the Royal Society, Series B, 274, 2429–2436.
Seiger, B. (2014). The clinical practice of harm reduction psychotherapy. In S. L. A. Straussner (Ed.), Clinical work with substance-abusing clients (pp. 165–178). New York, NY: Guilford Press.
Sewell, G. D. (1970). Ultrasonic communication in rodents. Nature (London), 227(256), 410.
Shayit, M., Nowak, R., Keller, M., & Weller, A. (2003). Establishment of a preference by the newborn lamb for its mother: The role of opioids. Behavioral Neuroscience, 117, 446–454.
Shippenberg, T. S. (1993). Motivational effects of opioids. InOpioids II. Berlin Heidelberg: Springer.
Smith, Y. R., Stohler, C. S., Nichols, T. E., Bueller, J. A., Koeppe, R. A., & Zubieta, J. K. (2006). Pronociceptive and antinociceptive effects of estradiol through endogenous opioid neurotransmission in women. Journal of Neuroscience, 26, 5777–5785.
Song, F. W. (2009). Virtual communities: Bowling alone, online together. New York, NY: Peter Lang.
Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality (SAMHSA). (2014). The NSDUH report: Substance use and mental health estimates from the 2013 national survey on drug use and health: Overview of findings. Rockville, MD. Retrieved from http://archive.samhsa.gov/data/2k14/NSDUH200/sr200-findings-overview-2014.pdf
Vest, N., Reynolds, C. J., & Tragesser, S. L. (2016). Impulsivity and risk for prescription opioid misuse in a chronic pain patient sample. Addictive Behaviors, 60, 184–190.
Volkow, N. D. (2014). America’s addiction to opioids: Heroin and prescription drug abuse. Senate Caucus on International Narcotics Control. Washington, DC.
Vuchinich, R. E., & Simpson, C. A. (1998). Hyperbolic temporal discounting in social drinkers and problem drinkers. Experimental and Clinical Psychopharmacology, 6, 292–305.
Way, B. M., Taylor, S. E., & Eisenberger, N. I. (2009). Variation in the mu-opioid receptor gene (OPRM1) is associated with dispositional and neural sensitivity to social rejection. Proceedings of the National Academy of Sciences, USA, 106, 15079–15084.
White, J. L., Moffitt, T. E., Caspi, A., Bartusch, D. J., Needles, D. J., & Stouthamer-Loeber, M. (1994). Measuring impulsivity and examining its relationship to delinquency. Journal of Abnormal Psychology, 103(2), 192–205.
Wilson, M., & Daly, M. (1985). Competitiveness, risk taking, and violence: The young male syndrome. Ethology and Sociobiology, 6, 59–73.
Wright, E. R., Kooreman, H. E., Greene, M. S., Chambers, R. A., Banerjee, A., & Wilson, J. (2014). The iatrogenic epidemic of prescription drug abuse: County-level determinants of opioid availability and abuse. Drug and Alcohol Dependence, 138, 209–215.
Yoo, J. H., Lee, S. Y., Loh, H. H., Ho, I. K., & Jang, C. G. (2004). Altered emotional behaviors and the expression of 5-HT1A and M1 muscarinic receptors in μ-opioid receptor knockout mice. Synapse, 54(2), 72–82.
Zubieta, J. K., Ketter, T. A., Bueller, J. A., Xu, Y., Kilbourn, M. R., … Koeppe, R. A. (2003). Regulation of human affective responses by anterior cingulate and limbic μ-opioid neurotransmission. Archives of General Psychiatry, 60(11), 1145–1153.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Hill, E.M., Hunt, L., Duryea, D.G. (2017). Evolved Vulnerability to Addiction: The Problem of Opiates. In: Shackelford, T., Zeigler-Hill, V. (eds) The Evolution of Psychopathology. Evolutionary Psychology. Springer, Cham. https://doi.org/10.1007/978-3-319-60576-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-60576-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-60575-3
Online ISBN: 978-3-319-60576-0
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)