Abstract
This chapter outlines the anatomy, clinical presentation, and relevant clinical investigations. Details of both non-neoplastic and neoplastic pathological conditions affecting the gallbladder are given. Clinical considerations in obtaining the diagnostic biopsy and therapeutic resection specimens are outlined, with details of their handling and dissection in the histopathology laboratory. This is correlated with relevant histopathology reports, giving summary core prognostic and patient management items. Current WHO and TNM classifications are referenced.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Anatomy
The gallbladder is a sac that lies on the inferoposterior surface of the liver. It is divided into the fundus (rounded portion that projects below the liver), body (lies in contact with the liver), and neck (becomes continuous with the cystic duct). Stones may cause a dilatation at the junction of the neck and cystic duct known as Hartmann’s pouch. The gallbladder is two-thirds surrounded by peritoneum which binds the non-peritonealized adventitial aspect of the body and neck to the under surface of the liver. The cystic duct is 4 cm long and joins the neck of the gallbladder to the right side of the common hepatic duct to form the common bile duct. The course of the cystic duct shows great variation between individuals. The gallbladder is concerned with the concentration, storage, and delivery of bile. To aid the concentration process the mucous membrane is thrown into permanent folds. The bile salts emulsify fats in the duodenum and so facilitate their digestion and absorption. When fatty food enters the duodenum, endocrine cells release hormones, which lead to contraction of the gallbladder and relaxation of the sphincter of Oddi, thus allowing bile to be delivered to the duodenum. The mucous membrane of the cystic duct is raised in the form of a spiral fold. This is thought to assist in keeping the lumen patent. An important surgical landmark (where the cystic artery can be found) is Calot’s triangle which is formed by the common hepatic duct, the cystic duct, and the liver (see Fig. 4.2).
Lymphovascular drainage:
The main arterial supply to the gallbladder is from the right hepatic artery via the cystic artery that runs through Calot’s triangle. The cystic vein drains directly to the portal system. Lymphatics from the gallbladder and bile ducts pass to the cystic node (situated near the gallbladder neck) and then through the infrahepatic nodes. At the distal end of the common bile duct, they pass into the peripancreatic and periduodenal nodes, and ultimately drain to the coeliac and superior mesenteric nodes (Fig. 9.1).
The regional lymph nodes are the hepatic hilus nodes (including nodes along the common bile duct, common hepatic artery, portal vein, and cystic duct), coeliac and superior mesenteric nodes (Used with the permission of the Union for International Cancer Control (UICC), Geneva, Switzerland. The original source for this material is from Wittekind et al. (2005))
2 Clinical Presentation
There is considerable overlap in the clinical features of gallbladder and extrahepatic bile duct disease. Gallstones are often asymptomatic. However, if there is gallbladder outlet obstruction by a stone, then progressively severe right upper quadrant “colicky” pain (biliary colic), associated with nausea and vomiting, may be felt. If the stone remains impacted, the gallbladder may become infected and acutely inflamed (acute cholecystitis)—this leads to severe constant right upper quadrant pain, pyrexia, and signs of localized peritonitis. This can progress to an empyema (pus-filled gallbladder). Stone impactation may also lead to a mucocele, i.e., a dilated gallbladder in which the bile has been resorbed but mucus secretion continues. A mucocele is heralded by a palpable gallbladder and dull right upper quadrant pain. Occasionally in the elderly the gallbladder may perforate, leading to generalized peritonitis. Gallstones localized to the cystic duct will occasionally cause obstructive jaundice, especially if the duct is short. The inflammation and oedema around the cystic duct impedes the flow of bile through the adjacent common bile duct (Mirizzi syndrome ). More commonly, a stone passes through and on into the common bile duct obstructing it. Gallstone ileus (small bowel obstruction due to impactation of a stone at the ileocaecal valve after the formation of a fistula between the gallbladder and duodenum) is a rare complication of cholecystitis.
Gallbladder carcinoma may present in a similar manner to gallstone disease, although weight loss and jaundice are additional features, obstructive jaundice being caused by metastatic spread to nodes which compress the bile ducts.
3 Clinical Investigations
There is considerable overlap in the investigation of gallbladder and extrahepatic bile duct disease.
-
Blood tests—FBC—elevated WCC in cholecystitis. LFTs may show elevated serum bilirubin or alkaline phosphatase, particularly if there is a stone in the common duct.
