Abstract
This review depicts the common variations in imaging appearances of biliary and pancreatic malignancies on FDG PET/CT. Pitfalls and artefacts arising due to treatment-related complications are also described.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
5.1 Introduction
FDG PET/CT is being increasingly used in the evaluation of biliary tract and pancreatic malignancies. Gall bladder cancer and cholangiocarcinoma constitute biliary tract malignancies. Pancreatic adenocarcinoma is frequently staged using FDG PET/CT. The varying histologies and presentations of these tumours give rise to a wide range of normal appearances on FDG PET/CT. Several treatment options like biliary drainage, stenting, surgery, radiation and chemotherapy are used to treat hepatobiliary and pancreatic cancers which produce various tissue changes and can lead to pitfalls and artefacts on PET/CT. Correct and timely recognition of these tissue changes and associated treatment-related complications is important in avoiding diagnostic pitfalls.
5.2 Variations in Imaging Appearance Due to Anatomy and Histology
Cholangiocarcinoma can show variable FDG uptake depending upon the anatomic location, growth pattern and histological subtype [1,2,3]. Lesions that are extrahepatic, infiltrative and mucinous in nature tend to show poor or no FDG concentration and can be difficult to localise on PET studies leading to false-negative results (Fig. 5.1). Dilatation of the biliary tree and its pattern on CT are often indirect signs that reveal the site of the lesion (Fig. 5.2). Images acquired at a delayed time point can also help by augmenting the FDG uptake in the lesion (Fig. 5.2).
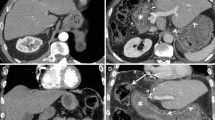
Poor FDG concentrating cholangiocarcinomas. Axial CT and fused PET/CT images shows a diffusely infiltrative type of cholangiocarcinoma showing low-grade FDG uptake (arrows in a, b). Axial CT and fused PET/CT images show extremely poor concentration of FDG in a diffuse mucinous type of cholangiocarcinoma (arrows in c, d)
Poor FDG concentrating GB neck and cystic duct malignancy. Coronal MIP and fused PET/CT images (arrows in a, c) do not show significant FDG concentration in a stricturous lesion involving the neck of the GB and the cystic duct (arrow in b). Surgical resection revealed a mucin-producing adenocarcinoma
Cystic neoplasms of the pancreas include serous cystadenoma, mucinous cystadenoma and intraductal pancreatic neoplasms (IPMN). IMPNs are mucin-producing neoplasms that can be benign or invasive carcinomas, and FDG PET very often is used to differentiate between them [4]. Mucinous nature of these tumours causes poor avidity of FDG on PET studies (Fig. 5.3) more so in patients with a tiny malignant focus.
Poor FDG concentration in intraductal papillary mucinous neoplasm of pancreas. Axial CT scan shows a lobulated cystic mass arising from the pancreatic body (arrow in a) causing atrophy of the distal pancreatic body and tail (arrowhead in a, c). Axial PET and fused FDG PET/CT reveal no FDG uptake in the lesion. Histopathology after surgical resection showed IPMN with invasive features
5.3 Inflammatory Pathology Mimicking Malignancy
Mass-forming pancreatitis (MFP) resembles pancreatic adenocarcinoma on CT scan, and differentiating one from the other can be challenging. FDG PET/CT has been found to be better in distinguishing MFP from pancreatic adenocarcinoma by virtue of lower tracer uptake in the inflammatory lesion [5, 6]. However, certain cases of MFP can show high FDG avidity due to the inflammatory process and can simulate malignancy (Fig. 5.4).
Gall bladder wall thickening can be because of benign causes like inflammation and adenomyosis or due to malignancy. FDG PET can be falsely positive in cases of cholecystitis, and differentiation from malignancy can be difficult [7, 8]. Mass-like or protuberant lesions are more likely to be due to malignancy. Diffuse and uniform FDG avid wall thickening is usually due to inflammation (Fig. 5.5), though imaging features can overlap.
FDG avid cholecystitis. Coronal PET and fusion PET/CT images (arrowheads in a, c) in a biopsy-proven case of cholangiocarcinoma show a FDG avid soft tissue lesion obstructing the common bile duct. FDG uptake along the thickened wall of the gall bladder (arrows in a–c) is due to cholecystitis and can be erroneously diagnosed as second malignancy
5.4 Pitfalls Due to Treatment-Related Changes and Complications
Significant proportion of gall bladder cancers are diagnosed incidentally from the surgical specimen after elective cholecystectomy is performed for symptomatic calculus disease. Staging PET/CT studies then performed often show FDG uptake in the operated bed of the gall bladder fossa which is due to postoperative inflammation associated with normal healing [2, 9]. This false-positive FDG uptake can persist for several weeks after surgery and mimic disease leading to futile surgical explorations to remove residual disease (Fig. 5.6).
False-positive PET/CT after recent cholecystectomy. Coronal MIP, axial PET and fusion PET/CT images show intense FDG uptake in the GB fossa (arrows in a, b, d) in a patient with recent history (4 weeks) of cholecystectomy for symptomatic gall stones. Persistent FDG uptake is due to postoperative inflammation and can be confused with residual disease. No obvious mass lesion is seen in the GB fossa on axial CT image (arrowhead in c)
Patients after laparoscopic cholecystectomy for unsuspected gall bladder cancer occasionally develop metastasis at the site of laparoscopy ports. PET/CT can detect port site metastases by demonstrating increased FDG uptake in those regions [10]. Persistent inflammation at the port site causes FDG avidity that can mimic a metastatic deposit (Fig. 5.7). Careful attention should be given to the morphological changes accompanying the metabolic findings. Absence of a nodular soft tissue or a mass lesion at the port site favours an inflammatory pathology.
False-positive PET/CT after laparoscopic cholecystectomy. Coronal MIP and fused PET/CT images show focal FDG uptake in the anterior abdominal wall (arrows in a, c) corresponding to the ill-defined soft tissue at the laparoscopic port site. Biopsy revealed inflammation. This finding can simulate port site metastasis
Surgery in combination with chemo- and radiation therapy is used biliary and pancreatic cancers. Biliary drainage using percutaneous transhepatic technique (PTBD) or by endoscopic retrograde techniques (ERBD) is used to relieve obstructive jaundice before surgery or radiation and also as a palliative measure in advanced non-resectable tumours. Drainage tubes and stents cause inflammation of the biliary tree resulting in tracer uptake in the region of the stent [11] (Fig. 5.8). In most cases, uptake is along the stent and low grade in nature. Occasionally it can be intense and may mimic malignant disease. Intense uptake along the stent can also mask underlying small malignant lesion. Cholangitis and cholangitic abscess are serious complications of biliary drainage tubes and stents and can impair quality of life (Fig. 5.9). Intense FDG uptake is seen in cholangitis and can closely resemble cholangiocarcinoma. Cholangitic abscesses can often be mistaken as metastatic disease. Distribution of FDG avidity in a linear branching pattern along the biliary radicles and a photopenic fluid-filled centre of an abscess are important imaging features that can help differentiate inflammation from malignancy. Pancreatitis is also seen as a complication of biliary stenting as well as radiation therapy. Diffuse FDG uptake in the substance of the gland in combination with inflammatory CT features like pancreatic oedema, peripancreatic stranding and fluid collections can point towards the diagnosis of pancreatitis (Fig. 5.10).
False-positive PET/CT due to stent inflammation. Coronal MIP, axial PET images show focal uptake in the left lobe of the liver (arrows in a, b) corresponding to a percutaneous biliary drainage tube on fused PET/CT image (arrow in c). Coronal MIP and fusion PET/CT images show intense inflammatory uptake along the ERBD stent (arrowheads in a, d, e). Stent-associated inflammatory FDG uptake can be intense and mimic disease
False-positive PET/CT due to stent-related cholangitic abscess . Coronal MIP, axial PET and fused PET/CT show focal FDG uptake in the left lobe of the liver (arrows in a–c) corresponding to ring-enhancing abscesses seen on contrast CT (arrowhead). Black arrow seen in fusion PET/CT (d) show the ERBD stent
False-positive PET/CT due to post radiation pancreatitis. Axial PET and fused PET/CT show intense FDG uptake in the body and tail of pancreas (arrowheads in a, b). Oedematous pancreas with peripancreatic fat stranding and small collections is seen on contrast CT scan which is diagnostic (arrows in c)
Conclusion
The anatomical and pathological complexity of pancreatico-biliary tumours leads to varying patterns of FDG PET appearances. Changes produced by surgery, radiation therapy and biliary drainage procedures and complications caused by them can lead to alterations in expected imaging appearances. Thorough knowledge of these imaging pitfalls is necessary to avoid errors in PET/CT interpretation.
Key Points
-
The anatomical and pathological complexity of pancreatico-biliary tumours leads to varying patterns of FDG PET appearances.
-
Cholangiocarcinoma can show variable FDG uptake depending upon the anatomic location, growth pattern and histological subtype.
-
Lesions that are extrahepatic, infiltrative and mucinous in nature tend to show poor or no FDG concentration and can be difficult to localise on PET studies leading to false-negative results.