-
AXR—limited diagnostic use for detecting gallstones as only 10–15% of stones are radio-opaque; gas in the gallbladder wall (emphysematous cholecystitis) is a serious complication of cholecystitis seen most commonly in diabetics; in gallstone ileus, it will show the classic triad of small intestinal obstruction, gallstone in the right iliac fossa, and gas in the biliary tree.
-
USS—sensitive for stones >4 mm. This has supplanted the use of oral cholecystogram.
-
Oral cholecystogram—oral contrast is taken and this is absorbed from the gut, bound to albumin in the portal vein, and subsequently secreted in bile. Radiological imaging of the gallbladder is then carried out 10 h after ingestion. May be indicated when the clinical symptoms are strongly suggestive of gallstones but the USS is negative.
-
Cholangiography—intravenous cholangiography has been replaced by MRCP (magnetic resonance cholangiopancreatography) to assess the biliary tree non-invasively. MRCP may identify a mass. ERCP (endoscopic retrograde cholangiopancreatography) and PTC (percutaneous transhepatic cholangiography) are generally reserved for removing ductal stones but may also define strictures in the ductal system and allow collection of biliary brushings.
-
Percutaneous drainage—under radiological guidance can be used to drain the gallbladder in, e.g., empyema.
-
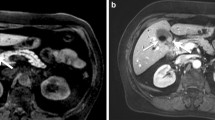
CT scan (chest, abdomen, and pelvis), may demonstrate a tumour mass, invasion of the liver, and compression of bile ducts.
4 Pathological Conditions
4.1 Non-neoplastic Conditions
Cholelithiasis (gallstones): The commonest aetiological agent in gallbladder pathology and classically occurring in fair, fat, fertile, females in their 40s. Mixed stones are the most frequent (80%) formed from an amalgam of bile, cholesterol, and calcium, and comprising biliary sludge, calculous gravel or multiple, faceted, laminated stones. Occasionally stones can be pure such as dark bilirubinate pigment stones in a congenital haemolytic disorder, e.g., spherocytosis, or, solitary, large, yellow, and cholesterol-rich.
Acute cholecystitis: 95% of cases are due to impaction of a stone in the cystic duct resulting in stasis, a bile-induced chemical reaction, and then secondary infection. The acute inflammation often subsides with conservative medical treatment but can persist producing an empyema—perforation and bile peritonitis are unusual. In a mucocele, the wall may calcify and form a “porcelain” gallbladder.
Chronic cholecystitis: Invariably associated with calculi, there are varying degrees of mucosal and transmural chronic inflammation, thickening of the muscularis, perimuscular fibrosis, and adherence to the liver bed. Indicators of chronicity are mucosal pseudopyloric metaplasia and transmural mucosal herniation to form Rokitansky–Aschoff sinuses . These mucosal pouches can inspissate with bile and mucus, becoming inflamed and forming extramural abscesses which may only partly resolve leaving a marked xanthogranulomatous histiocytic inflammatory reaction that encases the gallbladder. Prominent sinus formation at the fundus can similarly mimic a mucosal polyp or tumour, so-called cholecystitis glandularis proliferans . Unusual variants of chronic cholecysitis are follicular (reactive lymphoid aggregates), eosinophilic (often acalculous and chemical in nature), and malakoplakia. Due to the strong association with pancreatitis, fat necrosis and calcification may be seen.
Cholesterolosis: A relatively common finding of yellow mucosal flecks (“strawberry” gallbladder) due to accumulation of cholesterol-laden macrophages in the lamina propria. It is usually incidental and not associated with hypercholesterolaemia.
Oleogranulomas: The cystic duct lymph node is not infrequently enlarged and submitted along with the cholecystectomy specimen. It often contains oleogranulomas comprising fat spaces surrounded by histiocytes, presumably representing a gallbladder drainage phenomenon.