-
FDG PET/CT has been found to be better in distinguishing MFP from pancreatic adenocarcinoma by virtue of lower tracer uptake in the inflammatory lesion. However, certain cases of MFP can show high FDG avidity due to the inflammatory process and can simulate malignancy.
-
FDG PET can be falsely positive in cases of cholecystitis, and differentiation from malignancy can be difficult.
-
Patients after laparoscopic cholecystectomy for unsuspected gall bladder cancer occasionally develop metastasis at the site of laparoscopy ports. PET/CT can detect port site metastases by demonstrating increased FDG uptake in those regions.
-
Persistent inflammation at the port site causes FDG avidity that can mimic a metastatic deposit.
-
Intense FDG uptake is seen in cholangitis and can closely resemble cholangiocarcinoma.
-
Distribution of the FDG avidity in a linear branching pattern along the biliary radicles and a photopenic fluid-filled centre of an abscess are important imaging features that can help differentiate inflammation from malignancy.
-
Diffuse FDG uptake in the substance of the gland in combination with inflammatory CT features like pancreatic oedema, peripancreatic stranding and fluid collections can point towards the diagnosis of pancreatitis.
References
Kato T, Tsukamoto E, Kuge Y, Katoh C, Nambu T, Nobuta A, et al. Clinical role of [18]F-FDG PET for initial staging of patients with extrahepatic bile duct cancer. Eur J Nucl Med. 2002;29:1047e54.
Anderson CD, Rice MH, Pinson CW, Chapman WC, Chari RS, Delbeke D. Fluorodeoxyglucose PET imaging in the evaluation of gallbladder carcinoma and cholangiocarcinoma. J Gastrointest Surg. 2004;8:90e7.
Fritscher-Ravens A, Bohuslavizki KH, Broering DC, Jenicke L, Schafer H, Buchert R, et al. FDG PET in the diagnosis of hilar cholangiocarcinoma. Nucl Med Commun. 2001;22:1277e85.
Pedrazzoli S, Sperti C, Pasquali C, Bissoli S, Chierichetti F. Comparison of international consensus guidelines versus 18-FDG PET in detecting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Ann Surg. 2011;254(6):971.
Schick V, Franzius C, Beyna T, et al. Diagnostic impact of 18F-FDG PET-CT evaluating solid pancreatic lesions versus endosonography, endoscopic retrograde cholangio-pancreatography with intraductal ultrasonography and abdominal ultrasound. Eur J Nucl Med Mol Imaging. 2008;35:1775–85.
van Kouwen MC, Jansen JB, van Goor H, de Castro S, Oyen WJ, Drenth JP. FDG-PET is able to detect pancreatic carcinoma in chronic pancreatitis. Eur J Nucl Med Mol Imaging. 2005;32:399–404.
Koh T, Taniguchi H, Yamaguchi A, Kunishima S, Yamagishi H. Diffcerential diagnosis of gallbladder cancer using positron emission tomography with fluorine-18-labeled fluoro-deoxyglucose (FDG-PET). J Surg Oncol. 2003;84:74–81.
Oe A, Kawabe J, Torii K, Kawamura E, Higashiyama S, Kotani J, et al. Distinguishing benign from malignant gallbladder wall thickening using FDG-PET. Ann Nucl Med. 2006;20:699–703.
Abouzied MM, Crawford ES, Nabi HA. 18F-FDG imaging: pitfalls and artifacts. J Nucl Med Technol. 2005;33:145–55.
JB H, Sun XN, Xu J, He C. Port site and distant metastases of gallbladder cancer after laparoscopic cholecystectomy diagnosed by positron emission tomography. World J Gastroenterol. 2008;14:6428–31.
Corvera CU, Blumgart LH, Akhurst T, DeMatteo RP, D'Angelica M, Fong Y, Jarnagin WR. 18F-fluorodeoxyglucose positron emission tomography influences management decisions in patients with biliary cancer. J Am Coll Surg. 2008;206:57–65.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Purandare, N., Shah, S., Agrawal, A., Puranik, A., Rangarajan, V. (2018). FDG PET/CT: Normal Variants, Artefacts and Pitfalls in Hepatobiliary and Pancreatic Malignancies. In: Purandare, N., Shah, S. (eds) PET/CT in Hepatobiliary and Pancreatic Malignancies. Clinicians’ Guides to Radionuclide Hybrid Imaging(). Springer, Cham. https://doi.org/10.1007/978-3-319-60507-4_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-60507-4_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-60506-7
Online ISBN: 978-3-319-60507-4
eBook Packages: MedicineMedicine (R0)