4.2 Neoplastic Conditions
Dysplasia: This can be flat or raised/papillary. Flat dysplasia is often an incidental finding and may be multifocal. Low grade dysplasia should prompt further examination of the gallbladder and submission of extra blocks to assess for high grade change or invasive malignancy. High grade dysplasia, especially if flat, can spread rapidly through the gallbladder and may require entire submission of the gallbladder. The cystic duct should be carefully examined for dysplasia. Raised papillary lesions may be greater than 1 cm and if so are best classified as intracholecystic papillary neoplasms. A spectrum of dysplasia may be found within these lesions, as can invasive malignancy. There may be flat dysplasia in the surrounding mucosa. Papillary neoplasms include the entity formally referred to as “non-invasive papillary carcinomas.” These lesions should be carefully examined to exclude invasive disease. In general three epithelial subtypes of dysplasia are recognized in the gallbladder: biliary, intestinal or gastric.
Carcinoma: Usually occurs in late middle-aged females and many (50–75%) present already with regional lymph node metastasis and involvement of the gallbladder bed, liver, or other direct spread to duodenum, stomach, colon, and peritoneum. Calculi (80–90% of cases), chronic inflammatory bowel disease, and primary sclerosing cholangitis are risk factors. Often clinically inapparent and found incidentally as diffuse thickening of the wall at cholecystectomy for gallstones, 10–20% are initially diagnosed by histology of routine blocks, there having been no macroscopic suspicion of tumour. Fundal in location (60%) and grossly diffuse (70%) or polypoid (30%), the vast majority (95%) are adenocarcinomas of tubular or papillary patterns arising from a sequence of intestinal metaplasia—dysplasia—carcinoma. Adenosquamous, pure squamous carcinomas, neuroendocrine tumours (well differentiated and poorly differentiated), and gastrointestinal stromal tumours can also occur in the gallbladder. Assessment of the depth of invasion can be difficult and extension of carcinoma in situ into Rokitansky–Aschoff sinuses must be distinguished from true invasion of the wall. Perineural involvement is characteristic. Gallbladder cancer may, therefore, be encountered either in the context of an incidental finding in a simple cholecystectomy, or infrequently, as an electively planned extended cholecystectomy (+/− segmental resection of liver) with radical lymph node dissection.
Other cancers: Rare but can include embryonal rhabdomyosarcoma (children), leiomyosarcoma and malignant lymphoma, or metastatic carcinoma, especially transcoelomic—stomach, pancreas, ovary, bile ducts, colon, and breast.
Prognosis: Better if lesions are of papillary type, low histological grade, and confined to the mucous membrane when resection is potentially curative (90% 5-year survival). However, many cases present with disease beyond the gallbladder, involvement of liver (25% 5-year survival), and overall 5–10% 5-year survival figures.
5 Surgical Pathology Specimens: Clinical Aspects
5.1 Resection Specimens
5.1.1 Benign Conditions
In benign disease, the gallbladder may be removed either laparoscopically or by an open procedure.
Laparoscopic cholecystectomy is now by far the most popular method. There are no absolute contraindications except for those that apply to other operative procedures, e.g., poor anaesthetic risk. However, previous abdominal surgery with resultant fibrous adhesions and obesity may make a laparoscopic approach difficult. It may have to be abandoned and converted to an open cholecystectomy. In a laparoscopic cholecystectomy, an initial small infraumbilical stab wound is made and a spring-loaded Veress needle is passed through the abdominal wall into the peritoneal cavity. A CO2 supply is then connected to the needle and gas is insufflated into the abdomen to produce a pneumoperitoneum. The needle is then removed and the incision extended and deepened. A sheath is then inserted and the laparoscope is passed through this to make the optic port. The image from the laparoscope is transferred to a monitor and can be viewed by the surgeon. Three other incisions (ports) are made under direct visualization: for retraction and irrigation, for tools such as an electrosurgical hook, scissors, etc., and for grasping forceps. An initial examination of all areas of the abdomen is performed, including the pelvis. The fundus of the gallbladder is then grasped, the cystic artery and duct in Calot’s triangle both clipped and divided. If cholangiography ± exploration of the common bile duct is required, a cannula is passed into the common bile duct via an opening in the cystic duct before clipping. The gallbladder is then dissected from the liver bed and the contents removed by suction. It is then placed in a bag and removed through the optic port.
Open cholecystectomy is used in the few cases deemed inappropriate for laparoscopic cholecystectomy via a Kocher’s incision parallel to the right subcostal margin.
5.1.2 Gallbladder Cancer
Careful patient selection for surgery of gallbladder cancer is essential and only relatively fit patients with localized tumours and no evidence of metastatic spread should be considered. However, despite this, the results of surgery remain poor, with 90% of patients dying within 12 months.
A right subcostal incision is used and a complete examination of the abdomen undertaken. If there is no invasion of the bile ducts and no or only superficial liver invasion, an extended cholecystectomy is performed. In this, after determination of the depth of liver invasion by intraoperative USS, the gallbladder and the hepatic gallbladder bed are removed in the form of a wedge resection. A regional lymph node dissection is carried out by removing the lymph nodes draining the gallbladder as far as the coeliac nodes.
If the tumour extends more deeply into the liver, then a segmental liver resection (usually IV and V or IV, V, and VI) will be required. Very occasionally, if the tumour has spread to the extrahepatic bile ducts, a segmental liver resection and extrahepatic duct resection are required. Rarely a liver resection and an extended Whipple’s procedure may be used. Palliation can involve bypass surgery or stenting to relieve gastric outlet obstruction or jaundice.
6 Surgical Pathology Specimens: Laboratory Protocols
6.1 Biopsy Specimens
Not applicable.
6.2 Resection Specimens
Specimen:
-
Most cholecystectomy specimens are now done laparoscopically rather than by open surgery and submitted opened or unopened containing 5–10 mL of bile fluid. Occasionally, specimens are received in several pieces if operative access has been technically difficult. The proximal end comprises a variable length of cystic duct adjacent to which an enlarged lymph node may be present.
Initial procedure:
-
Measurements:
-
Gallbladder—length × maximum diameter (cm)
-
Cystic duct—length × maximum diameter (cm)
-
Lymph node—number and maximum diameter (cm)
-
-
Open longitudinally from the fundus toward the cystic duct with blunt-ended scissors draining off the bile and noting any contents.
-
Photograph if appropriate.
-
Paint the external serosal and adventitial aspects if there is any suspicion of tumour.
-
Fixation by immersion in 10% formalin for 36–48 h.
Description:
-
Received
-
Opened/unopened/intact/deficient/perforated/fragments
-
-
Adventitia
-
Adhesions/rim of liver/tumour
-
-
Serosa
-
Adhesions/exudate/perforation/tumour
-
-
Wall
-
Thickness (cm)/fibrosis/tumour/thinning/necrosis/perforation/sinuses/abscess/calcification
-
-
Mucosa
-
Tumour: polypoid/nodular/ulcerated/diffuse/mucinous
Length × width × depth (cm) or maximum dimension (cm)
Location (fundus/body/neck/cystic duct) and distance (mm) to the cystic duct limit
Confined to mucous membrane, in the wall or through the wall
-
Cholesterolosis/ulceration/haemorrhage/polyps
-
-
Contents
-
Bile/mucus/stones (size, number, shape, mixed, pigment, cholesterol)/fibrin/pus
-
-
Cystic duct
-
Stone impaction/dilatation/lymph node
-
Blocks for histology (Fig. 9.2):
Opening and transverse sectioning of the gallbladder (Reproduced, with permission, from Allen and Cameron (2013))
-
Sample by circumferential transverse section the proximal cystic duct limit.
-
Sample the cystic duct lymph node and any other separately submitted named nodes.
-
Serially transverse section the gallbladder at 3–4 mm intervals with either a sharp knife or scissors.
-
Usually one broken transverse ring will suffice for histology in the absence of any macroscopic abnormality.
-
Sample gross lesions with multiple transverse blocks as indicated, e.g., ulceration, perforation, tumour, abscess, polyps, wall thickening. Demonstrate tumour in relation to the serosa and adventitia including its resection margin.
-
If part of a radical cancer resection—describe and measure the attached segments of liver and bile ducts, and the relationship of any tumour to them and their resection limits. Sample multiple blocks to demonstrate these relationships. Sample all regional lymph nodes.
Histopathology report:
-
Non-neoplastic
-
Inflammation: acute/chronic/xanthogranulomatous
-
Necrosis/perforation/abscess/empyema/fistula
-
Mucocele
-
-
Tumour type
-
Adenocarcinoma/other
-
-
Tumour differentiation
-
Well/moderate/poor
-
-
Tumour edge
-
Pushing/infiltrative/lymphoid response
-
-
Extent of local tumour spread: TNM 8: for carcinoma
pTis | Carcinoma in situ |
|---|---|
pT1 | Tumour limited to gallbladder wall |
a | Lamina propria |
b | Muscularis |
pT2 | Tumour invades perimuscular connective tissue; no extension beyond serosa or into liver |
pT3 | Tumour perforates serosa (visceral peritoneum) and/or directly invades the liver and/or one other adjacent organ or structure, e.g., stomach, duodenum, colon, pancreas, omentum, extrahepatic bile ducts |
pT4 | Tumour invades main portal vein or hepatic artery, or invades two or more extrahepatic organs or structures |
-
Lymphovascular invasion
-
Present/not present. Note perineural invasion
-
-
Regional lymph nodes
Hepatic hilus nodes (including along common bile duct, hepatic artery, portal vein, and cystic duct), coeliac and superior mesenteric nodes. A regional lymphadenectomy will ordinarily include 6 or more lymph nodes
pN0 | No regional lymph node mestastasis |
pN1 | 1–3 regional lymph node(s) |
pN2 | 4 or more regional nodes |
-
Excision margins
Cystic duct limit of tumour and mucosal dysplasia clearance (mm)
Adventitial margin of tumour clearance (mm)
Hepatic and common bile duct margins of tumour clearance (mm)
-
Other pathology
Calculi, primary sclerosing cholangitis
Bibliography
Adsay V, Saka B, Basturk O, Roa JC. Criteria for Pathologic sampling of gallbladder specimens. Am J Clin Pathol. 2013;140:278–80.
Albores-Saavedra J, Henson DE, Klimstra DS. Tumors of the gallbladder, extrahepatic bile ducts and ampulla of vater, Atlas of tumor pathology, vol. 3rd series. Fascicle 27. Washington, DC: AFIP; 2000.
Allen DC. Histopathology reporting. Guidelines for surgical cancer. 3rd ed. London: Springer; 2013.
Allen DC, Cameron RI. Histopathology specimens: clinical, pathological and laboratory aspects. 2nd ed. Berlin: Springer; 2013.
Beckingham IJ, editor. ABC of liver, pancreas and gall bladder diseases. London: BMJ Books; 2001.
Bosman FT, Carneiro F. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC Press; 2010.
Brierley JD, Gospodarowicz MK, Wittekind C, editors. TNM classification of malignant tumours. 8th ed. Oxford: Wiley-Blackwell; 2017.
Carter D, Russell RCG, Pitt HA, Bismuth H, editors. Rob and Smith’s operative surgery: hepatobiliary and pancreatic surgery. 5th ed. London: Chapman and Hall; 1996.
Goldin RD, Roa JC. Gallbladder cancer: a morphological and molecular update. Histopathology. 2009;55:218–29.
Mann CV, Russell RCG, Williams NS, editors. Bailey & love’s short practice of surgery. 22nd ed. London: Chapman and Hall Medical; 1995.
Odze RD, Goldblum JR, editors. Odze and Goldblum surgical pathology of the GI tract, liver, biliary tract, and pancreas. 3rd ed. Philadelphia: Saunders/Elsevier; 2015.
The Royal College of Pathologists. Cancer datasets (oesophageal carcinoma, gastric carcinoma, carcinomas of the pancreas, ampulla of vater and common bile duct, colorectal cancer, gastrointestinal stromal tumours (GISTs), liver resection specimens and liver biopsies for primary and metastatic carcinoma, endocrine tumours of the gastrointestinal tract including pancreas) and tissue pathways (gastrointestinal and pancreatobiliary pathology, liver biopsies for the investigation of medical disease and for focal liver lesions). Available via https://www.rcpath.org/profession/publications/cancer-datasets.html. Accessed Oct 2016
Wittekind C, Greene L, Hutter RVP, Klimfinger M, Sobin LH. TNM atlas: illustrated guide to the TNM/pTNM classification of malignant tumours. 5th ed. Berlin: Springer; 2005.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Kelly, P.J., Allen, D.C., Cameron, R.I., Loughrey, M.B. (2017). Gallbladder. In: Allen, D., Cameron, R. (eds) Histopathology Specimens. Springer, Cham. https://doi.org/10.1007/978-3-319-57360-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-57360-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-57359-5
Online ISBN: 978-3-319-57360-1
eBook Packages: MedicineMedicine (R0)